A Multiyear Model of Influenza Vaccination in the United States
Abstract
:1. Introduction
2. Methods
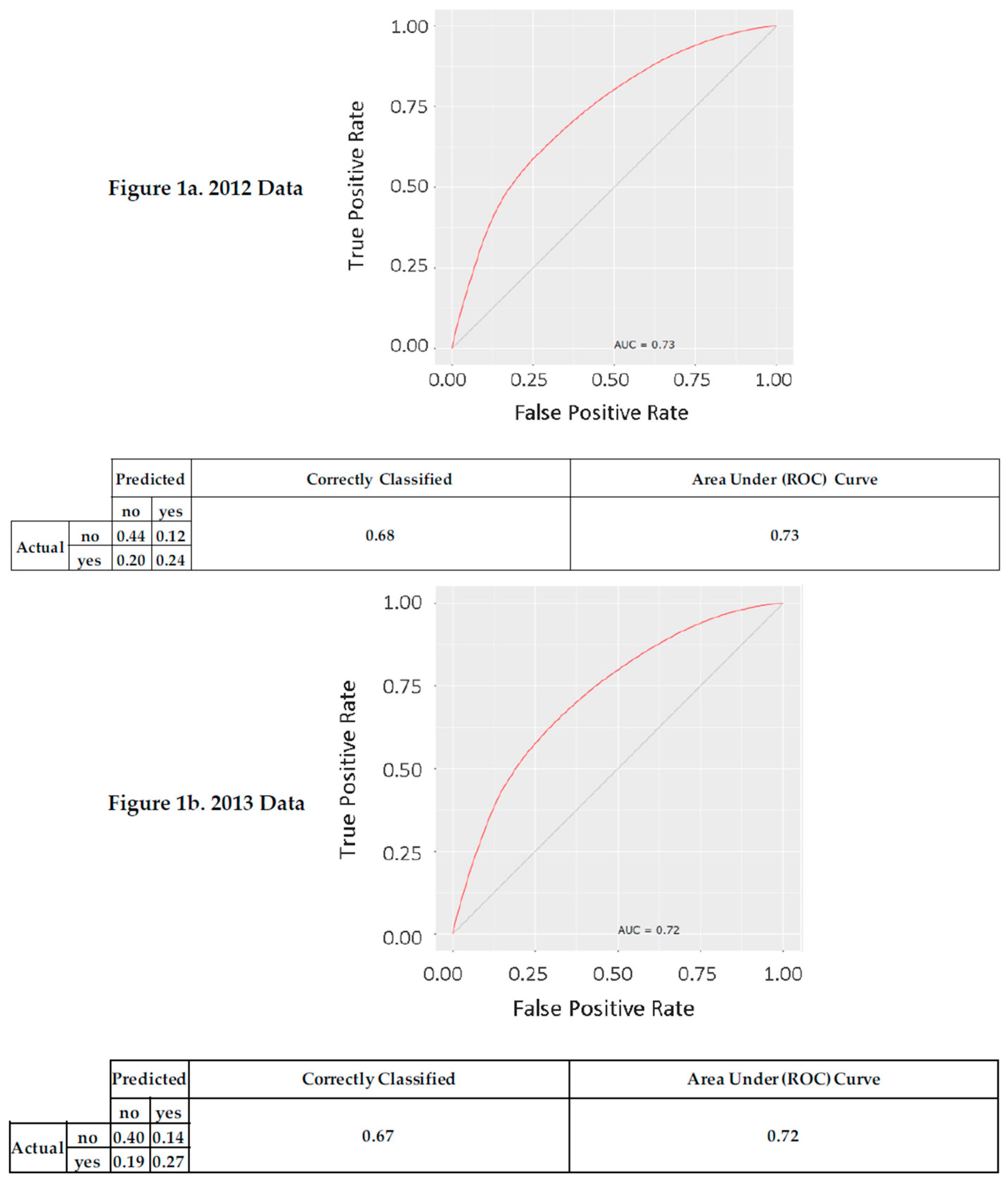
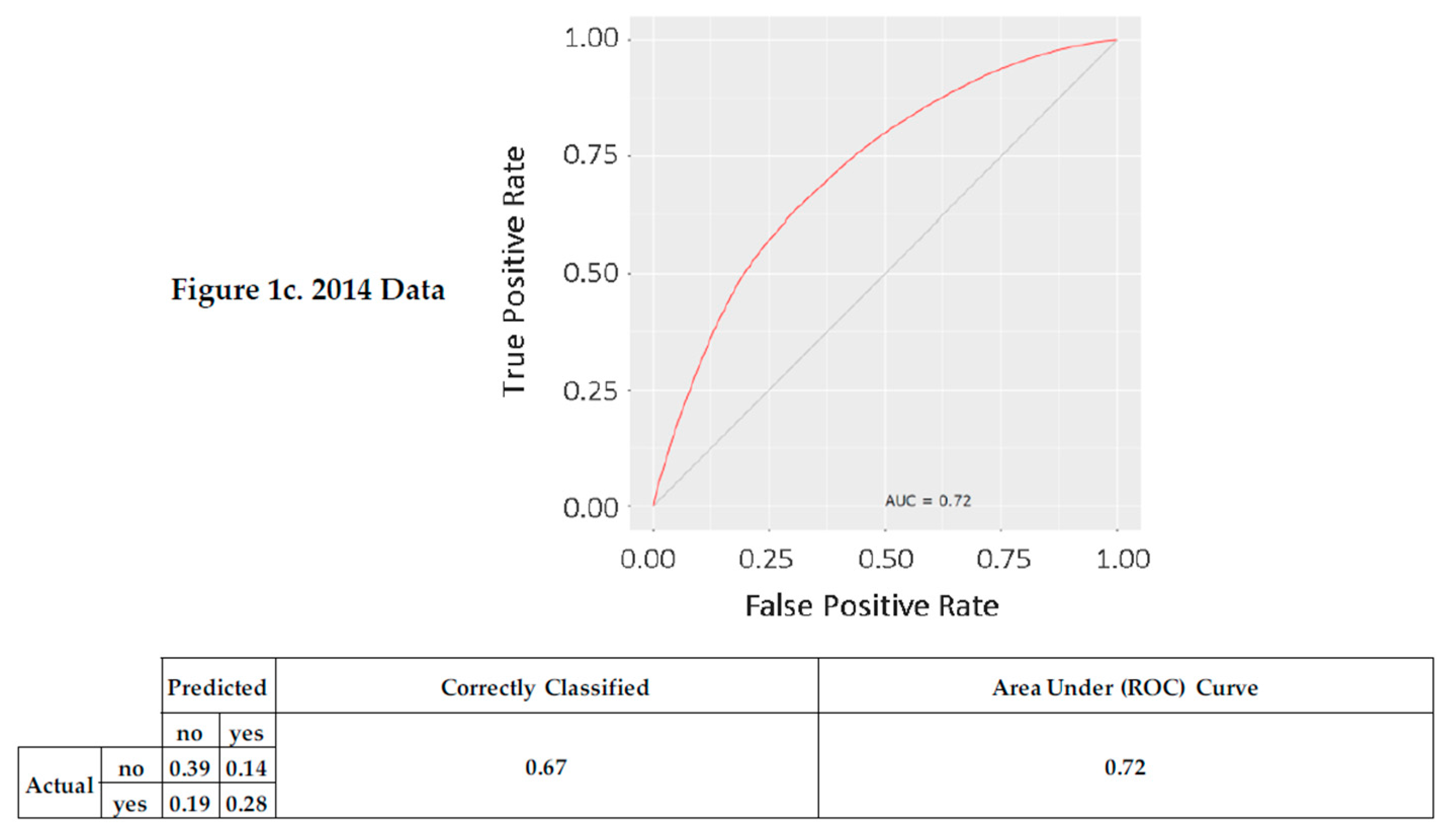
3. Results
4. Discussion
Implications and Future Research
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Gangarosa, E.J.; Galazka, A.; Wolfe, C.; Phillips, L.; Miller, E.; Chen, R.; Gangarosa, R. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361. [Google Scholar] [CrossRef]
- Majumder, M.S.; Cohn, E.L.; Mekaru, S.R.; Huston, J.E.; Brownstein, J.S. Substandard vaccination compliance and the 2015 measles outbreak. JAMA Pediatr. 2015, 169, 494–495. [Google Scholar] [CrossRef] [PubMed]
- Influenza (Flu). Available online: https://www.cdc.gov/flu/index.htm (accessed on 26 July 2017).
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of influenza vaccination intention and behavior—A systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.K.; Sebaldt, R.J.; Lohfeld, L.; Goeree, R.; Donald, F.C.; Burgess, K.; Kaczorowski, J. Practice and physician characteristics associated with influenza vaccination delivery rates following a patient reminder letter intervention. J. Prim. Prev. 2008, 29, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, N.D.; Kwitel, A.; McCaul, K.D.; Magnan, R.E.; Gerrard, M.; Gibbons, F.X. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychol. 2007, 26, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data, 2012–2014. Available online: http://www.cdc.gov/brfss/ (accessed on 26 July 2017).
- Ng, A.Y. Preventing “Overfitting” of Cross-Validation Data. Proccdings of the International Conference on Machine Learning, San Francisco, CA, USA, 8–12 July 1997. [Google Scholar]
- Fitzmaurice, G.M.; Laird, N.M. Binary response models and logistic regression. In International Encyclopedia of the Social & Behavioral Sciences; Elsevier: Amsterdam, The Netherlands, 2015; pp. 587–595. [Google Scholar]
- Behavioral Risk Factor Surveillance System Survey Questionnaire. Available online: http://www.cdc.gov/brfss/questionnaires/index.htm (accessed on 26 July 2017).
- Molinari, N.A.; Ortega-Sanchez, I.R.; Messonnier, M.L.; Thompson, W.W.; Wortley, P.M.; Weintraub, E.; Bridges, C.B. The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine 2007, 25, 5086–5096. [Google Scholar] [CrossRef] [PubMed]
- Nichol, K.L.; Nordin, J.; Mullooly, J.; Lask, R.; Fillbrandt, K.; Iwane, M. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N. Engl. J. Med. 2003, 348, 1322–1332. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.K.; McNeil, S.; Merry, H.; Rockwood, K. Rates of influenza vaccination in older adults and factors associated with vaccine use: A secondary analysis of the Canadian Study of Health and Aging. BMC Public Health 2004, 4, 36–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smeeth, L.; Thomas, S.L.; Hall, A.J.; Hubbard, R.; Farrington, P.; Vallance, P. Risk of myocardial infarction and stroke after acute infection or vaccination. N. Engl. J. Med. 2004, 351, 2611–2618. [Google Scholar] [CrossRef] [PubMed]
- Nagata, J.M.; Hernández-Ramos, I.; Kurup, A.S.; Albrecht, D.; Vivas-Torrealba, C.; Franco-Paredes, C. Social determinants of health and seasonal influenza vaccination in adults >65 years: A systematic review of qualitative and quantitative data. Public Health 2013, 13, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Grohskopf, L.A.; Sokolow, L.Z.; Broder, K.R.; Olsen, S.J.; Karron, R.A.; Jernigan, D.B.; Bresee, J.S. Prevention and Control of Seasonal Influenza with Vaccines Recommendations of the Advisory Committee on Immunization Practices—United States, 2016-17 Influenza Season; Recommendations and Reports 2016. Available online: https://www.cdc.gov/mmwr/volumes/65/rr/rr6505a1.htm (accessed on 3 July 2017).
- Jefferson, T.; Rudin, M.; di Pietrantonj, C.; Rivetti, D.; Rivetti, A.; Demicheli, V. Efficacy and effectiveness of influenza vaccines in elderly people: A systematic review. Lancet 2005, 336, 1165–1174. [Google Scholar] [CrossRef]
- Hamilton, J.G. Needle phobia: A neglected diagnosis. J. Fam. Pract. 1995, 41, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Key Facts About Seasonal Flu Vaccine. 2016. Available online: http://www.cdc.gov/flu/protect/keyfacts.htm (accessed on 26 July 2017).
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Morris, M.G. Why don’t men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS Quart. 2000, 24, 115–139. [Google Scholar] [CrossRef]
- Paris, L.A.H. Stopping Behavior: User Persistence in Online Searching and Its Relation to Optimal Cutoff Points for Information Retrieval Systems. Ph.D. Thesis, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, 1998. [Google Scholar]
- Davis, T.C.; Crouch, M.A.; Wills, G.; Miller, S.; Abdehou, D.M. The gap between patient reading comprehension and the readability of patient education materials. J. Fam. Pract. 1990, 31, 533. [Google Scholar] [PubMed]
- Brisson, M.; Edmunds, W.J. Economic evaluation of vaccination programs: The impact of herd-immunity. Med. Decis. Mak. 2003, 23, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; May, R.M. Vaccination and herd immunity to infectious diseases. Nature 1985, 318, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Bridges, C.B.; Thompson, W.W.; Meltzer, M.I.; Reeve, G.R.; Talamonti, W.J.; Cox, N.J.; Lilac, H.A.; Hall, H.; Klimov, A.; Fukuda, K. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA 2000, 284, 1655–1663. [Google Scholar] [CrossRef] [PubMed]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef] [PubMed]
- Kahneman, D.; Tversky, A. Prospect theory: An analysis of decision under risk. Econometrica 1979, 47, 263291. [Google Scholar] [CrossRef]
- Pierannunzi, C.; Hu, S.S.; Balluz, L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med. Res. Methodol. 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, R.; Baken, L.; Nelson, A.; Nichol, K.L. Validation of self-report of influenza and pneumococcal vaccination status in elder outpatients. Am. J. Prev. Med. 1999, 16, 173–177. [Google Scholar] [CrossRef]
- Kana'iaupuni, S.M.; Donato, K.M.; Thompson-Colón, T.; Stainback, M. Counting on kin: Social networks, social support, and child health status. Soc. Forces 2005, 83, 1137–1164. [Google Scholar] [CrossRef]
- Smith, K.P.; Christakis, N.A. Social networks and health. Annu. Rev. Sociol. 2008, 34, 405–429. [Google Scholar] [CrossRef]
- Cheung, K.W.; Mak, Y.W. Association between psychological flexibility and health beliefs in the uptake of influenza vaccination among people with chronic respiratory diseases in Hong Kong. Int. J. Environ. Res. Public Health 2016, 23, 155. [Google Scholar] [CrossRef] [PubMed]
- Nyhan, B.; Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 2015, 33, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Silver, N. The Signal and the Noise: Why So Many Predictions Fail—But Some Don't; Penguin Books: London, UK, 2015. [Google Scholar]
| Variable | Definition/Question Asked [11] |
|---|---|
| Influenza Vaccination (response) | During the past 12 months, have you had either a flu shot or a flu vaccine? |
| Age | [What is your] age in years? |
| Pneumococcal Vaccination | A pneumonia shot (or pneumococcal vaccine) is usually given only once or twice in a person’s lifetime and is different from the flu shot. Have you ever had a pneumonia shot? |
| Time Since Last Checkup | About how long has it been since you last visited a doctor for a routine checkup? [A routine checkup is a general physical exam, not an exam for a specific injury, illness, or condition.] |
| Highest Level of Education Attained | [What is your highest] level of education completed? |
| Employment | Are you currently Employed for wages, Self-employed…? |
| Health Care Coverage | Do you have any kind of health care coverage, including health insurance, prepaid plans such as Health Maintenance Organizations, or government plans such as Medicare, or Indian Health Service? |
| Number of Personal Doctors | Do you have one person you think of as your personal doctor or health care provider? (If “No” ask “Is there more than one or is there no person who you think of as your personal doctor or health care provider?”) |
| Smoking Status | Four-level smoker status: Everyday smoker, Someday smoker, Former smoker, Non-smoker |
| Annual Household Income | [What] is your annual household income from all sources…: (If respondent refuses at any income level, code “Refused”.) |
| 2012 | 2013 | 2014 | |||||
|---|---|---|---|---|---|---|---|
| Variable | Category | Freq. | Perc. | Freq. | Perc. | Freq. | Perc. |
| Pneumococcal Vaccination | Yes | 159,557 | 34.40 | 161,784 | 35.61 | 163,282 | 36.97 |
| No | 261,728 | 56.43 | 245,512 | 54.03 | 239,089 | 54.13 | |
| Don’t Know/Not Sure | 40,018 | 8.63 | 44,318 | 9.75 | 37,165 | 8.41 | |
| Refused | 2543 | 0.55 | 2770 | 0.61 | 2184 | 0.49 | |
| Time Since Last Checkup | Within past year | 341,897 | 71.87 | 356,253 | 72.44 | 340,587 | 73.30 |
| Within past 2 years | 56,165 | 11.81 | 57,338 | 11.66 | 53,668 | 11.55 | |
| Within past 5 years | 33,603 | 7.06 | 33,659 | 6.84 | 30,764 | 6.62 | |
| 5 or more years ago | 33,267 | 6.99 | 33,717 | 6.86 | 29,293 | 6.30 | |
| Don’t know/Not sure | 5677 | 1.19 | 5743 | 1.17 | 5601 | 1.21 | |
| Never | 4655 | 0.98 | 4523 | 0.92 | 4047 | 0.87 | |
| Refused | 422 | 0.09 | 540 | 0.11 | 702 | 0.15 | |
| Highest Level of Education Attained | Did not graduate High School | 42,351 | 8.90 | 42,132 | 8.57 | 37,003 | 7.96 |
| Graduated High school | 139,501 | 29.33 | 142,953 | 29.07 | 131,325 | 28.26 | |
| Attended College/Technical School | 128,404 | 26.99 | 134,242 | 27.30 | 125,635 | 27.04 | |
| Graduated College/Technical School | 163,510 | 34.37 | 170,173 | 34.60 | 166,972 | 35.93 | |
| Don’t know/Not sure/Missing | 1921 | 0.40 | 2273 | 0.46 | 3,729 | 0.80 | |
| Employment | Employed for wages | 196,289 | 41.31 | 202,169 | 41.17 | 189,219 | 40.93 |
| Self-employed | 38,863 | 8.18 | 39,853 | 8.11 | 39,102 | 8.46 | |
| Out of work for more than 1 year | 14,409 | 3.03 | 14,081 | 2.87 | 10,759 | 2.33 | |
| Out of work for less than 1 year | 12,312 | 2.59 | 12,241 | 2.49 | 9755 | 2.11 | |
| A homemaker | 31,587 | 6.65 | 31,654 | 6.45 | 29,028 | 6.28 | |
| A student | 12,225 | 2.57 | 12,664 | 2.58 | 11,021 | 2.38 | |
| Retired | 132,138 | 27.81 | 138,311 | 28.16 | 136,639 | 29.56 | |
| Unable to work | 35,260 | 7.42 | 37,419 | 7.62 | 34,021 | 7.36 | |
| Refused | 2053 | 0.43 | 2713 | 0.55 | 2,703 | 0.58 | |
| Health Care Coverage | Yes | 419,328 | 88.15 | 434,627 | 88.38 | 425,198 | 91.51 |
| No | 54,801 | 11.52 | 55,242 | 11.23 | 37,642 | 8.10 | |
| Don‘t Know/Not Sure | 932 | 0.20 | 1023 | 0.21 | 934 | 0.20 | |
| Refused | 624 | 0.13 | 881 | 0.18 | 890 | 0.19 | |
| Number of Personal Doctor(s) | 1 Personal Doctor | 365,483 | 76.83 | 369,084 | 75.05 | 354,623 | 76.32 |
| 2+ Personal Doctors | 38,854 | 8.17 | 41,306 | 8.40 | 37,199 | 8.01 | |
| No Personal Doctor | 69,855 | 14.69 | 79,587 | 16.18 | 70,891 | 15.26 | |
| Don’t know/Not Sure | 1088 | 0.23 | 1176 | 0.24 | 1271 | 0.27 | |
| Refused | 406 | 0.09 | 620 | 0.13 | 679 | 0.15 | |
| Smoking Status | Every Day | 54,940 | 11.55 | 55,157 | 11.22 | 47,122 | 10.14 |
| Some Days | 21,160 | 4.45 | 21,455 | 4.36 | 19,242 | 4.14 | |
| Former Smoker | 135,426 | 28.47 | 138,218 | 28.11 | 128,629 | 27.68 | |
| Never | 254,492 | 53.50 | 261,621 | 53.20 | 248,500 | 53.48 | |
| Don’t know/Refused/Missing | 9669 | 2.03 | 15,322 | 3.12 | 21,171 | 4.56 | |
| Annual Household Income | ≤$10,000 | 25,237 | 5.31 | 25,411 | 5.18 | 21,199 | 4.60 |
| $10,000–$15,000 | 26,406 | 5.56 | 26,759 | 5.45 | 22,943 | 4.98 | |
| $15,000–$20,000 | 34,081 | 7.18 | 34,885 | 7.11 | 30,511 | 6.63 | |
| $20,000–$25,000 | 40,384 | 8.50 | 41,738 | 8.50 | 37,531 | 8.15 | |
| $25,000–$35,000 | 47,352 | 9.97 | 48,863 | 9.95 | 44,315 | 9.62 | |
| $35,000–$50,000 | 59,877 | 12.61 | 61,506 | 12.53 | 57,418 | 12.47 | |
| $50,000–$75,000 | 63,951 | 13.47 | 65,238 | 13.29 | 62,175 | 13.50 | |
| ≥$75,000 | 111,654 | 23.51 | 115,982 | 23.63 | 117,176 | 25.45 | |
| Don’t know/Not sure | 33,034 | 6.96 | 34,946 | 7.12 | 31,622 | 6.87 | |
| Refused | 32,961 | 6.94 | 35,559 | 7.24 | 35,553 | 7.72 | |
| Influenza Vaccination | Yes | 202,640 | 43.61 | 208,387 | 45.79 | 205,328 | 46.41 |
| No | 258,088 | 55.55 | 242,939 | 53.38 | 233,769 | 52.84 | |
| Don’t Know/Not Sure | 1399 | 0.30 | 959 | 0.21 | 1158 | 0.26 | |
| Refused | 2519 | 0.54 | 2791 | 0.61 | 2179 | 0.49 | |
| 2012 Logistic Regression Deviance | 2012 Logistic Regression Deviance Rank | 2013 Logistic Regression Deviance | 2013 Logistic Regression Deviance Rank | 2014 Logistic Regression Deviance | 2014 Logistic Regression Deviance Rank | 2012–2014 Logistic Regression Mean Deviance Rank | |
|---|---|---|---|---|---|---|---|
| Age | 17,739.3 | 1 | 16,378.7 | 1 | 15,230.7 | 1 | 1.0 |
| Pneumococcal Vaccination | 13,599.2 | 2 | 10,199.2 | 2 | 10,833.8 | 2 | 2.0 |
| Time Since Last Checkup | 8280.7 | 3 | 7738.6 | 3 | 7577.9 | 3 | 3.0 |
| Number of Personal Doctors | 1659.5 | 5 | 2014.3 | 4 | 1910.7 | 4 | 4.3 |
| Employment | 2244.6 | 4 | 1577.3 | 6 | 1749.8 | 5 | 5.0 |
| Annual Household Income | 1543.9 | 6 | 2013.3 | 5 | 1681.4 | 6 | 5.7 |
| Smoking Status | 680.7 | 8 | 785.3 | 7 | 772.3 | 8 | 7.7 |
| Health Care Coverage | 837.1 | 7 | 709.8 | 8 | 701 | 9 | 8.0 |
| Highest Education Level Attained | 616.5 | 9 | 707.6 | 9 | 773.2 | 7 | 8.3 |
| 2012 Logistic Regression | 2013 Logistic Regression | 2014 Logistic Regression | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chi−Square p−Value: | 0.000 | 0.000 | 0.000 | |||||||||||||||||||
| Pseudo R−Square (Optimistic): | 0.401 | 0.389 | 0.383 | |||||||||||||||||||
| Estimate | Std. Error | Odds Ratio | Odds Ratio 95% | Z Value | Pr(>|z|) | Estimate | Std. Error | Odds Ratio | Odds Ratio 95% | Z Value | Pr(>|z|) | Estimate | Std. Error | Odds Ratio | Odds Ratio 95% | Z Value | Pr(>|z|) | |||||
| (Intercept) | −0.562 | 0.034 | 0.570 | (0.533, 0.610) | −16.432 | <2 × 10−16 | *** | −0.613 | 0.036 | 0.542 | (0.505, 0.581) | −17.269 | <2 × 10−16 | *** | −0.478 | 0.036 | 0.620 | (0.578, 0.666) | −13.229 | <2 × 10−16 | *** | |
| Age | years | 0.014 | 0.000 | 1.014 | (1.013, 1.014) | 38.508 | <2 × 10−16 | *** | 0.015 | 0.000 | 1.015 | (1.014, 1.016) | 39.791 | <2 × 10−16 | *** | 0.013 | 0.000 | 1.013 | (1.013, 1.014) | 35.685 | <2 × 10−16 | *** |
| Pneumococcal Vaccination | yes (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| no | −1.120 | 0.010 | 0.326 | (0.320, 0.333) | −113.618 | <2 × 10−16 | *** | −1.008 | 0.010 | 0.365 | (0.358, 0.372) | −101.101 | <2 × 10−16 | *** | −1.025 | 0.010 | 0.359 | (0.352, 0.366) | −103.598 | <2 × 10−16 | *** | |
| Don’t Know/Not Sure | −0.739 | 0.017 | 0.478 | (0.463, 0.493) | −44.737 | <2 × 10−16 | *** | −0.785 | 0.016 | 0.456 | (0.442, 0.471) | −48.287 | <2 × 10−16 | *** | −0.611 | 0.017 | 0.543 | (0.525, 0.561) | −36.362 | <2 × 10−16 | *** | |
| Time Since Last Checkup | <1 year ago (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| 1–2 years ago | −0.374 | 0.014 | 0.688 | (0.670, 0.706) | −27.702 | <2 × 10−16 | *** | −0.334 | 0.014 | 0.716 | (0.697, 0.735) | −24.365 | <2 × 10−16 | *** | −0.347 | 0.014 | 0.707 | (0.688, 0.726) | −25.427 | <2 × 10−16 | *** | |
| 2–5 years ago | −0.573 | 0.018 | 0.564 | (0.544, 0.585) | −30.987 | <2 × 10−16 | *** | −0.547 | 0.019 | 0.579 | (0.558, 0.600) | −29.125 | <2 × 10−16 | *** | −0.580 | 0.019 | 0.560 | (0.539, 0.581) | −30.627 | <2 × 10−16 | *** | |
| 5+ years ago | −0.761 | 0.021 | 0.467 | (0.449, 0.487) | −36.933 | <2 × 10−16 | *** | −0.794 | 0.021 | 0.452 | (0.434, 0.471) | −37.771 | <2 × 10−16 | *** | −0.765 | 0.021 | 0.465 | (0.446, 0.485) | −35.590 | <2 × 10−16 | *** | |
| Never | −0.626 | 0.050 | 0.535 | (0.485, 0.589) | −12.622 | <2 × 10−16 | *** | −0.451 | 0.050 | 0.637 | (0.578, 0.702) | −9.064 | <2 × 10−16 | *** | −0.626 | 0.054 | 0.535 | (0.481, 0.594) | −11.701 | <2 × 10−16 | *** | |
| Highest Education Level Attained | <High School Grad. (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| High School Graduate | 0.028 | 0.017 | 1.029 | (0.995, 1.064) | 1.668 | 0.0953 | . | −0.037 | 0.018 | 0.964 | (0.931, 0.998) | −2.080 | 0.0375 | * | −0.061 | 0.018 | 0.941 | (0.908, 0.974) | −3.409 | 0.0007 | *** | |
| College/Tech. Sch. Attendee | 0.093 | 0.017 | 1.098 | (1.061, 1.136) | 5.342 | <0.0001 | *** | 0.029 | 0.018 | 1.030 | (0.994, 1.067) | 1.613 | 0.1068 | n.s | 0.003 | 0.018 | 1.003 | (0.968, 1.040) | 0.173 | 0.8625 | n.s. | |
| College/Tech. Sch. Graduate | 0.276 | 0.018 | 1.317 | (1.272, 1.365) | 15.371 | <2 × 10−16 | *** | 0.243 | 0.018 | 1.275 | (1.229, 1.322) | 13.121 | <2 × 10−16 | *** | 0.227 | 0.019 | 1.255 | (1.210, 1.302) | 12.106 | <2 × 10−16 | *** | |
| Employment | Employed for wages (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| Self−employed | −0.539 | 0.017 | 0.583 | (0.564, 0.603) | −31.471 | <2 × 10−16 | *** | −0.463 | 0.017 | 0.629 | (0.608, 0.651) | −26.805 | <2 × 10−16 | *** | −0.498 | 0.017 | 0.608 | (0.588, 0.628) | −29.488 | <2 × 10−16 | *** | |
| Out of work for >1 year | −0.265 | 0.028 | 0.768 | (0.727, 0.811) | −9.452 | <2 × 10−16 | *** | −0.166 | 0.029 | 0.847 | (0.801, 0.896) | −5.774 | <0.0001 | *** | −0.221 | 0.031 | 0.802 | (0.755, 0.852) | −7.120 | <0.0001 | *** | |
| Out of work for <1 year | −0.256 | 0.030 | 0.774 | (0.730, 0.822) | −8.472 | <2 × 10−16 | *** | −0.145 | 0.031 | 0.865 | (0.815, 0.919) | −4.728 | <0.0001 | *** | −0.140 | 0.032 | 0.870 | (0.816, 0.926) | −4.343 | <0.0001 | *** | |
| A homemaker | −0.164 | 0.018 | 0.849 | (0.819, 0.880) | −9.007 | <2 × 10−16 | *** | −0.139 | 0.019 | 0.870 | (0.839, 0.903) | −7.443 | <0.0001 | *** | −0.153 | 0.019 | 0.859 | (0.828, 0.891) | −8.152 | <0.0001 | *** | |
| A student | −0.042 | 0.030 | 0.958 | (0.904, 1.016) | −1.429 | 0.1531 | n.s. | 0.074 | 0.030 | 1.077 | (1.016, 1.142) | 2.481 | 0.0131 | * | 0.030 | 0.030 | 1.030 | (0.971, 1.094) | 0.985 | 0.3247 | n.s. | |
| Retired | −0.044 | 0.014 | 0.957 | (0.932, 0.983) | −3.253 | 0.0011 | ** | −0.028 | 0.014 | 0.972 | (0.946, 0.999) | −2.061 | 0.0393 | * | −0.024 | 0.014 | 0.976 | (0.950, 1.002) | −1.791 | 0.0733 | . | |
| Unable to work | −0.007 | 0.018 | 0.993 | (0.957, 1.029) | −0.392 | 0.6947 | n.s. | −0.013 | 0.019 | 0.987 | (0.951, 1.024) | −0.717 | 0.4731 | n.s | 0.005 | 0.019 | 1.005 | (0.969, 1.043) | 0.262 | 0.7936 | n.s. | |
| Health Care Coverage | yes (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| no | −0.481 | 0.017 | 0.618 | (0.598, 0.639) | −28.287 | <2 × 10−16 | *** | −0.454 | 0.017 | 0.635 | (0.614, 0.657) | −26.069 | <2 × 10−16 | *** | −0.515 | 0.020 | 0.598 | (0.575, 0.621) | −25.739 | <2 × 10−16 | *** | |
| Personal Doctor(s) | 1 Personal Doctor (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| 2+ Personal Doctors | 0.043 | 0.015 | 1.044 | (1.013, 1.075) | 2.838 | 0.0045 | ** | 0.004 | 0.015 | 1.004 | (0.974, 1.034) | 0.254 | 0.7996 | n.s | −0.013 | 0.015 | 0.987 | (0.958, 1.017) | −0.840 | 0.4007 | n.s. | |
| No Personal Doctor | −0.434 | 0.015 | 0.648 | (0.629, 0.667) | −29.049 | <2 × 10−16 | *** | −0.421 | 0.014 | 0.657 | (0.639, 0.675) | −29.366 | <2 × 10−16 | *** | −0.431 | 0.014 | 0.650 | (0.632, 0.668) | −29.831 | <2 × 10−16 | *** | |
| Smoking Status | Every Day (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| Some Days | 0.093 | 0.024 | 1.097 | (1.046, 1.151) | 3.804 | 0.0001 | *** | 0.126 | 0.025 | 1.134 | (1.080, 1.191) | 5.057 | <0.0001 | *** | 0.068 | 0.025 | 1.070 | (1.018, 1.124) | 2.683 | 0.0073 | ** | |
| Former Smoker | 0.313 | 0.016 | 1.367 | (1.326, 1.410) | 20.136 | <2 × 10−16 | *** | 0.348 | 0.016 | 1.416 | (1.372, 1.461) | 21.796 | <2 × 10−16 | *** | 0.319 | 0.016 | 1.376 | (1.333, 1.421) | 19.711 | <2 × 10−16 | *** | |
| Never | 0.282 | 0.015 | 1.325 | (1.288, 1.364) | 19.269 | <2 × 10−16 | *** | 0.316 | 0.015 | 1.372 | (1.332, 1.413) | 21.103 | <2 × 10−16 | *** | 0.316 | 0.015 | 1.372 | (1.331, 1.413) | 20.684 | <2 × 10−16 | *** | |
| Annual Household Income | ≤$10,000 (ref. cat.) | 0.000 | 0.000 | 0.000 | ||||||||||||||||||
| $10,000–$15,000 | 0.070 | 0.026 | 1.073 | (1.019, 1.130) | 2.659 | 0.0078 | ** | 0.003 | 0.027 | 1.003 | (0.951, 1.058) | 0.120 | 0.9047 | n.s | 0.007 | 0.028 | 1.007 | (0.953, 1.065) | 0.253 | 0.8005 | n.s. | |
| $15,000–$20,000 | 0.084 | 0.025 | 1.088 | (1.035, 1.143) | 3.325 | 0.0009 | *** | 0.053 | 0.026 | 1.054 | (1.002, 1.109) | 2.025 | 0.0429 | * | 0.049 | 0.027 | 1.050 | (0.996, 1.107) | 1.822 | 0.0684 | . | |
| $20,000–$25,000 | 0.089 | 0.025 | 1.093 | (1.041, 1.147) | 3.596 | 0.0003 | *** | 0.083 | 0.025 | 1.087 | (1.034, 1.142) | 3.301 | 0.0010 | *** | 0.043 | 0.026 | 1.044 | (0.992, 1.099) | 1.643 | 0.1004 | n.s. | |
| $25,000–$35,000 | 0.154 | 0.024 | 1.167 | (1.113, 1.224) | 6.355 | <0.0001 | *** | 0.097 | 0.025 | 1.102 | (1.050, 1.157) | 3.915 | 0.0001 | *** | 0.076 | 0.026 | 1.079 | (1.026, 1.135) | 2.966 | 0.0030 | ** | |
| $35,000–$50,000 | 0.130 | 0.024 | 1.139 | (1.087, 1.194) | 5.489 | <0.0001 | *** | 0.141 | 0.024 | 1.152 | (1.098, 1.208) | 5.819 | <0.0001 | *** | 0.114 | 0.025 | 1.120 | (1.067, 1.177) | 4.531 | <0.0001 | *** | |
| $50,000–$75,000 | 0.190 | 0.024 | 1.210 | (1.154, 1.268) | 7.969 | <0.0001 | *** | 0.197 | 0.024 | 1.218 | (1.161, 1.278) | 8.093 | <0.0001 | *** | 0.157 | 0.025 | 1.170 | (1.114, 1.229) | 6.254 | <0.0001 | *** | |
| ≥$75,000 | 0.337 | 0.023 | 1.401 | (1.339, 1.466) | 14.527 | <2 × 10−16 | *** | 0.369 | 0.024 | 1.447 | (1.381, 1.515) | 15.592 | <2 × 10−16 | *** | 0.312 | 0.024 | 1.366 | (1.302, 1.432) | 12.811 | <2 × 10−16 | *** | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamis, A.; Zhang, Y.; Kamis, T. A Multiyear Model of Influenza Vaccination in the United States. Int. J. Environ. Res. Public Health 2017, 14, 849. https://doi.org/10.3390/ijerph14080849
Kamis A, Zhang Y, Kamis T. A Multiyear Model of Influenza Vaccination in the United States. International Journal of Environmental Research and Public Health. 2017; 14(8):849. https://doi.org/10.3390/ijerph14080849
Chicago/Turabian StyleKamis, Arnold, Yuji Zhang, and Tamara Kamis. 2017. "A Multiyear Model of Influenza Vaccination in the United States" International Journal of Environmental Research and Public Health 14, no. 8: 849. https://doi.org/10.3390/ijerph14080849




