Disparity in Retention in Care and Viral Suppression for Black Caribbean-Born Immigrants Living with HIV in Florida
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Individual-Level Characteristics
2.3. Neighborhood-Level Characteristics
2.4. Analytic Plan
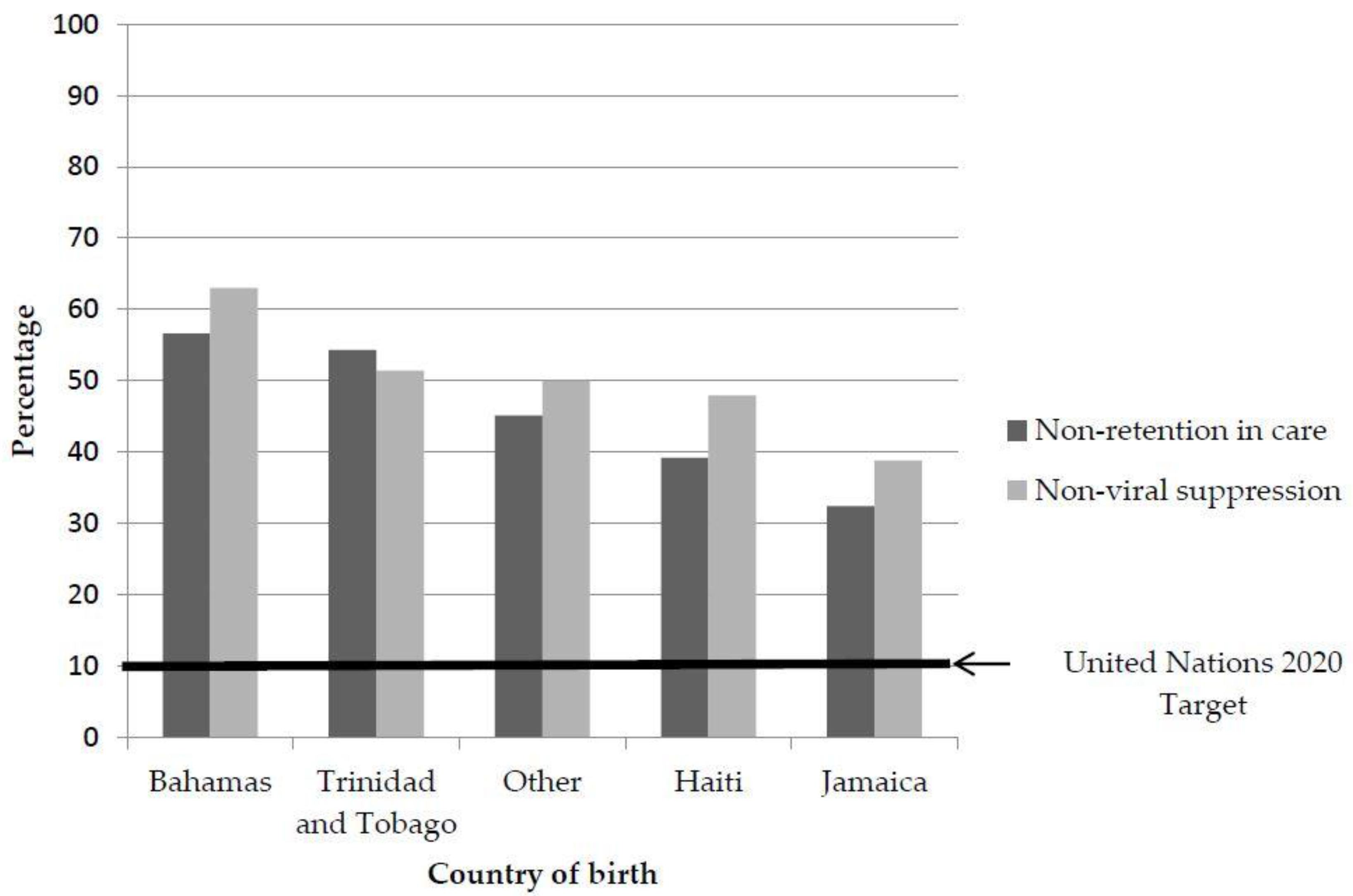
3. Results
Multivariate Analysis
Non-Retention in Care
Non-Viral Suppression
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention. HIV Surveillance Report. Available online: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf (accessed on 9 September 2015).
- Shah, M.; Perry, A.; Risher, K.; Kapoor, S.; Grey, J.; Sharma, A.; Rosenberg, E.S.; Del Rio, C.; Sullivan, P.; Dowdy, D.W. Effect of the US national HIV/AIDS strategy targets for improved HIV care engagement: A modelling study. Lancet HIV 2016, 3, e140–e146. [Google Scholar] [CrossRef]
- Cohen, M.; Chen, Y.; McCauley, M.; Gamble, T.; Hosseinipour, M.; Kumarasamy, N.; Hakim, J.; Kumwenda, N.; Brum, T.; Grinsztejn, B. Final results of the HPTN 052 randomized controlled trial: Antiretroviral therapy prevents HIV transmission. J. Int. AIDS Soc. 2015, 18. doi:10.7448/IAS.18.5.20482. [Google Scholar] [CrossRef]
- Saint-Jean, G.; Devieux, J.; Malow, R.; Tammara, H.; Carney, K. Substance abuse, acculturation, and HIV risk among Caribbean-born immigrants in the United States. J. Int. Assoc. Physicians AIDS Care 2011, 10, 326–332. [Google Scholar] [CrossRef] [PubMed]
- McCabe, K. Caribbean Immigrants in the United States; Migration Policy Institute: Washington, DC, USA, 2011. [Google Scholar]
- Johnson, A.S.; Hu, X.; Dean, H.D. Epidemiologic differences between native-born and foreign-born Black people diagnosed with HIV infection in 33 US States, 2001–2007. Public Health Rep. 2010, 125, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Florida Department of Health. HIV among the Haitian-Born in Florida and Miami-Dade. 2012. Available online: http://www.dadehealth.org/HIV-MDC_FS2012%20HAITIANS.pdf0.pdf (accessed on 22 December 2016).
- Cyrus, E.; Sheehan, D.M.; Fennie, K.; Sanchez, M.; Dawson, C.; Cameron, M.; Maddox, L.; Trepka, M.J. Delayed diagnosis among non-Latino Caribbean immigrants. J. Healthc. Poor Underserved 2017, in press. [Google Scholar]
- Gardner, E.M.; McLees, M.P.; Steiner, J.F.; Del Rio, C.; Burman, W.J. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin. Infect. Dis. 2011, 52, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.L.; Ward, J.W.; Janssen, R.S.; De Cock, K.M.; Valdiserri, R.O.; Gayle, H.D.; Jones, J.L.; Lehman, J.S.; Lindegren, M.L.; Nakashima, A.K. Guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. MMWR Recomm. Rep. 1999, 48, 1–28. [Google Scholar]
- Hall, H.I.; Gray, K.M.; Tang, T.; Li, J.; Shoulse, L.; Mermin, J. Retention in care of adults and adolescents living with HIV in 13 US areas. J. Acquir. Immune Defic. Syndr. 2012, 60, 77–82. [Google Scholar] [CrossRef] [PubMed]
- United States Department of Health and Human Services. HIV/AIDS Bureau Performance Measures. Available online: http://hab.hrsa.gov/deliverhivaidscare/coremeasures.pdf (accessed on 23 August 2016).
- Florida International University Metropolitan Center. Florida’s Changing Demographics: Hispanic Political Influence. Available online: http://metropolitan.fiu.edu/news/2010/florida-changing-demographics-hispanic-political-influence/naleo_2010.pdf (accessed on 12 December 2016).
- Castro, K.G.; Ward, J.W.; Slutsker, L.; Buehler, J.W.; Jaffe, H.W.; Berkelman, R.L.; Curran, J.W. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm. Rep. 1992, 41, 1–19. [Google Scholar] [CrossRef]
- Sheehan, D.M.; Trepka, M.J.; Fennie, K.P.; Prado, G.; Cano, M.A.; Maddox, L.M. Black-White Latino racial disparities in HIV survival, Florida, 2000–2011. Int. J. Environ. Res. Public Health 2015, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- WWAMI Rural Health Research Center. Rural Urban Commuting Areas. Available online: http://depts.washington.edu/uwruca/ruca-uses.php (accessed on 26 April 2015).
- SAS Institute. The SAS System for Windows. Available online: https://www.sas.com/en_us/software/sas9.html (accessed on 5 September 2011).
- Joint United Nations Programme on HIV/AIDS. 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic. Available online: http://www.unaids.org/en/resources/documents/2014/90-90-90 (accessed on 9 September 2014).
- Joint United Nations Programme on HIV/AIDS (UNAIDS). The Gap Report. Available online: http://files.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf (accessed on 9 September 2014).
- Sheehan, D.M.; Trepka, M.J.; Fennie, K.P.; Maddox, L.M. Rate of new HIV diagnoses among Latinos living in Florida: Disparities by country/region of birth. AIDS Care 2015, 27, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Perez, A.J. Wet foot, dry foot, no foot: The recurring controversy between Cubans, Haitians, and the United States immigration policy. Nova L. Rev. 2003, 28, 437. [Google Scholar]
- Migration Policy Institute. Haitian Immigrants in the United States. Available online: http://www.migrationpolicy.org/article/haitian-immigrants-united-states (accessed on 22 December 2016).
- Girard, C.C. Insulating an ideology: The enclave effect on South Florida’s Cuban Americans. Hisp. J. Behav. Sci. 2008, 30, 530–543. [Google Scholar] [CrossRef]
- Craton, M. The Bahamian self and the Haitian other: The migration of Haitians to and through the Bahamas, 1950–2000. Immigr. Minor. 1995, 14, 265–288. [Google Scholar] [CrossRef]
- Fielding, W.J.; Balance, V.; Scriven, C.; McDonald, T.; Johnson, P. The stigma of being “Haitian” in the Bahamas. Int. J. Bahamian Stud. 2008, 14, 38–50. [Google Scholar] [CrossRef]
- Tinker, K.L. The Migration of Peoples from the Caribbean to the Bahamas; University Press of Florida: Gainsville, FL, USA, 2011. [Google Scholar]
- Phillips, C.D.; McLeroy, K.R. Health in rural America: Remembering the importance of place. Am. J. Public Health 2004, 94, 1661–1663. [Google Scholar] [CrossRef] [PubMed]
- Gfroerer, J.C.; Larson, S.L.; Colliver, J.D. Drug use patterns and trends in rural communities. J. Rural Health 2007, 23, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Power, R.; Koopman, C.; Volk, J.; Israelski, D.M.; Stone, L.; Chesney, M.A.; Spiegel, D. Social support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected persons. AIDS Patient Care STDS 2003, 17, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Skarbinski, J.; Rosenberg, E.; Paz-Bailey, G.; Hall, H.I.; Rose, C.E.; Viall, A.H.; Fagan, J.L.; Lansky, A.; Mermin, J.H. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern. Med. 2015, 175, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Bradley, H.; Hall, H.I.; Wolitski, R.J.; Van Handel, M.M.; Stone, A.E.; LaFlam, M.; Skarbinski, J.; Higa, D.H.; Prejean, J.; Frazier, E.L. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 1113–1117. [Google Scholar] [PubMed]
- Rosenberg, E.S.; Millett, G.A.; Sullivan, P.S.; Del Rio, C.; Curran, J.W. Understanding the HIV disparities between Black and White men who have sex with men in the USA using the HIV care continuum: A modelling study. Lancet HIV 2014, 1, e112–e118. [Google Scholar] [CrossRef]
- Weinhardt, L.S.; Forsyth, A.D.; Care, M.P.; Jaworski, B.C.; Durant, L.E. Reliability and validity of self-report measures of HIV-related sexual behavior: Progress since 1990 and recommendations for research and practice. Arch. Sex. Behav. 1998, 27, 155–180. [Google Scholar] [CrossRef] [PubMed]
- Schroder, K.E.E.; Carey, M.P.; Vanable, P.A. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann. Behav. Med. 2003, 26, 104–123. [Google Scholar] [CrossRef] [PubMed]
- Parker, R.D.; Dykema, S. The reality of homeless mobility and implications for improving care. J. Community Health 2013, 38, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Hall, B.J.; Sou, K.; Beanland, R.; Lacky, M.; Tso, L.S.; Ma, Q.; Doherty, M.; Tucker, J.D. Barriers and facilitators to interventions improving retention in HIV care: A qualitative evidence meta-synthesis. AIDS Behav. 2016. doi:10.1007/s10461-016-1537-0. [Google Scholar] [CrossRef] [PubMed]
- Ghavami, N.; Katsiaficas, D.; Rogers, L.O. Chapter Two-toward an intersectional approach in developmental science: The role of race, gender, sexual orientation, and immigrant status. Adv. Child Dev. Behav. 2016, 50, 31–73. [Google Scholar] [PubMed]
| Caribbean-Born Blacks | US Born Cases | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Haiti | Jamaica | Bahamas | Trinidad & Tobago | Other a | US Blacks | Hispanic | Non-Hispanic Whites | p-Value | |
| (n, %) | (n, %) | (n, %) | (n, %) | (n, %) | (n, %) | (n, %) | (n, %) | ||
| Total [n (%)] b | 4491 (8) | 701 (1.3) | 265 (0.5) | 70 (0.12) | 122 (0.2) | 22,362 (39.9) | 13,859 (24.7) | 14,249 (25.4) | <0.001 |
| Individual-level variables | |||||||||
| Year of HIV diagnosis | |||||||||
| 2000–2004 | 1852 (41.2) | 216 (30.8) | 122 (46.0) | 30 (42.9) | 52 (42.6) | 8215 (36.7) | 4641 (33.5) | 5114 (35.9) | <0.001 |
| 2005–2009 | 1401 (32.2) | 264 (37.7) | 80 (30.2) | 26 (37.1) | 43 (35.2) | 7532 (33.7) | 4689 (33.8) | 5001 (35.1) | |
| 2010–2014 | 1238 (27.6) | 221 (31.5) | 63 (23.8) | 14 (20.0) | 27 (22.1) | 6615 (29.6) | 4529 (32.7) | 4134 (29.0) | |
| Sex at birth | |||||||||
| Female | 2225 (49.5) | 289 (41.2) | 141 (53.2) | 27 (38.6) | 47 (38.5) | 9399 (42.0) | 2466 (17.8) | 2289 (16.1) | <0.001 |
| Male | 2266 (50.5) | 412 (58.8) | 124 (46.8) | 43 (61.4) | 75 (61.5) | 12,963 (58.0) | 11,393 (82.2) | 11,960 (83.9) | |
| Age group at diagnosis | |||||||||
| 13–24 years | 306 (6.8) | 78 (11.1) | 42 (15.9) | 5 (7.1) | 9 (7.4) | 5178 (23.2) | 1775 (12.8) | 1291 (9.1) | <0.001 |
| 25–49 years | 3078 (68.5) | 470 (67.1) | 195 (73.6) | 51 (72.9) | 88 (72.1) | 14,018 (62.7) | 10,291 (74.3) | 10,340 (72.6) | |
| ≥50 years | 1107 (24.7) | 153 (21.8) | 28 (10.6) | 14 (20.0) | 25 (20.5) | 3166 (14.2) | 1793 (12.9) | 2618 (18.4) | |
| Mode of transmission | |||||||||
| IDU c | 78 (1.7) | 26 (3.7) | 11 (4.2) | 0 (0) | 9 (7.4) | 1875 (8.4) | 923 (6.7) | 1401 (9.8) | <0.001 |
| MSM | 432 (9.6) | 143 (20.4) | 56 (21.1) | 23 (32.9) | 26 (21.3) | 6883 (30.8) | 8408 (60.7) | 9747 (68.4) | |
| Heterosexual | 3350 (74.6) | 446 (63.6) | 158 (59.6) | 13 (18.6) | 71 (58.2) | 11772 (52.6) | 3366 (24.3) | 2250 (15.8) | |
| Other/unknown | 631 (14.1) | 86 (12.3) | 40 (15.9) | 34 (48.6) | 16 (13.1) | 1832 (8.2) | 1162 (8.4) | 851 (6.0) | |
| AIDS defining illness by 2015 | |||||||||
| 2505 (55.8) | 348 (49.6) | 143 (54.0) | 27 (38.6) | 65 (53.3) | 11137 (49.8) | 5915 (42.7) | 14,249 (25.4) | <0.001 | |
| ZIP code tabulation area-level variables | |||||||||
| Socioeconomic status (SES) index, quartiles | |||||||||
| 1 (lowest SES) | 2396 (55.3) | 294 (43.8) | 127 (49.6) | 29 (43.9) | 59 (50.4) | 12,556 (58.1) | 5094 (38.3) | 3056 (22.2) | <0.001 |
| 2 | 1254 (29.0) | 202 (30.1) | 75 (29.3) | 23 (34.9) | 24 (20.5) | 5342 (24.7) | 3113 (23.4) | 3664 (26.7) | |
| 3 | 464 (10.7) | 106 (15.8) | 39 (15.2) | 13 (19.7) | 23 (19.7) | 2448 (11.3) | 3375 (25.4) | 4061 (29.5) | |
| 4 (highest SES) | 216 (5.0) | 70 (10.4) | 15 (5.9) | 1 (1.5) | 11 (9.4) | 1266 (5.9) | 1720 (12.9) | 2970 (21.6) | |
| Rural Urban Commuting Area classification | |||||||||
| Urban | 4300 (95.8) | 664 (94.7) | 256 (96.6) | 66 (94.3) | 114 (93.4) | 20,948 (93.7) | 13,094 (94.5) | 13,223 (92.8) | <0.001 |
| Rural | 191 (4.3) | 37 (5.3) | 9 (3.4) | 4 (5.7) | 8 (6.6) | 1414 (6.3) | 765 (5.5) | 1026 (7.2) | |
| US Born Blacks | Hispanics | Non-Hispanic Whites | |
|---|---|---|---|
| Referent Group | Referent Group | Referent Group | |
| Country/region of birth | Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) |
| Bahamas | 2.49 (1.91–3.23) ** | 2.69 (2.07–3.50) ** | 3.13 (2.40–4.10) ** |
| Haiti | 1.21 (1.12–1.30) ** | 1.31 (1.20–1.42) ** | 1.52 (1.40–1.66) ** |
| Jamaica | 0.89 (0.75–1.06) | 0.97 (0.81–1.16) | 1.13 (0.94–1.34) |
| Trinidad and Tobago | 1.83 (1.10–3.04) ** | 1.98 (1.19–3.30) ** | 2.30 (1.38–3.83) ** |
| Other Caribbean | 1.52 (1.04–2.23) | 1.65 (1.12–2.42) ** | 1.92 (1.31–2.81) ** |
| Bahamas | Haiti | Jamaica | |
|---|---|---|---|
| aOR, (95% CI) | aOR, (95% CI) | aOR, (95% CI) | |
| Individual-level variables | |||
| Year of HIV Diagnosis | |||
| 2000–2004 | 3.02 (1.42–6.44) ** | 1.90 (1.60–2.25) ** | 1.67 (1.05–2.65) ** |
| 2005–2009 | 2.14 (0.98–4.69) * | 1.44 (1.20–1.72) ** | 1.60 (1.04–2.46) ** |
| 2010–2014 | Referent | Referent | Referent |
| Sex at birth | |||
| Male | 1.10 (0.54–2.27) | 1.46 (1.27–1.68) ** | 2.28 (1.50–3.48) ** |
| Female | Referent | Referent | Referent |
| Age at HIV diagnosis | |||
| 25–49 years | 1.07 (0.47–2.42) | 0.91 (0.69–1.18) * | 0.39 (0.23–0.68) ** |
| ≥50 years | 0.49 (0.16–1.56) | 0.87 (0.66–1.17) | 0.25 (0.13–0.49) ** |
| 13–24 years | Referent | Referent | Referent |
| HIV transmission mode | |||
| IDU a | 1.63 (0.38–6.98) | 1.04 (0.63–1.72) | 1.76 (0.71–4.37) |
| MSM | 1.11 (0.46–2.64) | 76 (0.60–0.97) ** | 79 (0.47–1.30) |
| Other/unknown | 4.62 (1.78–12.18) ** | 3.46 (2.82–4.21) ** | 2.18 (1.28–3.71) ** |
| Heterosexual | Referent | Referent | Referent |
| AIDS diagnosis | |||
| No AIDS diagnosis by 2015 | 2.80 (1.49–5.25) ** | 3.24 (2.82–3.72) ** | 2.84 (1.95–4.12) ** |
| Neighborhood-level variables | |||
| Socio economic status | |||
| 1 (lowest SES) | 0.80 (0.23–2.81) | .89 (0.65–1.23) | 1.56 (0.83–2.92) |
| 2 | 0.50 (0.14–1.84) | .85 (0.61–1.18) | 1.42 (0.74–2.72) |
| 3 | 0.54 (0.14–2.18) | 1.05 (0.73–1.51) | 1.67 (0.82–3.42) |
| 4 (highest SES) | Referent | Referent | Referent |
| Rural vs. Urban | |||
| Rural | - | 0.21 (0.05–0.85) * | - |
| US Blacks | Hispanics | Non-Hispanic Whites | |
|---|---|---|---|
| Referent Group | Referent Group | Referent Group | |
| Country/region of birth | Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) |
| Bahamas | 2.07 (1.59–2.69) ** | 2.70 (2.07–3.51) ** | 3.23 (2.48–4.21) ** |
| Haiti | 1.17 (1.09–1.26) ** | 1.52 (1.40–1.65) ** | 1.82 (1.68–1.98) ** |
| Jamaica | 0.83 (0.70–0.97) ** | 1.07 (0.91–1.27) | 1.29 (1.09–1.52) ** |
| Trinidad and Tobago | 1.13 (0.68–1.86) | 1.47 (0.89–2.42) | 1.76 (1.06–2.90) ** |
| Other Caribbean | 1.30 (.89–1.89) | 1.69 (1.16–2.46) | 2.02 (1.39–2.95) ** |
| Bahamas | Haiti | Jamaica | |
|---|---|---|---|
| aOR, (95% CI) | aOR, (95% CI) | aOR, (95% CI) | |
| Individual-level variables | |||
| Year of HIV Diagnosis | |||
| 2000–2004 | 2.26 (1.07–4.75) ** | 1.65 (1.40–1.93) ** | 1.40 (0.91–2.17) |
| 2005–2009 | 2.13 (0.98–4.65) | 1.42 (1.20–1.67) ** | 1.89 (1.26–2.84) ** |
| 2010–2014 | Referent | Referent | Referent |
| Sex at birth | |||
| Male | 1.00 (0.48–2.06) | 1.33 (1.16–1.52) * | 2.37 (1.60–3.52) ** |
| Female | Referent | Referent | Referent |
| Age at HIV diagnosis | |||
| 25–49 years | 1.28 (0.56–2.88) | 0.78 (0.60–1.00) * | 0.46 (0.27–0.78) ** |
| ≥50 years | 0.55 (0.17–1.73) | 0.78 (0.59–1.03) * | 0.29 (0.16–0.56) ** |
| 13–24 years | Referent | Referent | Referent |
| HIV transmission mode | |||
| IDU | 2.18 (0.48–9.93) | 0.84 (0.52–1.36) | 1.96 (0.79–4.84) |
| MSM | 1.16 (0.48–2.76) | 0.76 (0.61–0.96) * | 0.69 (0.43–1.11) |
| Other/unknown | 7.42 (2.25–22.44) ** | 2.51 (2.07–3.06) ** | 1.36 (0.81–2.84) |
| Heterosexual | Referent | Referent | Referent |
| AIDS Diagnosis | |||
| No AIDS Diagnosis by 2015 | 2.59 (1.37–4.89) ** | 2.17 (1.91–2.48) ** | 1.96 (1.38–2.77) ** |
| Neighborhood-level variables | |||
| Socio economic status | |||
| 1 (lowest SES) | 0.80 (0.23–2.78) | 0.88 (0.65–1.20) | 1.57 (0.87–2.84) |
| 2 | 0.45 (0.12–1.63) | 0.83 (0.61–1.14) | 1.34 (0.73–2.44) |
| 3 | 0.70 (0.18–2.78) | 1.01 (0.72–1.44) | 1.45 (0.74–2.83) |
| 4 (highest SES) | Referent | Referent | Referent |
| Rural vs. Urban | |||
| Rural | - | 0.21 (0.06–0.78) * | - |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cyrus, E.; Dawson, C.; Fennie, K.P.; Sheehan, D.M.; Mauck, D.E.; Sanchez, M.; Maddox, L.M.; Trepka, M.J. Disparity in Retention in Care and Viral Suppression for Black Caribbean-Born Immigrants Living with HIV in Florida. Int. J. Environ. Res. Public Health 2017, 14, 285. https://doi.org/10.3390/ijerph14030285
Cyrus E, Dawson C, Fennie KP, Sheehan DM, Mauck DE, Sanchez M, Maddox LM, Trepka MJ. Disparity in Retention in Care and Viral Suppression for Black Caribbean-Born Immigrants Living with HIV in Florida. International Journal of Environmental Research and Public Health. 2017; 14(3):285. https://doi.org/10.3390/ijerph14030285
Chicago/Turabian StyleCyrus, Elena, Christyl Dawson, Kristopher P. Fennie, Diana M. Sheehan, Daniel E. Mauck, Mariana Sanchez, Lorene M. Maddox, and Mary Jo Trepka. 2017. "Disparity in Retention in Care and Viral Suppression for Black Caribbean-Born Immigrants Living with HIV in Florida" International Journal of Environmental Research and Public Health 14, no. 3: 285. https://doi.org/10.3390/ijerph14030285
APA StyleCyrus, E., Dawson, C., Fennie, K. P., Sheehan, D. M., Mauck, D. E., Sanchez, M., Maddox, L. M., & Trepka, M. J. (2017). Disparity in Retention in Care and Viral Suppression for Black Caribbean-Born Immigrants Living with HIV in Florida. International Journal of Environmental Research and Public Health, 14(3), 285. https://doi.org/10.3390/ijerph14030285






