An Increase in Consuming Adequately Iodized Salt May Not Be Enough to Rectify Iodine Deficiency in Pregnancy in an Iodine-Sufficient Area of China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sampling Design and Sample Collection
2.2. Determination of Iodine Concentration and Iodine Status Assessment Criteria
2.3. Statistical Analysis
2.4. Ethical Stament
3. Results
3.1. Characteristics of the Total Study Population of Pregnant Women
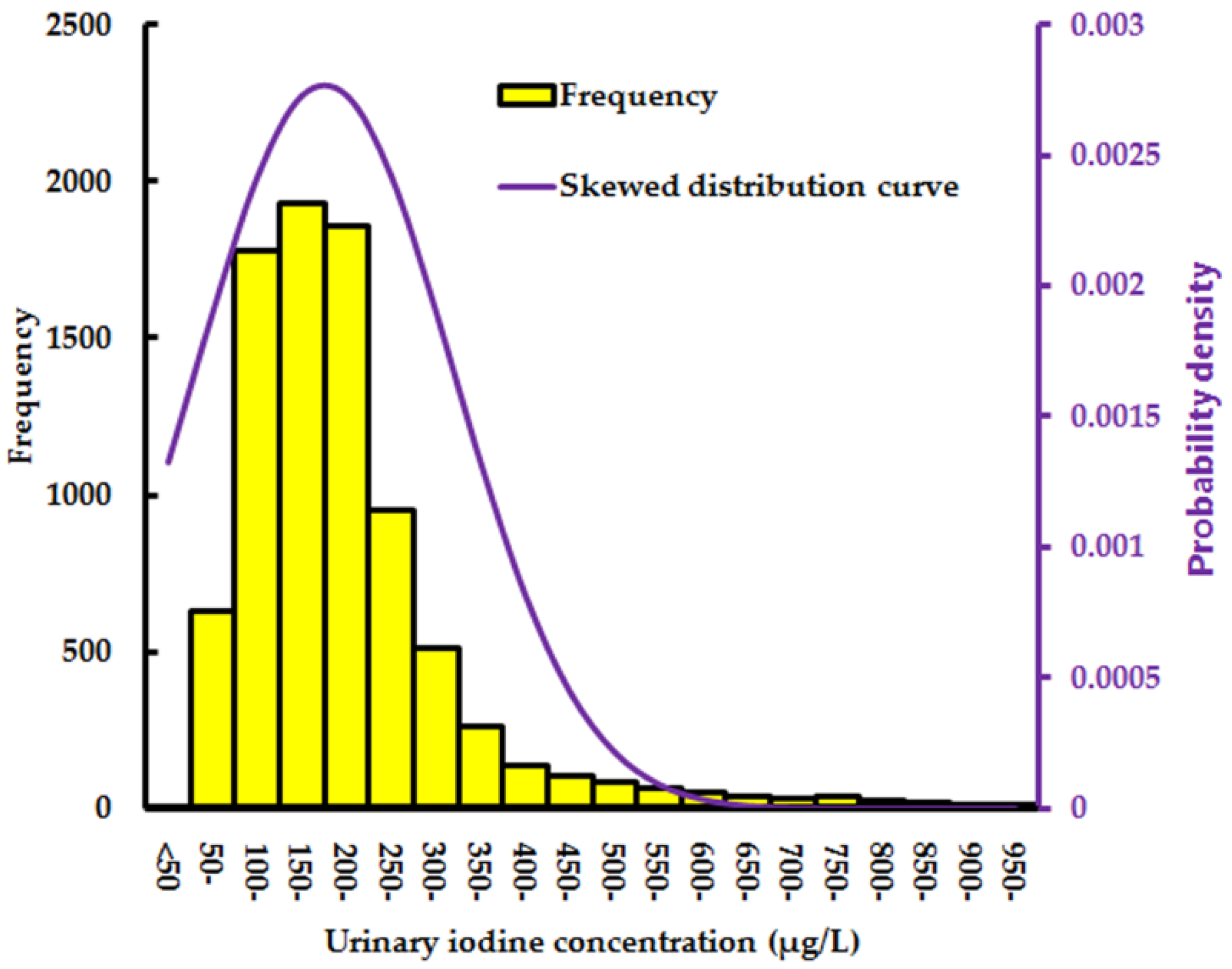
3.2. Median UIC in Pregnant Women
3.3. Distribution of Salt Containing Different Iodine Content
3.4. Distribution of UIC in Pregnant Women Consuming Salt Containing Different Iodine Content
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| USI | universal salt iodization |
| IDD | iodine deficiency disorder |
| UIC | urinary iodine concentration |
| WHO | World Health Organization |
| UNICEF | United Nations Children’s Fund |
| ICCIDD | International Council for the Control of Iodine Deficiency Disorders |
| SPSS | Statistical Package for the Social Sciences |
References
- Zimmermann, M.B. Iodine deficiency. Endocr. Rev. 2009, 30, 376–408. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.Y.; Jiang, X.M.; Dou, Z.H.; Murdon, A.R.; Zhang, M.L.; Karen, D.; Ma, T.; Kareem, A.; Nancy, D.; Robert, D. Timing of vulnerability of the brain to iodine deficiency in endemic cretinism. N. Engl. J. Med. 1994, 331, 1739–1744. [Google Scholar]
- Sun, D.J.; Wei, H.L.; Shen, H.M.; Wang, Z.B.; Wang, Z.W.; Liu, S.J.; Sun, Y.F.; Chen, Z. Achievements on controlling and preventing endemic diseases in China during the recent 50 years. Chin. J. Endemiol. 2003, 22, 20–23. [Google Scholar]
- Yu, J.; Liu, S.J.; Su, X.H.; Zhang, S.B. Results of water iodine in the 2002 national iodine deficiency disorders surveillance. Chin. J. Endemiol. 2004, 23, 223–224. [Google Scholar]
- Yu, Z.H.; Liu, S.J. The achievements of prevention of iodine deficiency during 50 years in China. Chin. J. Prev. Med. 2003, 9, 315–318. [Google Scholar]
- Meng, F.G.; Zhao, R.C.; Liu, P.; Liu, L.X.; Liu, S.J. Assessment of iodine status in children, adults, pregnant women and lactating women in iodine-replete areas of China. PLoS ONE 2013, 8, e81294. [Google Scholar] [CrossRef] [PubMed]
- National Iodine Deficiency Disorders Surveillance Group. An analysis and report of China national deficiency disorders surveillance data in 1999. Chin. J. Endemiol. 2000, 19, 269–271. [Google Scholar]
- Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination. A Guide for Programme Managers. Available online: http://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/9789241595827/en/ (accessed on 5 January 2017).
- Chinese National Standards on Edible Salt (GB 5461-2000). Available online: http://www.360doc.com/content/12/0720/17/10327450_225478130.shtml (accessed on 8 February 2017).
- Iodine Content in Edible Salt (GB26878-2011). Available online: http://www.cnsalt.cn/d.asp?id=7642 (accessed on 8 February 2017).
- Su, X.H.; Liu, S.J.; Shen, H.M.; Zhang, S.B.; Wei, H.L.; Yu, J.; Ye, Y.X.; Li, Y.; Liu, Y.; Zhang, Z.Y.; et al. National iodine deficiency disorder surveillance: A sum up of data in 2005 and an analysis. Chin. J. Endemiol. 2007, 26, 67–69. [Google Scholar]
- Liu, P.; Su, X.H.; Shen, H.M.; Meng, F.G.; Fan, L.J.; Liu, S.J.; Sun, D.J. National iodine deficiency disorders: An analysis of surveillance data in 2011. Chin. J. Endemiol. 2015, 34, 181–185. [Google Scholar]
- Sun, D.J.; Xiao, D.L.; Liu, S.J. The Chinese National Iodine Deficiency Diseases Surveillance in 2011, 1st ed.; People’s Health Publication House: Beijing, China, 2014; pp. 5–10. [Google Scholar]
- Mao, G.M.; Ding, G.Q.; Lou, X.M.; Zhang, R.H.; Zheng, P.; Mo, Z.; Wang, X.; Zhu, W.; Zhou, J.; Gu, F. Survey of iodine nutritional status in 2011, Zhejiang, China. Asia Pac. J. Clin. Nutr. 2015, 24, 234–244. [Google Scholar] [PubMed]
- Mo, Z.; Lou, X.M.; Zhu, W.M.; Wang, X.F.; Mao, G.M.; Zhou, J.S.; Ding, G.Q. A cross-sectional study on iodine nutrition in general population from Zhejiang province, China. Chin. J. Endemiol. 2013, 34, 464–470. [Google Scholar]
- National Health and Family Planning Commission of China. The Surveillance Guidelines of Assess IDD National Programs. Available online: http://www.nhfpc.gov.cn/jkj/s5873/201604/950811922fb944b5ab3b59e4ae21a3a3.shtml (accessed on 8 February 2017).
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in population: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Khair, S.A.; Crooks, J.; Turnbull, A.C.; Hytten, F.E. The physiological changes in thyroid function during pregnancy. Clin. Sci. 1964, 27, 195–207. [Google Scholar] [PubMed]
- Zou, Y.; Lou, X.M.; Ding, G.Q.; Mo, Z.; Mao, G.M. Iodine nutritional status after the implementation of the new iodized salt concentration standard in Zhejiang province, China. BMC Public Health 2014, 14, 836. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Ding, G.Q.; Lou, X.M.; Mo, Z.; Zhu, W.M.; Mao, G.M.; Zhou, J. A study on the influencing factors of urinary iodine concentration and the relationship between iodized salt concentration and urinary iodine concentration. Br. J. Nutr. 2015, 113, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Lou, X.M.; Ding, G.Q.; Mo, Z.; Zhu, W.M.; Mao, G.M. A cross-sectional comparison study on the iodine nutritional status between rural and urban residents in Zhejiang province, China. BMJ Open 2014, 4, e005484. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y.; Lou, X.M.; Ding, G.Q.; Mo, Z.; Zhu, W.M.; Mao, G.M.; Zhou, J. An assessment of iodine nutritional status and thyroid hormone levels in children aged 8–10 years living in Zhejiang province, China: A cross-sectional study. Eur. J. Pediatr. 2014, 173, 929–934. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.L.; Sorensen, L.K.; Krejbjerg, A.; Moller, M.; Laurberg, P. Iodine deficiency in Danish pregnant women. Dan. Med. J. 2013, 60, A4657. [Google Scholar] [PubMed]
- Granfors, M.; Andersson, M.; Stinca, S.; Åkerud, H.; Skalkidou, A.; Poromaa, I.S.; Wikström, A.K.; Nyström, H.F. Iodine deficiency in a study population of pregnant women in Sweden. Acta Obstet. Gynecol. Scand. 2015, 94, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Vandevjvere, S.; Amsalkhir, S.; Mourri, A.B.; Åkerud, H.; Skalkidou, A.; Poromaa, I.S.; Wikström, A.K.; Nyström, H.F. Iodine deficiency among Belgian pregnant women not fully corrected by iodine-containing multivitamins: A national cross-sectional survey. Br. J. Nutr. 2013, 109, 2276–2284. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.L.; Sorensen, L.K.; Krejbjerg, A.; Møller, M.; Klitbo, D.M.; Nøhr, S.B.; Pedersen, K.M.; Laurberg, P. Iodine status in Danish pregnant and breastfeeding women including studies of some challenges in urinary iodine status evaluation. J. Trace Elem. Med. Biol. 2015, 31, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N.; Andersson, M.; Zimmermann, M.B. Global iodine nutrition: Where do we stand in 2013. Thyroid 2013, 23, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Marchioni, E.; Fumarola, A.; Calvanese, A.; Piccirilli, F.; Tommasi, V.; Cugini, P.; Ulisse, S.; Fanelli, F.; D’Armiento, M. Iodine deficiency in pregnant women residing in an area with adequate iodine intake. Nutrition 2008, 24, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Pedreol, M.; Ribas-Fito, N.; Garcia-Esteban, R.; Rodriguez, A.; Soriano, D.; Guxens, M.; Mendez, M.; Sunyer, J. Iodine sources and iodine levels in pregnant women from an area without known iodine deficiency. Clin. Endocrinol. 2010, 72, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.L.; Sun, D.J.; Bai, H.Q.; Liu, S.J. The Chinese National Iodine Deficiency Diseases Surveillance in 2005, 1st ed.; People’s Health Publication House: Beijing, China, 2007; pp. 4–21. [Google Scholar]
- Wu, Y.; Li, X.; Chang, S.; Liu, L.; Zou, S.; Hipgrave, D.B. Variable iodine intake persists in the context of universal salt iodization in China. J. Nutr. 2012, 142, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.H.; Xu, L.S.; Wang, M.H. Iodine nutritional status of residents in coastal areas of Fujian province. Chin. J. Endemiol. 2011, 30, 606–610. [Google Scholar]
- Wang, M.H.; Chen, Z.H.; Wu, J.N.; Lan, Y.; Wu, X.Y.; Chen, D.Q. Typical population iodine nutrition and health survey results analysis of Fujian province in 2014. Chin. J. Ctrl. Endem. Dis. 2016, 31, 245–283. [Google Scholar]
- Yang, J.; Zhu, L.; Li, X.F.; Zheng, H.; Wang, Z.; Liu, Y.; Hao, Z. Iodine status of vulnerable population in Henan province of China 2013–2014 after the implementation of the new iodized salt standard. Biol. Trace Elem. Res. 2016, 173, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Delange, F. Iodine deficiency of pregnant women in Europe: A review and recommendations. Eur. J. Clin. Nutr. 2004, 58, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.C.; Rayman, M.P. A review of iodine status of UK pregnant women and its implications for the offspring. Environ. Geochem. Health 2015, 37, 619–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clifton, V.L.; Hodyl, N.A.; Fogarty, P.A.; Torpy, D.J.; Roberts, R.; Nettelbeck, T.; Ma, G.; Hetzel, B. The impact of iodine supplementation and bread fortification on urinary iodine concentration in a mildly iodine-deficient population of pregnant women in South Australia. Nutr. J. 2013. [Google Scholar] [CrossRef] [PubMed]
- Delshad, H.; Touhidi, M.; Abdollahi, Z.; Hedayati, M.; Salehi, F.; Azizi, F. Inadequate iodine nutrition of pregnant women in an area of iodine sufficiency. J. Endocrinol. Investig. 2016, 39, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Simpong, D.L.; Adu, P.; Bashiru, R.; Morna, M.T.; Yeboah, F.A.; Akakpo, K.; Ephraim, R.K. Assessment of iodine status among pregnant women in a rural community in Ghana—A cross sectional study. Arch. Public Health 2016, 74, 8. [Google Scholar] [CrossRef] [PubMed]
- Versloot, P.M.; Schroder, J.P.; Heide, D.; Boogerd, L. Effects of marginal iodine deficiency during pregnancy: Iodide uptake by the maternal and fetal thyroid. Am. J. Physiol. 1997, 273, E1121–E1126. [Google Scholar] [PubMed]
- Liu, Y.; Zhang, L.; Li, J.; Shan, Z.; Teng, W. Maternal marginal iodine efficiency affects the expression of relative proteins during brain development in rat offspring. J. Endocrinol. 2013, 217, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Caron, P. Neurocognitive outcomes of children secondary to mild iodine deficiency in pregnant women. Ann. Endocrinol. 2015, 76, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Hynes, K.L.; Otahal, P.; Hay, I.; Burgess, J.R. Mild iodine deficiency during pregnancy is associated with reduced educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J. Clin. Endocrinol. Metab. 2013, 98, l954–1962. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Iodine and Health: Eliminating Iodine Deficiency Disorders Safely through Salt Iodization. Available online: http://www.who.int/nutrition/publications/micronutrients/iodine_deficiency/WHO_NUT_94.4/en/ (accessed on 8 February 2017).
- Iodine Nutrition and Universal Salt Iodization: A Landscape Analysis in 2012. Available online: http://ign.org/newsletter/idd_nov12_iodine_nutrition_landscape_analysis.pdf (accessed on 8 February 2017).
- Iodine and Pregnancy. Available online: http://www.foodstandards.gov.au/consumer/generalissues/pregnancy/Pages/iodineandpregnancy.aspx (accessed on 8 February 2017).
- Iodine Supplementation in Pregnant and Lactating Women. Available online: http://www.who.int/elena/titles/iodine_pregnancy/en/ (accessed on 8 February 2017).
- Salt Iodization and Risk Assessment of Iodine Status in Chinese Population. Available online: http://www.nhfpc.gov.cn/sps/s3594/201007/d8e251ad2dfd44408755e05acdeb36e3.shtml (accessed on 5 January 2017).
- Mao, G.M.; Ding, G.Q.; Huang, L.C.; Lou, X.M.; Zhang, R.H.; Zhu, W.M.; Wang, X.F.; Mo, Z.; Zhou, J.S. Study on level of dietary iodine intake and its contribution rate of residents in Zhejiang. Chin. J. Prev. Med. 2013, 47, 1031–1035. [Google Scholar]
- Zhu, W.M.; Lou, X.M.; Ding, G.Q.; Mao, G.M.; Mo, Z.; Miao, X.F.; Zhou, J.S. A cross-sectional study on iodine nutrition in population in Zhejiang province in 2009. Zhejiang Prev. Med. 2010, 22, 1–4. [Google Scholar]

| Median UIC (μg/L) | Iodine Intake | Iodine Nutrition Status |
|---|---|---|
| <150 | Insufficient | Iodine deficiency |
| 150–249 | Adequate | Optimal |
| 250–499 | Above requirements | - |
| ≥500 | Excessive | - |
| Variables | Number (%) |
|---|---|
| Maternal Age | |
| ≤30 years | 5973 (73.2) |
| >31 years | 2186 (26.8) |
| Areas | |
| Coastal | 4372 (53.6) |
| Inland | 3787 (46.4) |
| Total | 8159 (100) |
| Variables | N | Median UIC, Interquartile Range (µg/L) | p-Value |
|---|---|---|---|
| Maternal Age | |||
| ≤30 years | 6240 | 149.9 (93.3–212.3) | 0.085 |
| >31 years | 2270 | 143.9 (92.5–204.3) | |
| Salt | |||
| Non-iodized salt | 450 | 99.6 (62.22–16.8) | <0.001 |
| Adequately iodized salt | 7392 | 151.9 (97.6–215.0) | |
| Areas | |||
| Coastal | 4075 | 130.1 (79.9–193.9) | <0.001 |
| Inland | 4435 | 158.1 (107.1–222.3) |
| Variables | Non-Iodized Salt | Adequately Iodized Salt | χ2 Value | p-Value |
|---|---|---|---|---|
| Maternal Age | ||||
| ≤30 years | 5.5 (314) | 94.5 (5312) | 3.006 | 0.083 |
| >31 years | 6.5 (136) | 93.5 (1951) | ||
| Areas | ||||
| Coastal | 10.5(378) | 89.5 (3216) | 279.6 | <0.001 |
| Inland | 1.7 (71) | 98.3 (4147) |
| Salt | Percentage of UIC Levels, % (N) | Sum | |||
|---|---|---|---|---|---|
| <150 µg/L | 150–249 µg/L | 250–499 µg/L | ≥500 µg/L | ||
| Non-iodized salt | 71.6 (322) | 16.7 (75) | 7.5 (34) | 4.2 (19) | 100.0 (450) |
| Adequately iodized salt | 49.5 (3662) | 33.8 (2498) | 13.3 (979) | 3.4 (253) | 100.0 (7392) |
| All salt | 51.0 (4341) | 32.9 (2803) | 12.8 (1082) | 3.3 (284) | 100.0 (8510) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Zhu, W.; Mo, Z.; Wang, Y.; Mao, G.; Wang, X.; Lou, X. An Increase in Consuming Adequately Iodized Salt May Not Be Enough to Rectify Iodine Deficiency in Pregnancy in an Iodine-Sufficient Area of China. Int. J. Environ. Res. Public Health 2017, 14, 206. https://doi.org/10.3390/ijerph14020206
Wang Z, Zhu W, Mo Z, Wang Y, Mao G, Wang X, Lou X. An Increase in Consuming Adequately Iodized Salt May Not Be Enough to Rectify Iodine Deficiency in Pregnancy in an Iodine-Sufficient Area of China. International Journal of Environmental Research and Public Health. 2017; 14(2):206. https://doi.org/10.3390/ijerph14020206
Chicago/Turabian StyleWang, Zhifang, Wenming Zhu, Zhe Mo, Yuanyang Wang, Guangming Mao, Xiaofeng Wang, and Xiaoming Lou. 2017. "An Increase in Consuming Adequately Iodized Salt May Not Be Enough to Rectify Iodine Deficiency in Pregnancy in an Iodine-Sufficient Area of China" International Journal of Environmental Research and Public Health 14, no. 2: 206. https://doi.org/10.3390/ijerph14020206
APA StyleWang, Z., Zhu, W., Mo, Z., Wang, Y., Mao, G., Wang, X., & Lou, X. (2017). An Increase in Consuming Adequately Iodized Salt May Not Be Enough to Rectify Iodine Deficiency in Pregnancy in an Iodine-Sufficient Area of China. International Journal of Environmental Research and Public Health, 14(2), 206. https://doi.org/10.3390/ijerph14020206





