Epidemiology of Burns in Rural Bangladesh: An Update
Abstract
:1. Introduction
2. Materials and Methods
Ethical Statement
3. Results
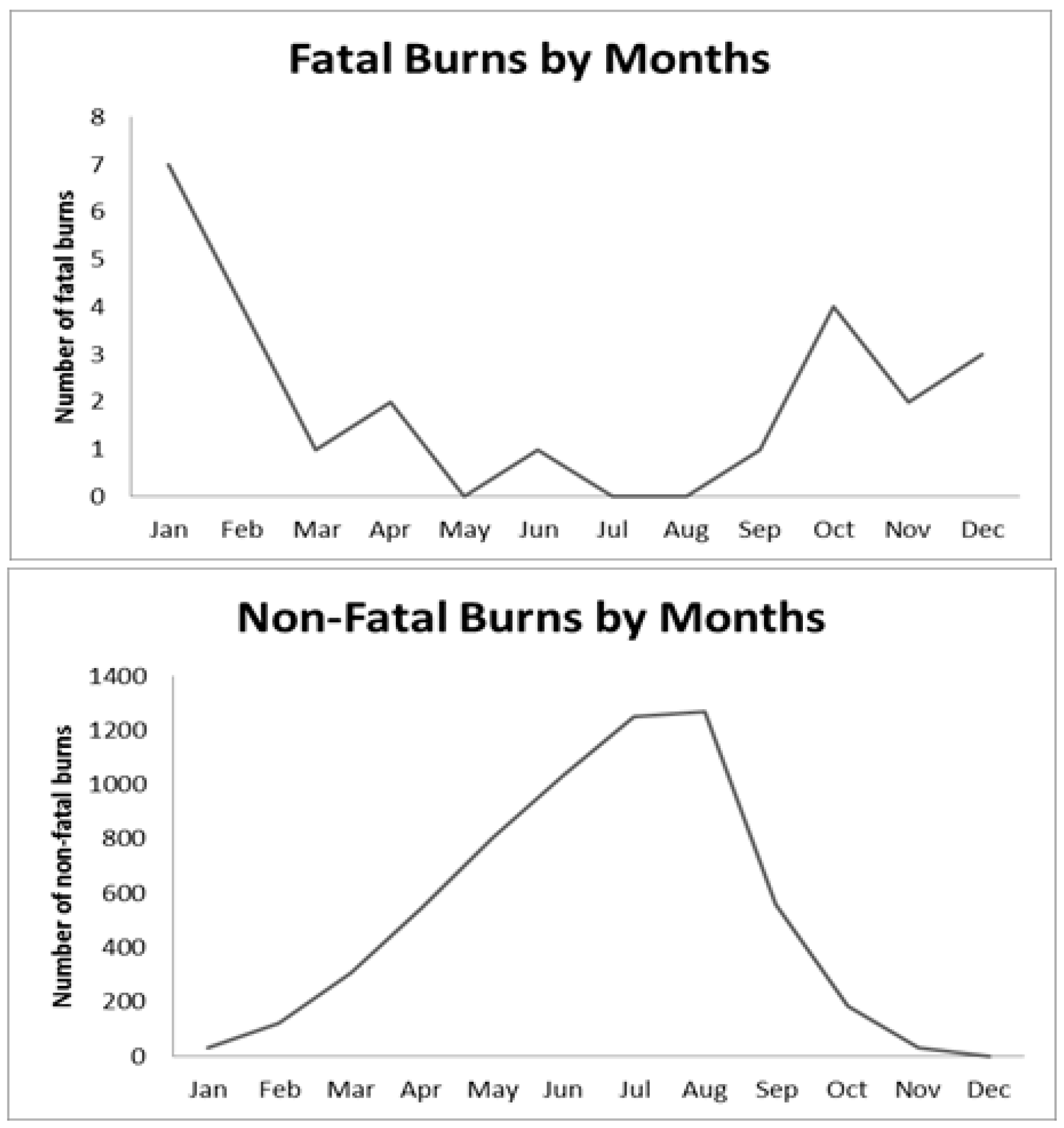
3.1. Fatal Burn Mortality Characteristics
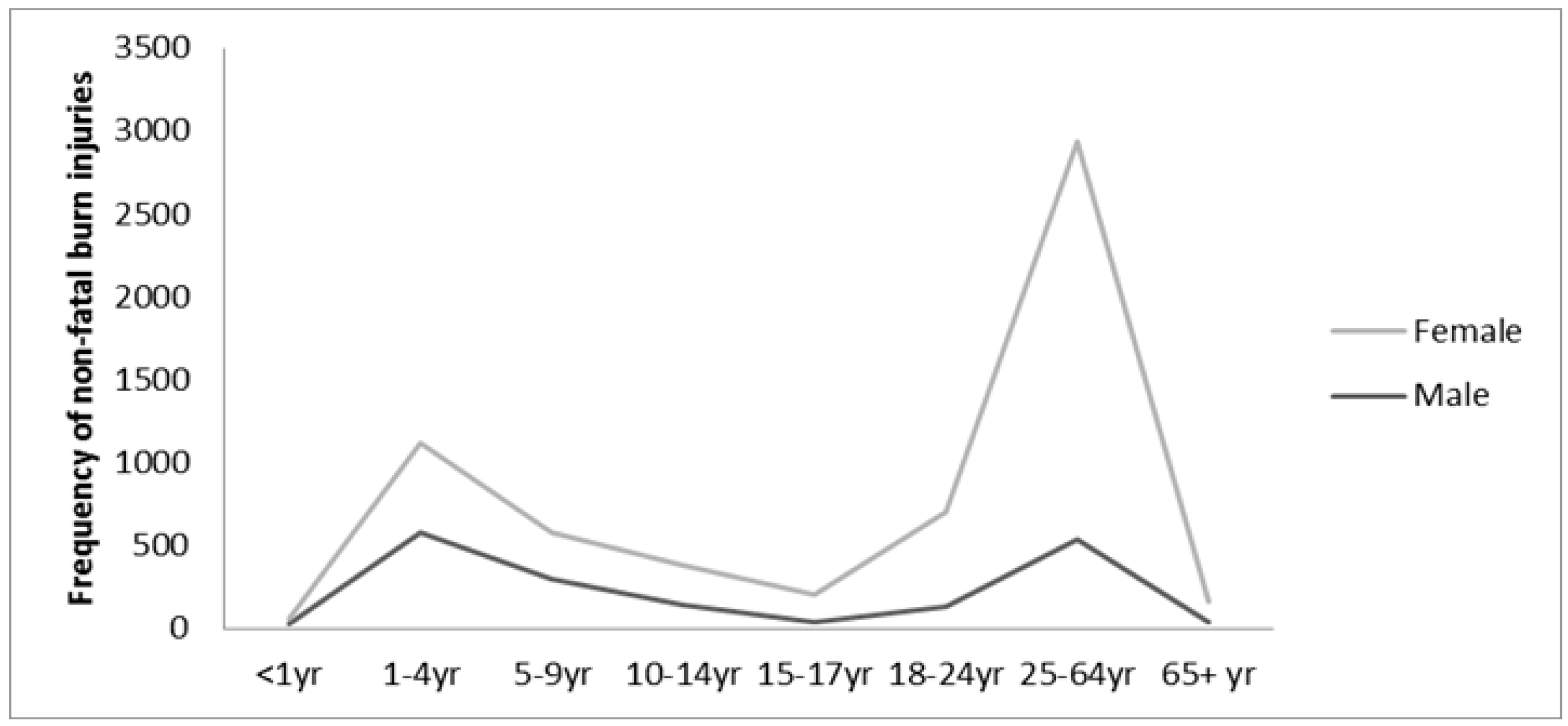
3.2. Non-Fatal Burn Morbidity Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| LMIC | low and middle income countries |
| HIC | high income countries |
| CIPRB | Center for Injury Prevention and Research, Bangladesh |
| Icddr,b | International Center for Diarrheal Disease Research, Bangladesh |
| CI | Confidence Interval |
| OR | Odds ratio |
References
- World Health Organization Media Center. Burns. Available online: http://www.who.int/mediacentre/factsheets/fs365/en/ (accessed on 1 March 2017).
- Peden, M. World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. Available online: https://www.ncbi.nlm.nih.gov/pubmed/?term=Peden%2C+M.+World+report+on+child+injury+prevention (accessed on 19 August 2015).
- Forjuoh, S.N. Burns in low-and middle-income countries: A review of available literature on descriptive epidemiology, risk factors, treatment and prevention. Burns 2006, 32, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.D. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 2011, 37, 1087–1100. [Google Scholar] [CrossRef] [PubMed]
- Golshan, A.; Patel, C.; Hyder, A.A. A systematic review of the epidemiology of unintentional burn injuries in South Asia. J. Public Health 2013, 35, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Wolf, S.E.; Arnoldo, B.D. The year in burns 2011. Burns 2012, 38, 1096–1108. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Lahoti, B.; Khandelwal, G.; Mathur, R.; Sharma, S.; Laddha, A. Epidemiological trends of pediatric trauma: A single-center study of 791 patients. J. Indian Assoc. Pediatr. Surg. 2011, 16, 88. [Google Scholar] [CrossRef] [PubMed]
- Atiyeh, B.; Masellis, A.; Conte, C. Optimizing burn treatment in developing low-and middle-income countries with limited health care resources (part 1). Ann. Burns Fire Disasters 2009, 22, 121. [Google Scholar] [PubMed]
- Mashreky, S.R.; Rahman, A.; Chowdhury, S.; Giashuddin, S.; Svanström, L.; Linnan, M.; Shafinaz, S.; Uhaa, I.J.; Rahman, F. Epidemiology of childhood burn: Yield of largest community based injury survey in Bangladesh. Burns 2008, 34, 856–862. [Google Scholar] [CrossRef] [PubMed]
- Delgado, J.; Ramirez-Cardich, M.; Gilman, R.H.; Lavarello, R.; Dahodwala, N.; Bazán, A.; Rodriguez, V.; Cama, R.I.; Tovar, M.; Lescano, A. Risk factors for burns in children: Crowding, poverty, and poor maternal education. Inj. Prev. 2002, 8, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Mashreky, S.R.; Rahman, A.; Khan, T.F.; Svanström, L.; Rahman, F. Determinants of childhood burns in rural Bangladesh: A nested case-control study. Health Policy 2010, 96, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Daisy, S.; Mostaque, A.; Bari, S.; Khan, A.; Karim, S.; Quamruzzaman, Q. Socioeconomic and cultural influence in the causation of burns in the urban children of Bangladesh. J. Burn Care Res. 2001, 22, 269–273. [Google Scholar] [CrossRef]
- Hyder, A.A.; Alonge, O.; He, S.; Wadhwaniya, S.; Rahman, F.; Rahman, A.; Arifeen, S.E. Saving of children’s lives from drowning project in Bangladesh. Am. J. Prev. Med. 2014, 47, 842–845. [Google Scholar] [CrossRef] [PubMed]
- Alonge, O.; Agrawal, P.; Khatlani, K.; Mashreky, S.R.; Islam, I.; Hyder, A.A. Injury Severity Index for population-based survey, manuscript. (Johns Hopkins University, Baltimore, MD, USA, manuscript in preparation).
- Lau, Y. An insight into burns in a developing country: A Sri Lankan experience. Public Health 2006, 120, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Mahmood, U.; Gurung, S.; Shrestha, S.; Kushner, A.; Nwomeh, B.C.; Charles, A.G. Burns in Nepal: A population based national assessment. Burns 2015, 41, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Singh, A.; Sharma, A.K.; Sodhi, L. Burn mortality in Chandigarh zone: 25 years autopsy experience from a tertiary care hospital of India. Burns 1998, 24, 150–156. [Google Scholar] [CrossRef]
- Batra, A.K. Burn mortality: Recent trends and sociocultural determinants in rural India. Burns 2003, 29, 270–275. [Google Scholar] [CrossRef]
- Laloe, V. Epidemiology and mortality of burns in a general hospital of Eastern Sri Lanka. Burns 2002, 28, 778–781. [Google Scholar] [CrossRef]
- Carroll, S.; Gough, M.; Eadie, P.; McHugh, M.; Edwards, G.; Lawlor, D. A 3-year epidemiological review of burn unit admissions in Dublin, Ireland: 1988–1991. Burns 1995, 21, 379–382. [Google Scholar] [CrossRef]
- El-Badawy, A.; Mabrouk, A.R. Epidemiology of childhood burns in the burn unit of Ain Shams University in Cairo, Egypt. Burns 1998, 24, 728–732. [Google Scholar] [CrossRef]
- Afify, M.M.; Mahmoud, N.F.; El Azzim, G.M.A.; El Desouky, N.A. Fatal burn injuries: A five year retrospective autopsy study in Cairo city, Egypt. Egypt J. Forensic Sci. 2012, 2, 117–122. [Google Scholar] [CrossRef]
- Mashreky, S.R.; Rahman, A.; Chowdhury, S.; Khan, T.; Svanström, L.; Rahman, F. Non-fatal burn is a major cause of illness: Findings from the largest community-based national survey in Bangladesh. Inj. Prev. 2009, 15, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, R.B.; Dash, J.K.; Shrivastava, P. A comparative analysis of liquefied petroleum gas (LPG) and kerosene related burns. Burns 2011, 37, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Gupta, O.; Goil, P. Paediatric burns in Jaipur, India: An epidemiological study. Burns 1992, 18, 63–67. [Google Scholar] [CrossRef]
- Razzak, J.A.; Luby, S.; Laflamme, L.; Chotani, H. Injuries among children in Karachi, Pakistan—What, where and how. Public Health 2004, 118, 114–120. [Google Scholar] [CrossRef]
- Liu, E.; Khatri, B.; Shakya, Y.; Richard, B. A 3 year prospective audit of burns patients treated at the Western Regional Hospital of Nepal. Burns 1998, 24, 129–133. [Google Scholar] [CrossRef]
- Lama, B.B.; Duke, J.M.; Sharma, N.P.; Thapa, B.; Dahal, P.; Bariya, N.D.; Marston, W.; Wallace, H.J. Intentional burns in Nepal: A comparative study. Burns 2015, 41, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Mashreky, S.R.; Rahman, F.; Rahman, A.; Baset, K.U.; Biswas, A.; Hossain, J. Burn injury in Bangladesh: Electrical injury a major contributor. Int. J. Burns Trauma 2011, 1, 62. [Google Scholar] [PubMed]
- Balan, B.; Lingam, L. Unintentional injuries among children in resource poor settings: Where do the fingers point? Arch. Dis. Child. 2012, 97, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Ali, W.; Verma, A.K.; Pandey, A.; Rathore, S. Epidemiology and mortality of burns in the Lucknow Region, India—A 5 year study. Burns 2013, 39, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Ibran, E.A.; Mirza, F.H.; Memon, A.A.; Farooq, M.Z.; Hassan, M. Mortality associated with burn injury—A cross sectional study from Karachi, Pakistan. BMC Res. Notes 2013, 6, 545. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.D.; Kruger, G.E.; van der Merwe, A.E.; Godakumbura, W.; Ahuja, R.B. Burns and fires from non-electric domestic appliances in low and middle income countries: Part I. The scope of the problem. Burns 2008, 34, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Edelman, L.S. Social and economic factors associated with the risk of burn injury. Burns 2007, 33, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Park, J.O.; Do Shin, S.; Kim, J.; Song, K.J.; Peck, M.D. Association between socioeconomic status and burn injury severity. Burns 2009, 35, 482–490. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | All Population (N = 1,169,594) | Fatal Burn Injuries (N = 25) | Non-Fatal Burns (N = 6142) | |||
|---|---|---|---|---|---|---|
| N | (%) | N (%) | Mortality Rate/1,000,000 | N (%) | Morbidity Rate/100,000 | |
| Upazila | ||||||
| Matlab North | 265,897 | (22.7) | 5 (20.0) | 18.8 | 1019 (16.6) | 385.3 |
| Matlab South | 209,772 | (17.9) | 3 (12.0) | 14.3 | 1103 (18.0) | 528.6 |
| Chadpur Sadar | 128,356 | (11.0) | 0 (0.0) | 0 | 347 (5.7) | 271.6 |
| Raiganj | 104,357 | (8.9) | 6 (24.0) | 57.5 | 932 (15.2) | 898.2 |
| Sherpur | 228,519 | (19.5) | 6 (24.0) | 26.3 | 1378 (22.4) | 606.1 |
| Manohardi | 204,319 | (17.5) | 4 (16.0) | 19.6 | 1150 (18.7) | 566.2 |
| Daud Kandi | 28,373 | (2.4) | 1 (4.0) | 35.2 | 213 (3.5) | 755.8 |
| Sex | ||||||
| Male | 567,674 | (48.5) | 2 (8.0) | 3.5 | 1787 (29.1) | 316.5 |
| Female | 601,919 | (51.5) | 23 (92.0) | 38.2 | 4355 (70.9) | 727.5 |
| Age | ||||||
| <1 year | 22,141 | (1.9) | 0 (0.0) | 0 | 92 (1.0) | 427.4 |
| 1–4 years | 90,523 | (7.7) | 0 (0.0) | 0 | 1121 (18.3) | 1243.3 |
| 5–9 years | 139,728 | (12.0) | 0 (0.0) | 0 | 574 (9.4) | 411.1 |
| 10–14 years | 142,121 | (12.2) | 1 (4.0) | 7.0 | 377 (6.1) | 265.4 |
| 15–17 years | 62,098 | (5.3) | 1 (4.0) | 16.1 | 208 (3.4) | 335.2 |
| 18–24 years | 133,534 | (11.4) | 4 (16.0) | 29.9 | 701 (11.4) | 525.5 |
| 25–64 years | 508,059 | (43.4) | 6 (24.0) | 11.8 | 2932 (47.7) | 579.2 |
| 65+ years | 71,389 | (6.1) | 13 (52.0) | 182.1 | 167 (2.7) | 244.6 |
| Education | ||||||
| No education | 295,314 | (25.3) | 17 (68.0) | 230.3 | 1538 (25.0) | 526.8 |
| Primary | 407,923 | (34.9) | 4 (16.0) | 39.2 | 1753 (28.5) | 430.8 |
| Secondary | 289,658 | (24.8) | 3 (12.0) | 41.4 | 1443 (23.5) | 499.3 |
| A levels | 45,618 | (3.9) | 0 (0.0) | 0 | 176 (2.9) | 386.7 |
| College | 13,526 | (1.2) | 0 (0.0) | 0 | 38 (0.6) | 281.8 |
| Advanced/professional degree | 4729 | (0.4) | 1 (4.0) | 845.8 | 11 (0.2) | 234.0 |
| Not applicable (Under 5) | 112,664 | (9.6) | 0 (0.0) | 0 | 1183 (19.3) | 1059.2 |
| Occupation | ||||||
| Agriculture | 104,956 | (9.0) | 1 (4.0) | 38.1 | 234 (3.8) | 225.4 |
| Business | 61,661 | (5.3) | 0 (0.0) | 0 | 147 (2.4) | 239.7 |
| Skilled labor (Professional) | 89,151 | (7.6) | 1 (4.0) | 44.9 | 263 (4.3) | 296.0 |
| Unskilled/domestic (Unskilled) | 24,520 | (2.1) | 0 (0.0) | 0 | 72 (1.2) | 295.1 |
| Rickshaw/bus (Transport worker) | 17,037 | (1.5) | 0 (0.0) | 0 | 47 (0.8) | 276.6 |
| Students | 312,537 | (26.7) | 1 (4.0) | 12.8 | 922 (15.0) | 295.2 |
| Retired/unemployed/housewife | 408,583 | (35.0) | 22 (88.0) | 215.4 | 3059 (49.8) | 754.1 |
| Not applicable (children) | 144,454 | (12.4) | 0 (0.0) | 0 | 1369 (22.3) | 954.6 |
| Not applicable (others) | 5948 | (0.5) | 0 (0.0) | 0 | 28 (0.5) | 484.3 |
| Marital status | ||||||
| Married | 571,206 | (48.8) | 11 (44.0) | 77.0 | 3358 (54.7) | 591.5 |
| Never married | 227,319 | (19.4) | 3 (12.0) | 52.8 | 622 (10.1) | 273.9 |
| Divorced | 3220 | (0.3) | 0 (0.0) | 0 | 8 (0.1) | 250.2 |
| Widowed | 53,096 | (4.5) | 10 (40.0) | 753.4 | 239 (3.9) | 462.8 |
| Separated | 2717 | (0.2) | 0 (0.0) | 0 | 16 (0.3) | 592.2 |
| Others (children under 12) | 312,035 | (26.7) | 1 (4.0) | 12.8 | 1899 (30.9) | 610.7 |
| SES quintiles | ||||||
| Lowest | 211,601 | (18.1) | 4 (16.0) | 18.9 | 1254 (20.4) | 596.4 |
| Low | 218,695 | (18.7) | 9 (36.0) | 41.1 | 1166 (19.0) | 535.8 |
| Middle | 238,371 | (20.4) | 6 (24.0) | 25.2 | 1199 (19.5) | 505.6 |
| High | 247,716 | (21.2) | 3 (12.0) | 12.1 | 1258 (20.5) | 510.5 |
| Highest | 253,210 | (21.7) | 3 (12.0) | 11.9 | 1265 (20.6) | 502.3 |
| Characteristics | Fatal Injuries | Non-Fatal Injuries | ||
|---|---|---|---|---|
| N | (%) | N | (%) | |
| Place of injury | ||||
| Bedroom | 7 | 28 | 273 | 4.44 |
| Kitchen | 14 | 56 | 4385 | 71.39 |
| Veranda | 1 | 4 | 32 | 0.52 |
| Yard | 3 | 12 | 729 | 11.87 |
| Others | - | - | 644 | 11.78 |
| Item causing injury | ||||
| Flame | 22 | 88 | 1555 | 25.32 |
| Hot liquid | 2 | 8 | 3472 | 56.53 |
| Hot object | 0 | 0 | 1003 | 16.33 |
| Explosive | 0 | 0 | 19 | 0.31 |
| Chemical | 0 | 0 | 30 | 0.49 |
| Other | 1 | 4 | 63 | 1.03 |
| Place of death | ||||
| Home | 13 | 52 | - | - |
| On the way to hospital 1 | 1 | 4 | ||
| Hospital | 9 | 36 | ||
| On the road 2 | 2 | 8 | ||
| Injury Severity | Non-Fatal Injuries | |
|---|---|---|
| N | (%) | |
| Low | 4283 | 69.73 |
| Medium | 1499 | 24.41 |
| High | 245 | 3.99 |
| Characteristics | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Age group | ||||||
| 10–14 years | Reference group | Reference group | ||||
| 15–17 years | 1.26 | 1.07–1.49 | <0.001 | 1.08 | 0.89–1.32 | 0.381 |
| 18–24 years | 1.98 | 1.75–2.25 | <0.001 | 1.05 | 0.86–1.29 | 0.618 |
| 25–64 years | 2.18 | 1.97–2.44 | <0.001 | 1.02 | 0.83–1.27 | 0.830 |
| 65+ years | 0.92 | 0.77–1.11 | 0.378 | 0.52 | 0.39–0.68 | <0.001 |
| Sex | ||||||
| Male | ||||||
| Female | 3.62 | 3.36–3.89 | <0.001 | 3.18 | 2.83–3.58 | <0.001 |
| Education | ||||||
| No education | ||||||
| Primary | 0.79 | 0.73–0.85 | <0.001 | 0.87 | 0.80–0.94 | 0.001 |
| Secondary | 0.91 | 0.84–0.98 | 0.012 | 0.92 | 0.84–0.99 | 0.049 |
| A levels | 0.71 | 0.60–0.82 | <0.001 | 0.86 | 0.73–1.03 | 0.105 |
| College | 0.51 | 0.37–0.71 | <0.001 | 0.88 | 0.49–0.95 | 0.025 |
| Advanced/professional degree | 0.43 | 0.24–0.76 | 0.005 | 0.60 | 0.33–1.10 | 0.102 |
| Occupation | ||||||
| Agriculture | ||||||
| Business | 1.06 | 0.86–1.29 | 0.51 | 1.06 | 0.87–1.32 | 0.562 |
| Skilled labor (Professional) | 1.31 | 1.10–1.56 | 0.003 | 1.19 | 0.99–1.43 | 0.062 |
| Unskilled/domestic (Unskilled) | 1.29 | 0.99–1.69 | 0.06 | 1.11 | 0.85–1.46 | 0.420 |
| Rickshaw/bus (Transport worker) | 1.22 | 0.89–1.67 | 0.21 | 1.19 | 0.87–1.63 | 0.269 |
| Students | 3.37 | 2.95–3.85 | <0.001 | 1.12 | 0.72–1.14 | 0.407 |
| Retired/unemployed/housewife | 1.42 | 20.79–2.54 | 0.25 | 0.91 | 1.01–1.43 | 0.035 |
| Marital status | ||||||
| Married | ||||||
| Never married | 0.46 | 0.42–0.50 | <0.001 | 0.65 | 0.55–0.76 | <0.001 |
| Divorced | 0.42 | 0.21–0.84 | 0.02 | 0.34 | 0.17–0.67 | 0.002 |
| Widowed | 0.78 | 0.69–0.89 | <0.001 | 0.68 | 0.58–0.78 | <0.001 |
| Separated | 1.00 | 0.61–1.64 | 1.00 | 0.78 | 0.47–1.28 | 0.334 |
| Others (children 10–12) | 0.41 | 0.34–0.48 | <0.001 | 0.58 | 0.45–0.76 | <0.001 |
| SES quintiles | ||||||
| Lowest | ||||||
| Low | 0.94 | 0.85–1.04 | 0.01 | 0.98 | 0.89–1.08 | 0.685 |
| Middle | 0.93 | 0.84–1.02 | <0.001 | 0.96 | 0.87–1.06 | 0442 |
| High | 0.94 | 0.79–0.92 | <0.001 | 0.98 | 0.89–1.04 | 0.745 |
| Highest | 0.95 | 0.78–0.91 | <0.001 | 0.98 | 0.89–1.08 | 0.687 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, S.; Alonge, O.; Agrawal, P.; Sharmin, S.; Islam, I.; Mashreky, S.R.; Arifeen, S.E. Epidemiology of Burns in Rural Bangladesh: An Update. Int. J. Environ. Res. Public Health 2017, 14, 381. https://doi.org/10.3390/ijerph14040381
He S, Alonge O, Agrawal P, Sharmin S, Islam I, Mashreky SR, Arifeen SE. Epidemiology of Burns in Rural Bangladesh: An Update. International Journal of Environmental Research and Public Health. 2017; 14(4):381. https://doi.org/10.3390/ijerph14040381
Chicago/Turabian StyleHe, Siran, Olakunle Alonge, Priyanka Agrawal, Shumona Sharmin, Irteja Islam, Saidur Rahman Mashreky, and Shams El Arifeen. 2017. "Epidemiology of Burns in Rural Bangladesh: An Update" International Journal of Environmental Research and Public Health 14, no. 4: 381. https://doi.org/10.3390/ijerph14040381
APA StyleHe, S., Alonge, O., Agrawal, P., Sharmin, S., Islam, I., Mashreky, S. R., & Arifeen, S. E. (2017). Epidemiology of Burns in Rural Bangladesh: An Update. International Journal of Environmental Research and Public Health, 14(4), 381. https://doi.org/10.3390/ijerph14040381






