Comparison of Influenza Epidemiological and Virological Characteristics between Outpatients and Inpatients in Zhejiang Province, China, March 2011–June 2015
Abstract
:1. Introduction
2. Materials and Methods
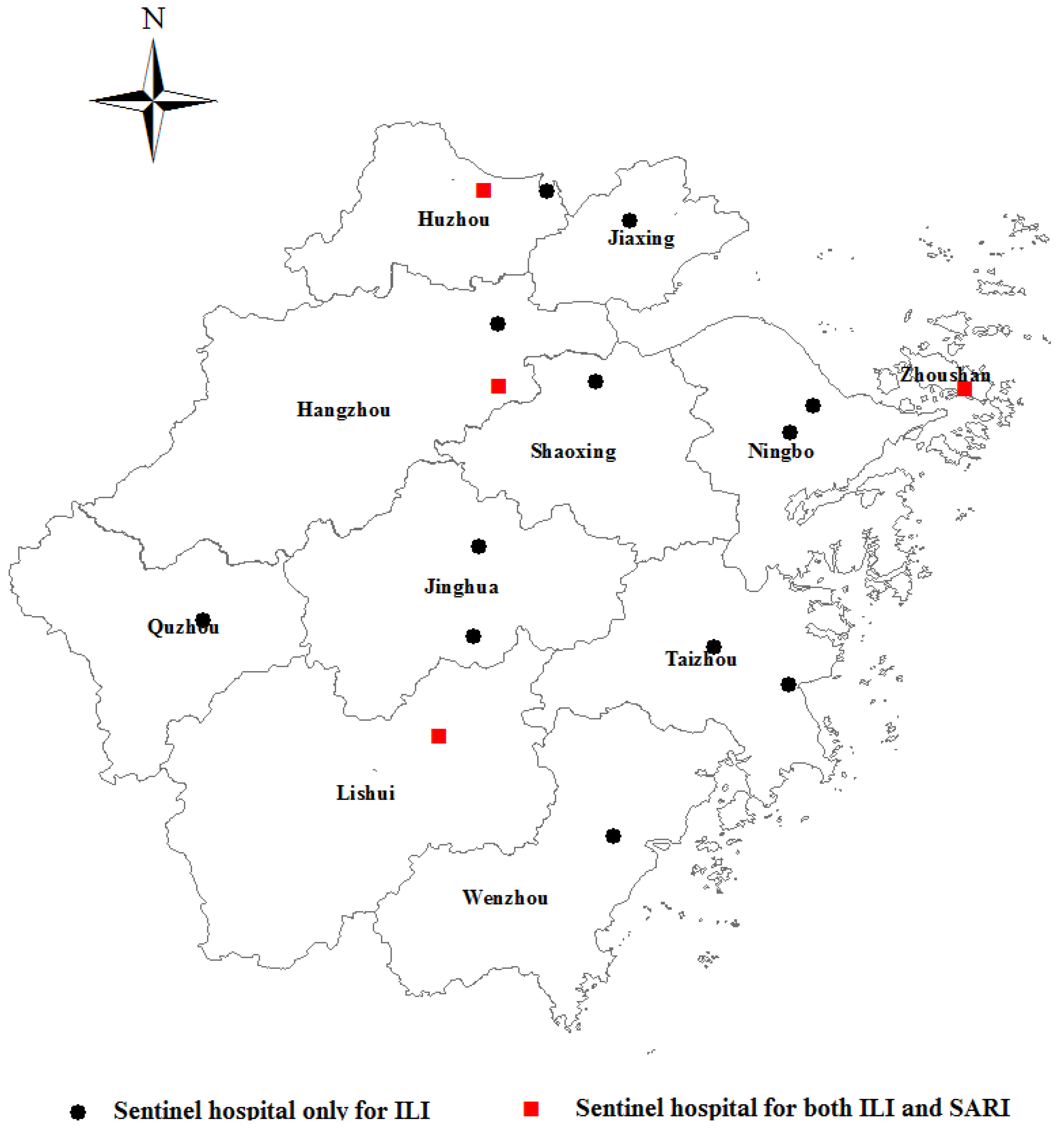
2.1. Flu Surveillance
2.2. Case Definition
2.3. Data Collection
2.4. Statistical Methods
2.5. Ethical Consideration
3. Results
3.1. Age Distribution among Total ILI and SARI Cases
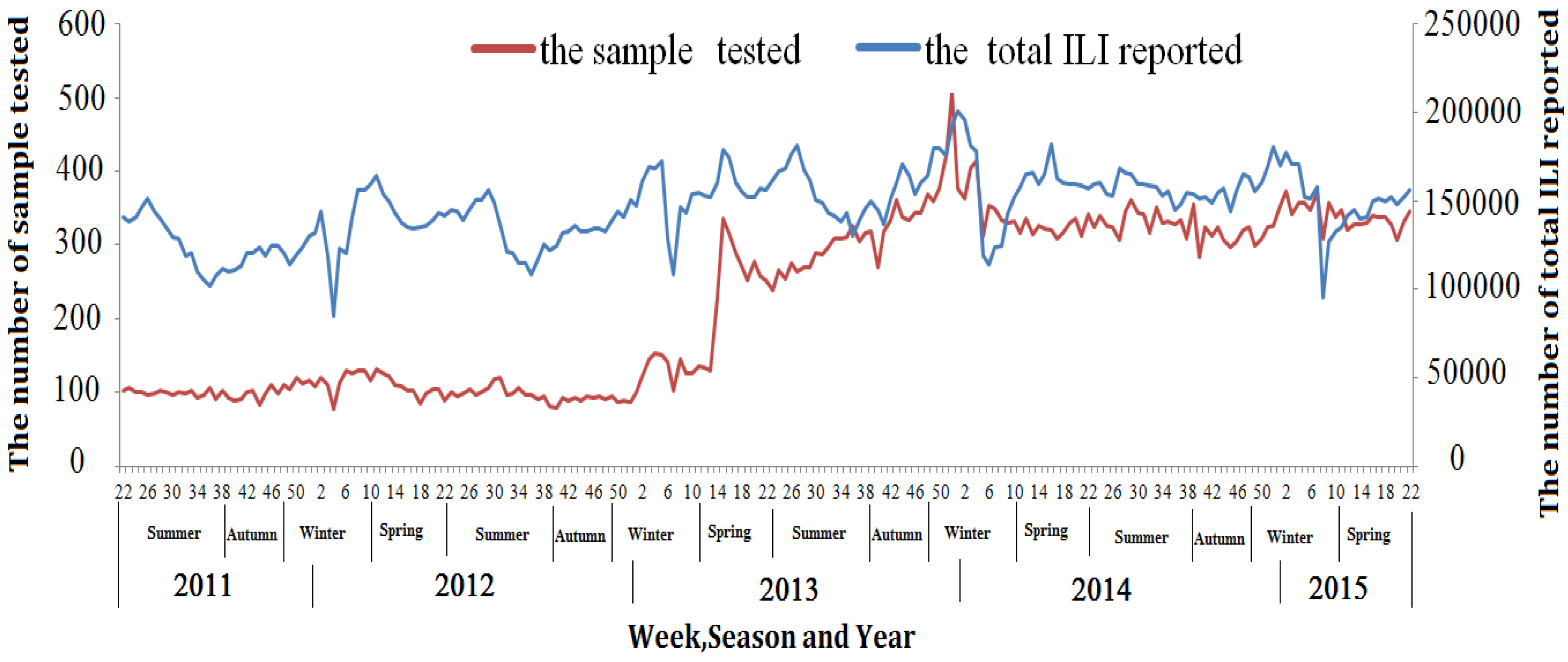
3.2. Demographic and Virologic Characteristics of the Sampled Patients
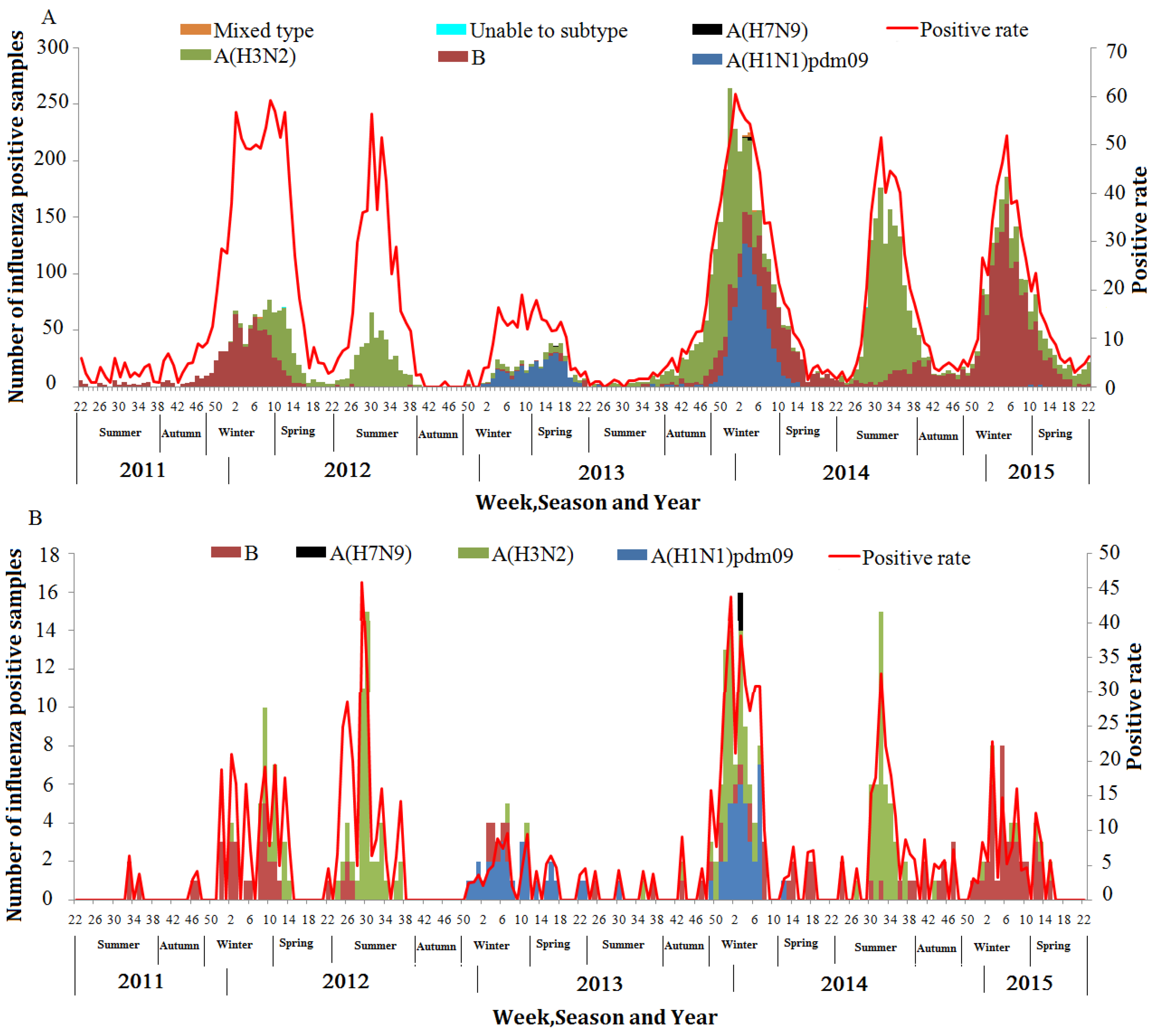
3.3. Constitution of the Detected Influenza Virus and Influenza A Virus among ILI and SARI Patients
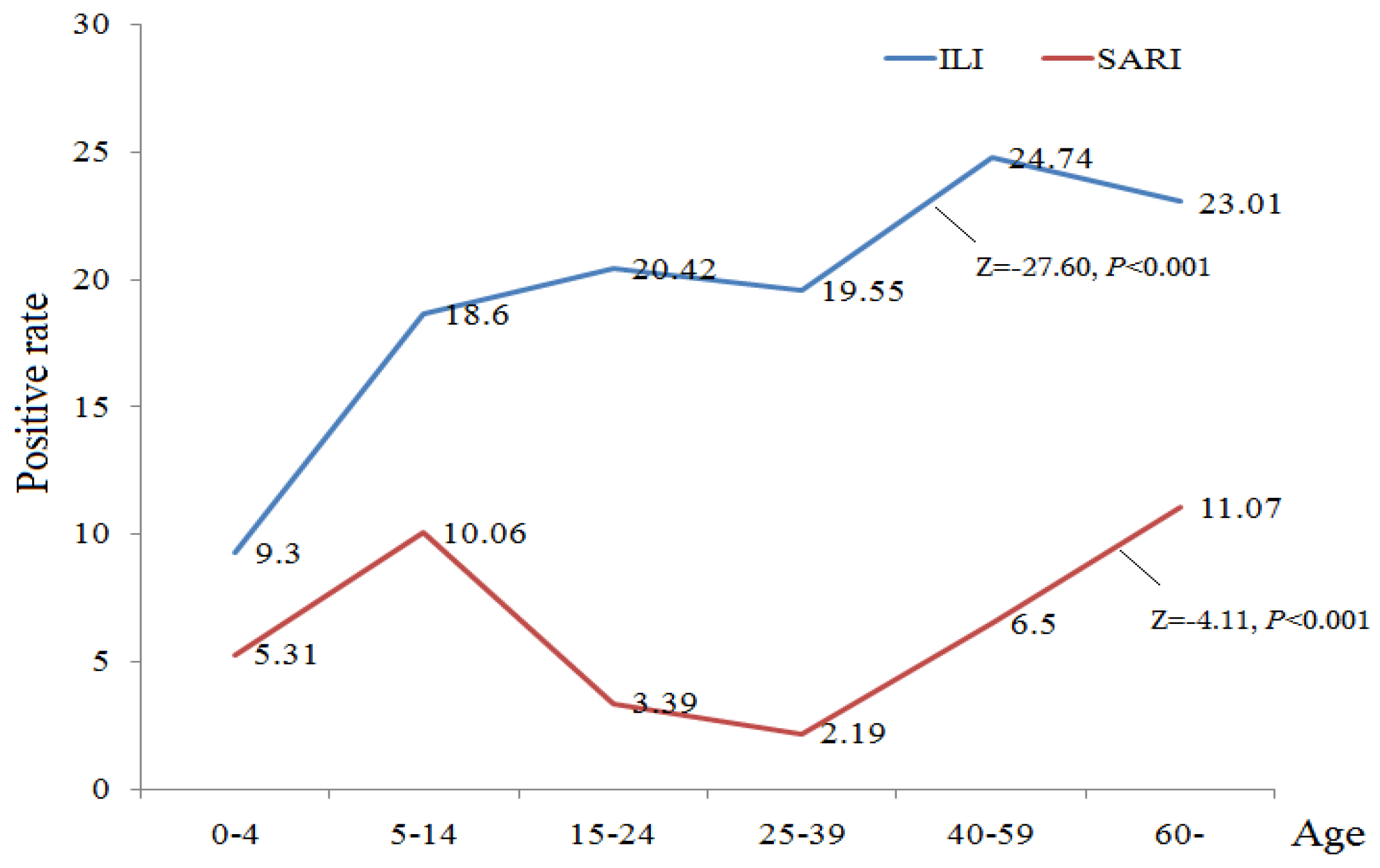
3.4. Influenza Virus Detection Rate across Age, Sex and Season among Sampled ILI and SARI Patients
3.5. Seasonality and Circulation of Influenza Types and Subtypes among ILI and SARI Cases
3.6. Correlation Analysis between Weekly ILI Influenza-Positive Rate and SARI Influenza-Positive Rate, ILI Percentage and ILI Influenza-Positive Rate, SARI Percentage and SARI Influenza-Positive Rate
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Influenza Overview. Available online: http://www.who.int/mediacentre/factsheets/fs211/en/ (accessed on 6 July 2016).
- De Francisco Shapovalova, N.; Donadel, M.; Jit, M.; Hutubessy, R. A systematic review of the social and economic burden of influenza in low- and middle-income countries. Vaccine 2015, 33, 6537–6544. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Jit, M.; Leung, K.S.; Zheng, Y.M.; Feng, L.Z.; Wang, L.P.; Lau, E.H.; Wu, J.T.; Yu, H.J. The economic burden of influenza-associated outpatient visits and hospitalizations in China: A retrospective survey. Infect. Dis. Poverty 2015, 4, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, Z.; Feng, L.; Carolyn, G.M.; Wang, K.; Zhu, G.; Zhang, Y.; Hu, J.; Huang, Y.; Pan, H.; Guo, N.; et al. Characterizing the epidemiology, virology, and clinical features of influenza in China’s first severe acute respiratory infection sentinel surveillance system, February 2011–October 2013. BMC Infect. Dis. 2015, 15, 143. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Epidemiological Surveillance Standards for Influenza. Available online: http://www.who.int/influenza/resources/documents/influenza_surveillance_manual/en/ (accessed on 1 June 2016).
- Al-Awaidy, S.; Hamid, S.; Al Obaidani, I.; Al Baqlani, S.; Al Busaidi, S.; Bawikar, S.; El-Shoubary, W.; Dueger, E.L.; Said, M.M.; Elamin, E.; et al. The Burden of Influenza-Associated Hospitalizations in Oman, January 2008–June 2013. PLoS ONE 2015, 10, e0144186. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Situ, S.; Huang, T.; Hu, S.; Wang, X.; Zhu, X.; Gao, L.; Li, Z.; Feng, A.; Jin, H.; et al. Direct medical cost of influenza-related hospitalizations among severe acute respiratory infections cases in three provinces in China. PLoS ONE 2013, 8, e63788. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.; Cohen, A.; Walaza, S.; Groome, M.; Madhi, S.; Variava, E.; Kahn, K.; Dawood, H.; Tempia, S.; Tshangela, A.; et al. Determining the Provincial and National Burden of Influenza-Associated Severe Acute Respiratory Illness in South Africa Using a Rapid Assessment Methodology. PLoS ONE 2015, 10, e0132078. [Google Scholar] [CrossRef] [PubMed]
- Lutwama, J.J.; Bakamutumaho, B.; Kayiwa, J.T.; Chiiza, R.; Namagambo, B.; Katz, M.A.; Geissler, A.L. Clinic- and hospital-based sentinel influenza surveillance, Uganda 2007–2010. J. Infect. Dis. 2012, 206 (Suppl. 1), S87–S93. [Google Scholar] [CrossRef] [PubMed]
- Burmaa, A.; Kamigaki, T.; Darmaa, B.; Nymadawa, P.; Oshitani, H. Epidemiology and impact of influenza in Mongolia, 2007–2012. Influenza Other Respir. Viruses 2014, 8, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Tallo, V.L.; Kamigaki, T.; Tan, A.G.; Pamaran, R.R.; Alday, P.P.; Mercado, E.S.; Javier, J.B.; Oshitani, H.; Olveda, R.M. Estimating influenza outpatients’ and inpatients’ incidences from 2009 to 2011 in a tropical urban setting in the Philippines. Influenza Other Respir. Viruses 2014, 8, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Azziz-Baumgartner, E.; Alamgir, A.S.; Rahman, M.; Homaira, N.; Sohel, B.M.; Sharker, M.A.; Zaman, R.U.; Dee, J.; Gurley, E.S.; Al Mamun, A.; et al. Incidence of influenza-like illness and severe acute respiratory infection during three influenza seasons in Bangladesh, 2008–2010. Bull. World Health Organ. 2012, 90, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Nyatanyi, T.; Nkunda, R.; Rukelibuga, J.; Palekar, R.; Muhimpundu, M.A.; Kabeja, A.; Kabanda, A.; Lowrance, D.; Tempia, S.; Koama, J.B.; et al. Influenza sentinel surveillance in Rwanda, 2008–2010. J. Infect. Dis. 2012, 206 (Suppl. 1), S74–S79. [Google Scholar] [CrossRef] [PubMed]
- Radin, J.M.; Katz, M.A.; Tempia, S.; Talla Nzussouo, N.; Davis, R.; Duque, J.; Adedeji, A.; Adjabeng, M.J.; Ampofo, W.K.; Ayele, W.; et al. Influenza surveillance in 15 countries in Africa, 2006–2010. J. Infect. Dis. 2012, 206 (Suppl. 1), S14–S21. [Google Scholar] [CrossRef] [PubMed]
- Badar, N.; Bashir Aamir, U.; Mehmood, M.R.; Nisar, N.; Alam, M.M.; Kazi, B.M.; Zaidi, S.S. Influenza virus surveillance in Pakistan during 2008–2011. PLoS ONE 2013, 8, e79959. [Google Scholar] [CrossRef] [PubMed]
- Dalhatu, I.T.; Medina-Marino, A.; Olsen, S.J.; Hwang, I.; Gubio, A.B.; Ekanem, E.E.; Coker, E.B.; Akpan, H.; Adedeji, A.A. Influenza viruses in Nigeria, 2009–2010: Results from the first 17 months of a national influenza sentinel surveillance system. J. Infect. Dis. 2012, 206 (Suppl. 1), S121–S128. [Google Scholar] [CrossRef] [PubMed]
- Mainassara, H.B.; Lagare, A.; Tempia, S.; Sidiki, A.; Issaka, B.; AbdouSidikou, B.; OuweMissiOukem-Boyer, O. Influenza Sentinel Surveillance among Patients with Influenza-Like-Illness and Severe Acute Respiratory Illness within the Framework of the National Reference Laboratory, Niger, 2009–2013. PLoS ONE 2015, 10, e0133178. [Google Scholar] [CrossRef] [PubMed]
- Muyembe Tamfum, J.J.; Nkwembe, E.; Bi Shamamba, S.K.; Bankoshi, F.; Ilunga, B.K.; Katz, K.A.; Cohen, A.L.; Kabamba, J.; Wemankoy, E.O. Sentinel surveillance for influenza-like illness, severe acute respiratory illness, and laboratory-confirmed influenza in Kinshasa, Democratic Republic of Congo, 2009–2011. J. Infect. Dis. 2012, 206 (Suppl. 1), S36–S40. [Google Scholar] [CrossRef] [PubMed]
- Refaey, S.; Amin, M.; Labib, M.; Kandeel, A. Influenza virus positivity and circulating subtypes among cases of influenza-like illness and severe acute respiratory infection, Egypt, 2012–2015. East. Mediterr. Health J. 2016, 22, 527–536. [Google Scholar] [PubMed]
- Feng, L.; Shay, D.K.; Jiang, Y.; Zhou, H.; Chen, X.; Zheng, Y.; Jiang, L.; Zhang, Q.; Lin, H.; Wang, S.; et al. Influenza-associated mortality in temperate and subtropical Chinese cities, 2003–2008. Bull. World Health Organ. 2012, 90, 279B–288B. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Alonso, W.J.; Feng, L.; Tan, Y.; Shu, Y.; Yang, W.; Viboud, C. Characterization of regional influenza seasonality patterns in China and implications for vaccination strategies: Spatio-temporal modeling of surveillance data. PLoS Med. 2013, 10, e1001552. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Wu, L.; Gao, D.; Fan, G. Method for four seasons division in Zhejiang Province. Meteorol. Sci. Technol. 2014, 42, 474–481. [Google Scholar]
- Al-Abdallat, M.; Dawson, P.; Haddadin, A.J.; El-Shoubary, W.; Dueger, E.; Al-Sanouri, T.; Said, M.M.; Talaat, M. Influenza hospitalization epidemiology from a severe acute respiratory infection surveillance system in Jordan, January 2008–February 2014. Influenza Other Respir. Viruses 2016, 10, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Barakat, A.; Ihazmad, H.; Benkaroum, S.; Cherkaoui, I.; Benmamoun, A.; Youbi, M.; El Aouad, R. Influenza surveillance among outpatients and inpatients in Morocco, 1996–2009. PLoS ONE 2011, 6, e24579. [Google Scholar] [CrossRef] [PubMed]
- CDC. Summary Recommendations: Prevention and Control of Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2013–14. Available online: http://www.cdc.gov/flu/professionals/acip/2013-summary-recommendations.htm (accessed on 1 July 2015).
- Caini, S.; Andrade, W.; Badur, S.; Balmaseda, A.; Barakat, A.; Bella, A.; Bimohuen, A.; Brammer, L.; Bresee, J.; Bruno, A.; et al. Temporal Patterns of Influenza A and B in Tropical and Temperate Countries: What Are the Lessons for Influenza Vaccination? PLoS ONE 2016, 11, e0152310. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Expert Group Meeting on Seasonal Influenza Vaccine Composition for Tropics and Subtropics. Available online: http://www.who.int/influenza/resources/publications/expert_group_meeting_seasonal_influenza_vaccine_tropics/en/ (accessed on 1 July 2016).
- Murray, E.L.; Khagayi, S.; Ope, M.; Bigogo, G.; Ochola, R.; Muthoka, P.; Njenga, K.; Odhiambo, F.; Burton, D.; Laserson, K.F.; et al. What are the most sensitive and specific sign and symptom combinations for influenza in patients hospitalized with acute respiratory illness? Results from western Kenya, January 2007–July 2010. Epidemiol. Infect. 2013, 141, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Njouom, R.; Yekwa, E.L.; Cappy, P.; Vabret, A.; Boisier, P.; Rousset, D. Viral etiology of influenza-like illnesses in Cameroon, January–December 2009. J. Infect. Dis. 2012, 206 (Suppl. 1), S29–S35. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Pan, L.; Sun, Q.; Zhu, W.; Zhu, L.; Ye, C.; Xue, C.; Wang, Y.; Liu, Q.; Ma, P.; et al. The clinical and etiological characteristics of influenza-like illness (ILI) in outpatients in Shanghai, China, 2011 to 2013. PLoS ONE 2015, 10, e0119513. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.Y.; Song, J.Y.; Cheong, H.J.; Choi, W.S.; Lee, J.; Lee, J.S.; Wie, S.H.; Jeong, H.W.; Kim, Y.K.; Choi, S.H.; et al. Laboratory surveillance of influenza-like illness in seven teaching hospitals, South Korea: 2011–2012 season. PLoS ONE 2013, 8, e64295. [Google Scholar] [CrossRef]
- Zhang, C.; Zhu, N.; Xie, Z.; Lu, R.; He, B.; Liu, C.; Ma, X.; Tan, W. Viral etiology and clinical profiles of children with severe acute respiratory infections in China. PLoS ONE 2013, 8, e72606. [Google Scholar] [CrossRef] [PubMed]
- Simusika, P.; Bateman, A.C.; Theo, A.; Kwenda, G.; Mfula, C.; Chentulo, E.; Monze, M. Identification of viral and bacterial pathogens from hospitalized children with severe acute respiratory illness in Lusaka, Zambia, 2011–2012: A cross-sectional study. BMC Infect. Dis. 2015, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.Y.; Chai, C.L.; Li, F.D.; He, F.; Yu, Z.; Wang, X.X.; Shang, X.P.; Liu, S.L.; Lin, J.F. Epidemiology of human infections with avian influenza A(H7N9) virus in the two waves before and after October 2013 in Zhejiang province, China. Epidemiol. Infect. 2015, 143, 1839–1845. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Overall (%) | ILI (%) | SARI (%) | p-Value |
|---|---|---|---|---|
| Tested specimens | 52,293 | 46,868 | 5425 | |
| Age, year | ||||
| Median, IQR | 15 (3–34) | 18 (4–35) | 1 (0.5–6) | <0.001 |
| 0–4 | 16,919 (32.35) | 13,038 (27.82) | 3881 (71.54) | |
| 5–14 | 8318 (15.91) | 7817 (16.68) | 501 (9.24) | |
| 15–24 | 5330 (10.19) | 5284 (11.27) | 46 (0.85) | |
| 25–39 | 9516 (18.20) | 9379 (20.01) | 137 (2.53) | |
| 40–59 | 6709 (12.83) | 6355 (13.56) | 354 (6.53) | |
| ≥60 | 5501 (10.52) | 4995 (10.66) | 506 (9.33) | |
| Sex | <0.001 | |||
| Male | 27,070 (51.77) | 23,747 (50.67) | 3323 (61.25) | |
| Female | 25,223 (48.23) | 23,121 (49.33) | 2102 (38.75) | |
| Seasons | <0.001 | |||
| Spring | 12,057 (23.06) | 10,998 (23.47) | 1059 (19.52) | |
| Summer | 15,820 (30.25) | 14,250 (30.40) | 1570 (28.94) | |
| Autumn | 9292 (17.77) | 8348 (17.81) | 944 (17.40) | |
| Winter | 15,124 (28.92) | 13,272 (28.32) | 1852 (34.14) | |
| Influenza virus type detected | 0.774 | |||
| Influenza A virus | 5334 (62.02) | 5119 (61.97) | 215 (63.05) | |
| Influenza B virus | 3258 (37.88) | 3132 (37.92) | 126 (36.95) | |
| Mixed type | 9 (0.10) | 9 (0.11) | 0 (0.00) | |
| Influenza A virus subtype detected | 0.067 | |||
| A(H3N2) | 3997 (74.93) | 3839 (75.00) | 158 (73.49) | |
| A(H1N1)pdm09 | 1328 (24.90) | 1273 (24.87) | 55 (25.58) | |
| A(H7N9) | 7 (0.13) | 5 (0.10) | 2 (0.93) | |
| A(Untype) | 2 (0.04) | 2 (0.04) | 0 (0.00) |
| Characteristic | ILI | SARI | p-Value |
|---|---|---|---|
| Overall | 8260 (17.62) | 341 (6.29) | 0.001 |
| Age, year | |||
| 0–4 | 1212 (9.30) | 204 (5.31) | 0.001 |
| 5–14 | 1543 (18.60) | 51 (10.06) | 0.001 |
| 15–24 | 1228 (20.42) | 2 (3.39) | 0.001 |
| 25–39 | 1834 (19.55) | 3 (2.19) | 0.001 |
| 40–59 | 1572 (24.74) | 23 (6.50) | 0.001 |
| ≥60 | 871 (23.01) | 58 (11.07) | 0.001 |
| Sex | |||
| Male | 4017 (16.92) | 220 (6.62) | 0.001 |
| Female | 4243 (18.35) | 121 (5.76) | 0.001 |
| Seasons | |||
| Spring | 1135 (10.32) | 38 (3.59) | 0.001 |
| Summer | 1951 (13.69) | 106 (6.75) | 0.001 |
| Autumn | 614 (7.36) | 15 (1.59) | 0.001 |
| Winter | 4560 (34.36) | 182 (9.83) | 0.001 |
| Variable | Correlation Coefficient | p-Value |
|---|---|---|
| A(H1N1)pdm09 | 0.51 | <0.001 |
| A(H3N2) | 0.43 | <0.001 |
| Influenza B | 0.17 | 0.013 |
| Variable | Correlation Coefficient | p-Value |
|---|---|---|
| ILI influenza-positive rate and SARI influenza-positive rate | 0.63 | <0.001 |
| ILI percentage and ILI influenza-positive rate | 0.53 | <0.001 |
| SARI percentage and SARI influenza-positive rate | 0.19 | 0.006 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, W.; Yu, Z.; Liu, S.; Zhang, X.; Wang, X.; Cai, J.; Ling, F.; Chen, E. Comparison of Influenza Epidemiological and Virological Characteristics between Outpatients and Inpatients in Zhejiang Province, China, March 2011–June 2015. Int. J. Environ. Res. Public Health 2017, 14, 217. https://doi.org/10.3390/ijerph14020217
Cheng W, Yu Z, Liu S, Zhang X, Wang X, Cai J, Ling F, Chen E. Comparison of Influenza Epidemiological and Virological Characteristics between Outpatients and Inpatients in Zhejiang Province, China, March 2011–June 2015. International Journal of Environmental Research and Public Health. 2017; 14(2):217. https://doi.org/10.3390/ijerph14020217
Chicago/Turabian StyleCheng, Wei, Zhao Yu, Shelan Liu, Xueying Zhang, Xiaoxiao Wang, Jian Cai, Feng Ling, and Enfu Chen. 2017. "Comparison of Influenza Epidemiological and Virological Characteristics between Outpatients and Inpatients in Zhejiang Province, China, March 2011–June 2015" International Journal of Environmental Research and Public Health 14, no. 2: 217. https://doi.org/10.3390/ijerph14020217
APA StyleCheng, W., Yu, Z., Liu, S., Zhang, X., Wang, X., Cai, J., Ling, F., & Chen, E. (2017). Comparison of Influenza Epidemiological and Virological Characteristics between Outpatients and Inpatients in Zhejiang Province, China, March 2011–June 2015. International Journal of Environmental Research and Public Health, 14(2), 217. https://doi.org/10.3390/ijerph14020217





