Designing Fit for Purpose Health and Social Services for Ageing Populations
Abstract
:1. Introduction
2. Hong Kong as a Case Study
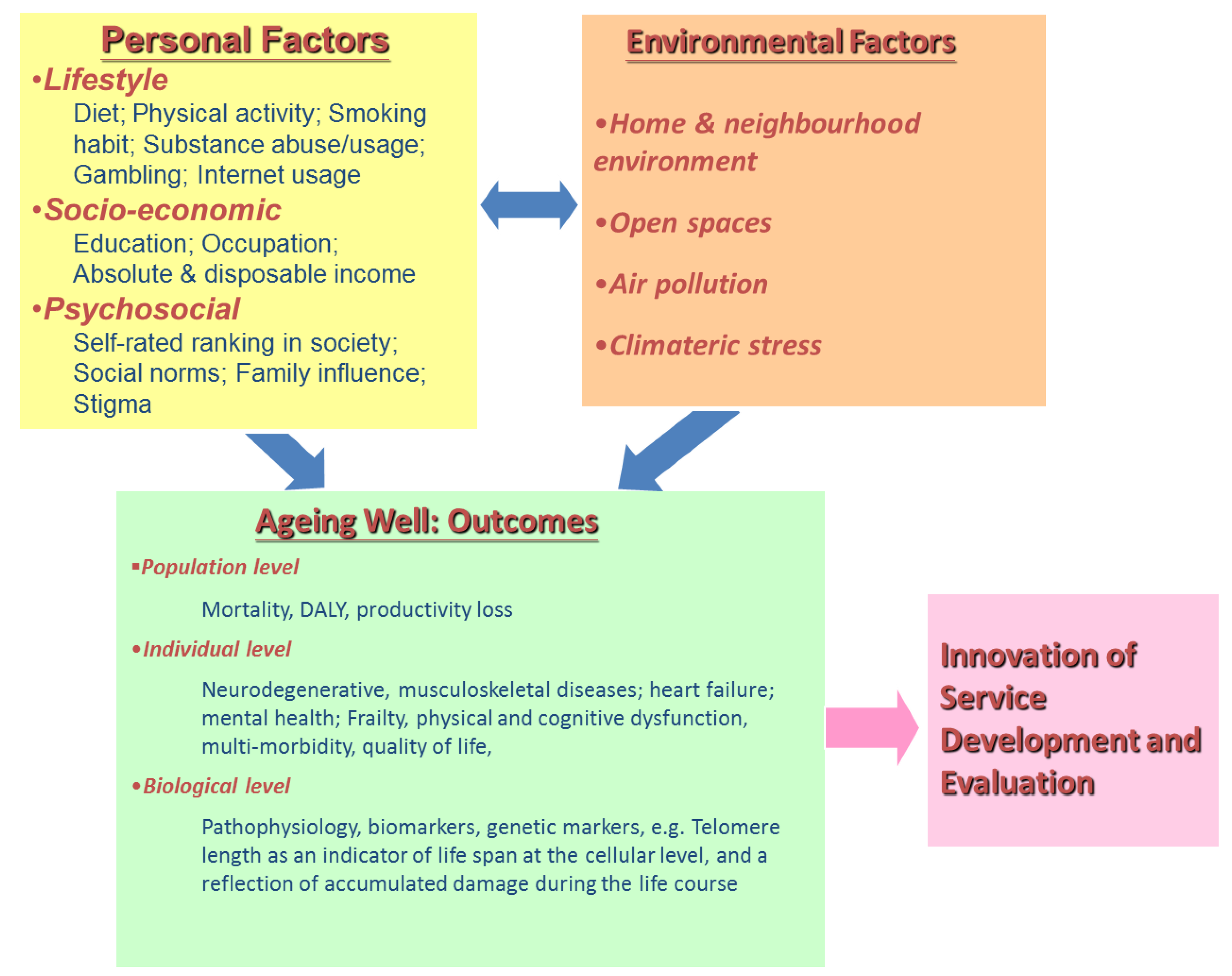
2.1. Documenting the Needs of the Ageing Hong Kong Population
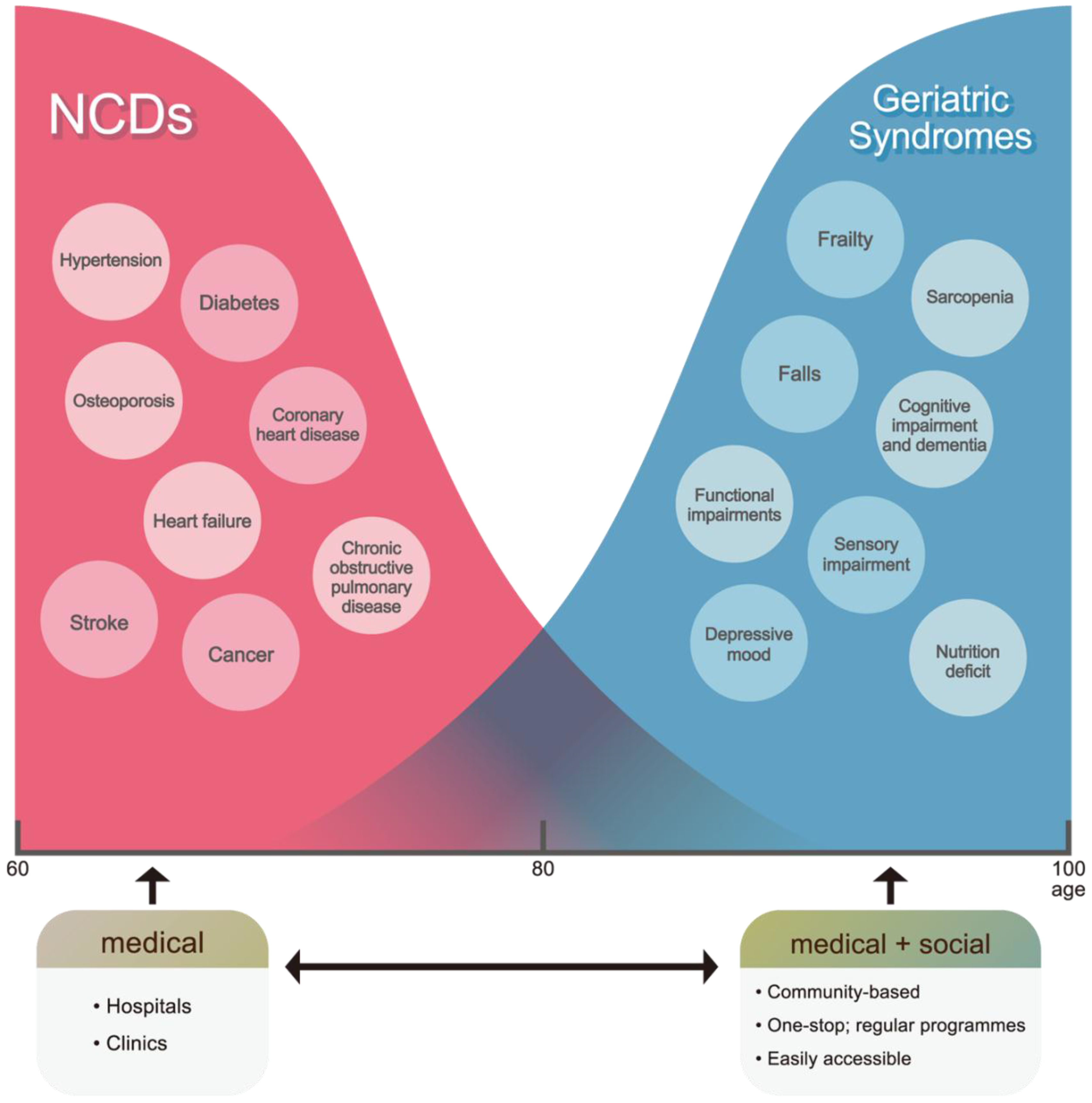
2.2. Designing Fit for Purpose Models of Care
3. Conclusions
Conflicts of Interest
References
- DALYs, G.B.D.; Collaborators, H. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1603–1658. [Google Scholar]
- Collaborators, G.S. Measuring the health-related Sustainable Development Goals in 188 countries: A baseline analysis from the Global Burden of Disease Study 2015. Lancet 2016, 388, 1813–1850. [Google Scholar]
- World Health Organization. World Report on Ageing and Health. Available online: http://www.who.int/ageing/publications/world-report-2015/en/ (accessed on 13 March 2017).
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef]
- Woo, J.; Leung, J.; Zhang, T. Successful Aging and Frailty: Opposite Sides of the Same Coin? J. Am. Med. Dir. Assoc. 2016, 17, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Wong, M.; Chang, B.; Lai, X.; Lum, C.M.; Auyeung, T.W.; Lee, J.; Tsoi, K.; Lee, R.; Woo, J. Trends in activities of daily living disability in a large sample of community-dwelling Chinese older adults in Hong Kong: An age-period-cohort analysis. BMJ 2016, 6, e013259. [Google Scholar]
- Zeng, Y.; Feng, Q.; Hesketh, T.; Christensen, K.; Vaupel, J.W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: A cohort study. Lancet 2017. [Google Scholar] [CrossRef]
- Collard, R.M.; Boter, H.; Schoevers, R.A.; Oude Voshaar, R.C. Prevalence of frailty in community-dwelling older persons: A systematic review. J. Am. Geriatr. Soc. 2012, 60, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Yu, R.; Wong, M.; Yeung, F.; Wong, M.; Lum, C. Frailty Screening in the Community Using the FRAIL Scale. J. Am. Geriatr. Soc. 2015, 16, 412–419. [Google Scholar] [CrossRef] [PubMed]
- British Geriatrics Society. Fit for Frailty. Available online: https://britishgeriatricssociety.wordpress.com/2014/06/25/fit-for-frailty/ (accessed on 13 March 2017).
- Gan, K.Y. Geriatrics beyond Borders: Are We Frailty Ready? Available online: https://www.moh.gov.sg/content/moh_web/home/pressRoom/speeches_d/2016/speech-by-mr-gan-kim-yong--minister-of-health--at-the-asia-pacif.html (accessed on 13 March 2017).
- Vellas, B.; Balardy, L.; Gillette-Guyonnet, S.; Van Kan, G.A.; Ghisolfi-Marque, A.; Subra, J.; Bismuth, S.; Oustric, S.; Cesari, M. Looking for frailty in community-dwelling older persons: The Gerontopole Frailty Screening Tool (GFST). J. Nutr. Health Aging 2013, 17, 629–631. [Google Scholar] [CrossRef] [PubMed]
- Shinkai, S.; Yoshida, H.; Taniguchi, Y.; Murayama, H.; Nishi, M.; Amano, H.; Nofuji, Y.; Seino, S.; Fujiwara, Y. Public health approach to preventing frailty in the community and its effect on healthy aging in Japan. Geriatr. Gerontol. Int. 2016, 16 (Suppl. 1), 87–97. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef]
- Naci, H.; Ioannidis, J.P. Evaluation of Wellness Determinants and Interventions by Citizen Scientists. JAMA 2015, 314, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Wong, M.; Chog, B.; Lum, C.M.; Auyeung, T.W.; Lee, J.; Lee, R.; Woo, J. Trajectories of Frailty in an Elderly Health Service Cohort in Hong Kong: An Age-period-cohort Analysis. Unpublished work. 2017. [Google Scholar]
- Mak, B.; Woo, J.; Bowling, A.; Wong, F.; Chau, P.H. Health care prioritization in ageing societies: Influence of age, education, health literacy and culture. Health Policy 2011, 100, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Ho, S.C.; Lau, J.; Yuen, Y.K.; Chiu, H.; Lee, H.C.; Chi, I. The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatr. Scand. 1994, 89, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Conwell, Y.; Thompson, C. Suicidal behavior in elders. Psychiatr. Clin. N. Am. 2008, 31, 333–356. [Google Scholar] [CrossRef] [PubMed]
- CUHK. Report on Age Watch Index for Hong Kong. 2014. Available online: http://www.ioa.cuhk.edu.hk/images/content/Report_AgeWatch2014.pdf (accessed on 14 March 2017).
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Ronzi, S.; Hanratty, B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart 2016, 102, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.L.; Chen, S.L.; Conwell, Y. Effects of Transient Versus Chronic Loneliness on Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. Am. J. Geriatric. Psychiatry 2016, 24, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Routasalo, P.; Pitkala, K.H. Loneliness among older people. Rev. Clin. Gerontol. 2003, 13, 303–311. [Google Scholar] [CrossRef]
- Yeoh, E.K.; Lai, A.H.Y. An Investment for the Celebration of Aging. Available online: http://ourhkfoundation.org.hk/sites/default/files/media/pdf/OHKF_20161206_Aging_eng.pdf (accessed on 24 April 2017).
- Hui, E.; Woo, J. Telehealth for older patients: The Hong Kong experience. J. Telemed. Telecare 2002, 8, 39–41. [Google Scholar] [CrossRef] [PubMed]
- Yeung, P.Y.; Chan, W.; Woo, J. A community-based Falls Management Exercise Programme (FaME) improves balance, walking speed and reduced fear of falling. Prim. Health Care Res. Dev. 2015, 16, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J. Social Inequalities in Health. New Evidence and Policy Implications, 1st ed.; Marmot, J., Ed.; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woo, J. Designing Fit for Purpose Health and Social Services for Ageing Populations. Int. J. Environ. Res. Public Health 2017, 14, 457. https://doi.org/10.3390/ijerph14050457
Woo J. Designing Fit for Purpose Health and Social Services for Ageing Populations. International Journal of Environmental Research and Public Health. 2017; 14(5):457. https://doi.org/10.3390/ijerph14050457
Chicago/Turabian StyleWoo, Jean. 2017. "Designing Fit for Purpose Health and Social Services for Ageing Populations" International Journal of Environmental Research and Public Health 14, no. 5: 457. https://doi.org/10.3390/ijerph14050457





