1. Introduction
In recent years, more and more attention has been paid to the association between climate change and human health. It has been reported that the ambient temperature, the key climatic change indicator, is able to lead to not only direct deaths and illnesses, but also the aggravation of cardiovascular and respiratory diseases [
1,
2,
3,
4]. Besides that, diurnal temperature range (DTR), defined as the difference between maximal and minimal temperature within one day, is considered as an important index of climate change and variability because it provides more information than the mean temperature alone [
5]. Due to the fact that during the 20th century, the minimum temperature raised three times quicker than the maximum temperature, DTR is currently decreasing in most parts of the world [
6,
7]. The reason for the observed changes in DTR might be related to both large-scale climate forcing and local effects [
7,
8]. Although DTR is decreasing in the context of long-term climate change, important short-term impacts of large DTR on human health are continuously found in many countries and regions, which still supports the notion of DTR being a risk factor for human health.
Until now, the adverse effects of higher DTR have been observed to be associated with mortality and morbidity. Most of these studies targeted the association between DTR and human death, including non-accidental, cardiovascular, and respiratory mortality, and significant effects were shown in Hong Kong [
9], Taiwan [
10], mainland China [
11], Japan [
10], Korea [
12] and Canada [
13]. Only a small portion of studies based on emergency and hospital data showed significant effects of DTR on cardiovascular and respiratory morbidity [
14,
15,
16,
17]. These studies mostly focused on the relationship between DTR and broad categories of cardiovascular and respiratory causes of death and morbidity. Information about the association between DTR and subgroups of cardiovascular disease of emergency room (ER) admissions is quite scarce. The elderly, who are more sensitive to temperature variations, constitute the largest proportion of cardiovascular deaths. Meanwhile, it has been reported that they were also a susceptible population affected by DTR [
10,
18]. Nevertheless, few studies have focused on the association between DTR and cause-specific cardiovascular disease among the elderly. In addition, less evidence is available to illustrate the effect modification of DTR, especially in cities of developing countries with a high risk of DTR exposure. Hence, there is a need to explore the adverse effects of DTR on cause-specific cardiovascular diseases morbidity, mortality and these modifying effects among the elderly.
In the present study, a time-series analysis was conducted to examine the modifying effect of gender, age and season on the association between DTR and ER admissions for cause-specific cardiovascular diseases among the elderly in Beijing, China. Better understanding of the effect modification of DTR on morbidity among the elderly, will provide useful information for the development of public health plans and risk assessments in the ambient environment.
4. Discussion
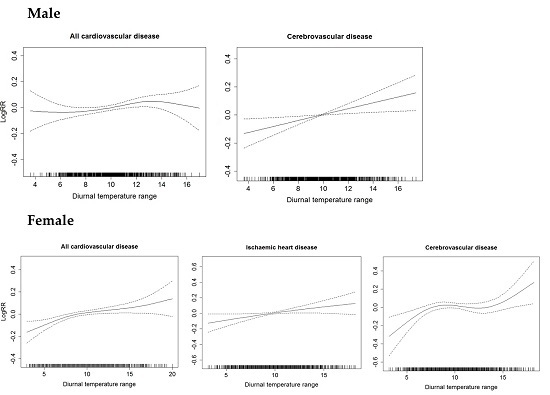
In this time series study, we examined the relationship between diurnal variations in temperature and the ER admissions for cause-specific cardiovascular disease among the elderly in Beijing. We found significantly acute effects of DTR on all cardiovascular and cerebrovascular disease ER admissions among males. Among females, DTR was significantly associated with ER admissions for all cardiovascular disease, ischemic heart disease and cerebrovascular disease. We observed stronger effects of DTR in people aged 75 years and over. The DTR caused greater adverse effects on both genders in warm season, but the effect estimates on females were higher in cold season than in warm season. The associations between DTR and ER admissions for cause-specific cardiovascular disease were robust to the adjustment for weather conditions and air pollutant concentrations.
Previous studies have shown the significant associations between DTR and cardiovascular mortality and morbidity. A recent study on 30 cities in China, Japan, Korea and Taiwan, China showed that DTR was associated with increased risk of death [
10]. In most cities, the adverse health association was greater for circulatory mortality and among the elderly, and the effect estimates of DTR among those ≥65 years varied from 0.45 (−0.76, 1.68) to 1.58 (0.00, 3.18) with cardiovascular mortality. In Korea [
16], a multicity study on the risk of hospital admissions for various cardiovascular diseases showed that DTR had adverse effect on cardiac failure with an effect estimates of 3.0 (1.4, 4.6). In Hong Kong (China) [
15], the adverse effect of DTR was associated with emergency heart failure admissions with an effect estimate of 0.86% (0.31%, 1.43%), and DTR exhibited a significantly greater effect on elderly patients (aged ≥75 years). In Japan [
28], a cohort study showed that all stroke and intracerebral hemorrhage in men aged 40 years and over was significantly related to intradiurnal temperature change. Our current study showed a greater effect of DTR on ER admissions for cause-specific cardiovascular diseases among the elderly, which was consistent with these reported studies. However, the evidence of the relationship between DTR and cardiovascular-specific morbidity was limited, with most of the findings concentrated in Asia. Similar studies needs to be conducted to assess DTR effects in other regions.
In the present study, we found that gender and age may modify the health effects of DTR. Compared with the younger population, the elderly were more susceptible to the adverse impact of DTR, which is consistent with prior studies in China [
11,
15], Korea [
12] and Japan [
10]. We also found the effects of DTR on all cardiovascular disease and ischemic heart disease ER admissions were greater in females than in males, and the effect of DTR on cerebrovascular disease ER admissions was reversed in both genders. However, results from prior studies on gender-specific effects of DTR were inconsistent. For example, Yang
et al. [
29] found that women in Guangzhou (China) were consistently more sensitive to the adverse effects of DTR on the total and cardiovascular mortality. Meanwhile, Lim
et al. [
12] found the similar results of deaths among females, which were associated more strongly with DTR than among males in six Korean cities. Qiu
et al. [
15] also reported significant effects of DTR on emergency hospital admissions for heart failure among females in Hong Kong (China). In contrast, Kan
et al. [
8] found significant effects of DTR on total mortality in both genders without a statistical significant difference by gender in Shanghai (China). Lim
et al. [
16] did not observe any gender-based DTR effects on cardiovascular and respiratory hospital admissions in four Korean cities. In previous systematic reviews on the effect modifiers of the temperature-mortality or -morbidity relationship, the differences of the temperature effects by gender were dependent on location and population [
1,
30], but evidence for modifiers of the DTR-health relationship in previous studies was limited, so the reasons for our gender-specific observations are unclear and deserve further investigation.
We also found that season may modify the effect of DTR. In our study, significant effects of DTR on both genders were observed in warm season, and the adverse effects on females were found to be higher in cold season than in warm season. According to previous studies, the joint effects between DTR and seasons on health were rarely explored and not explicitly indicated [
18]. Lim
et al.’s study [
12] showed that DTR was the greatest threat to vulnerable study populations, with greater influence in fall. The greater estimated effects of DTR were also observed in cold season in Hong Kong (China) on emergency heart failure admissions [
15] and in eight Chinese cities on total and cardiovascular mortality [
11], which implied the interaction between DTR and season. In our previous study, we also found that the significant effects of DTR on four major causes of ER admissions varied in spring, autumn and winter [
14]. For the present study, DTR was slightly larger in warm season than in cold season in Beijing, which may explain the fact that more adverse effects of DTR were found in warm season. Kim
et al. [
10] found the greater DTR effect in the higher DTR areas with the results from the meta-analysis in East Asia accordingly. In addition, women have been reported to have a greater risk from temperature change for coronary events and ischemic stroke in cold periods than do men [
31,
32]. In our study the stronger effect estimates of DTR among females in cold season were more likely to be caused by the cold effect.
Elderly people have been widely regarded as a susceptible population for temperature change [
18,
33]. They are less able to regulate body temperature, which thus may be more prone to adverse effects of temperature variation. A large change in temperature within one day may cause a sudden change in the heart rate and circulation of elderly people, which all may act to increase the risk of cardiovascular and other diseases, even lead to fatal consequences. Up to now, the physiological mechanism of DTR on cardiovascular disease has not been elucidated, although there are possible explanations on its effects. Temperature-induced damage is thought to be related to enhanced sympathetic reactivity followed by activation of the sympathetic nervous system, renin-angiotensin system, as well as dehydration and a systemic inflammatory response [
34]. Several cold pressor tests showed that the hemodynamic stresses and neurohumoral activation in association with temperature reduction were able to exacerbate heart failure, induce myocardial ischemia and precipitate arrhythmias [
35,
36,
37]. Under this background, the elderly with cardiovascular diseases may not adjust well to sudden outside temperature variation due to a decline in immune function and organs. Therefore, studies on the underlying mechanisms, by which temperature variation induces pathophysiological response and cardiovascular diseases, await profound and lasting investigation.
According to the data of the World Health Organization (WHO), cardiovascular diseases were the leading cause of non-communicable diseases (NCD) around the world in 2012, accounting for 46.2% of NCD deaths, or approximately 30% of all global deaths [
38]. Most previous epidemiological studies indicated that both low and high temperatures contributed to the increased risks of cardiovascular mortality or morbidity [
1,
33,
39,
40]. Two decades of research have also shown that air pollution can trigger heart attacks, strokes, and irregular heart rhythms, particularly in people whom already at risk for these conditions [
19,
41,
42]. Our findings of significant associations among mean temperature, air pollution and cardiovascular disease ER admissions within the elderly, are in consistent with those prior studies (
Table A1). However, the effect of DTR on ER admissions for cardiovascular disease remained statistically significant before and after adjustment for mean temperature and air pollutants in multiple models. Our results showed that the change in covariates for weather conditions and air pollutants did not substantially affect the estimated effects of DTR, suggesting that DTR is an independent risk factor for ER admissions among the elderly.
Our findings have potentially important health management implications. First, increased vigilance for large diurnal temperature fluctuations is important in elderly patients with cardiovascular disease, in order to prevent and control clinical symptoms at an early stage. Early warning systems for impending large temperature changes may reduce the impact of DTR on people’s health [
9]. Elderly females and people aged 75 years and older with cardiovascular disease should be monitored closely by family members or healthcare workers. They should be given advice on appropriate clothing and timely medication use for sudden temperature changes. Second, age, gender and season may modify the health effects of DTR on ER admissions for cardiovascular diseases in Beijing. Third, the effect of temperature change on morbidity emphasizes the need to better understand the underlying mechanisms.
In addition, our study has several limitations. Firstly, the data of ER admissions were only collected from three hospitals in Beijing, so a selection bias may exist. Secondly, we only used weather condition data from one meteorological station as a surrogate of personal exposure levels to diurnal temperature ranges. The use of ambient rather than personal exposure measurements is expected to result in exposure misclassification. However, the difference between these proxy values and the true exposures is an inherent and unavoidable measurement error. Thirdly, we did not analyze the effect on DTR modification by socioeconomic and educational level in our study. Although significant DTR effects after a modification by socioeconomic and educational level were found in a few studies [
12,
29], we would not collect that information from emergency room records. Fourth, we did not consider the difference between first-time ER admissions and people with a history of ER admissions, which may affect our results. Finally, since temperature variation may occur both indoors and outdoors, a few studies found that ownership and usage of air conditioning might reduce the effects of temperature on some health outcomes [
43,
44]. In addition, a large difference between outdoor and indoor temperature may have short-term impact on heart rate and blood pressure [
45]. We did not analyze the potentially confounding effect of air conditioning and the effect of indoor-outdoor temperature differences due to the lack of necessary data, which suggests research directions for another future in-depth study.