The Development of Psychiatric Services Providing an Alternative to Full-Time Hospitalization Is Associated with Shorter Length of Stay in French Public Psychiatry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
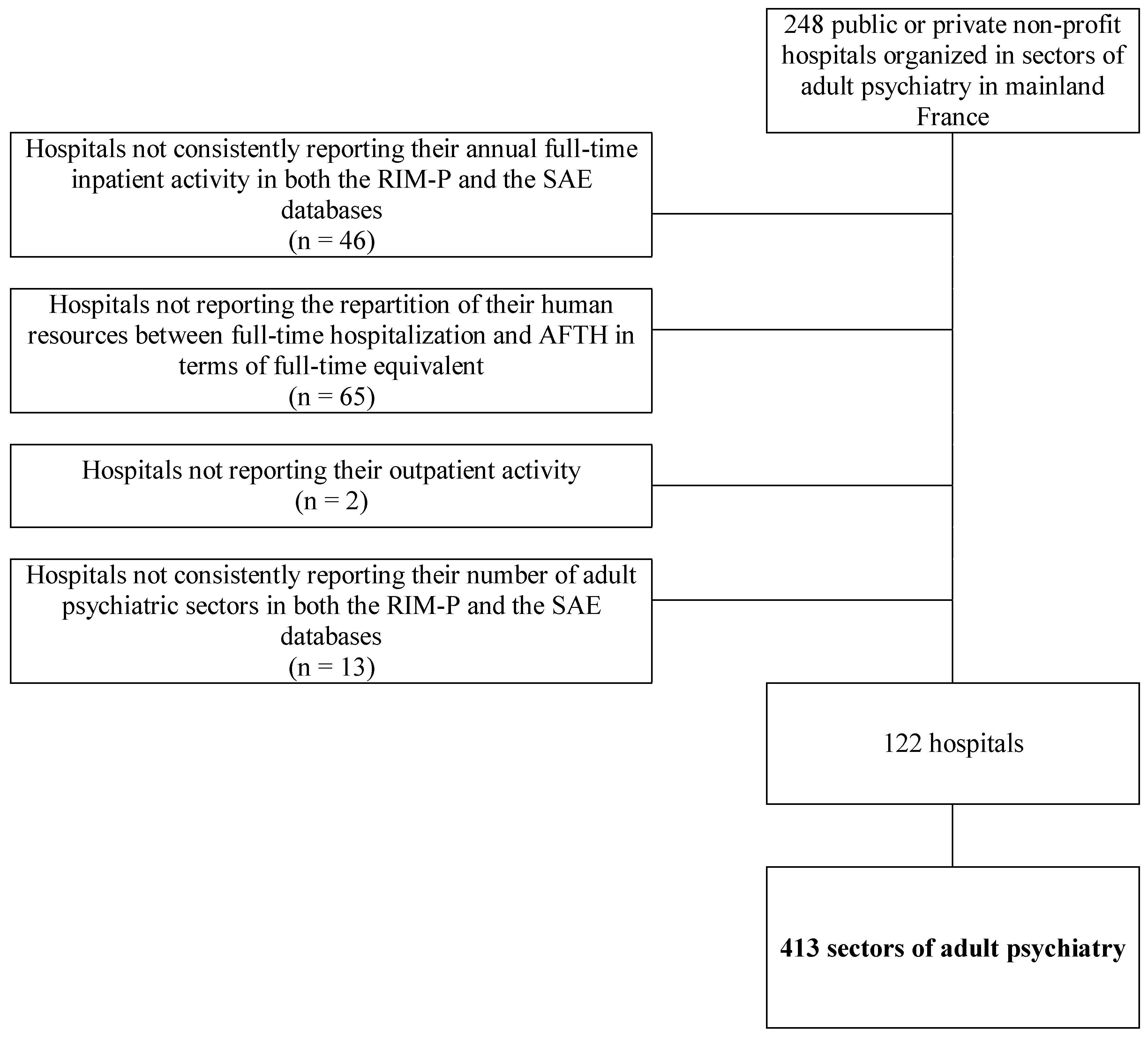
2.2. Study Population
2.3. Development of AFTH
2.4. LOS in Full-Time Hospitalization
2.5. Factors Potentially Associated with the LOS in Full-Time Hospitalization
2.6. Analysis
2.6.1. Descriptive Analysis
2.6.2. Multivariate Analysis
3. Results
3.1. Setting
3.2. Descriptive Analysis
3.3. Multivariate Analysis
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Mental Health—Facing the Challenges, Building Solutions report from the WHO European Ministerial Conference; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Murray, C.J.; Lopez, A.D. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet Lond. Engl. 1997, 349, 1498–1504. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- World Health Organization. WHO Estimates for 2000–2012. Available online: http://www.who.int/healthinfo/global_burden_disease/estimates/en/ (accessed on 18 August 2016).
- Cuerq, A.; Païta, M.; Ricordeau, P. Les causes médicales de l’invalidité en 2006. Points Repère 2008, 16, 5. [Google Scholar]
- Organization for Economic Co-Operation and Development. “Suicide” in Health at a Glance 2011: OECD Indicators; Organisation for Economic Co-Operation and Development: Paris, France, 2011. [Google Scholar]
- Assurance Maladie Analyse Médicalisée des Dépenses de Santé. Available online: http://www.ameli.fr/espace-presse/communiques-et-dossiers-de-presse/les-derniers-communiques-de-la-caisse-nationale/detail-d-un-communique/2515.php (accessed on 18 March 2016).
- Chevreul, K.; Prigent, A.; Bourmaud, A.; Leboyer, M.; Durand-Zaleski, I. The cost of mental disorders in France. Eur. Neuropsychopharmacol. 2013, 23, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Mental Health Policy Implementation Guide: Adult Acute Inpatient Care Provision; Department of Health: London, UK, 2002. [Google Scholar]
- Evans, J.; Rose, D.; Flach, C.; Csipke, E.; Glossop, H.; McCrone, P.; Craig, T.; Wykes, T. VOICE: Developing a new measure of service users’ perceptions of inpatient care, using a participatory methodology. J. Ment. Health Abingdon Engl. 2012, 21, 57–71. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2001: Mental Health: New Understanding, New Hope; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- World Health Organization. Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- World Health Organization. WHO Quality Rights Tool Kit. Assessing and Improving Quality and Human Rights in Mental Health and Social Care Facilities; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Organisation for Economic Co-Operation and Development. Health at a Glance 2013. OECD Indicators; Organisation for Economic Co-Operation and Development: Paris, France, 2013. [Google Scholar]
- Jacobs, R.; Barrenho, E. Impact of crisis resolution and home treatment teams on psychiatric admissions in England. Br. J. Psychiatry J. Ment. Sci. 2011, 199, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Bourgon, J.; Salvador-Carulla, L.; Vázquez-Barquero, J.L. Community alternatives to acute inpatient care for severe psychiatric patients. Acta Esp. Psiquiatr. 2012, 40, 323–332. [Google Scholar]
- Becker, I.; Vázquez-Barquero, J.L. The European perspective of psychiatric reform. Acta Psychiatr. Scand. Suppl. 2001, 104, 8–14. [Google Scholar] [CrossRef]
- World Health Organization. The European Mental Health Action Plan 2013–2020; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Taylor Salisbury, T.; Killaspy, H.; King, M. An international comparison of the deinstitutionalisation of mental health care: Development and findings of the Mental Health Services Deinstitutionalisation Measure (MENDit). BMC Psychiatry 2016, 16, 54. [Google Scholar] [CrossRef] [PubMed]
- Ministère du Travail, de L’emploi et de la Santé. Plan Psychiatrie et Santé Mentale 2011–2015; Ministère du Travail, de L’emploi et de la Santé: Paris, France, 2012.
- Cour des Comptes. L’organisation des Soins Psychiatriques, les Effets du Plan “Psychiatrie et Santé Mentale” (2005–2010); Cour des Comptes: Paris, France, 2011. [Google Scholar]
- National Institute for Clinical Excellence. Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Primary and Secondary Care. Clinical Guideline 1; National Institute for Clinical Excellence: Leicester, UK, 2002. [Google Scholar]
- World Health Organization. Mental Health Policy and Service Guidance Package—Mental Health Legislation and Human Rights; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- World Health Organization. World Health Organization Assessment Instrument for Mental Health Systems. WHO-AIMS Version 2.2; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Thomas, J.W.; Guire, K.E.; Horvat, G.G. Is patient length of stay related to quality of care? Hosp. Health Serv. Adm. 1997, 42, 489–507. [Google Scholar] [PubMed]
- Quirk, A.; Lelliott, P. What do we know about life on acute psychiatric wards in the UK? A review of the research evidence. Soc. Sci. Med. 1982 2001, 53, 1565–1574. [Google Scholar]
- Creed, F.; Black, D.; Anthony, P.; Osborn, M.; Thomas, P.; Tomenson, B. Randomised controlled trial of day patient versus inpatient psychiatric treatment. BMJ 1990, 300, 1033–1037. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Needle, J.; Bindman, J.; Thornicroft, G. Crisis Resolution and Home Treatment in Mental Health; Cambridge University Press: New York, NY, USA, 2008. [Google Scholar]
- Ryu, Y.; Mizuno, M.; Sakuma, K.; Munakata, S.; Takebayashi, T.; Murakami, M.; Falloon, I.R.H.; Kashima, H. Deinstitutionalization of long-stay patients with schizophrenia: The 2-year social and clinical outcome of a comprehensive intervention program in Japan. Aust. N. Z. J. Psychiatry 2006, 40, 462–470. [Google Scholar] [PubMed]
- Schene, A.H.; van Wijngaarden, B.; Poelijoe, N.W.; Gersons, B.P. The Utrecht comparative study on psychiatric day treatment and inpatient treatment. Acta Psychiatr. Scand. 1993, 87, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, V.; Tehranidoost, M.; Yunesian, M.; Amini, H.; Mohammadi, M.; Jalali Roudsari, M. Effectiveness of a low-intensity home-based aftercare for patients with severe mental disorders: A 12-month randomized controlled study. Community Ment. Health J. 2012, 48, 766–770. [Google Scholar] [PubMed]
- Killaspy, H.; Johnson, S.; King, M.; Bebbington, P. Developing mental health services in response to research evidence. Epidemiol. Psichiatr. Soc. 2008, 17, 47–56. [Google Scholar] [PubMed]
- Marshall, M.; Crowther, R.; Almaraz-Serrano, A.; Creed, F.; Sledge, W.; Kluiter, H.; Roberts, C.; Hill, E.; Wiersma, D. Day hospital versus admission for acute psychiatric disorders. Cochrane Database Syst. Rev. 2003, CD004026. [Google Scholar] [CrossRef] [Green Version]
- Wennberg, J. Time to tackle unwarranted variations in practice. BMJ 2011, 342, d1513. [Google Scholar] [CrossRef]
- Wennberg, J.; Fisher, E.S.; Skinner, J.S. Geography and the debate over Medicare reform. Health Aff. Proj. Hope 2002, 36, W96–W114. [Google Scholar]
- Mattioni, T.; Di Lallo, D.; Roberti, R.; Miceli, M.; Stefani, M.; Maci, C.; Perucci, C.A. Determinants of psychiatric inpatient admission to general hospital psychiatric wards: An epidemiological study in a region of central Italy. Soc. Psychiatry Psychiatr. Epidemiol. 1999, 34, 425–431. [Google Scholar] [PubMed]
- Lloyd-Evans, B.; Slade, M.; Jagielska, D.; Johnson, S. Residential alternatives to acute psychiatric hospital admission: Systematic review. Br. J. Psychiatry J. Ment. Sci. 2009, 195, 109–117. [Google Scholar]
- Tulloch, A.; Fearon, P.; David, A.S. Length of stay of general psychiatric inpatients in the United States: Systematic review. Adm. Policy Ment. Health 2011, 38, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Harvey, C.; Andrew, C. Factors associated with length of stay and the risk of readmission in an acute psychiatric inpatient facility: A retrospective study. Aust. N. Z. J. Psychiatry 2011, 45, 578–585. [Google Scholar] [PubMed]
- Oiesvold, T.; Saarento, O.; Sytema, S.; Christiansen, L.; Göstas, G.; Lönnerberg, O.; Muus, S.; Sandlund, M.; Hansson, L. The Nordic Comparative Study on Sectorized Psychiatry—Length of in-patient stay. Acta Psychiatr. Scand. 1999, 100, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Gutacker, N.; Mason, A.; Goddard, M.; Gravelle, H.; Kendrick, T.; Gilbody, S. Determinants of hospital length of stay for people with serious mental illness in England and implications for payment systems: A regression analysis. BMC Health Serv. Res. 2015, 15, 439. [Google Scholar] [CrossRef] [PubMed]
- Pertile, R.; Donisi, V.; Grigoletti, L.; Angelozzi, A.; Zamengo, G.; Zulian, G.; Amaddeo, F. DRGs and other patient-, service- and area-level factors influencing length of stay in acute psychiatric wards: The Veneto Region experience. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, M.; Niimura, J.; Tanoue, M.; Yamamura, M.; Hirata, T.; Asukai, N. Association between length of hospital stay and implementation of discharge planning in acute psychiatric inpatients in Japan. Int. J. Ment. Health Syst. 2015, 9, 23. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.; Chang, H.-S.; Oh, S.-M.; Yoon, C.-W. Factors associated with long-stay status in patients with schizophrenia: An analysis of national databases covering the entire Korean population. Int. J. Soc. Psychiatry 2013, 59, 207–216. [Google Scholar] [CrossRef] [PubMed]
- ATIH Base Nationale RIM-P. Available online: http://www.atih.sante.fr/base-nationale-rim-p (accessed on 5 December 2016).
- Ministry of Health SAE. Available online: https://www.sae-diffusion.sante.gouv.fr/sae-diffusion/recherche.htm (accessed on 6 February 2017).
- World Health Organization ICD-10 Version 2010. Available online: http://apps.who.int/classifications/icd10/browse/2010/en (accessed on 18 March 2016).
- Haro, J.M.; Ayuso-Mateos, J.L.; Bitter, I.; Demotes-Mainard, J.; Leboyer, M.; Lewis, S.W.; Linszen, D.; Maj, M.; McDaid, D.; Meyer-Lindenberg, A.; et al. ROAMER: Roadmap for mental health research in Europe. Int. J. Methods Psychiatr. Res. 2014, 23 (Suppl. 1), 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prigent, A.; Auraaen, A.; Kamendje-Tchokobou, B.; Durand-Zaleski, I.; Chevreul, K. Health-related quality of life and utility scores in people with mental disorders: A comparison with the non-mentally ill general population. Int. J. Environ. Res. Public Health 2014, 11, 2804–2817. [Google Scholar] [CrossRef] [PubMed]
- Graf von der Schulenburg, J.M. The Influence of Economic Evaluation Studies on Health Care Decision Making: A European Survey; IOS Press: Amsterdam, The Netherlands, 2000. [Google Scholar]
- Thampi, N.; Showler, A.; Burry, L.; Bai, A.D.; Steinberg, M.; Ricciuto, D.R.; Bell, C.M.; Morris, A.M. Multicenter study of health care cost of patients admitted to hospital with Staphylococcus aureus bacteremia: Impact of length of stay and intensity of care. Am. J. Infect. Control 2015, 43, 739–744. [Google Scholar] [CrossRef] [PubMed]
- Ezenduka, C.; Ichoku, H.; Ochonma, O. Estimating the costs of psychiatric hospital services at a public health facility in Nigeria. J. Ment. Health Policy Econ. 2012, 15, 139–148. [Google Scholar] [PubMed]
- Wolff, J.; McCrone, P.; Berger, M.; Patel, A.; Ackermann, C.; Gerhardt, K.; Normann, C. A work time study analysing differences in resource use between psychiatric inpatients. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1309–1315. [Google Scholar] [CrossRef] [PubMed]
- Cromwell, J.; Maier, J.; Gage, B.; Drozd, E.; Osber, D.; Richter, E.; Greenwald, L.; Goldman, H. Characteristics of High Staff Intensive Medicare Psychiatric Inpatients. Health Care Financ. Rev. 2004, 26, 103. [Google Scholar] [PubMed]
- Chung, W.; Cho, W.H.; Yoon, C.W. The influence of institutional characteristics on length of stay for psychiatric patients: A national database study in South Korea. Soc. Sci. Med. 1982 2009, 68, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.M. Generalized anxiety disorder and psychiatric comorbidities such as depression, bipolar disorder, and substance abuse. J. Clin. Psychiatry 2009, 70 (Suppl. 2), 10–14. [Google Scholar] [CrossRef] [PubMed]
- Buckley, P.F.; Miller, B.J.; Lehrer, D.S.; Castle, D.J. Psychiatric comorbidities and schizophrenia. Schizophr. Bull. 2009, 35, 383–402. [Google Scholar] [CrossRef] [PubMed]
- Rey, G.; Jougla, E.; Fouillet, A.; Hémon, D. Ecological association between a deprivation index and mortality in France over the period 1997–2001: Variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 2009, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Windenberger, F.; Rican, S.; Jougla, E.; Rey, G. Spatiotemporal association between deprivation and mortality: Trends in France during the nineties. Eur. J. Public Health 2012, 22, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Westert, G.P.; Groenewegen, P.P.; Boshuizen, H.C.; Spreeuwenberg, P.M.M.; Steultjens, M.P.M. Medical practice variations in hospital care; time trends of a spatial phenomenon. Health Place 2004, 10, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Insee Base Permanente des Équipements. Available online: https://www.data.gouv.fr/fr/datasets/base-permanente-des-equipements-1/ (accessed on 2 August 2016).
- Insee Définitions, Méthodes et Qualité—Base des Unités Urbaines 2010. Available online: http://www.insee.fr/fr/methodes/default.asp?page=zonages/unites_urbaines.htm (accessed on 2 August 2016).
- CépiDc Causes de Mortalité. Available online: http://www.cepidc.inserm.fr/inserm/html/index2.htm (accessed on 26 January 2015).
- Irdes Bases de Données Eco-Santé en Ligne. France, Régions & Départements, Québec. Available online: http://www.ecosante.fr/ (accessed on 12 February 2014).
- Insee Bases de Données—Les Résultats des Recensements de la Population. Available online: http://www.insee.fr/fr/bases-de-donnees/default.asp?page=recensements.htm (accessed on 2 August 2016).
- Abdi, H. Coefficient of variation. In Encyclopedia of Research Design; Salkind, N., Ed.; SAGE: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Organisation for Economic Co-Operation and Development. Geographic Variations in Health Care. What Do We Know and What Can Be Done to Improve Health System Performance? OECD Health Policy Studies, OECD Publishing: Paris, France, 2014. [Google Scholar]
- Bristol University | Centre for Multilevel Modelling | Multilevel Structures and Classifications. Available online: http://www.bristol.ac.uk/cmm/learning/multilevel-models/data-structures.html (accessed on 16 January 2016).
- Kreft, I. Are Multilevel Techniques Necessary? An Overview, Including Simulation Studies; California State University Press: Long Beach, CA, USA, 1996. [Google Scholar]
- Hox, J. Multilevel Modeling: When and Why. Classification, Data Analysis, and Data Highways; Springer: Berlin/Heidelberg, Germany, 1998. [Google Scholar]
- Maas, C.J.M.; Hox, J.J. Robustness issues in multilevel regression analysis. Stat. Neerlandica 2004, 58, 127–137. [Google Scholar] [CrossRef]
- Maas, C.J.M.; Hox, J.J. Sufficent sample sizes for multilevel modeling. Methodology 2005, 1, 86–92. [Google Scholar] [CrossRef]
- Clarke, P. When can group level clustering be ignored? Multilevel models versus single-level models with sparse data. J. Epidemiol. Community Health 2008, 62, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Bell, B.; Morgan, G.; Schoeneberger, J.; Loudermilk, B.; Kromrey, J.; Ferron, J. Dancing the sample size limbo with mixed models: How low can you go? SAS Glob. Forum 2010 2010, 197, 1–11. [Google Scholar]
- Ivert, A.-K.; Torstensson Levander, M.; Merlo, J. Adolescents’ utilisation of psychiatric care, neighbourhoods and neighbourhood socioeconomic deprivation: A multilevel analysis. PLoS ONE 2013, 8, e81127. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, M.; Kim, H.; Lee, K.; Chang, S.; Kim, V.; Myong, J.P.; Jeon, S. Factors affecting diabetic screening behavior of Korean adults: A multilevel analysis. Asian Nurs. Res. 2013, 7, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Yang, J. Interpreting Coefficients in Regression with Log-Transformed Variables; Cornell University: Ithaca, NY, USA, 2012. [Google Scholar]
- Fortney, J.C.; Booth, B.M.; Smith, G.R. Variation among VA hospitals in length of stay for treatment of depression. Psychiatr. Serv. 1996, 47, 608–613. [Google Scholar] [PubMed]
- Lee, S.; Rothbard, A.B.; Noll, E.L. Length of Inpatient Stay of Persons with Serious Mental Illness: Effects of Hospital and Regional Characteristics. Psychiatr. Serv. 2012, 63, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Harman, J.S.; Cuffel, B.J.; Kelleher, K.J. Profiling hospitals for length of stay for treatment of psychiatric disorders. J. Behav. Health Serv. Res. 2004, 31, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, S.; Warren Salmon, J.; Kong, S.; Zhao, S. Administrative databases and outcomes assessment: An overview of issues and potential utility. J. Manag. Care Spec. Pharm. 1999, 215–222. [Google Scholar] [CrossRef]
- Coldefy, M.; Nestrigue, C.; Zeynep, O. Etude de Faisabilité sur la Diversité des Pratiques en Psychiatrie; Institut de Recherche et Documentation en Economie de la Santé: Paris, France, 2012. [Google Scholar]
- Byrne, S.L.; Hooke, G.R.; Page, A.C. Readmission: A useful indicator of the quality of inpatient psychiatric care. J. Affect. Disord. 2010, 126, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; McKevitt, C.; Rudd, A.G.; Wolfe, C.D.A. Socioeconomic deprivation and survival after stroke: Findings from the prospective South London Stroke Register of 1995 to 2011. Stroke 2014, 45, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kroll, M.E.; Stiller, C.A.; Richards, S.; Mitchell, C.; Carpenter, L.M. Evidence for under-diagnosis of childhood acute lymphoblastic leukaemia in poorer communities within Great Britain. Br. J. Cancer 2012, 106, 1556–1559. [Google Scholar] [CrossRef] [PubMed]
- Toor, I.S.; Jaumdally, R.; Lip, G.Y.H.; Pagano, D.; Dimitri, W.; Millane, T.; Varma, C. Differences between South Asians and White Europeans in five year outcome following percutaneous coronary intervention. Int. J. Clin. Pract. 2011, 65, 1259–1266. [Google Scholar] [CrossRef] [PubMed]
- Le Breton, J.; Journy, N.; Attali, C.; Le Corvoisier, P.; Brixi, Z.; Bastuji-Garin, S.; Chevreul, K. Improving participation in colorectal cancer screening: Targets for action. Prev. Med. 2012, 55, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Ligier, K.; Dejardin, O.; Launay, L.; Benoit, E.; Babin, E.; Bara, S.; Lapôtre-Ledoux, B.; Launoy, G.; Guizard, A.-V. Health professionals and the early detection of head and neck cancers: A population-based study in a high incidence area. BMC Cancer 2016, 16, 456. [Google Scholar]
- Bryere, J.; Dejardin, O.; Launay, L.; Colonna, M.; Grosclaude, P.; Launoy, G.; French Network of Cancer Registries (FRANCIM). Socioeconomic status and site-specific cancer incidence, a Bayesian approach in a French Cancer Registries Network study. Eur. J. Cancer Prev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Haut Conseil de la Santé Publique. Indicateurs de Suivi des Inégalités Sociales de Santé; Haut Conseil de la Santé Publique: Paris, France, 2013. [Google Scholar]
- Fernandez, A.; Gillespie, J.A.; Smith-Merry, J.; Feng, X.; Astell-Burt, T.; Maas, C.; Salvador-Carulla, L. Integrated mental health atlas of the Western Sydney Local Health District: Gaps and recommendations. Aust. Health Rev. Publ. Aust. Hosp. Assoc. 2016. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, A.; Salinas-Perez, J.A.; Gutierrez-Colosia, M.R.; Prat-Pubill, B.; Serrano-Blanco, A.; Molina, C.; Jorda, E.; Garcia-Alonso, C.R.; Salvador-Carulla, L. Use of an integrated Atlas of Mental Health Care for evidence informed policy in Catalonia (Spain). Epidemiol. Psychiatr. Sci. 2015, 24, 512–524. [Google Scholar] [CrossRef] [PubMed]
| Diagnostic Group | ICD-10 Wording | ICD-10 Code(s) |
|---|---|---|
| Addictions | Mental and behavioural disorders due to psychoactive substance abuse | F10-F19 |
| Schizophrenia | Schizophrenia | F20 |
| Other psychotic disorders | Schizotypal and delusional disorders | F21-F29 |
| Bipolar disorders | Bipolar affective disorders | F31 |
| Other mood disorders | Mood (affective) disorders (except bipolar affective disorder) | F30, F32, F33, F34, F38, F39 |
| Anxiety disorders | Neurotic, stress-related and somatoform disorders | F40-F48 |
| Other mental or behavioural disorders | Behavioural syndromes associated with physiological disturbances and physical factors | F50-F59 |
| Disorders of adult personality and behaviour | F60-F69 | |
| Pervasive developmental disorders | F84 | |
| Behavioural and emotional disorders with onset usually occurring in childhood and adolescence | F90-F98 | |
| Unspecified mental disorder | F99 |
| Mean (Standard Deviation) | Median (Interquartile Range) | Range | CV (%) | Ratio 90/10th Percentiles | |
|---|---|---|---|---|---|
| Mean LOS by sector (n = 413), days | 36.05 (22.30) | 30.91 (18.37) | 236.91 | 61.86 | 3.31 |
| Development of AFTH by hospital hosting each sector (n = 122), ratio of FTEs | 0.34 (0.11) | 0.35 (0.13) | 0.58 | 32.72 | 2.50 |
| Patient characteristics | Demographic characteristics | Age |
| Sex | ||
| Clinical characteristics | Presence of each diagnostic group | |
| Socio-economic characteristics | Deprivation index | |
| Psychiatric sector characteristics | Case-mix characteristics of patients seen in full-time hospitalization in the sector | Mean age |
| % of patients with anxiety disorders | ||
| % of patients with bipolar disorders | ||
| Institutional characteristics of the hospital hosting each sector | Legal status of the hospital | |
| Specialization in psychiatry | ||
| Participation to teaching activities | ||
| Participation to emergency care | ||
| Organizational characteristics of the hospital hosting each sector | Nb. of inpatient beds per 1000 inh. * | |
| Environmental characteristics | Overall health status of the population (variables computed per 1000 inhabitants of a sector catchment area) | Acute admission rate for somatic disorders |
| Mortality rate | ||
| Suicide rate | ||
| Nb. of individuals suffering from long-duration diseases | ||
| % of individuals suffering from psychiatric long-duration diseases among people suffering from long-duration diseases | ||
| Inpatient psychiatric admission rate | ||
| Availability of medical and social care (variables computed per 1000 inhabitants of a sector catchment area) | Nb. of general practitioners | |
| Nb. of community-based private psychiatrists | ||
| Nb. of psychologists | ||
| Nb. of non-psychiatric inpatient beds | ||
| Nb. of inpatient beds of private psychiatry | ||
| Capacity of housing institutions for disabled individuals | ||
| Capacity of centres providing care through employment | ||
| Capacity of housing and social rehabilitation centres | ||
| Other | Level of urbanization |
| Model 1 (Null Model with No Explanatory Variables) | Model 2 (Model with Individual Patients’ Characteristics) | Model 3 (Model with Individual Patients’ Characteristics and Sectors Characteristics) | |
|---|---|---|---|
| Inter-sectors variance (p-value) | 0.2176 (<0.0001) | 0.1466 (<0.0001) | 0.1192 (<0.0001) |
| Standard error | 0.0147 | 0.0101 | 0.0084 |
| ICC (%) | 13.4106 | 10.3685 | 8.5972 |
| Δ variance (%) | - | 32.6287 | 18.6903 |
| Variable | Modality for Categorical Variable | Estimated Value of the Coefficient | Standard Error | p-Value (in Bold When Significant) |
|---|---|---|---|---|
| Intercept | - | 0.7418 | 0.4377 | 0.0907 |
| Explanatory variables introduced at the patient level (level 1) | ||||
| Age | - | 0.0077 | 0.0002 | <0.0001 |
| Diagnosis of anxiety disorder | 1 | −0.2058 | 0.0088 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of schizophrenia | 1 | 0.1590 | 0.0089 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of other psychotic disorder | 1 | 0.2109 | 0.0090 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of other mental or behavioural disorder | 1 | −0.0650 | 0.0089 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of addictive disorder | 1 | −0.0488 | 0.0092 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of bipolar disorder | 1 | 0.1957 | 0.0109 | <0.0001 |
| 0 | 0.0000 | |||
| Diagnosis of other mood disorder | 1 | 0.0349 | 0.0082 | <0.0001 |
| 0 | 0.0000 | |||
| Deprivation index quintile (from lower to higher deprivation) | 1 | 0.0283 | 0.0129 | 0.0285 |
| 2 | 0.0212 | 0.0113 | 0.0623 | |
| 3 | 0.0262 | 0.0114 | 0.0220 | |
| 4 | 0.0182 | 0.0109 | 0.0969 | |
| 5 | 0.0000 | |||
| Female gender | 1 | 0.0000 | ||
| 0 | −0.0485 | 0.0063 | <0.0001 | |
| Explanatory variables introduced at the sector level (level 2) | ||||
| Characteristics of patients seen in inpatient care aggregated by sector | ||||
| Mean age | 0.0080 | 0.0024 | 0.0009 | |
| % of patients suffering from anxiety disorders | −0.0075 | 0.0016 | <0.0001 | |
| % of patients suffering from bipolar disorders | 0.0001 | 0.0035 | 0.9892 | |
| Institutional characteristics of the hospital hosting the psychiatric sector | ||||
| Type of legal status of hospital | Private non-profit | 0.0612 | 0.1032 | 0.5534 |
| Public | 0.0000 | |||
| Specialization in psychiatry of the hospital | 1 | 0.0464 | 0.0477 | 0.3318 |
| 0 | 0.0000 | |||
| Participation of the hospital to teaching activities | 1 | −0.1063 | 0.0563 | 0.0594 |
| 0 | 0.0000 | |||
| Participation of the hospital to emergency care | 1 | −0.0979 | 0.0619 | 0.1147 |
| 0 | 0.0000 | |||
| Organizational characteristics of the hospital hosting the psychiatric sector | ||||
| Nb. of inpatient beds in the hospital per 1000 inh. | 0.0005 | 0.0325 | 0.9890 | |
| Level of development of AFTH | −0.0034 | 0.0017 | 0.0493 | |
| Characteristics of the environment | ||||
| Overall health status of the population of the catchment area (per 1000 inhabitants) | ||||
| Acute admission rate for somatic disorders | 0.0017 | 0.0008 | 0.0225 | |
| Mortality rate | 0.0853 | 0.0534 | 0.1105 | |
| Suicide rate | 0.0010 | 0.0169 | 0.9548 | |
| Nb. of individuals suffering from long-duration diseases | −0.0015 | 0.0010 | 0.1598 | |
| % of individuals suffering from psychiatric long-duration diseases among people suffering from long-duration diseases | −0.0235 | 0.0162 | 0.1483 | |
| Inpatient psychiatric admission rate | −0.1353 | 0.0471 | 0.0042 | |
| Availability of medical care in the catchment area (per 1000 inhabitants) | ||||
| Nb. of general practitioners | −0.0726 | 0.1331 | 0.5858 | |
| Nb. of community-based private psychiatrists | 0.3185 | 0.3460 | 0.3577 | |
| Nb. of psychologists | 0.0314 | 0.0454 | 0.4898 | |
| Nb. of non-psychiatric inpatient beds | 0.0020 | 0.0054 | 0.7140 | |
| Nb. of inpatient beds of private psychiatry | 0.2433 | 0.1157 | 0.0360 | |
| Availability of social care in the catchment area (per 1000 inhabitants) | ||||
| Capacity of housing institutions for disabled individuals | 0.0618 | 0.0337 | 0.0669 | |
| Capacity of centres providing care through employment | −0.0142 | 0.0432 | 0.7420 | |
| Capacity of housing and social rehabilitation centres | −0.1169 | 0.0553 | 0.0349 | |
| Level of urbanization | ||||
| Level of urbanization (from lower to higher urbanization) | 1 | −0.0922 | 0.0578 | 0.1110 |
| 2 | −0.0137 | 0.0832 | 0.8693 | |
| 3 | 0.0879 | 0.2652 | 0.7406 | |
| 4 | −0.1259 | 0.2629 | 0.6323 | |
| 5 | −0.1057 | 0.0618 | 0.0878 | |
| 6 | 0.0000 | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gandré, C.; Gervaix, J.; Thillard, J.; Macé, J.-M.; Roelandt, J.-L.; Chevreul, K. The Development of Psychiatric Services Providing an Alternative to Full-Time Hospitalization Is Associated with Shorter Length of Stay in French Public Psychiatry. Int. J. Environ. Res. Public Health 2017, 14, 325. https://doi.org/10.3390/ijerph14030325
Gandré C, Gervaix J, Thillard J, Macé J-M, Roelandt J-L, Chevreul K. The Development of Psychiatric Services Providing an Alternative to Full-Time Hospitalization Is Associated with Shorter Length of Stay in French Public Psychiatry. International Journal of Environmental Research and Public Health. 2017; 14(3):325. https://doi.org/10.3390/ijerph14030325
Chicago/Turabian StyleGandré, Coralie, Jeanne Gervaix, Julien Thillard, Jean-Marc Macé, Jean-Luc Roelandt, and Karine Chevreul. 2017. "The Development of Psychiatric Services Providing an Alternative to Full-Time Hospitalization Is Associated with Shorter Length of Stay in French Public Psychiatry" International Journal of Environmental Research and Public Health 14, no. 3: 325. https://doi.org/10.3390/ijerph14030325





