Class and Health Inequality in Later Life: Patterns, Mechanisms and Implications for Policy
Abstract
:1. Introduction
“Among the many trends that compete for the attention of policy makers these days, none is more likely to shape economic, social, and political developments in the early twenty first century than the simultaneous aging of Japan, Europe, and the United States ... The human life cycle is undergoing unprecedented change. To preserve economic security, we must adapt the social institutions built around it to these new realities”.
2. Materials and Methods
2.1. Data
2.2. Measures of Health and Wellbeing
2.3. Measures of Socioeconomic Inequalities
2.4. Statistical Methods
2.5. Ethics
3. Results
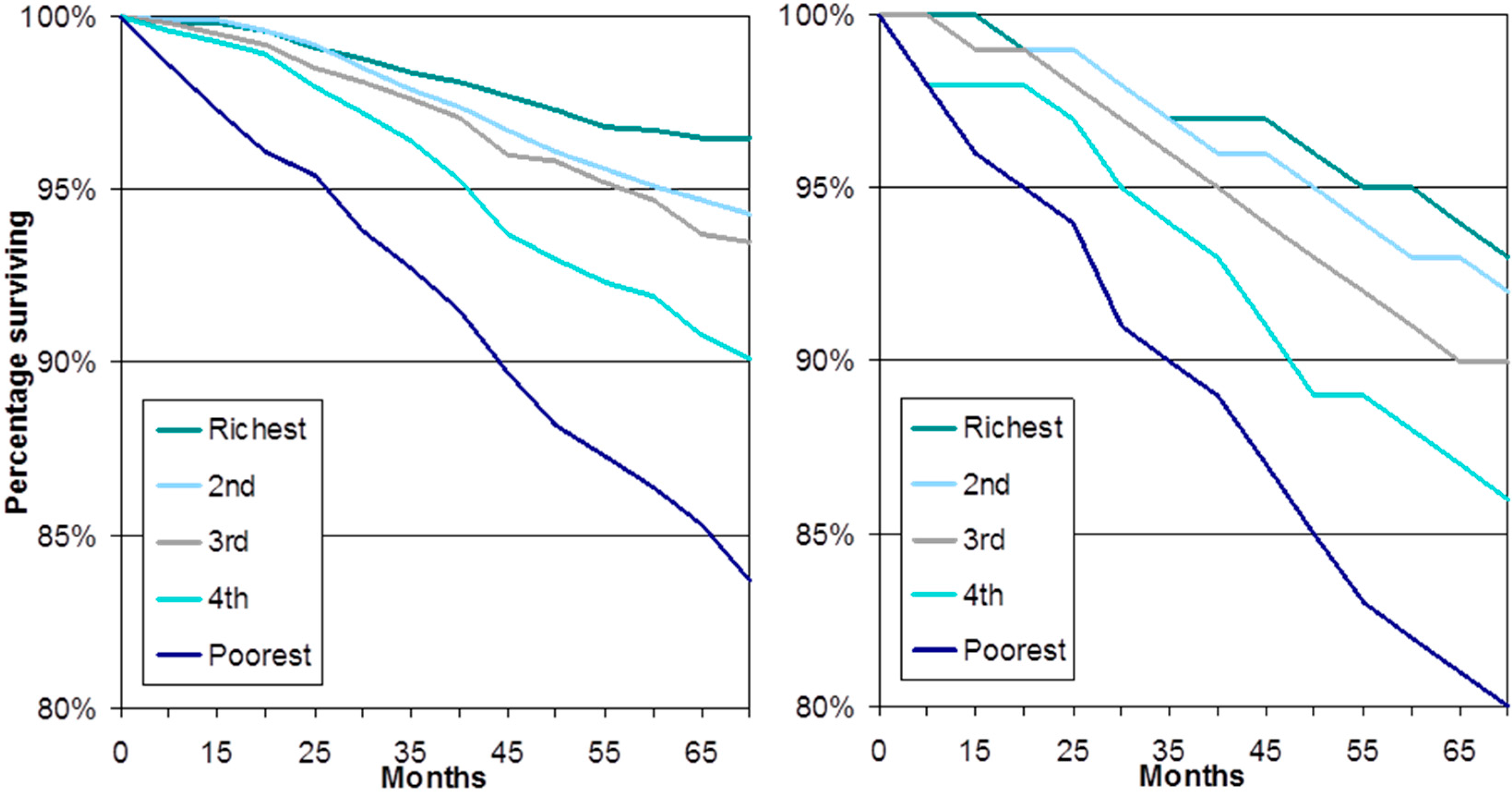
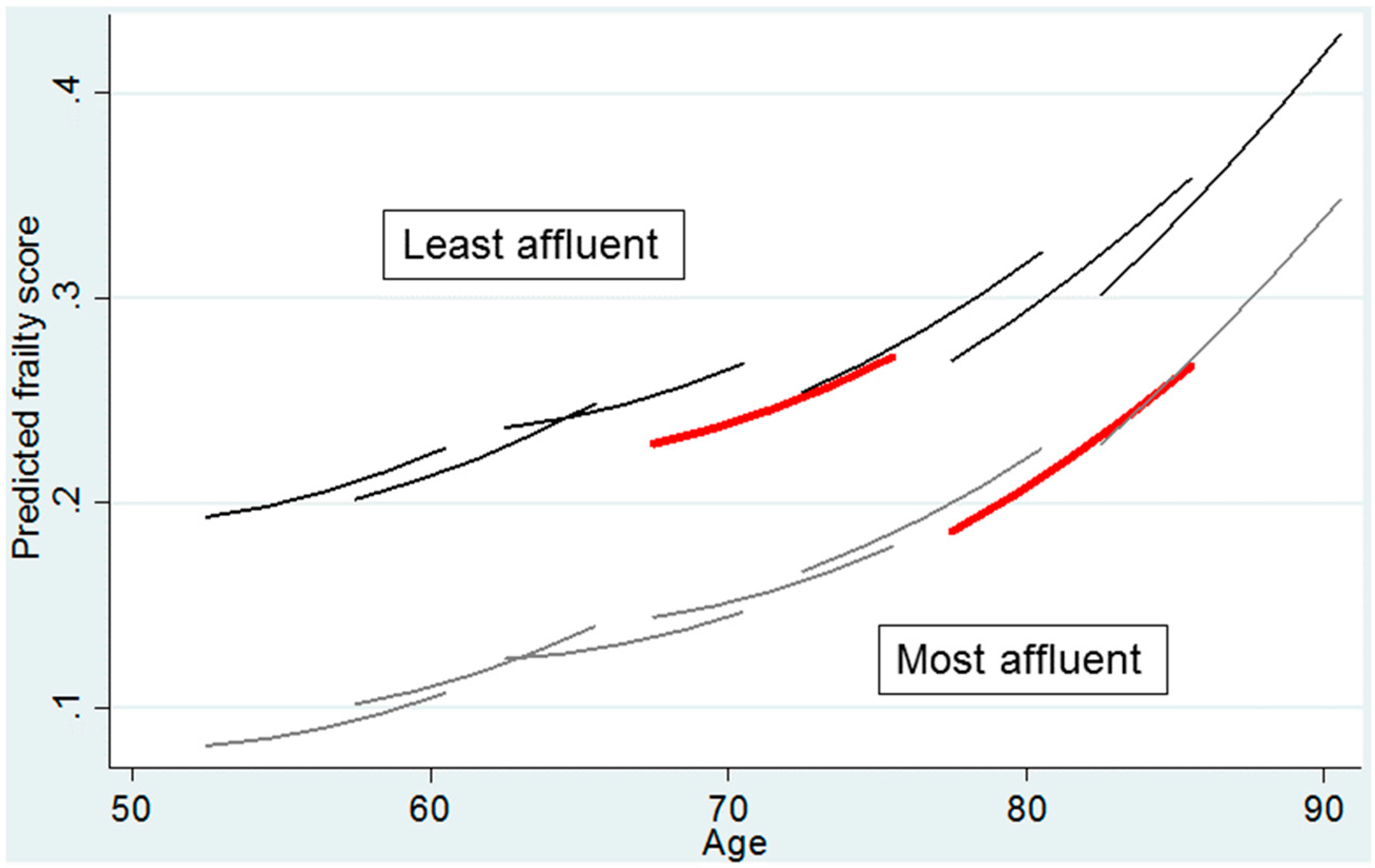
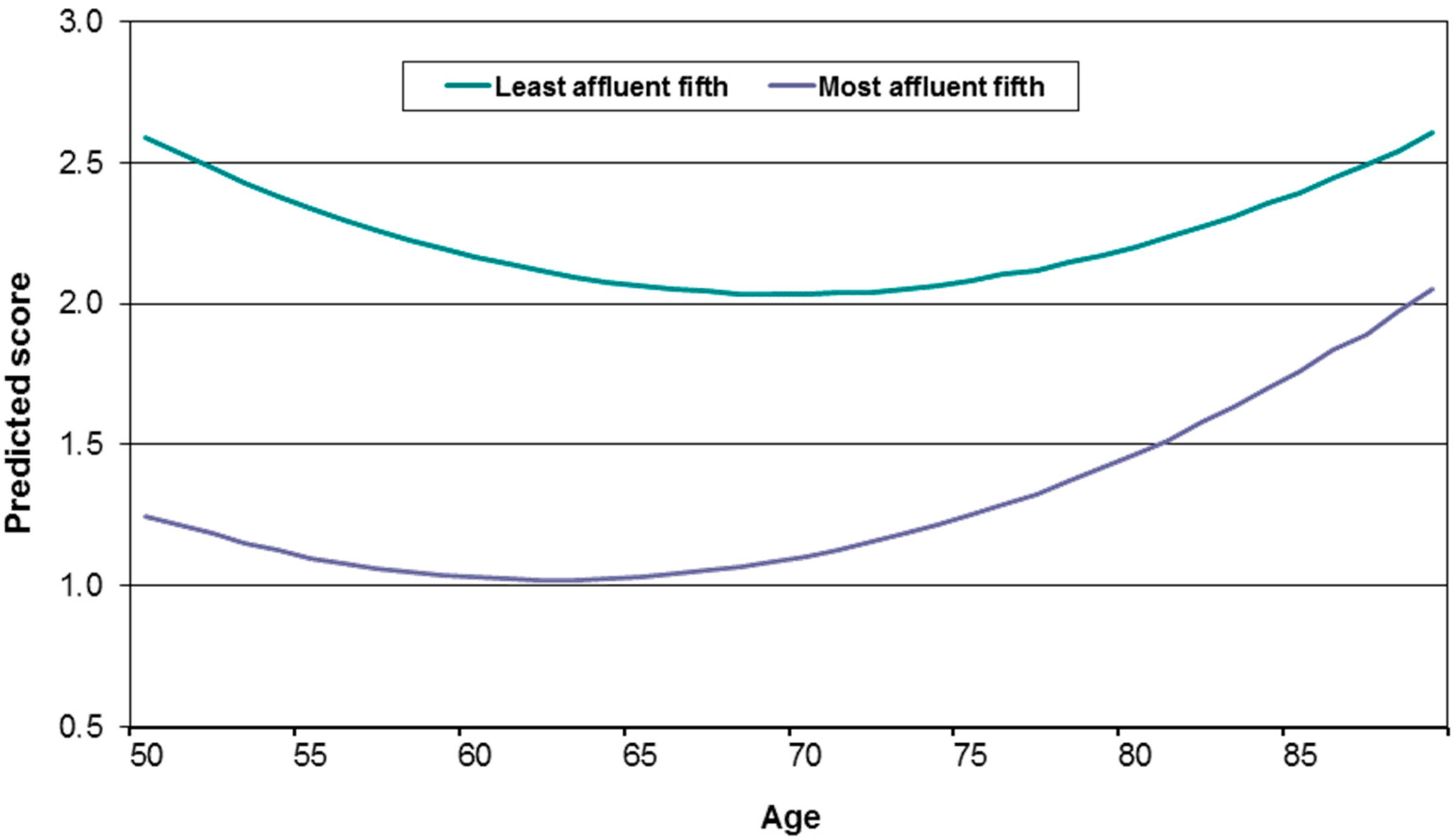
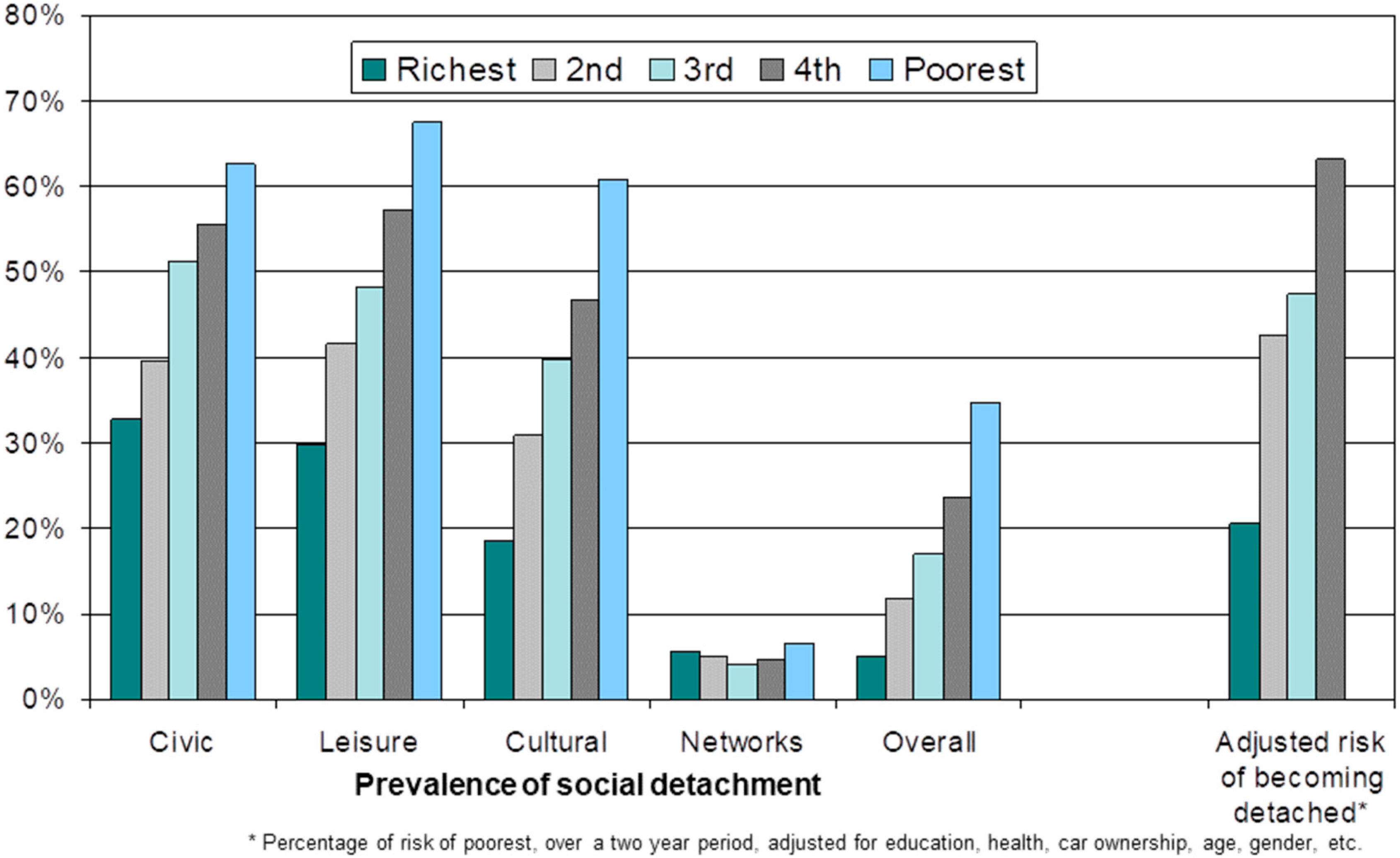
3.1. The Extent of Socioeconomic Inequalities in Health in Later Life
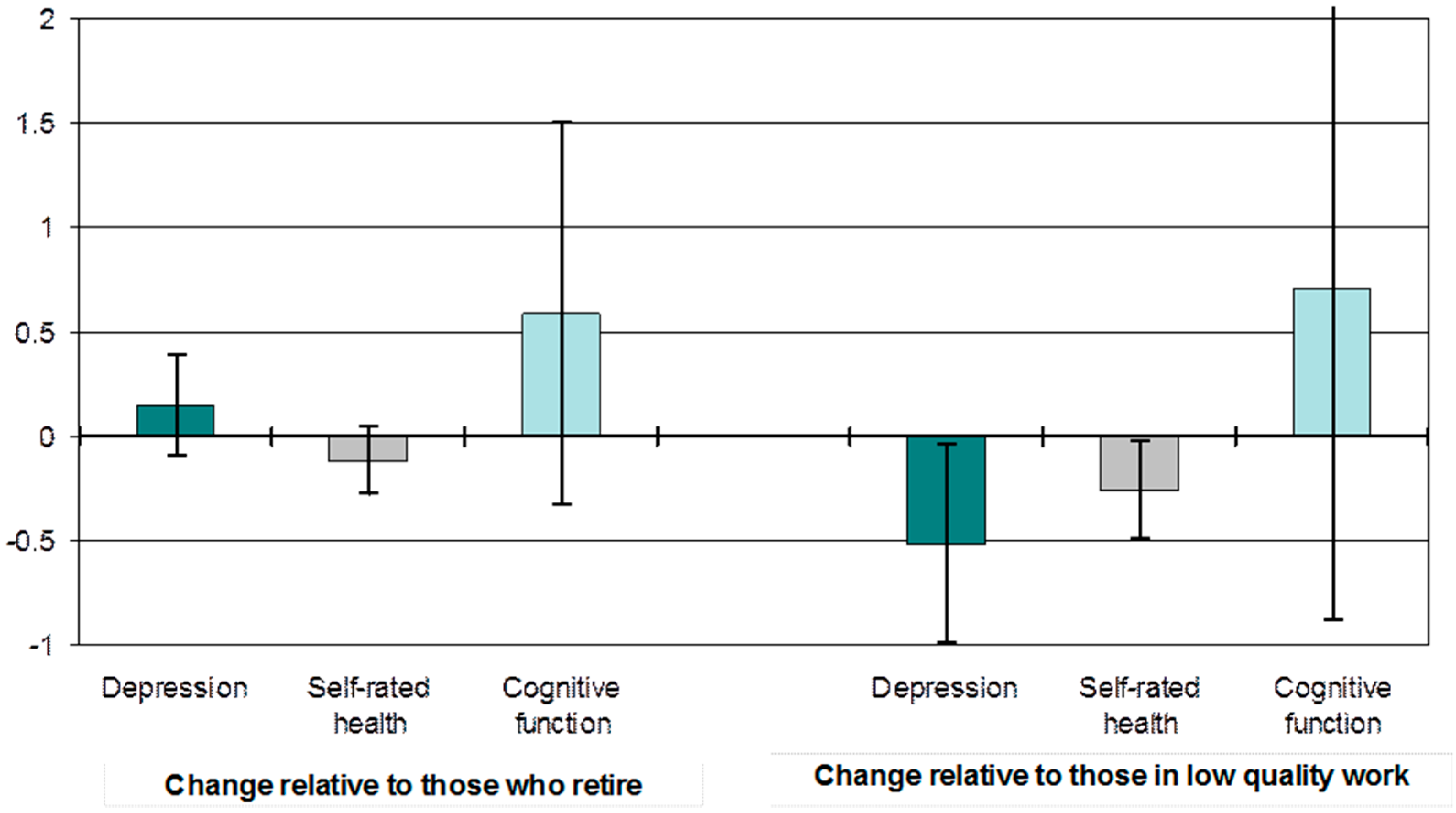
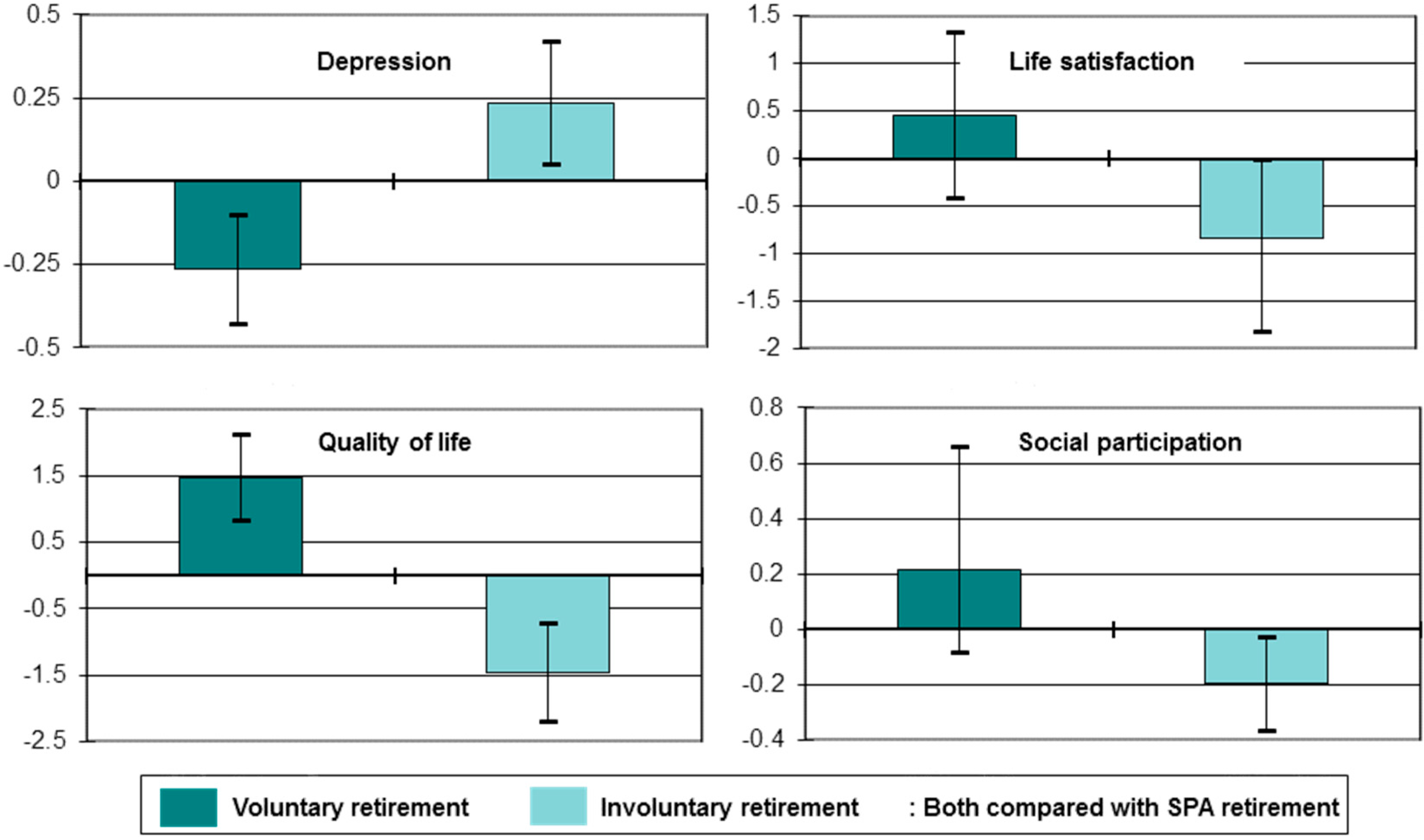
3.2. The Impact of Inequalities in Later Life Transitions on Health and Wellbeing
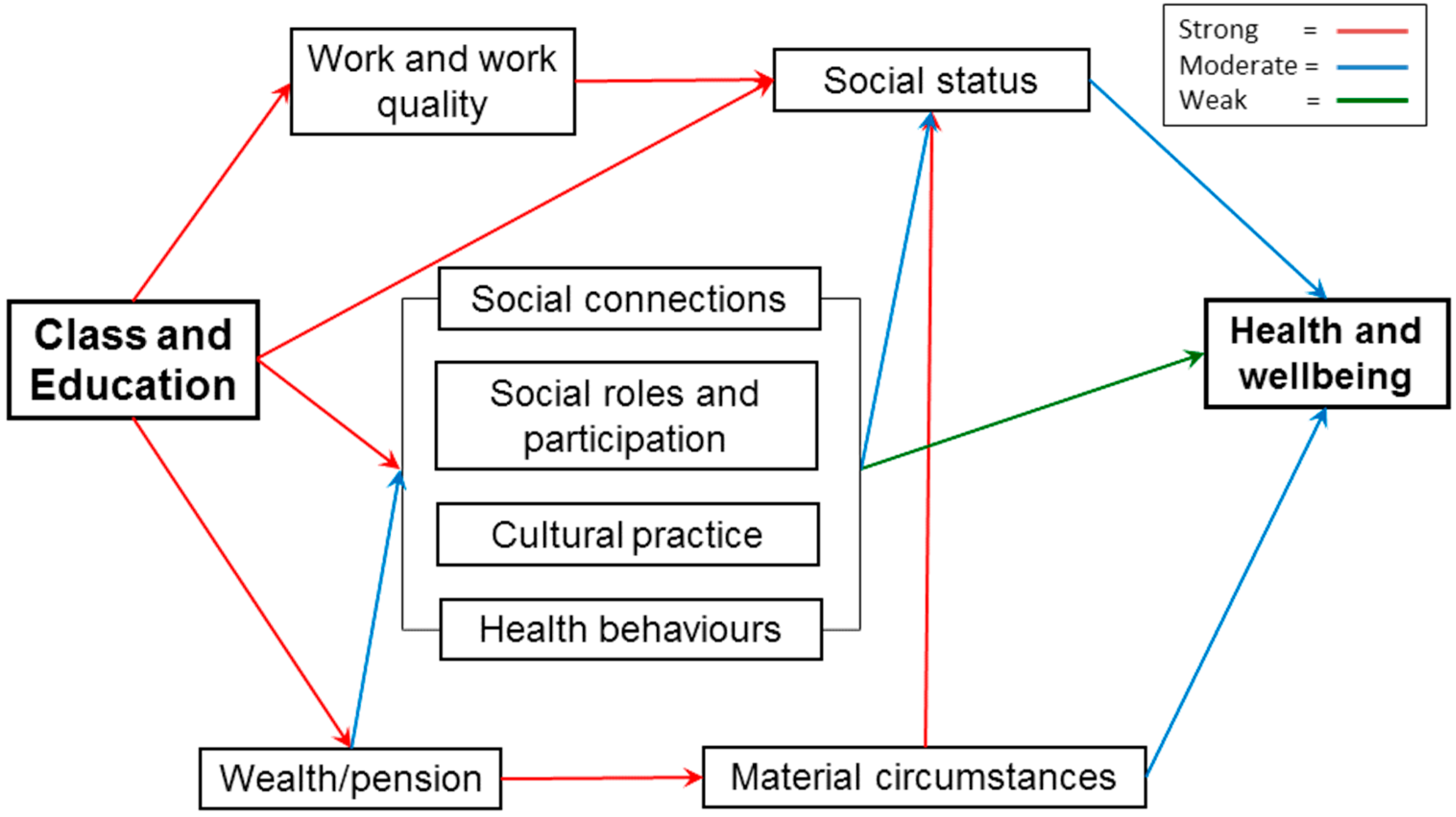
3.3. The Significance of Class in Later Life
4. Discussion
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- United Nations. Vienna International Plan of Action on Aging; United Nations: New York, NY, USA, 1983. [Google Scholar]
- Commission on Global Aging. Global Aging: The Challenge of the New Millennium; Centre for Strategic and International Studies and Watson Wyatt Worldwide: Washington, DC, USA, 1999. Available online: http://www.caregiverslibrary.org/portals/0/CGM.Global%20Aging%20WATSON%20WYATT.pdf (accessed on 11 October 2017).
- Banks, J. Employment and labour market transitions at older ages in England, 2002–2003 to 2014–2015. In The Dynamics of Ageing: Evidence from the English Longitudinal Study of Ageing 2002-2015; Banks, J., Batty, D., Nazroo, J., Steptoe, A., Eds.; The Institute for Fiscal Studies: London, UK, 2006. [Google Scholar]
- Bound, J.; Waidmann, T. Estimating the health effects of retirement. Mich. Retired Res. Center Work Pap. 2007. [Google Scholar] [CrossRef]
- Drentea, P. Retirement and mental health. J. Aging Health 2002, 14, 167–194. [Google Scholar] [CrossRef] [PubMed]
- Coyle, J.T. Use it or lose it-do effortful mental activities protect against dementia? N. Engl. J. Med. 2003, 348, 2489–2490. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y. Productive activities and psychological well-being among older adults. J. Gerontol. Ser. B: Psychol. Sci. Soc. Sci. 2008, 63, S64–S72. [Google Scholar] [CrossRef]
- Marmot Review. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post 2010; University College London: London, UK, 2011. [Google Scholar]
- Steptoe, A.; Breeze, E.; Banks, J.; Nazroo, J. Cohort profile: The English Longitudinal Study of Ageing (ELSA). Int. J. Epidemiol. 2013, 42, 1640–1648. [Google Scholar] [CrossRef] [PubMed]
- Rockwood, K.; Mitnitski, A. Frailty in relation to the accumulation of deficits. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62A, 722–727. [Google Scholar] [CrossRef]
- Marshall, A.; Nazroo, J.; Tampubolon, G.; Vanhoutte, B. Cohort differences in the levels and trajectories of frailty among older people in England. J. Epidemiol. Community Health 2015, 69, 316–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radloff, L.S. The CES-D Scale. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Matthews, K.; Nazroo, J. Later-Life Work, Health and Well-Being: Enduring Inequalities. In Paid Work beyond Pension Age; Scherger, S., Ed.; Palgrave McMillan: London, UK, 2015; pp. 259–277. [Google Scholar]
- Hyde, M.; Wiggins, R.D.; Higgs, P.; Blane, D.B. A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging Ment. Health 2003, 7, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Emmons, R.; Larsen, R.; Griffin, S. The Satisfaction with Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Crawford, R.; Tetlow, G. Employment, retirement and pensions. In Financial Circumstances, Health and Well-Being of the Older Population in England: The 2008 English Longitudinal Study of Ageing (Wave 4); Banks, J., Lessof, C., Nazroo, J., Rogers, N., Stafford, M., Steptoe, A., Eds.; The Institute for Fiscal Studies: London, UK, 2010; pp. 11–75. [Google Scholar]
- Rose, D.; Pevalin, D. The National Statistics Socio-economic Classification: Origins, Development and Use; Palgrave Macmillan: Basingstoke, UK, 2005. [Google Scholar]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.F. Relationship of subjective and objective social status with psychological and physicological functioning: Preliminary data in healthy white women. Health Psychol. 2000, 19, 586–592. [Google Scholar] [CrossRef] [PubMed]
- Jivraj, S.; Nazroo, J.; Barnes, M. Change in social detachment in older age in England. In The Dynamics of Ageing: Evidence from the English Longitudinal Study of Ageing 2002–2010 (Wave 5); Banks, J., Nazroo, J., Steptoe, A., Eds.; Institute for Fiscal Studies: London, UK, 2012; pp. 49–97. [Google Scholar]
- Banks, J.; Breeze, E.; Lessof, C.; Nazroo, J. Retirement, Health and Relationships of the Older Population in England: The 2004 English Longitudinal Study of Ageing; The Institute for Fiscal Studies: London, UK, 2006. [Google Scholar]
- Marmot, M.; Banks, J.; Blundell, R.; Lessof, C.; Nazroo, J. Health, Wealth and Lifestyles of the Older Population in England: The 2002 English Longitudinal Study of Ageing; The Institute for Fiscal Studies: London, UK, 2003. [Google Scholar]
- Nazroo, J.; Zaninotto, P.; Gjonça, E. Mortality and healthy life expectancy. In Living in the 21st Century: Older People in England. The 2006 English Longitudinal Study of Ageing; Banks, J., Breeze, E., Lessof, C., Nazroo, J., Eds.; The Institute for Fiscal Studies: London, UK, 2008; pp. 253–280. [Google Scholar]
- McMunn, A.; Nazroo, J.; Breeze, E. Inequalities in health at older ages: A longitudinal investigation of onset of illness and survival effects in England. Age Ageing 2009, 38, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Vanhoutte, B.; Nazroo, J. Cognitive, affective and eudemonic well-being in later life: Measurement equivalence over gender and age. Sociol. Res. Online 2014, 19, 4. [Google Scholar] [CrossRef] [PubMed]
- Deci, E.L.; Ryan, R.M. Hedonia, eudaimonia, and well-being: An introduction. J. Happiness Stud. 2006, 9, 1–11. [Google Scholar] [CrossRef]
- Ryff, C.D.; Singer, B. The contours of positive human health. Psychol. Inq. 1998, 9, 1–28. [Google Scholar] [CrossRef]
- Diener, E.D. Assessing subjective well-being: Progress and opportunities. Soc. Indic. Res. 1994, 31, 103–157. [Google Scholar] [CrossRef]
- Baltes, P.M.; Baltes, M.M. Psychological perspectives on successful aging: The model of selective optimization with compensation. In Successful Aging; Baltes, P.M., Baltes, M.M., Eds.; Cambridge University Press: Cambridge, UK, 1990. [Google Scholar]
- Baird, B.M.; Lucas, R.E.; Donnellan, M.B. Life Satisfaction across the Lifespan: Findings from Two Nationally Representative Panel Studies. Soc. Indic. Res. 2010, 99, 183–203. [Google Scholar] [CrossRef] [PubMed]
- Jivraj, S.; Nazroo, J.; Vanhoutte, B.; Chandola, T. Aging and subjective well-being in later life. J. Gerontol. Ser. B: Psychol. Sci. Soc. Sci. 2014, 69, 930–941. [Google Scholar] [CrossRef] [PubMed]
- Adam, S.; Bonsang, E.; Germain, S.; Perelman, S. Retirement and Cognitive Reserve: A Stochastic Frontier Approach Applied to Survey Data, CREPP (Center of Research in Public Economics and Population Economics) Working Paper No. 2007/4; University of Liège: Liège, Belgium, 2007. [Google Scholar]
- Rohwedder, S.; Willis, R.J. Mental retirement. J. Econ. Perspect. 2010, 24, 119–138. [Google Scholar] [CrossRef] [PubMed]
- Behncke, S. Does retirement trigger ill health? Health Econ. 2012, 21, 282–300. [Google Scholar] [CrossRef] [PubMed]
- Bonsang, E.; Adam, S.; Perelman, S. Does retirement affect cognitive functioning? J. Health Econ. 2012, 31, 490–501. [Google Scholar] [CrossRef] [PubMed]
- Coe, N.B.; Zamtablearro, G. Retirement effects on health in Europe. J. Health Econ. 2011, 30, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Coe, N.B.; Lindeboom, M. Does Retirement Kill You? Evidence from Early Retirement Windows, CentER Discussion Paper Series No. 2008-93; Center for Economic Research, Tilburg University: Tilburg, The Netherlands, 2008. [Google Scholar]
- Siegrist, J.; Starke, D.; Chandola, T.; Godin, I.; Marmot, M.; Niedhammer, I.; Peter, R. The measurement of effort-reward imbalance at work: European comparisons. Soc. Sci. Med. 2004, 58, 1483–1499. [Google Scholar] [CrossRef]
- McMunn, A.; Nazroo, J.; Wahrendorf, M.; Breeze, E.; Zaninotto, P. Participation in socially productive activities, reciprocity and wellbeing in later life: Baseline results in England. Ageing Soc. 2009, 29, 765–782. [Google Scholar] [CrossRef]
- Chandola, T.; Ferrie, J.; Sacker, A.; Marmot, M. Social inequalities in self-reported health in early old age: Follow-up of prospective cohort study. BMJ 2007, 334, 990. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.R.; Rubin, D. The central role of the propensity score in observational studies for causal effects. Biometrika 1983, 70, 41–45. [Google Scholar] [CrossRef]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Marshall, A.; Nazroo, J. Trajectories in the Prevalence of Self-Reported Illness around Retirement. Popul. Ageing 2016, 9, 11–48. [Google Scholar] [CrossRef]
- Higgs, P.; Scambler, G. Explaining health inequalities: How useful are concepts of social class? In Modernity, Medicine and Health: Medical Sociology towards 2000; Scambler, G., Higgs, P., Eds.; Routledge: London, UK, 1998; pp. 82–99. [Google Scholar]
- Bolam, B.; Murphy, S.; Gleeson, K. Individualisation and inequalities in health: A qualitative study of class identity and health. Soc. Sci. Med. 2004, 59, 1355–1365. [Google Scholar] [CrossRef] [PubMed]
- Roelfs, D.J.; Shor, E.; Davidson, K.W.; Schwartz, J.E. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011, 72, 840–854. [Google Scholar] [CrossRef] [PubMed]
- Borrell, C.; Muntaner, C.; Gil-Gonzalez, D.; Artazioz, L.; Rodriguez-Sanz, M.; Rohlfs, I.; Perez, K.; Garcia-Calvente, M.; Villegas, R.; Alvarez-Dardet, C. Perceived discrimination and health by gender, social class and country of birth in a Southern European country. Prev. Med. 2010, 50, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, A.; Bentley, R.J.; Turrell, G.; Shaw, J.; Dunstan, D.; Subramanian, S.V. Socioeconomic position, gender, health behaviours and biomarkers of cardiovascular disease and diabetes. Soc. Sci. Med. 2010, 71, 1150–1160. [Google Scholar] [CrossRef] [PubMed]
- Lahelma, E.; Lallukka, T.; Laaksonen, M.; Martikainen, P.; Rahkonen, O.; Chandola, T.; Head, J.; Marmot, M.; Kagamimori, S.; Tatsuse, T.; et al. Social class differences in health behaviours among employees from Britain, Finland and Japan: The influence of psychosocial factors. Health Place 2010, 16, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Malmusi, D.; Borrell, C.; Benach, J. Migration-related health inequalities: Showing the complex interactions between gender, social class and place of origin. Soc. Sci. Med. 2010, 71, 1610–1619. [Google Scholar] [CrossRef] [PubMed]
- Vanroelen, C.; Levecque, K.; Moors, G.; Louckx, F. Linking credentialed skills, social class, working conditions and self-reported health: A focus on health inequality-generating mechanisms. Sociol. Health Illn. 2010, 32, 948–964. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, J. Socioeconomic status and depression across Japan, Korea and China: Exploring the impact of labour market structures. Soc. Sci. Med. 2011, 73, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, S. Triple jeopardy? Mental health at the intersection of gender, race and class. Soc. Sci. Med. 2012, 74, 1791–1801. [Google Scholar] [CrossRef] [PubMed]
- Demakakos, P.; Nazroo, J.; Breeze, E.; Marmot, M. Socioeconomic status and health: The role of subjective social status. Soc. Sci. Med. 2008, 67, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Huijts, T.; Eikemo, T.A.; Skalicka, V. Income-related health inequalities in the Nordic countries: Examining the role of education, occupational class and age. Soc. Sci. Med. 2010, 71, 1964–1972. [Google Scholar] [CrossRef] [PubMed]
- Prus, S.G. Comparing social determinants of self-rated health across the United States and Canada. Soc. Sci. Med. 2011, 73, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, Z.; Prachuabmoh, V. Comparing the socioeconomic status-health gradient among adults 50 and older across rural and urban areas of Thailand in 1994 and 2007. Soc. Sci. Med. 2012, 71, 1964–1972. [Google Scholar] [CrossRef] [PubMed]
- Bourdieu, P. Distinction: A Social Critique of the Judgement of Taste; Routledge: Abingdon, UK, 1979. [Google Scholar]
- Bourdieu, P. The Forms of Capital. In Handbook of Theory of Research for the Sociology of Education; Richardson, J.G., Ed.; Greenwood: New York, NY, USA, 1986. [Google Scholar]
- Putnam, R.D. Making Democracy Work: Civic Traditions in Modern Italy; Princeton University Press: Princeton, NJ, USA, 1993. [Google Scholar]
- Carpiano, R.M. Toward a neighbourhood resource-based theory of social capital for health: Can Bourdieu and sociology help? Soc. Sci. Med. 2006, 62, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, A.; Macintyre, S. Is social participation associated with cardiovascular disease risk factors? Soc. Sci. Med. 2007, 64, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Murayama, H.; Fujiwara, Y.; Kawachi, I. Social capital and health: A review of prospective multilevel studies. J. Epidemiol. 2012, 22, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyqvist, F.F.; Forsman, A.K.; Giuntoli, G.; Cattan, M. Social capital as a resource for mental well-being in older people: A systematic review. Aging Ment. Health 2013, 17, 394–410. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, J.F.; Putnam, R. The social context of wellbeing. Proc. R. Soc. B Biol. Sci. 2004, 359, 1435–1446. [Google Scholar]
- Schultz, J.; OBrien, A.M.; Tadesse, B. Social capital and self-rated health: Results from the US 2006 Social Capital Survey of One Community. Soc. Sci. Med. 2008, 67, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Snelgrove, J.W.; Pikhart, H.; Stafford, M. A multilevel analysis of social capital and self-rated health: Evidence from the British Household Panel Survey. Soc. Sci. Med. 2009, 68, 1993–2001. [Google Scholar] [CrossRef] [PubMed]
- Giordano, G.N.; Lindstrom, M. The impact of changes in different aspects of social capital and material conditions on self-rated health over time: A longitudinal cohort study. Soc. Sci. Med. 2010, 70, 700–710. [Google Scholar] [CrossRef] [PubMed]
- Cockerham, W. Health lifestyle theory and the convergence of agency and structure. J. Health Soc. Behav. 2005, 46, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.G. Status Syndrome: How Your Social Standing Directly Affects Your Health and Life Expectancy; Bloomsbury: London, UK, 2004. [Google Scholar]
- Singh-Manoux, A.; Adler, N.A.; Marmot, M.G. Subjective social status: Its determinants and its associations with measures of ill-health in the Whitehall II Study. Soc. Sci. Med. 2003, 56, 1321–1333. [Google Scholar] [CrossRef]
- Shankar, A.; McMunn, A.; Steptoe, A. Health-related behaviors in older adults: Relationships with socioeconomic status. Am. J. Prev. Med. 2010, 38, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Netuveli, G.; Bartley, M. Perception is reality: Effect of subjective versus objective socio-economic position on quality of life. Sociology 2012, 46, 1208–1215. [Google Scholar] [CrossRef]
- McGovern, P.; Nazroo, J. Patterns and Causes of Health Inequalities in Later Life: A Bourdieusian Approach. Sociol. Health Illn. 2015, 37, 143–160. [Google Scholar] [CrossRef] [PubMed]
- Agahi, N.; Parker, M.G. Leisure activities and mortality: Does gender matter? J. Aging Health 2008, 20, 855–871. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P. Trajectories of social engagement and limitations in late life. J. Health Soc. Behav. 2011, 52, 430–443. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, M.; Kim, J. Social Activities and Health of Korean Elderly Women by Age Groups. Educ. Gerontol. 2013, 39, 640–654. [Google Scholar] [CrossRef]
- Kouvonen, A.; Swift, J.A.; Stafford, M.; Cox, T.; Vahtera, J.; Väänänen, A.; Heponiemi, T.; De Vogli, R.; Griffiths, A.; Kivimäki, M. Social participation and maintaining recommended waist circumference: Prospective evidence from the English Longitudinal Study of Ageing. J. Aging Health 2012, 24, 250–268. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.X.; Xu, W.; Pei, J.J. Leisure activities, cognition and dementia. Biochim. Biophys. Acta 2012, 1822, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Cornwell, E.Y.; Waite, L.J. Measuring Social Isolation among Older Adults Using Multiple Indicators from the NSHAP Study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64B (Suppl. 1), i38–i46. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, R.; Yadollah, A.M.; Tengku, A.H. Social isolation in older Malaysians: Prevalence and risk factors. Psychogeriatrics 2013, 13, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Strain, L.; Grabusic, C.C.; Searle, M.S.; Dunn, N.J. Continuing and ceasing leisure activities in later life: A longitudinal study. Gerontologist 2002, 42, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Villar, F. Successful ageing and development: The contribution of generativity in older age. Ageing Soc. 2011, 32, 1087–1105. [Google Scholar] [CrossRef]
- Stowe, J.D.; Cooney, T.M. Examining Rowe and Kahn’s Concept of Successful Aging: Importance of Taking a Life Course Perspective. Gerontologist 2015, 55, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Youssim, I.; Hank, K.; Litwin, H. The Role of Family Social Background and Inheritance in Later Life Volunteering: Evidence from SHARE-Israel. Res. Aging 2014, 37, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.B. Volunteering in retirement: Perceptions of midlife workers. Nonprofit Volunt. Sect. Q. 2004, 33, 55–73. [Google Scholar] [CrossRef]
- Van Willigen, M. Differential benefits of volunteering across the life course. J. Gerontol. Ser. B: Psychol. Sci. Soc. Sci. 2000, 55, S308–S318. [Google Scholar] [CrossRef]
- Morrow-Howell, N.; Hinterlong, J.; Rozario, P.A.; Tang, F. Effects of volunteering on the well-being of older adults. J. Gerontol. Ser. B: Psychol. Sci. Soc. Sci. 2003, 58, S137–S145. [Google Scholar] [CrossRef]
- Nazroo, J.; Matthews, K. The Impact of Volunteering on Well-Being in Later Life; WRVS: Cardiff, UK, 2012. [Google Scholar]
- Moen, P. A life course perspective on retirement, gender, and well-being. J. Occup. Health Psychol. 1996, 1, 131–144. [Google Scholar] [CrossRef] [PubMed]
- Arber, S.; Cooper, H. Gender and inequalities in health across the lifecourse. In Gender Inequalities in Health; Annandale, E., Hunt, K., Eds.; Open University Press: Buckingham, UK, 2000. [Google Scholar]
- Arber, S.; Andersson, L.; Hoff, A. Changing approaches to Gender and Ageing. Curr. Sociol. 2007, 55, 147–153. [Google Scholar] [CrossRef]
- Anderson, N.; Bulatao, R.; Cohen, B. (Eds.) Critical Perspectives on Racial and Ethnic Differentials in Health in Late Life; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Bajekal, M.; Blane, D.; Grewal, I.; Karlsen, S.; Nazroo, J. Ethnic differences in influences on quality of life at older ages: A quantitative analysis. Ageing Soc. 2004, 24, 709–728. [Google Scholar] [CrossRef]
- Bowling, A.; Stafford, M. How do objective and subjective assessments of neighbourhood influence social and physical functioning in older age? Findings from a British survey of ageing. Soc. Sci. Med. 2007, 64, 2533–2549. [Google Scholar] [CrossRef] [PubMed]
- Marshall, A.; Jivraj, J.; Nazroo, J.; Tampubolon, G.; Vanhoutte, B. Does the level of wealth inequality within an area influence the prevalence of depression amongst older people? Health Place 2014, 27, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Westwood, S. (Ed.) Ageing, Gender and Sexuality: Equality in Later Life; Routledge: Abingdon, UK, 2016; ISBN 978-1-138-91240-3. [Google Scholar]
- Marshall, A.; Nazroo, J.; Feeney, K.; Lee, J.; Vanhoutte, B.; Pendleton, N. Comparison of hypertension healthcare outcomes among older people in the USA and England. J. Epidemiol. Community Health 2016, 70, 264–270. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nazroo, J. Class and Health Inequality in Later Life: Patterns, Mechanisms and Implications for Policy. Int. J. Environ. Res. Public Health 2017, 14, 1533. https://doi.org/10.3390/ijerph14121533
Nazroo J. Class and Health Inequality in Later Life: Patterns, Mechanisms and Implications for Policy. International Journal of Environmental Research and Public Health. 2017; 14(12):1533. https://doi.org/10.3390/ijerph14121533
Chicago/Turabian StyleNazroo, James. 2017. "Class and Health Inequality in Later Life: Patterns, Mechanisms and Implications for Policy" International Journal of Environmental Research and Public Health 14, no. 12: 1533. https://doi.org/10.3390/ijerph14121533



