Underweight, Stunting and Wasting among Children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Site
2.2. Study Population
2.3. Sampling Procedures
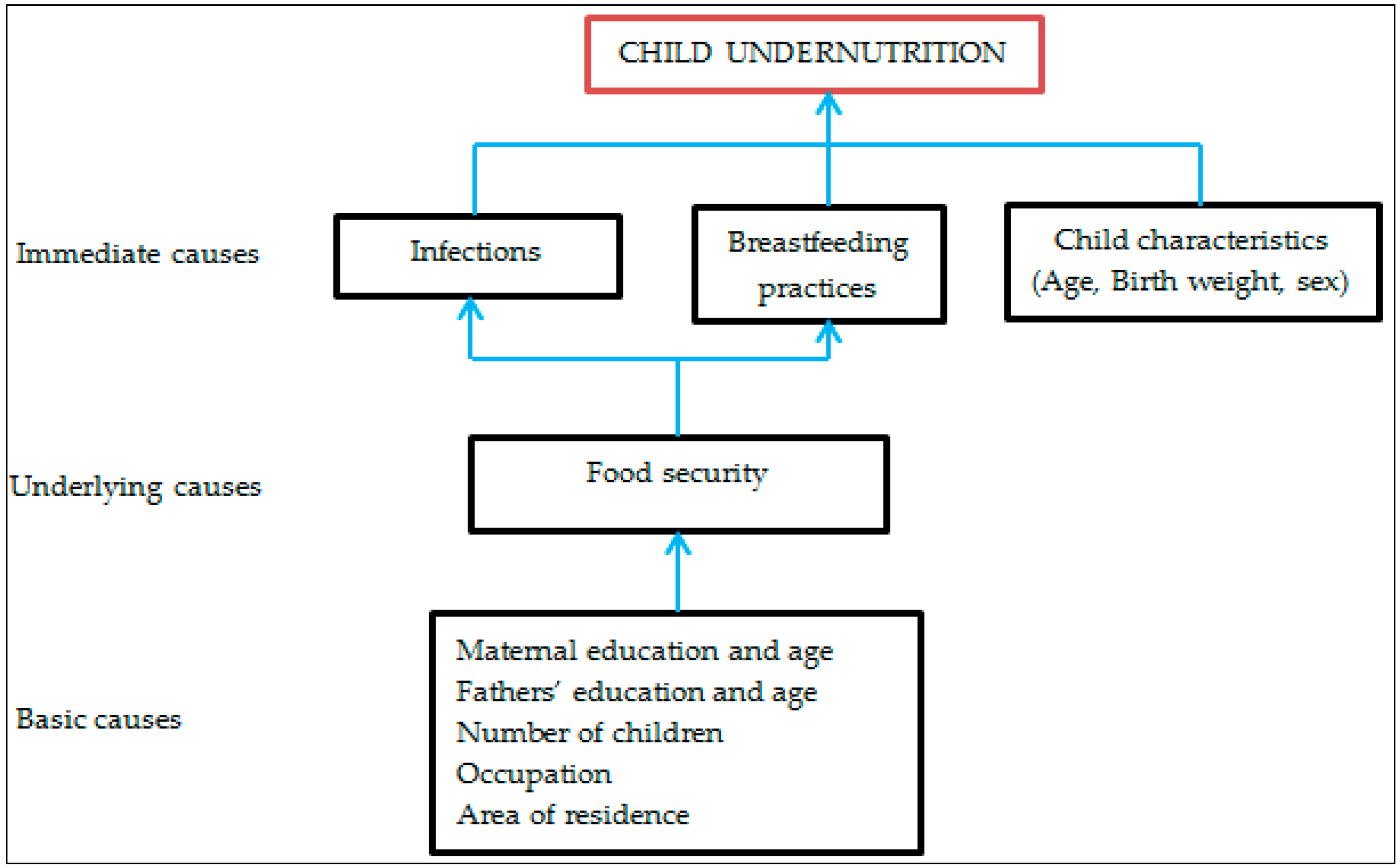
2.4. Measures
2.4.1. Sociodemographic and Economic Data
2.4.2. Anthropometry
2.4.3. Haemoglobin Levels
2.4.4. Data Analysis
3. Results
3.1. Child Information
3.2. Nutritional Status
3.3. Breastfeeding Practices
3.4. Factors Associated with Underweight, Stunting and Wasting
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Bryce, J.; Boschi-Pinto, C.; Shibuya, K.; Black, R.E. WHO estimates of the causes of death in children. Lancet 2005, 365, 1147–1152. [Google Scholar] [CrossRef]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef]
- Victora, C.G.; Adair, L.; Fall, C.; Hallal, P.C.; Martorell, R.; Ritcher, L.; Sachdev, H.S. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet 2008, 371, 340–357. [Google Scholar] [CrossRef]
- World Health Organization. World Health Statistics; 2015. Available online: http://apps.who.int/iris/bitstream/10665/170250/1/9789240694439_eng.pdf?ua=1 (accessed on 28 September 2016).
- Ministry of Health and Social Welfare. The National Road Map Strategic Plan to Accelerate Reduction of Maternal, Newborn and Child Deaths in Tanzania 2008–2015, Sharpened One Plan; Ministry of Health and Social Welfare: Dar es Salaam, Tanzania, 2008.
- World Health Organization. Nutrition Landscape Information System (NLIS). In Country Profile Indicators: Interpretation Guide; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- National Bureau of Statistics (NBS) [Tanzania] and ICF Macro. Tanzania Demographic and Health Survey 2010; NBS and ICF Macro: Dar es Salaam, Tanzania, 2011. [Google Scholar]
- National Bureau of Statistics (NBS) [Tanzania] and ORC Macro. Tanzania Demographic and Health Survey 2004–2005; National Bureau of Statistics and ORC Macro: Dar es Salaam, Tanzania, 2005. [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar] National Bureau of Statistics (NBS); Office of the Chief Government Statistician (OCGS), and ICF International. Tanzania and Demographic Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015–2016; MoHCDGEC: Dar es Salaam, Tanzania; MoHSW, MoH, NBS, OCGS and ICF International: Rockville, MD, USA, 2016. [Google Scholar]
- Dewey, K.G.; Mayers, D.R. Early child growth: How do nutrition and infection interact? Matern. Child Nutr. 2011, 7, 129–142. [Google Scholar] [CrossRef] [PubMed]
- Amugsi, D.A.; Mittelmark, M.B.; Lartey, A.; Matanda, D.J.; Urke, H.B. Influence of childcare practices on nutritional status of Ghanaian children: A regression analysis of the Ghana Demographic and Health Surveys. BMJ Open 2014, 4, e005340. [Google Scholar] [CrossRef] [PubMed]
- Van de Poel, E.; Hosseinpoor, A.R.; Jehu-Appiah, C.; Vega, J.; Speybroeck, N. Malnutrition and the disproportional burden on the poor: The case of Ghana. Int. J. Equity Health 2007, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Chirande, L.; Charwe, D.; Mmbwana, H.; Victor, R.; Kimboka, S.; Issaka, A.I.; Baines, R.K.; Dibley, A.J.; Agho, K.E. Determinants of stunting and severe stunting among under-fives in Tanzania: Evidence from the 2010 cross-sectional household survey. BMC Pediatr. 2015, 15, 165. [Google Scholar] [CrossRef] [PubMed]
- Uriyo, J.G.; Abubakar, A.; Swai, M.; Msuya, S.E.; Stray-Pedersen, B. Prevalence and correlates of common mental disorders among mothers of young children in Kilimanjaro region of Tanzania. PLoS ONE 2013, 8, e69088. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics, Ministry of Finance. Population Distribution by Age and Sex; National Bureau of Statistics, Ministry of Finance: Dar es Salaam, Tanzania; Office of Chief Government Statistician President Office, Finance, Economy and Development Planning: Zanzibar, Tanzania, 2013. [Google Scholar]
- De Onis, M.; Garza, C.; Victora, C.G.; Onyango, A.W.; Frongillo, E.A.; Martines, J. The WHO Multicentre. Growth Reference Study: Planning, study design, and methodology. Food Nutr. Bull. 2004, 25 (Suppl. 1), S15–S26. [Google Scholar]
- World Health Organization. Complementary feeding in the WHO Multicentre Growth Reference Study. Acta Pediatr. 2006, 450, 27–37. [Google Scholar]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. In Vitamin and Mineral Nutrition Information Cystem; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Abubakar, A.; Uriyo, J.; Msuya, S.E.; Swai, M.; Stray-Pedersen, B. Prevalence and risk factors for poor nutritional status among children in the Kilimanjaro Region of Tanzania. Int. J. Environ. Res. Public Health 2012, 9, 3506–3518. [Google Scholar] [CrossRef] [PubMed]
- Yalew, B. Prevalence of Malnutrition and Associated Factors among Children Age 6–59 Months at Lalibela Town Administration, North WolloZone, Anrs, Northern Ethiopia. J. Nutr. Disord. Ther. 2014, 4, 132. [Google Scholar] [CrossRef]
- Suskind, D.L. Nutritional deficiencies during normal growth. Pediatr. Clin. N. Am. 2009, 56, 1035–1053. [Google Scholar] [CrossRef] [PubMed]
- Mamiro, P.S.; Kolsteren, P.; Robertfroid, D.; Tatala, S.; Opsomer, A.S.; Van Camp, J.H. Feeding practices and factors contributing to wasting, stunting, and iron-deficiency anaemia among 3–23-month old children in Kilosa district, rural Tanzania. J. Health Popul. Nutr. 2005, 3, 222–230. [Google Scholar]
- Safari, J.G.; Kimambo, S.C.; Lwelamira, J.E. Feeding practices and nutritional status of infants in Morogoro Municipality, Tanzania. Tanzan. J. Health Res. 2013, 3, 178–185. [Google Scholar] [CrossRef]
- Black, R.E.; Alderman, H.; Bhutta, Z.A.; Gillespie, S.; Haddad, L.; Horton, S.; Lartey, A.; Mannar, V.; Ruel, M.; Victora, C.G.; et al. Maternal and child nutrition: Building momentum for impact. Lancet 2013, 382, 372–375. [Google Scholar]
- Food and Agriculture Organization; IFAD; WFP. The State of Food Insecurity in the World 2014: Strengthening the Enabling Environment for Food Security and Nutrition; FAO: Rome, Italy, 2014. [Google Scholar]
- Sachs, J.D. From millennium development goals to sustainable development goals. Lancet 2012, 379, 2206–2211. [Google Scholar] [CrossRef]
- Saha, K.K.; Frongilo, E.A.; Alam, D.; Arifeen, S.E.; Persson, L.A.; Rasmussen, K.M. Appropriate infant feeding practices result in better growth of infants and young children in rural Bangladesh. Am. J. Clin. Nutr. 2008, 87, 1852–1859. [Google Scholar] [PubMed]
- Fekadu, Y.; Mesfin, A.; Haile, D.; Stoecker, B.J. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: A cross-sectional study. BMC Public Health 2015, 15, 846. [Google Scholar] [CrossRef] [PubMed]
- Mbori-Ngacha, D.A.; Otieno, J.A.; Njeru, E.K.; Onyango, F.E. Prevalence of persistent diarrhoea in children aged 3–36 months at the Kenyatta National Hospital, Nairobi, Kenya. E. Afr. Med. J. 1995, 72, 711–714. [Google Scholar]
- Marriott, B.P.; White, A.; Hadden, L.; Davies, J.C.; Wallingford, J.C. World Health Organization (WHO) infant and young child feeding indicators: Associations with growth measures in 14 low-income countries. Matern. Child Nutr. 2011, 8, 354–370. [Google Scholar] [CrossRef] [PubMed]
- Mahgoub, S.E.; Nnyepi, M.; Bandeke, T. Factors affecting prevalence of malnutrition among children under three years of age in Botswana. Afr. J. Food Agric. Nutr. 2006, 6. [Google Scholar]
- Fawzi, W.W.; Herrera, M.G.; Nestel, P.; El Amin, A.; Mohamed, K.A. A longitudinal study of prolonged breastfeeding in relation to child undernutrition. Int. J. Epidemiol. 1998, 27, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Anuradha, R.; Ranjit, S.; Sam, D.S.; Roniya, F.; Roopa, D.; Sakthi, S.; Sabu, S.R.; Ranjit, P. Nutritional Status of Children Aged 3–6 Years in a Rural Area of Tamilnadu. J. Clin. Diagn. Res. 2014, 8, JC01–JC04. [Google Scholar]
- Dhakal, M.M.; Rai, A.; Singh, C.M.; Mohapatra, S.C. Health impact assessment: A futuristic approach in under-five care. Indian J. Prev. Soc. Med. 2005, 36, 114–120. [Google Scholar]
- Van de Poel, E.; Hosseinpoor, A.R.; Speybroeck, N.; Ourti, T.M.; Vega, J. Socioeconomic inequality in malnutrition in developing countries. Bull. World Health Organ. 2008, 86, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Kenya National Bureau of Statistics (KNBS) and ICF Macro. Kenya Demographic and Health Survey 2008–2009; KNBS and ICF Macro: Calverton, MD, USA, 2010. [Google Scholar]
- Correia, L.L.; Silva, A.C.; Campos, J.S.; Andrade, F.M.O.; Machado, M.M.T.; Lindsay, A.C.; Leite, A.J.; Rocha, H.A.; Cunha, A.J. Prevalence and determinants of child undernutrition and stunting in semiarid region of Brazil. Rev. Saude Publica 2014, 48, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Merialdi, M.; Gulmezoglu, A.M.; Abalos, E.; Carroli, G.; Kulier, R.; de Onis, M. Nutritional interventions during pregnancy for the prevention or treatment of maternal morbidity and preterm delivery: An overview of randomized controlled trials. J. Nutr. 2003, 133, 1606S–1625S. [Google Scholar] [PubMed]
- Shah, P.S.; Ohlsson, A. Effects of prenatal multimicronutrient supplementation on pregnancy outcomes: A meta-analysis. CMAJ 2009, 180, E99–E108. [Google Scholar] [CrossRef] [PubMed]
| Variable Name | N | % |
|---|---|---|
| Child age (months) | ||
| 0–6 | 482 | 23.9 |
| 7–12 | 649 | 32.2 |
| 13–24 | 739 | 36.7 |
| Sex | ||
| Male | 977 | 52.2 |
| Female | 893 | 47.8 |
| Anaemia status * | ||
| Normal | 646 | 34.8 |
| Anaemic | 1213 | 65.3 |
| Residence | ||
| Urban | 623 | 33.3 |
| Rural | 1247 | 66.7 |
| Variable Name | N | Stunted n (%) | p Value | Underweight n (%) | p Value | Wasted n (%) | p Value |
|---|---|---|---|---|---|---|---|
| Age (months) | |||||||
| 0–6 | 482 | 145 (30.1) | <0.001 | 104 (21.6) | <0.001 | 77 (16.0) | <0.0001 |
| 7–12 | 649 | 255 (34.7) | 291 (44.8) | 166 (25.6) | |||
| 13–24 | 739 | 414 (56.0) | 466 (63.1) | 218 (29.5) | |||
| Sex | |||||||
| Male | 977 | 416 (42.6) | 0.549 | 466 (47.7) | 0.133 | 260 (26.6) | 0.040 |
| Female | 893 | 368 (41.2) | 395 (44.2) | 201 (22.5) | |||
| Districts | |||||||
| Mwanga | 168 | 82 (48.8) | <0.001 | 79 (47.2) | 0.116 | 34 (20.2) | 0.144 |
| Rombo | 470 | 231 (49.2) | 234 (49.8) | 106 (22.55) | |||
| Moshi District Council | 582 | 220 (37.8) | 252 (43.3) | 143 (24.6) | |||
| Moshi Municipal Council | 230 | 97 (42.2) | 93 (40.3) | 55 (23.9) | |||
| Hai | 225 | 74 (32.9) | 105 (46.7) | 63 (28.0) | |||
| Siha | 195 | 80 (41.0) | 98 (50.3) | 60 (30.8) |
| Variable Name | N | n (%) Underweight | COR (95% CI) | p Value | AOR (95% CI) | p Value |
|---|---|---|---|---|---|---|
| Mother’s education | ||||||
| None/primary incomplete | 138 | 80 (58.0) | 1 | 1 | ||
| Primary complete | 1542 | 709 (46) | 0.6 (0.4, 0.9) | 0.012 | 0.7 (0.4, 1.1) | 0.136 |
| Secondary and above | 190 | 72 (37.9) | 0.5 (0.3, 0.7) | 0.001 | 0.5 (0.3, 0.9) | 0.039 |
| Child information | ||||||
| Child’s age 0–6 | 482 | 104 (21.6) | 1 | 1 | ||
| 7–12 | 649 | 291 (44.8) | 3.0 (2.3, 4.0) | <0.001 | 3.1 (2.2, 4.3) | <0.001 |
| 13–24 | 739 | 466 (63.1) | 6.5 (5.0, 8.6) | 6.3 (4.5, 8.8) | ||
| Sex | ||||||
| Male | 977 | 466 (47.8) | 1 | 1 | ||
| Female | 893 | 395 (44.2) | 0.9 (0.7, 1.0) | 0.128 | 0.9 (0.7, 1.1) | 0.190 |
| Birth weight * | ||||||
| Low birth weight | 98 | 75 (76.5) | 1 | 1 | ||
| Normal | 1705 | 749 (43.9) | 0.2 (0.1, 0.4) | <0.001 | 0.2 (0.1, 0.4) | <0.001 |
| Breastfeeding * | ||||||
| No | 287 | 180 (62.7) | 1 | |||
| Yes | 1540 | 656 (42.6) | 0.4 (0.3, 0.5) | <0.001 | 0.6 (0.4, 0.8) | 0.001 |
| Child illness * | ||||||
| No | 1500 | 623 (41.5) | 1 | 1 | ||
| Yes | 360 | 233 (64.7) | 2.6 (2.0, 3.3) | <0.001 | 2.0 (1.5, 2.7) | <0.001 |
| SES | ||||||
| Low | 500 | 251 (50.2) | ||||
| Medium | 505 | 238 (47.1) | 0.9 (0.7, 1.1) | 0.248 | 0.9 (0.6, 1.2) | 0.333 |
| High | 487 | 208 (42.7) | 0.7 (0.5, 0.9) | 0.016 | 0.8 (0.6, 1.0) | 0.073 |
| Variable Name | N | n (%) Stunted | COR | p Value | AOR | p Value |
|---|---|---|---|---|---|---|
| Mother’s education | ||||||
| None/primary incomplete | 138 | 73 (52.9) | 1 | 1 | ||
| Primary complete | 1542 | 636 (41.3) | 0.6 (0.4, 0.9) | 0.008 | 0.6 (0.4, 0.9) | 0.025 |
| Secondary and above | 190 | 75 (39.5) | 0.6 (0.4, 0.9) | 0.020 | 0.6 (0.3, 0.9) | 0.043 |
| Father’s age * | ||||||
| 15–24 | 167 | 78 (46.7) | 1 | 1 | ||
| 25–34 | 759 | 325 (42.8) | 0.8 (0.6, 1.2) | 0.8 (0.5, 1.2) | ||
| 35+ | 755 | 282 (37.5) | 0.7 (0.5, 0.9) | 0.029 | 0.6 (0.4, 0.8) | 0.008 |
| Child information | ||||||
| Child’s age 0–6 | 482 | 145 (30.1) | 1 | 1 | ||
| 7–12 | 649 | 255 (34.7) | 1.2 (1.0, 1.6) | 0.090 | 1.2 (0.9, 1.6) | 0.233 |
| 13–24 | 739 | 414 (56.0) | 3.1 (2.4, 4.0) | <0.001 | 2.9 (2.3, 3.9) | <0.001 |
| Sex | ||||||
| Male | 977 | 416 (42.6) | 1 | 1 | ||
| Female | 893 | 368 (41.2) | 0.9 (0.8, 1.1) | 0.498 | 0.8 (0.6, 1.0) | 0.047 |
| Birth weight * | ||||||
| Low birth weight | 98 | 77 (78.6) | 1 | 1 | ||
| Normal | 1705 | 676 (39.7) | 0.2 (0.1, 0.3) | <0.001 | 0.2 (0.1, 0.3) | <0.001 |
| Breastfeeding | ||||||
| No | 287 | 160 (55.8) | 1 | |||
| Yes | 1540 | 601 (39.0) | 0.5 (0.4, 0.7) | <0.001 | 0.7 (0.5, 1.0) | 0.047 |
| Child illness * | ||||||
| No | 1500 | 573 (38.2) | ||||
| Yes | 360 | 205 (56.9) | 2.1 (1.7, 2.8) | <0.001 | 1.7 (1.3, 2.2) | <0.001 |
| Districts | ||||||
| Mwanga | 168 | 82 (44.8) | 1 | 1 | 1 | |
| Rombo | 470 | 231 (49.2) | 1.0 (0.8, 1.6) | 0.939 | 1.2 (0.7, 1.8) | 0.595 |
| Moshi District council | 582 | 220 (37.8) | 0.6 (0.4, 0.9) | 0.012 | 0.7 (0.4, 1.1) | 0.059 |
| Moshi Municipal council | 230 | 97 (42.2) | 0.7 (0.5, 1.2) | 0.201 | 0.7 (0.4, 1.1) | 0.113 |
| Hai | 225 | 74 (32.9) | 0.5 (0.3, 0.8) | 0.002 | 0.5 (0.3, 0.8) | 0.006 |
| Siha | 195 | 80 (41.0) | 0.7 (0.5, 1.1) | 0.148 | 0.7 (0.4, 1.2) | 0.231 |
| SES | ||||||
| Low | 500 | 226 (45.2) | 1 | |||
| Medium | 505 | 211 (41.8) | 0.9 (0.7, 1.1) | 0.243 | ||
| High | 487 | 191 (39.2) | 0.8 (0.6, 1.1) | 0.060 |
| Variable Name | N | n (%) Wasted | COR | p Value | AOR | p Value |
|---|---|---|---|---|---|---|
| Child information | ||||||
| Child’s age 0–6 | 482 | 77 (16.0) | 1 | 1 | ||
| 7–12 | 649 | 166 (25.6) | 1.8 (1.4, 2.5) | <0.01 | 1.9 (1.3, 2.6) | <0.001 |
| 13–24 | 739 | 218 (29.5) | 2.3 (1.7, 3.0) | <0.01 | 1.9 (1.4, 2.7) | <0.001 |
| Sex | ||||||
| Male | 977 | 260 (26.6) | 1 | 1 | ||
| Female | 893 | 201 (22.5) | 0.8 (0.6, 1.0) | 0.038 | 0.8 (0.6, 0.9) | 0.015 |
| Birth weight * | ||||||
| Low weight | 98 | 36 (36.7) | 1 | 1 | ||
| Normal | 1705 | 400 (23.5) | 0.5 (0.3, 0.8) | 0.004 | 0.5 (0.3, 0.8) | 0.005 |
| Breastfeeding * | ||||||
| No | 287 | 99 (34.5) | 1 | 1 | ||
| Yes | 1540 | 351 (22.8) | 0.5 (0.4, 0.7) | <0.001 | 0.6 (0.5, 0.9) | 0.006 |
| Child illness * | ||||||
| No | 1500 | 316 (21.1) | 1 | 1 | ||
| Yes | 360 | 142 (39.4) | 2.4 (1.9, 3.1) | <0.01 | 2.3 (1.7, 3.0) | <0.001 |
| SES | ||||||
| Low | 500 | 126 (25.2) | 1 | |||
| Medium | 505 | 121 (24.0) | 0.9 (0.7, 1.2) | 0.598 | ||
| High | 487 | 120 (24.6) | 1.0 (0.7, 1.3) | 0.773 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mgongo, M.; Chotta, N.A.S.; Hashim, T.H.; Uriyo, J.G.; Damian, D.J.; Stray-Pedersen, B.; Msuya, S.E.; Wandel, M.; Vangen, S. Underweight, Stunting and Wasting among Children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 509. https://doi.org/10.3390/ijerph14050509
Mgongo M, Chotta NAS, Hashim TH, Uriyo JG, Damian DJ, Stray-Pedersen B, Msuya SE, Wandel M, Vangen S. Underweight, Stunting and Wasting among Children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2017; 14(5):509. https://doi.org/10.3390/ijerph14050509
Chicago/Turabian StyleMgongo, Melina, Nikolas A. S. Chotta, Tamara H. Hashim, Jacqueline G. Uriyo, Damian J. Damian, Babill Stray-Pedersen, Sia E. Msuya, Margareta Wandel, and Siri Vangen. 2017. "Underweight, Stunting and Wasting among Children in Kilimanjaro Region, Tanzania; a Population-Based Cross-Sectional Study" International Journal of Environmental Research and Public Health 14, no. 5: 509. https://doi.org/10.3390/ijerph14050509





