Improving Environmental Health Literacy and Justice through Environmental Exposure Results Communication
Abstract
:1. Introduction
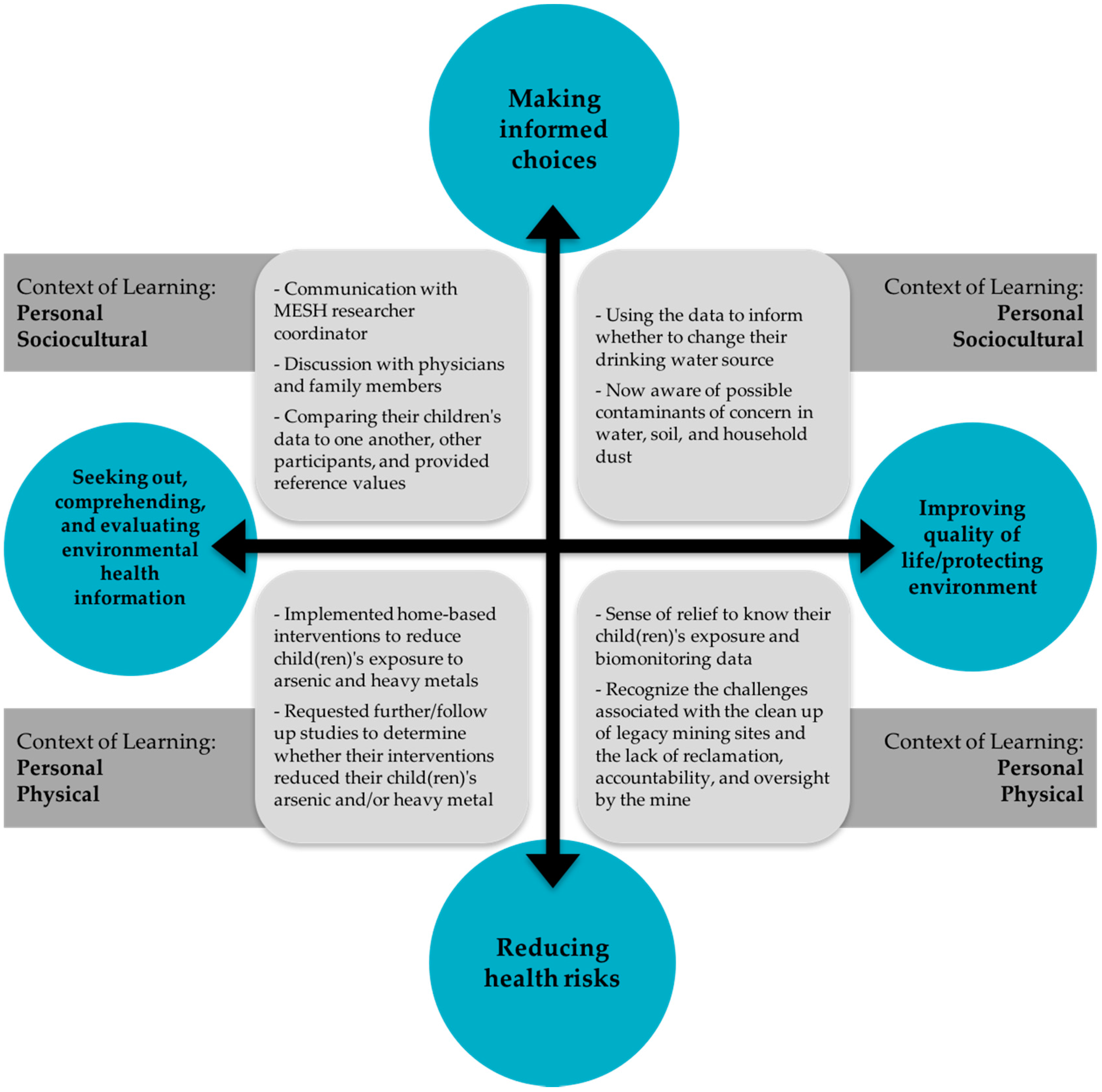
Theoretical and Analytical Frameworks
Environmental Justice
Environmental Health Literacy
Contextual Model of Learning
2. Materials and Methods
2.1. Study Population
2.2. The University of Arizona’s Metals Exposure Study in Homes
- The concentration of arsenic in their water sample was above 50 μg/L
- The concentration of lead in their water sample was above 15 μg/L (the current maximum contaminant level, MCL)
- Multiple children in home had creatinine-corrected urinary arsenic values over the 2013 National Health and Nutrition Examination Survey (NHANES) 95th percentile for children 6–11 years of age.
2.3. Personal Exposure Report-Back Ethics Study
2.4. Analysis
3. Results
3.1. Why Parents Participated in MESH
Because they’ve [US EPA] done air studies, and the air studies are saying … there’s not a lot of arsenic or lead in the particles in the dust, but somehow or another, I didn’t believe it; I really didn’t. … I’ve always wanted to see for myself what’s going on, and so that’s one of the reasons why I wanted to participate”.
3.2. Reducing Health Risks and Making Informed Choices
The Humboldt Unified Water Company that I'm currently spending $75 a month for my water, because I don’t think that I should have to pay for something that isn’t up to par. And if they’re posting signs not to use the water and cooking in and drinking, then I think that maybe there should be some kind of rebate.
We know it’s in the tap water even if you don’t have your own well, and there’s notices all over Humboldt about the—it doesn’t say “Don’t drink the water. Don’t have the water.” It just says “The Humboldt water has a higher level of arsenic this week” or whatever, and they put it in the paper. But they don’t tell you what to do.
Yes, I had heard that the water was bad here prior to the warnings that we had gotten from the sheriff's department. But once you see it compared from home samples on your own land that you're living in soil and water tables it strikes you deeper.
When you’re sweeping and dusting, try to do a wet dust when you’re wiping things down. Switch out your vacuum cleaner bag more often…. My kids now take off their shoes as they enter the house. So that there’s less dust accumulating in the home.
I’ve got a really good view of that whole thing. So when wind comes through you can see the dust flying. And that dirt back there on the Iron King [mine tailings pile] one is orange. And the one here closest to me [smelter slag pile] is whiter. It looks like ash kind of. So. Even though like 95 percent of the storms and the winds that were always coming from the south and going north…I know that they [US EPA] got a big plan together and they put some kind of stuff over the dust to keep it from blowing in the wind and everything. But that only lasts so long and it starts up again…Is there anybody else besides the EPA? I mean do they bring other people? Do they have people that monitor for them while they′re not here?
3.3. Seeking Out, Comprehending, and Evaluating Environmental Health Information
3.3.1. Understandings about Exposure or Health Outcomes
Before the MESH study I didn't even think at all that there were metals in the soil and in our water. It just brought to light that there are certain chemicals and metals and things that are combined with our water and our soil and that they can have a—if the levels are raised enough, they can have a negative effect.
When I was a kid, like my mom said, it was there before I was born. We used to go out there. My dad would be doing stuff out there, and we’d be playing around, and—you know I’ve just been around it my whole entire life. And it’s never seemed to bother anything.
3.3.2. Report Back Styles and Comparisons Made by Parents
I liked the individual reports. It was easier for me to see the information that I wanted. In the final summary I can compare to other people but, ultimately, I don’t really care in a personal sense. It's interesting in a scientific sense for me to know what’s going on in the area. In this area I wanted to know what the exposure was in our daily routine.
3.3.3. Comparing Siblings
She’s my oldest…she’s not outside as much as the younger ones. But is it concerning to me that her levels are higher than theirs in regards to arsenic. It’s almost double or triple the amount that the two younger ones are at…that’s probably the main concern really.
The lead in my daughter… Hers was raised, compared to my younger ones. And she's not really outside that much compared to the activity that they are outside. But that's probably the main concern really, the main question that I had was because why is hers, her level higher than theirs and she's not out as much as they are.
This says that my son, the oldest child that went to the study, has higher levels of arsenic than the other two. I have no idea why that’s the case. They’re all exposed to the same air, water, and dirt. Possibly, now that I’m analyzing it, it has something to do with the fact that he takes insulin. He’s diabetic, or maybe it’s the other way around, or maybe that’s why he’s diabetic. We don’t know what causes diabetes.
(One parent talking to another): Remember when we talked about that, because she went to school, he stayed home. That’s going to have somewhat of a big difference because she was away from the house, she wasn’t, I don’t know—it’s kind of a big difference, because she was at school.
3.3.4. Comparing Across the Study
3.3.5. Environmental Samples
3.3.6. Desire for Further/Future Studies
I want to look into it and see if there’s any long lasting results for my children is mainly the thing I want to—you know is there anything I can do? Other than obviously by knowing this I’m gonna change how they play outside and, you know the water they’re drinking and all that kind of thing. But is there anything else I do to kind of help with what they’ve already been exposed to?
3.4. Challenges Reported by Participants
3.4.1. Additional Inquiries
That was why I asked [MESH manager] when he called. He said “what don’t you understand” and [participant responded] “is there anything in there that we need to worry about?”.
I was going back and forth. But still, I know that I didn’t have all of it 100 percent in my head. So, you know when I went over it on the phone with [MESH manager] and at that time I remember him explaining it and I was understanding it better.
All I can think of is how much is the maximum you can have without it hurting you.
What is bad? What is the risk at that level? What do I do if it’s something that’s above the standard? What do I do?
I would say in some of the metals, maybe explain what the metal is. And maybe if it has a negative effect on your body.
I understand what lead is, but there were other things that were different names that I’d never even heard of before, and I didn’t understand what they were…The elements should have been described, explain how the children could be in contact with the element and what each element is.
Now that you know your results, here’s what you can do for your kids. That would be kind of neat.
Before I talked to [MESH manager] I opened it up, I looked at it, and I go, “What the heck? What is this about?” I read this over here, yes, and then, of course, I put two and two together, but there are thousands of questions on my mind. How’s it going to affect a four or five-year-old child? What’s the effect of his brain growing, his body growing, and what’s he going to do? How can we flush his body, get all those metals out? Something like that. Go in depth, especially when children are involved.
One set of parents noticed their beryllium levels were elevated in water and stated “the concern is what is beryllium? And then what’s the effect of beryllium? And then what can we do to ourselves to protect us from it?”
3.4.2. Physician Knowledge and Advice
3.4.3. Comparative Values
In terms of the standards of what it should be, our kids are well within that or well below that. One of them was about the 50th percentile and one of them was below it. That’s the 50th percentile so they’re average, what the average person is. I still was the same. Why is there arsenic in their urine? I don't want any arsenic in their urine but then I thought about this is still pretty standard or average for most people. That’s the way I thought about it.
3.4.4. Reporting Data Spatially
3.4.5. Resource Networking
4. Discussion
4.1. Study Limitations
4.2. Implications for Future Report Back Efforts
4.2.1. Improving Health Care Practitioner’s EHL and Involvement in EJ Communities
4.2.2. Mapping Data and Privacy
You can know where I live and what my exposure…it is not necessarily super private information. It′s not like I′m telling people my personal medical information…Anyway, I personally would consent to being a dot on a map and the details of that even if it did disclose that I participated in that study or that I was part of it.
4.2.3. Reporting Data Back in the Context of Risk and Health Outcomes
- Cancer Slope Factor-Based upon previous epidemiological studies, the US EPA has established a reference dose (RfD) and cancer slope factor (CSF) for arsenic. The CSF (1.5 milligram/kilogram, body weight-day) may be used by regulatory agencies to estimate an increased cancer risk from a lifetime oral exposure to an agent. Perhaps the CSF could have been used to interpret the data and provide a frame related to risk. For example, the concentrations observed in the environmental samples (water, soil, dust), combined with the child health questionnaire data on exposure (e.g., ingestion of water, duration out/indoors), could have been used to estimate the child’s average daily dose of arsenic, and then this value could then be compared to the CSF. If a CSF is available, it may be useful to use them, but only with an explanation of how these values are developed and with a clear description of the assumptions that go into an exposure assessment. Though a CSF could have been used for the MESH study, in general, few health-based values (such as a RfD, CSF, reference concentration or BEI) are available to put biomonitoring results into context [5].
- A Transparent, Bi-directional Discussion about Risk Assessment with Communities—Current knowledge of exposure and dose is limited for most contaminants of concern and since the human health risk model is sequential, the lack of accurate information can severely weaken the ability to assess risk and protect human health [68]. These data gaps are more pronounced in children’s exposure assessment (e.g., [69]). A more holistic approach is necessary if risk assessment is to remain a relevant and reliable decision-making tool [70]. Efforts are needed to improve cumulative (multiple chemicals) and aggregate (multiple routes) exposure and dose modeling and children’s exposure assessments need to be further informed by physiologic characteristics (e.g., absorbed dose), behavioral development (e.g., manual dexterity), hand-to-mouth frequency (e.g., [71]), physical activities, diet and eating habits, gender, socioeconomic status (SES) and race/ethnicity [72]. A risk assessment that clearly defines the gaps and limitations of the current paradigm, in addition to NHANES data, may provide an additional level of learning, offer another way to interpret exposure data, and further assist a community member to translate the results into action. Reporting data back in terms of risk may prepare and equip communities neighboring state and federal Superfund sites with the “risk language” in order to then critically assess cleanup decisions [25]. It is recommended to initiate a risk assessment dialogue with communities neighboring contamination beyond the one-directional traditional model. This dialogue should not only describe the inherent difficulty of establishing the existence of a causal relationship between measured concentrations of environmental pollutants and health effects, but more importantly, to work with the community to more accurately define the characteristics that influence a child’s exposure. Children themselves (ages 8 and up) can report their activity patterns and diet and eating [73] and this would facilitate informal science learning. Families can work together to inform exposure parameters related, but not limited to behavioral development and the role socioeconomic status and race/ethnicity play in their child’s exposures.
- Provide Other Empirical Data Sets for Reference-Another suggestion would be to frame participants’ results in terms of other empirical data sets and this suggestion echoes a MESH participant’s recommendation to add international data to the report, and specifically referenced Bangladesh (known for high arsenic levels in drinking water). Researchers could provide the data from larger epidemiological studies and the type of health effects that were associated with those findings. For example, a table or infographic depicting population size, sources of pollutants (in this case arsenic), exposure route(s), environmental and biomonitoring data, identified health effects, and other relevant factors related to the population (e.g., SES) from studies completed in highly exposed populations such as Bangladesh (e.g., [74]), Chile (e.g., [75]), Mexico (e.g., [76]), and Taiwan (e.g., [77]) and those that have been exposed at relatively low levels (e.g., [78,79,80]). These studies could be presented to participants to address their interest in health effects and risks associated with arsenic exposure, such as increased risk of cancer, cardiovascular and respiratory conditions, and diabetes mellitus [79]. This approach would frame their exposure by referencing other large-scale studies and it would further participants’ EHL and understanding of exposure science and epidemiology, shed light upon the studies used to generate reference doses and CSF, and further emphasize that more research needs to be focused upon low-level chronic exposure in children. In contrast, there is a chance that this comparison could make people think they are okay since others are worse off. By providing the data from previous epidemiological studies, including both those with high and relatively low exposure levels, we anticipate this will not be the case and that participants will observe the range of exposures and what type of short- and long-term health effects are associated with the contaminant of concern and exposure pathway. Overall, this approach will provide another opportunity to promote EHL.
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ADEQ | Arizona Department of Environmental Quality |
| CAB | Community Advisory Board |
| CDC | Center for Disease Control |
| MESH | Metal Exposure Study in Homes |
| NHANES | National Health and Nutrition Examination Survey |
| PERE | Personal Exposure Report-Back Ethics |
| US EPA | United States Environmental Protection Agency |
| UASRP | University of Arizona Superfund Research Program |
References
- Sexton, K.; Needham, L.; Pirkle, J. Human biomonitoring of environmental chemicals: Measuring chemicals in human tissues is the “gold standard” for assessing exposure to pollution. Am. Sci. 2004, 92, 38–41. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Fourth Report on Human Exposure to Environmental Chemicals, Updated Tables, (February, 2015). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA. Available online: http://www.cdc.gov/exposurereport/ (accessed on 25 April 2016).
- Morello-Frosch, R.; Brody, J.G.; Brown, P.; Altman, R.G.; Rudel, R.A.; Pérez, C. Toxic ignorance and right-to-know in biomonitoring results communication: A survey of scientists and study participants. Environ. Health 2009. [Google Scholar] [CrossRef] [PubMed]
- Vastag, B. CDC unveils first report on toxins in people. J. Am. Med. Assoc. 2001, 285, 1827–1828. [Google Scholar]
- Committee on Human Biomonitoring for Environmental Toxicants; Board on Environmental Studies and Toxicology; Division on Earth and Life Studies. National Academy of Sciences. Human Biomonitoring for Environmental Chemicals; Committee on Human Biomonitoring for Environmental Toxicants; Board on Environmental Studies and Toxicology; Division on Earth and Life Studies: Washington, DC, USA, 2006. [Google Scholar]
- Brody, J.G.; Dunagan, S.C.; Morello-Frosch, R.; Brown, P.; Patton, S.; Rudel, R.A. Reporting individual results for biomonitoring and environmental exposures: Lessons learned from environmental communication case studies. Environ. Health 2014, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
- US General Accounting Office. Siting of Hazardous Waste Landfills and Their Correlation with Racial and Economic Status of Surrounding Communities; United States General Accounting Office: Washington, DC, USA, 1983.
- United Church of Christ. Toxic Wastes and Race in the United States: A National Report on the Racial and Socio-Economic Characteristics of Communities Surrounding Hazardous Waste Sites; United Church of Christ, Commission for Racial Justice: New York, NY, USA, 1987. [Google Scholar]
- Bullard, R.; Johnson, S. Environmental justice: Grassroots activism and its impact on public policy decision making. J. Soc. Issues 2000, 56, 555–578. [Google Scholar] [CrossRef]
- Pastor, M., Jr.; Sadd, J.; Hipp, J. Which came first? Toxic facilities, minority move-in, and environmental justice. J. Urban Affairs 2001, 23, 1–21. [Google Scholar] [CrossRef]
- Chakraborty, J.; Collins, T.W.; Grineski, S.E.; Montgomery, M.C.; Hernandez, M. Comparing Disproportionate Exposure to Acute and Chronic Pollution Risks: A Case Study in Houston, Texas. Risk Anal. 2014, 34, 2005–2020. [Google Scholar] [CrossRef] [PubMed]
- Brown, P. Race, class, and environmental health: A review and systematization of the literature. Environ. Res. 1995, 69, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Morello-Frosch, R.; Pastor, M.; Porras, C.; Sadd, J. Environmental justice and regional inequality in Southern California: Implications for future research. Environ. Health Perspect. 2002, 110, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Agyeman, J.; Bullard, R.D.; Evans, B. Exploring the nexus: Bringing together sustainability, environmental justice and equity. Space Polity 2010, 6, 77–90. [Google Scholar] [CrossRef]
- Grineski, S.E. Incorporating health outcomes into environmental justice research: The case of children’s asthma and air pollution in Phoenix, Arizona. Environ. Hazard. 2007, 7, 360–371. [Google Scholar] [CrossRef]
- Hartley, D. Rural Health Disparities, Population Health, and Rural Culture. Am. J. Public Health 2004, 94, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- Emmett, E.; Desai, C. Community first communication: Reversing information disparities to achieve environmental justice. Environ. Justice 2010, 3, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Kozlowski, M.; Perkins, H.A. Environmental justice in Appalachia Ohio? An expanded consideration of privilege and the role it plays in defending the contaminated status quo in a white, working-class community. Local Environ. 2015, 1, 1–17. [Google Scholar] [CrossRef]
- Sparks, P.J. Rural Health Disparities. In International Handbook of Rural Demography; Springer: Dordrecht, The Netherlands, 2011; Volume 3, pp. 255–271. [Google Scholar]
- Glasmeier, A.; Farrigan, T. Poverty, sustainability, and the culture of despair: Can sustainable development strategies support poverty alleviation in America’s most environmentally challenged communities? Ann. Am. Acad. Pol. Soc. Sic. 2003, 590, 131–149. [Google Scholar] [CrossRef]
- Ramirez-Andreotta, M.D.; Lothrop, N.; Wilkinson, S.T.; Root, R.; Artiola, J.F.; Klimecki, W.; Loh, M.M. Analyzing Patterns of Community Interest at a Legacy Mining Waste Site to Assess and Inform Environmental Health Literacy Efforts. J. Environ. Stud. Sci. 2015. [Google Scholar] [CrossRef]
- Hoover, A. Connecting Disciplines to Inform and Develop the Emerging Field of Environmental Health Literacy. 2014. Available online: http://www.niehs.nih.gov/research/supported/dert/programs/peph/webinars/health_literacy/ (accessed on 5 May 2015). [Google Scholar]
- Society for Public Health Education. What Is Environmental Health Literacy? Available online: http://www.sophe.org/environmentalHealth/key_ehl.cfm (accessed on 4 May 2015).
- Finn, S.; O’Fallon, L. The Emergence of Environmental Health Literacy—From Its Roots to Its Future Potential. Environ. Health Perspect. 2015. [Google Scholar] [CrossRef]
- Ramirez-Andreotta, M.D.; Brody, J.; Lothrop, N.; Loh, M.; Beamer, P.; Brown, P. Reporting Back Environmental Exposure Data and Free-Choice Learning. Environ. Health 2016. [Google Scholar] [CrossRef]
- Ramirez-Andreotta, M.D.; Brusseau, M.L.; Artiola, J.F.; Maier, R.M.; Gandolfi, A.J. Building a co-created citizen science program with gardeners neighboring a Superfund site: The Gardenroots case study. Int. Public Health J. 2014, 7, 139–153. [Google Scholar]
- Altman, R.G.; Morello-Frosch, R.; Brody, J.B.; Brown, P. Pollution Comes Home and Gets Personal: Women’s Experience of Household Chemical Exposure. J. Health Soc. Behav. 2009, 49, 417–435. [Google Scholar] [CrossRef]
- Adams, C.; Brown, P.; Morello-Frosch, R.; Brody, J.G.; Rudel, R.; Zota, A.; Dunagan, S.; Tovar, J.; Patton, S. Disentangling the exposure experience: The roles of community context and report-back of environmental exposure data. J. Health Soc. Behav. 2011, 52, 180–196. [Google Scholar] [CrossRef] [PubMed]
- Falk, J.H.; Storksdieck, M. Using the Contextual Model of Learning to understand visitor learning from a science center exhibition. Sci. Educ. 2005, 89, 744–778. [Google Scholar] [CrossRef]
- Falk, J.H.; Storksdieck, M.; Dierking, L.D. Investigating public science interest and understanding: Evidence for the importance of free-choice learning. Public Underst. Sci. 2007, 16, 455–469. [Google Scholar] [CrossRef]
- U.S. Census Bureau 2010 Census. Available online: http://factfinder.census.gov/faces/affhelp/jsf/pages/metadata.xhtml?lang=en&type=table&id=table.en.DEC_10_DP_DPDP1#main_content (accessed on 4 May 2015).
- Ramirez-Andreotta, M.D.; Brusseau, M.L.; Beamer, P.; Maier, R.M. Home gardening near a mining site in an As-endemic region of Arizona: Assessing as exposure dose and risk via ingestion of home garden vegetables, soils, and water. Sci. Total Environ. 2013. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Andreotta, M.D.; Brusseau, M.L.; Artiola, J.F.; Maier, R.M. A Greenhouse and Field-Based Study to Determine the Accumulation of Arsenic in Common Homegrown Vegetables. Sci. Total Environ. 2013, 443, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Loh, M.L.; Sugeng, A.; Lothrop, N.; Klimecki, W.; Cox, M.; Wilkinson, S.T.; Lu, Z.; Beamer, P. Multimedia exposures to arsenic and lead for children near an inactive mine tailings and smelter site. Environ. Res. 2016, 146, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Uhlman, K.; Rock, C.; Artiola, J.F. Arizona Drinking Water Well Contaminants. The University of Arizona Extension Bulletin AZ 1503. 2009. Available online: https://www.cals.arizona.edu/pubs/water/az1503.pdf (accessed on 15 July 2012).
- Towne, D.; Jones, J. Groundwater Quality in Arizona: A 15-Year Overview of the ADEQ Ambient Monitoring Program (1995–2009), 2011. Available online: https://www.azdeq.gov/environ/water/assessment/download/1104ofr.pdf (accessed on 20 May 2015).
- US Department of Human Health Services, Health Resources and Services Administration. Medically Underserved Areas/Populations. Available online: http://www.hrsa.gov/shortage/mua/index.html (accessed on 20 November 2014).
- Ramirez-Andreotta, M.D.; Brusseau, M.L.; Artiola, J.F.; Maier, R.M.; Gandolfi, A.J. Environmental Research Translation: Enhancing Interactions with Communities at Contaminated Sites. Sci. Total Environ. 2014, 497–498, 651–664. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). CDC’s Childhood Lead Poisoning Prevention Program, (March 2016). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA. Available online: http://www.cdc.gov/nceh/lead/acclpp/blood_lead_levels.htm (accessed on 29 April 2016).
- Center for Disease Control and Prevention. Fourth National Report on Human Exposure to Environmental Chemicals, Updated Tables, February 2015. Available online: http://www.cdc.gov/biomonitoring/pdf/FourthReport_UpdatedTables_Feb2015.pdf (accessed on 16 June 2016).
- Pinson-Millburn, N.M.; Fabian, E.S.; Schlossberg, N.K.; Pyle, M. Grandparents Raising Grandchildren. J. Couns. Dev. 1996, 74, 548–545. [Google Scholar] [CrossRef]
- American Association of Retired Person. Grandfacts: State Factsheets for Grandparents and Other relatives Raising Children. 2014. Available online: http://www.aarp.org/relationships/friends-family/grandfacts-sheets/ (accessed on 8 February 2015).
- Sievers, E. Nutrient Minerals in Drinking Water: Implications for the Nutrition of Infants and Young Children; WHO Press: Geneva, Switzerland, 2005; pp. 164–179. [Google Scholar]
- Azoulay, A.; Garzon, P.; Eisenberg, M.J. Comparison of the Mineral Content of Tap Water and Bottled Waters. J. Gen. Intern. Med. 2001, 16, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Stone, R. Arsenic and Paddy Rice: A Neglected Cancer Risk? Science 2008, 321, 184–185. [Google Scholar] [CrossRef] [PubMed]
- US Food and Drug Administration. Arsenic in Rice and Rice Products. Available online: http://www.fda.gov/Food/FoodborneIllnessContaminants/Metals/ucm319870.htm (accessed on 25 April 2016).
- Aposhian, H.V.; Gurzau, E.S.; Le, X.C.; Gurzau, A.; Healy, S.M.; Lu, X.; Ma, M.; Yip, L.; Zakharyan, R.A.; Maiorino, R.M.; et al. Occurrence of monomethylarsonous acid in urine of humans exposed to inorganic arsenic. Chem. Res. Toxicol. 2000, 13, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, K.L.; Jones, R.L.; Verdon, C.P.; Jarrett, J.M.; Caudill, S.P.; Osterloh, J.D. Levels of urinary total and speciated arsenic in the U.S. population: National Health and Nutrition Examination Survey 2003–2004. J. Expo. Sci. Environ. Epidemiol. 2009, 19, 59–68. [Google Scholar] [CrossRef] [PubMed]
- US Environmental Protection Agency. Exposure Factors Handbook: 2011 Edition. National Center for Environmental Assessment, Washington, DC; EPA/600/R-09/052F. Available from the National Technical Information Service, Springfield, VA. Available online: http://www.epa.gov/ncea/efh.2011 (accessed on 8 June 2015).
- National Oceanic and Atmospheric Administration. Fisheries of the United States. National Marine Fisheries Service. 2013. Available online: http://www.st.nmfs.noaa.gov/commercial-fisheries/fus/fus13/index (accessed on 8 June 2015). [Google Scholar]
- Agusa, T.; Kunito, T.; Minh, T.B.; Kim Trang, P.T.; Iwata, H.; Viet, P.H.; Tanabe, S. Relationship of urinary arsenic metabolites to intake estimates in residents of the Red River Delta, Vietnam. Environ. Pollut. 2009, 157, 396–403. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Safety Evaluation of Certain Contaminants in Food. 2011. Available online: http://whqlibdoc.who.int/publications/2011/9789241660631_eng.pdf (accessed on 3 June 2015).
- Agency for Toxic Substances and Disease Registry. Toxicological Profile for Arsenic. 2005. Available online: http://www.atsdr.cdc.gov/toxprofiles/tp2.pdf (accessed on 10 May 2015). [Google Scholar]
- Gollenberg, A.L.; Hediger, M.L.; Lee, P.A.; John, H.; Himes, J.H.; Buck Louis, G.M. Association between Lead and Cadmium and Reproductive Hormones in Peripubertal U.S. Girls. Environ. Health Perspect. 2010, 18, 1782–1787. [Google Scholar] [CrossRef] [PubMed]
- Diamond, G.L.; Thayer, W.C.; Choudhury, H. Pharmacokinetic/pharmacodynamics (PK/PD) modeling of risks of kidney toxicity from exposure to cadmium: Estimates of dietary risks in the U.S. population. J. Toxicol. Environ. Health 2003, 66, 2141–2164. [Google Scholar] [CrossRef] [PubMed]
- Khoong, E.C.; Gibbert, W.S.; Garbutt, J.M.; Sumner, W.; Brownson, R.C. Rural, Suburban, and Urban Differences in Factors That Impact Physician Adherence to Clinical Preventive Service Guidelines. J. Rural Health 2014, 30, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Crain, E.F. Environmental threats of children’s health: A challenge for pediatrics: 2000 Ambulatory Pediatric Association presidential address. Pediatrics 2000, 106, 871–875. [Google Scholar] [PubMed]
- Etzel, R.A.; Crain, E.F.; Gitterman, B.A.; Oberg, C.; Scheidt, P.; Landrigan, P.J. Pediatric environmental health competencies for specialists. Ambul. Pediatr. 2003, 3, 60–63. [Google Scholar] [CrossRef]
- Brody, J.G.; Morello-Frosch, R.; Brown, P.; Rudel, R.A.; Altman, R.G.; Frye, M.; Osimo, C.A.; Perez, C.; Seryak, L.M. Improving disclosure and consent: “Is It safe?”: New ethics for reporting personal exposures to environmental chemicals. Am. J. Public Health 2007, 97, 1547–1554. [Google Scholar] [CrossRef] [PubMed]
- Occupational Safety and Health Administration. Section II, Chapter 2: Surface Contaminants, Skin Exposure, Biological Monitoring and Other Analyses, (February 2014). U.S. Department of Labor: Washington, DC, USA. Available online: https://www.osha.gov/dts/osta/otm/otm_ii/otm_ii_2.html (accessed on 30 April 2016).
- Brown, P. Popular Epidemiology, Toxic Wastes, and Social Movements. In Medicine, Health and Risk: Sociological Perspectives; Jonathan, G., Ed.; Blackwell: Oxford, UK, 1995; pp. 91–112. [Google Scholar]
- US Environmental Protection Agency. Environmental Health Resources for Community Members. 2016. Available online: https://www.epa.gov/communityhealth (accessed on 15 June 2016). [Google Scholar]
- Center for Disease Control. Protocol for Assessing Community Excellence in Environmental Health. 2016. Available online: https://www.cdc.gov/nceh/ehs/ceha/pace_eh.htm (accessed on 15 June 2016). [Google Scholar]
- Bradman, A.; Salvatore, A.L.; Boeniger, M.; Castorina, R.; Snyder, J.; Barr, D.; Jewell, N.P.; Kavanagh-Baird, G.; Striley, C.; Eskenazi, B. Community-Based Intervention to Reduce Pesticide Exposure to Farmworkers and Potential Take-Home Exposure to their Families. J. Expo. Sci. Environ. Epidemiol. 2009, 19, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Pediatrics Environmental Health Specialty Units. Available online: http://www.pehsu.net/ (accessed on 15 June 2016).
- US Environmental Protection Agency. Search for Superfund Sites Where You Live. 2016. Available online: https://www.epa.gov/superfund/search-superfund-sites-where-you-live (accessed on 30 April 2016). [Google Scholar]
- US Environmental Protection Agency. Toxic Release Inventory Program. 2016. Available online: https://www.epa.gov/toxics-release-inventory-tri-program (accessed on 30 April 2016). [Google Scholar]
- Ott, W.; Wallace, L.; Mage, D.; Akland, G.; Lewis, R.; Sauls, H.; Rodes, C.; Kleffman, D.; Kuroda, D.; Morehouse, K. The Environmental Protection Agency’s Research Program on Total Human Exposure. Environ. Int. 1986, 12, 475–494. [Google Scholar] [CrossRef]
- Xue, J.; Zartarian, V.; Moya, J.; Freeman, N.; Beamer, P.; Black, K.; Tulve, N.; Shalat, S. A Meta-Analysis of Children’s Hand-to-Mouth Frequency Data for Estimating Nondietary Ingestion Exposure. Risk Anal. 2007, 27, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Sexton, K. Cumulative Risk Assessment: An Overview of Methodological Approaches for Evaluating Combined Health Effects from Exposure to Multiple Environmental Stressors. Int. J. Environ. Res. Public Health 2012, 9, 370–390. [Google Scholar] [CrossRef] [PubMed]
- AuYeung, W.; Canales, R.A.; Beamer, P.; Ferguson, A.C.; Leckie, J.O. Young children’s mouthing behavior: An observational study via videotaping in a primarily outdoor residential setting. J. Child Health 2004, 2, 271–295. [Google Scholar] [CrossRef]
- Cohen Hubel, E.A.; Sheldon, L.S.; Burke, J.M.; McCurdy, T.R.; Berry, M.R.; Rigas, M.L.; Zartarian, V.G.; Freeman, N.C.G. Children’s Exposure Assessment: A Review of Factors Influencing Children’s Exposure, and the Data Available to Characterize and Assess that Exposure. Environ. Health Perspect. 2000, 108, 475–486. [Google Scholar] [CrossRef]
- Burrows, T.L.; Truby, H.; Morgan, P.J.; Callister, R.; Davies, P.S.W.; Collins, C.E. A comparison and validation of child versus parent reporting of children’s energy intake using food frequency questionnaires versus food records: Who’s an accurate reporter? Clin. Nutr. 2013, 32, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.H.; Lingas, E.O.; Rahman, M. Contamination of drinking-water by arsenic in Bangladesh: A public health emergency. Bull. World Health Organ. 2000, 78, 1093–1103. [Google Scholar] [PubMed]
- Ferreccio, C.; Sancha, A.M. Arsenic exposure and its impact on health in Chile. J. Health Popul. Nutr. 2006, 24, 164–175. [Google Scholar] [PubMed]
- Recio-Vega, R.; Gonzalez-Cortes, T.; Olivas-Calderon, E.; Lantz, R.C.; Gandolfi, A.J.; Alba, C.G. In utero and early childhood exposure to arsenic decreases lung function in children. J. Appl. Toxicol. 2015, 35, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.H. An overview on peripheral vascular disease in blackfoot disease-hyperendemic villages in Taiwan. Angiology 2002, 53, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Gilbert-Diamond, D.; Li, Z.; Perry, A.E.; Spencer, S.K.; Gandolfi, A.J.; Karagas, M.R. A population-based case—Control study of urinary arsenic species and squamous cell carcinoma in New Hampshire, USA. Environ. Health Perspect. 2013, 121, 1154–1160. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority. EFSA Panel on Contaminants in the Food Chain (CONTAM): Scientific Opinion on Arsenic in Food. EFSA J. 2009, 7, 60–71. [Google Scholar]
- Karagas, M.R.; Tosteson, T.D.; Morris, J.S.; Demidenko, E.; Mott, L.A.; Heaney, J.; Schned, A. Incidence of transitional cell carcinoma of the bladder and arsenic exposure in New Hampshire. Cancer Cause Control 2004, 15, 465–472. [Google Scholar] [CrossRef] [PubMed]


| 1st Results Packet-Individual Report | 2nd Results Packet-Summary of Results |
|---|---|
|
|
| Exposure Pathway | Intervention |
|---|---|
| Ingestion, Potable Water n = 11 |
|
| Ingestion, Incidental Soil n = 8 |
|
| Inhalation, outdoor dust n = 3 |
|
| Inhalation, indoor dust n = 5 |
|
| Ingestion, Food n = 3 |
|
| Variable | Not Included in PERE | Included in PERE | p | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Adult Annual Income | 0.99 | ||||
| $0–19,000 | 14 | 48 | 12 | 44 | |
| $20–39,000 | 5 | 17 | 6 | 22 | |
| $40–59,000 | 3 | 10 | 3 | 11 | |
| $60–79,000 | 4 | 14 | 3 | 11 | |
| >$80,000 | 3 | 10.3 | 3 | 11 | |
| Educational Attainment | 0.51 | ||||
| Less than High School | 4 | 11 | 3 | 11 | |
| High School/GED | 10 | 29 | 6 | 21 | |
| Some College or Vocational School | 12 | 34 | 11 | 39 | |
| College | 3 | 9 | 3 | 21 | |
| Graduate Degree | 6 | 17 | 2 | 7 | |
| Race/Ethnicity | 0.88 | ||||
| Asian | 1 | 3 | 0 | 0 | |
| Hispanic | 2 | 6 | 1 | 4 | |
| White | 32 | 91 | 26 | 93 | |
| Households Below Poverty Level | 8 | 50 | 5 | 36 | 0.48 |
| Variable | Arsenic Micrograms Per Liter (μg/L) 1 | Not Included in PERE | Included in PERE | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| >MESH 50th percentile | 10.4 | 20 | 52.6 | 16 | 50 | 1.00 |
| >MESH 95th percentile | 29.4 | 4 | 10.5 | 2 | 6.3 | 0.68 |
| >NHANES 50th percentile | 5.36 | 32 | 84.2 | 27 | 84.4 | 1.00 |
| >NHANES 95th percentile | 13.4 | 14 | 36.8 | 10 | 31.3 | 0.80 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramirez-Andreotta, M.D.; Brody, J.G.; Lothrop, N.; Loh, M.; Beamer, P.I.; Brown, P. Improving Environmental Health Literacy and Justice through Environmental Exposure Results Communication. Int. J. Environ. Res. Public Health 2016, 13, 690. https://doi.org/10.3390/ijerph13070690
Ramirez-Andreotta MD, Brody JG, Lothrop N, Loh M, Beamer PI, Brown P. Improving Environmental Health Literacy and Justice through Environmental Exposure Results Communication. International Journal of Environmental Research and Public Health. 2016; 13(7):690. https://doi.org/10.3390/ijerph13070690
Chicago/Turabian StyleRamirez-Andreotta, Monica D., Julia Green Brody, Nathan Lothrop, Miranda Loh, Paloma I. Beamer, and Phil Brown. 2016. "Improving Environmental Health Literacy and Justice through Environmental Exposure Results Communication" International Journal of Environmental Research and Public Health 13, no. 7: 690. https://doi.org/10.3390/ijerph13070690






