Dynamics of Implementation and Maintenance of Organizational Health Interventions
Abstract
1. Introduction
- Economic impact of obesity: The obesity epidemic has a potential economic impact in the U.S. Overall health expenditures in the U.S. from 2009 to 2012 were 17.7% of the GDP, the highest rate among 221 countries and more than twice the average for all countries (6.9%) [6]. The economic impacts associated with the obesity epidemic include medical, productivity, transportation, and human capital costs, which makes obesity-linked costs a noticeable portion of total national health expenditures [7,8].
- Complexity of organizational health interventions: Social systems are complex and implementing health related interventions within organizations is specifically complex [9,10]. Such interventions require changes in work processes that are often in a complex zone where uncertainty and lack of agreement are common [11]. We particularly select interventions involving multiple stakeholders, and this selection further increases the organizational complexity of implementation and maintenance of interventions.
- Endogenous dynamics: The selected intervention programs provide health organizations with capabilities that have the potential to tackle obesity in a target population and provide additional benefits. A general belief is that the level of these capabilities (e.g., capabilities achieved by installing an outdoor playground in a child daycare center) is degraded over time and irrespective of other factors, but recent theories in the strategic management literature present the idea that such erosion could also be a result of systematic and endogenous dynamics within the organization [12]. These theories contend that, in addition to exogenous factors, capabilities can erode based on endogenous dynamics, which can take an organization from efficient to inferior capabilities. These endogenous dynamics could result from unfavorable temporal trade-offs between performance and robustness and long delays between the “better” and “worse” parts of temporal trade-offs [12].
- Multiple stakeholders: Health organizations often have multiple stakeholders [13,14,15], making it difficult to trace the shortcomings of dynamics of implementation and maintenance of obesity interventions and tease out the sources of those shortcomings. Multiple stakeholders not only have different goals and perceptions, but their goals and perceptions may also change dynamically over time [16]. The organizational sciences literature also shows that there is often no agreement in perceptions of success factors among stakeholders (e.g., see Davis [17]). In addition, research shows that the allocation of clear stakeholder responsibilities is often problematic (e.g., [18]). We contend that even if stakeholder roles and responsibilities are clearly defined in the development of interventions, other pitfalls in organizational processes driven by endogenous dynamics may turn cooperative or complementary interactions into conflicting interactions, which can potentially cause the erosion of intervention components. The organizational literature also stresses the importance of interactions and communication among stakeholders, but without an understanding of the underlying dynamics of such interactions, it would be hard to assess the consequences of insufficient interactions. In fact, the literature shows that even simple organizational systems, if they include time delays and multiple feedback relationships, can create complicated outcomes, which therefore become hard to anticipate via intuition [19].
- Trade-offs in building alternative resources: There are usually trade-offs in building alternative resources that increase the complexity of managers’ decisions for allocating effort to those resource investment [20]. For example, organizations are susceptible to focusing on doing what they know best and ignoring emerging opportunities [21,22]. They also routinely undervalue investments with long-term payoffs [23,24]. Empirical studies provide strong support for many quality and process improvement programs [25,26]. However, organizations often fail to fully realize these benefits because: resources are withdrawn from programs before complete results are observed; initial enthusiasm overwhelms the training capacity for keeping the programs effective; or seeking short-term gains overloads the system with demand and the organizations are pushed into a firefighting mode of operation [27,28,29,30]. Similar to process improvement initiatives, many organizational health interventions may be beneficial over the long haul, but require initial investments and delays before the benefits materialize.
2. Study Design and Empirical Setting
2.1. Shape North Carolina (Shape NC)
2.2. Healthy Food Environments in Hospitals (HFEH)
2.3. Baltimore Healthy Carry-Outs (BHC)
3. Data and Methods
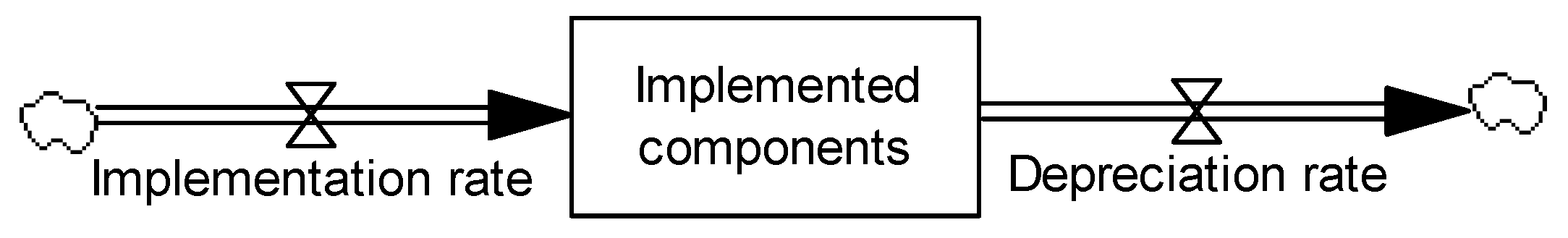
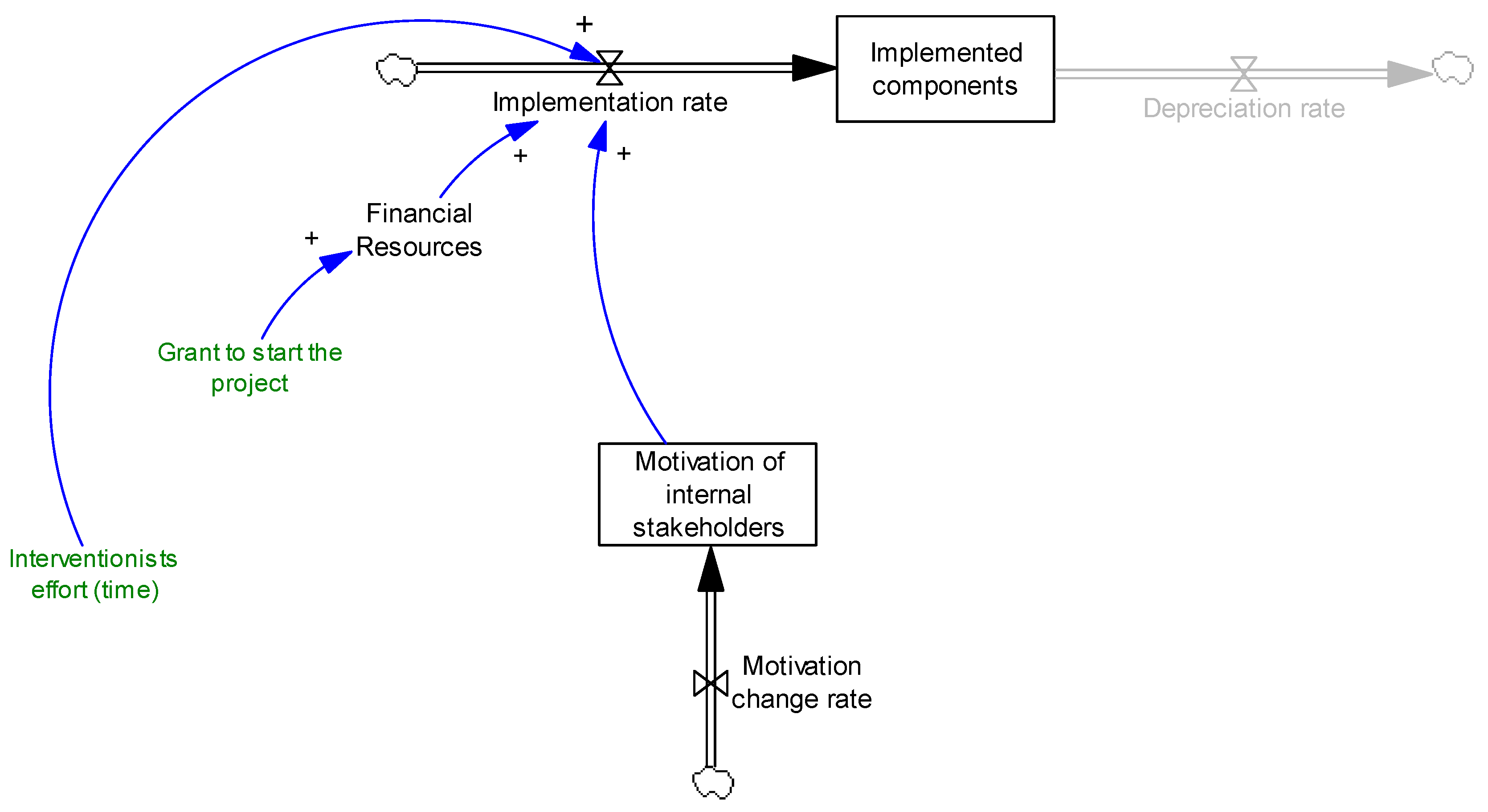
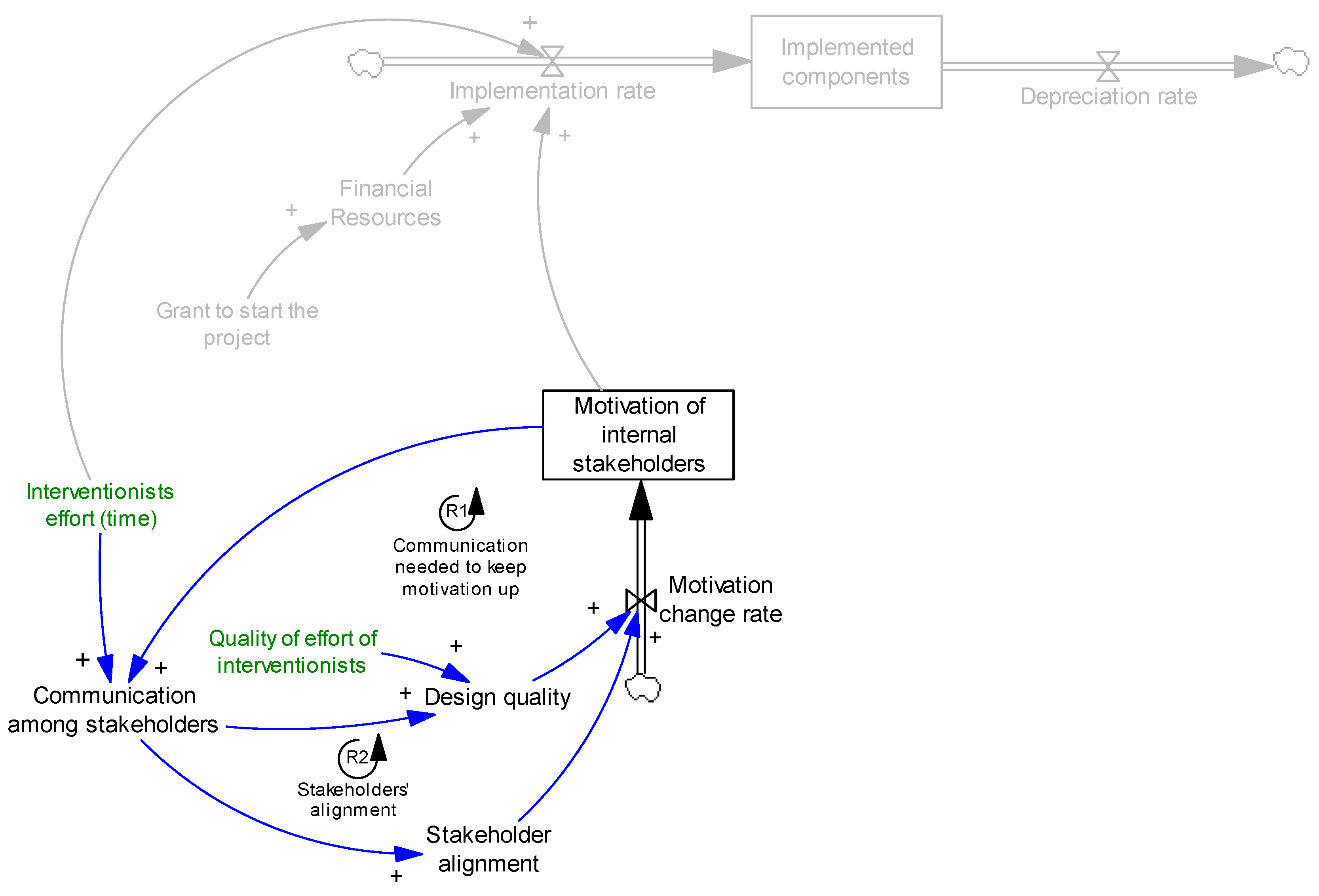
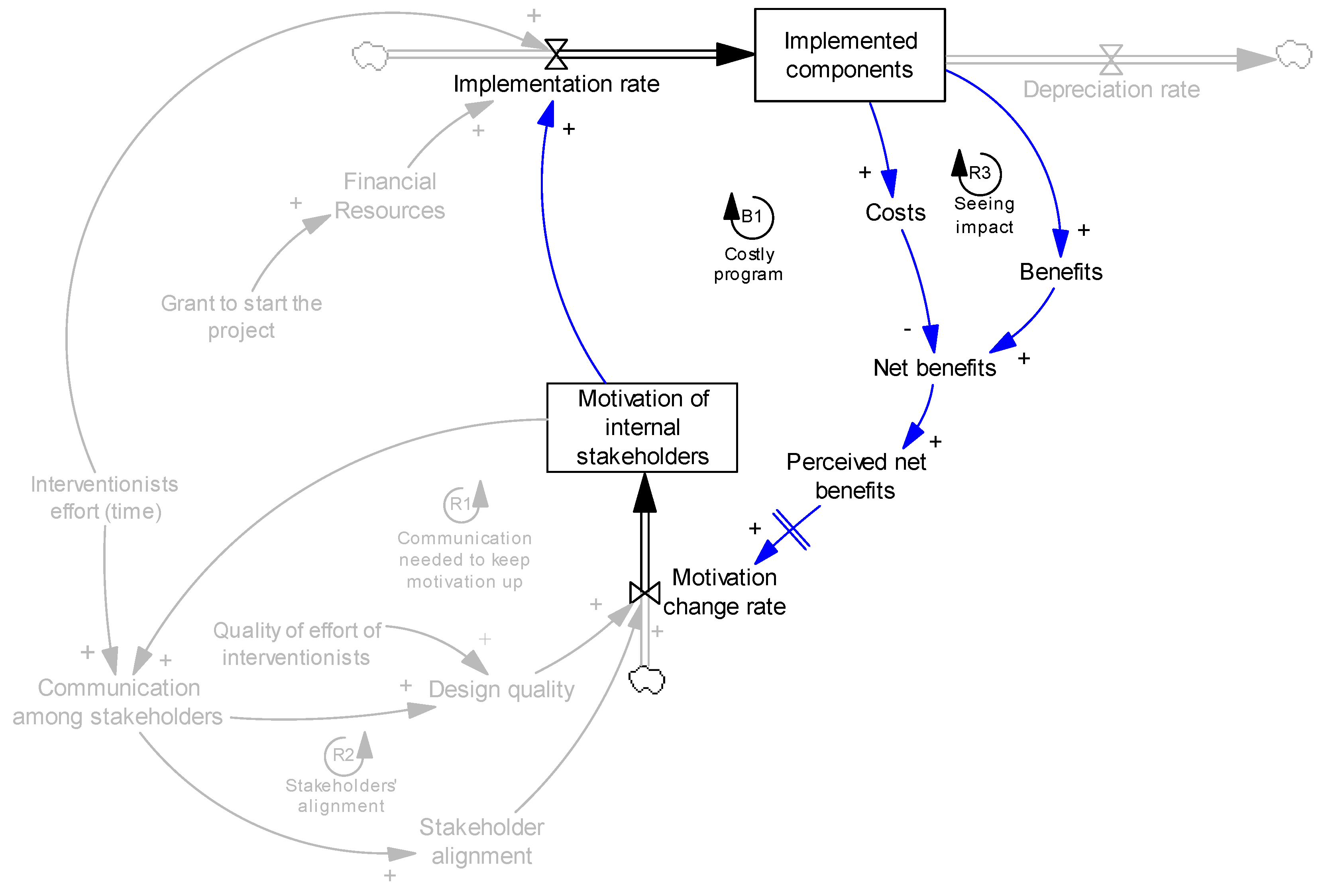
4. Modeling
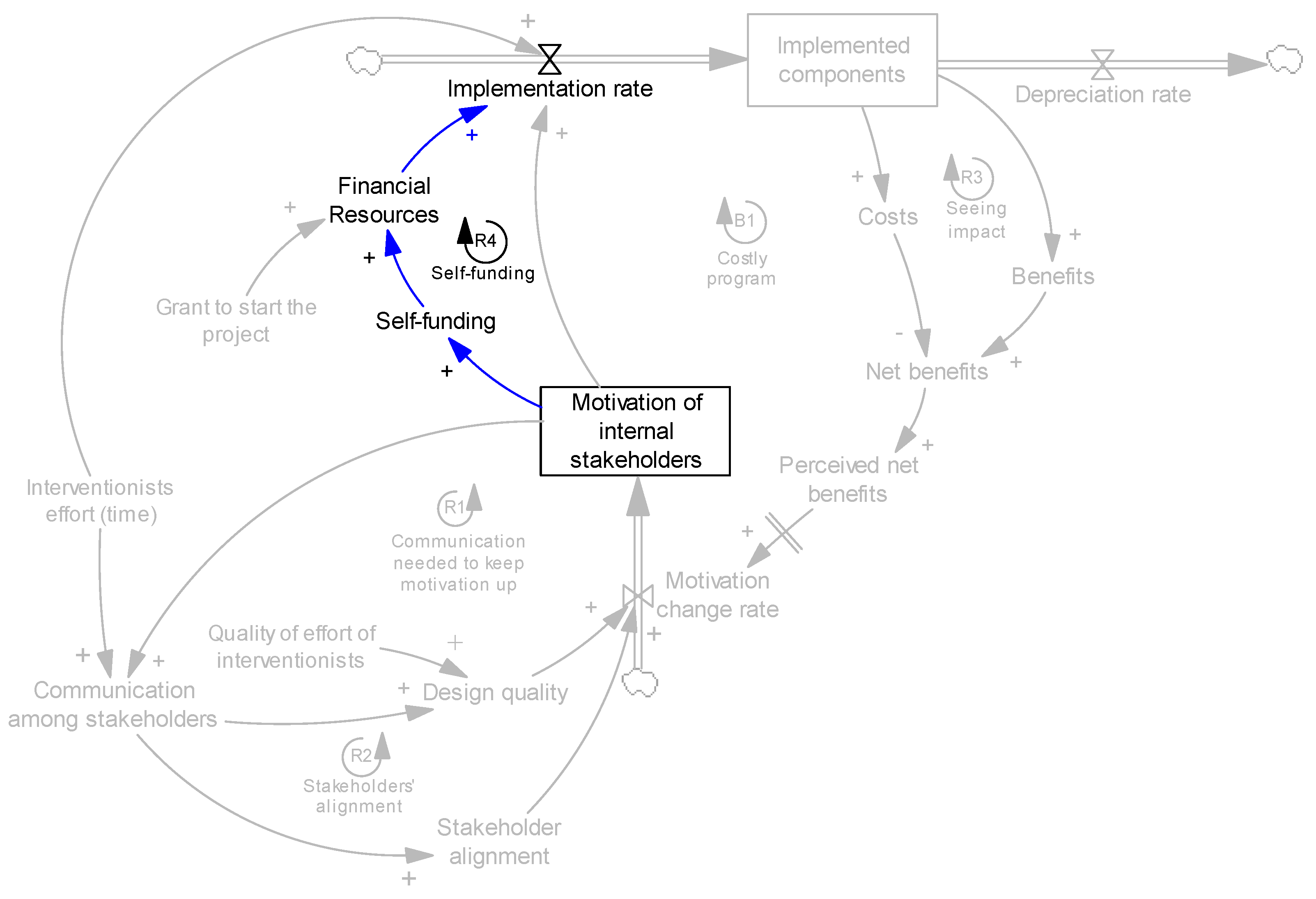
4.1. Resources and Motivation
4.1.1. Shape NC
Financially, the first grant was $3000 which helped us get started. We won't have been able to get started if we didn't have that little push.
Forever we have always tried to get a leg up on other centers, because we felt like in order to get the children, we needed to be something a little different.
Sometimes it comes from—not because she knew about it but because she came to a meeting and someone else said this is what we are doing. So then she'll go out and figure out how to get that done in her center, so it is kind of that competitive. Her competitiveness is motivating her to do more… She is competitive. That is the first thing that comes to my mind when I think of Ms. [A.]. She was lower stars and she didn't care about increasing her stars [an assessment measure for the centers], because she knew she already had quality, she didn't care about the star rating system, but when that NC pre-k program came, she was like, what!? And sure enough she got it together. They had to apply to be the model early learning site—she made sure she had every piece that had to be in it. So she competed with 5 or 6 centers that applied and she made sure she had everything above what they could do so she could be that model learning center. So that competitive nature.
4.1.2. Healthy Food Environments in Hospitals (HFEH)
I think they [interventionists] have been pretty helpful. There are a lot of things that we’ve done on our own. But we’ve used them as just an extra piece. I think we will continue to use it a lot more, because I know they built the toolkit, they’ve built a lot more resources, they have lots of webinars that they provide, and I think just continuing to communicate that to the rest of our staff internally so they know it’s there. I think it’s going to be helpful, because you don’t have to reinvent the wheel every time.
…we all felt it was the right thing to do. And I think quite frankly you don’t want to be the hospital that is not on the map, because they have a map of North Carolina that shows the hospitals that are and that aren’t [involved in the wellness program, the intervention]. I think if you were the leadership of the hospitals that aren’t, I think it might put some pressure on you to be the ones that are. Does that make sense? Because one of the things I learned about healthcare, I got into healthcare about ten year ago. I never realized really how competitive it is. It is very competitive. So you don’t want to be the hospital that’s in the market that doesn’t promote wellness because the one down the street is.
…one thing that we are doing now more than in the early days, and this is part of our attempt or work to move from just the hospital, to expand from the hospital sector to other sectors. So now we are working to bring the program to whole communities. We look at the hospital to become an anchor for that community.
I think we had a real commitment. As a community hospital, we very much want to represent to our community a healthy way of living, and we thought it is important to I guess be a mirror to our community. So it was important to our CEO, it was important to our wellness leadership that we partner with NC Prevention Partners to make a statement and to give us a pathway to becoming a healthier organization and being healthier for our customers.
…getting the directors on board with the staff and saying, ‘Hey, look, this is gonna launch. This is gonna benefit you.’ I think that’s the only way we can upscale it, because if you just email people, ‘Oh, this is happening, such and such.’ Okay, they most of the time just delete it...
…having a strong leader who is willing to do what it takes and be inspirational and motivating and facilitating into the roadblocks that they run into and of course staff who buys into that vision.
4.2. Communication and Design Quality
4.2.1. Shape NC
It [our relationship with the technical assistants—interventionists] has been like a glove, we work very closely together. A lot of times they push me, because sometimes I get busy doing other things and [Ms.] R. [the key interventionist] gets me back on track; we should be doing this, change this, etc. She has been very instrumental with that and probably one of the key components to the whole program being successful is the partnership office.
Of course [Ms.] R. [the key interventionist] is phenomenal; she's worth her weight in gold! She has come out and sits down with me for a few minutes and I am thinking, you know I can't go this next step. I just really don't want to go out and beg for more money or more help. She will say, Ms. A., you just have to... By the time she gets through, I'm thinking this is going to be a piece of cake! I go do whatever we need to do and I don't always make the best decisions with the people that we hire, but we look pretty good out there and kids love it. That is name of the game.
Actually really the biggest killers are the teachers. If they say, eww... I'm not going to try that. Then the kids react the same… The little bit of stuff you hear from the kids is the food, but mostly it’s because they heard a teacher say they didn't want to eat something. If you get the teachers on board and get them to introduce it and be excited about it and have taste testing parties.
…in the beginning, we really focused on the working and training and as the hours grew I think we put a little more of a hands off rule specially this last year, because I think they [TAs] feel more confident in their field compared to the previous years and they had a lot more experience behind them.
They [the TAs] have learned to believe in the program so strongly... I've done this training for every employee that I've had.
Everyone is very willing to share resources. If you need something that you don't know, you can just email them and if they don't have it they will find it. So, I think we have a good system for sharing resources and I try to come back and share it with all of the TA girls, so it can spread throughout the county.
4.2.2. HFEH
…they [interventionists] are great at answering as soon we have questions. I think we get an e-mail every week or two with maybe an upcoming webinar or anything that may be of interest to us. So, I’d say maybe once a week, once every two weeks we’re in contact with them… We communicate a little more often around the times that we take the assessments, because we’re gathering information, preparing slides and getting things ready to show that we’ve met certain requirements to earn an A in those areas.
We have the e-mail blasts that go out every week, weekly reminding people that you have the opportunity to earn points, don’t forget to go in and track your exercise, bulletin boards, [and] staff meetings.
When we were first designing the intervention, we’ve always had a very open, qualitative approach, where we read the science, we write it down, but then we spend a lot of time with our stakeholders, saying, really, what do you need? Like what are your stresses, what are your frustrations, what are your pain points? And then put the two together, so that it’s a little bit more user-friendly, and it really meets their interests, instead of just our goals.
I think for our program here, you can either participate here at the gym, or you can do it at home and be part of the wellness program… You don’t have to be linked in here, but that seems like the biggest issue. Concern-wise, I think, the few people that I’ve mentioned, like insurance benefits and stuff like that [incentives for the wellness program]… [but] I think some people feel like it kind of steps into their personal lives too much.
I think the biggest challenge I could see… as far as I enjoy exercising, but the biggest challenge for me, and motivational factor for me is the transition with the weather or the seasons to still keep people motivated... So you just incorporate it into your daily routine, [but] I could see [it] as a really big challenge, because they drew people in at the first part of the year, but then with the warm weather, it’s kind of like, how do you keep them engaged? So I think that’s been one piece that hasn’t quite been figured out yet.
Like the first year, we started something called Walking Wednesdays, which was supposed to be, the idea was, that every Wednesday employees would gather and walk during their break time. Complete flop...! You know, it became too difficult to coordinate that sort of things, so we pretty quickly found out. This is not effective; this is not a good use of time for our staff. Let’s pull back and put in something else that’ll work a little bit better.
I think some of the wellness challenges, as I mentioned, have been a little bit flops. Not a little bit, they’ve been flops! I do think some different incentives will be a big help, even if they’re not directly tied to insurance premiums, if we made the incentives a little more relatable to insurance cost, I think that would be a big step in the right direction as far as incentives go. The incentives we have now just frankly do not motivate everybody. They’ll only be motivators for some people, which I guess is true of any incentive, but I think having some more incentives will just give a broader spectrum of people to incentivize or to motivate.
4.3. Stakeholder Alignment
4.3.1. Shape NC
The owner may say they want it but the director may not be fulfilling the extent of the intentions made. And the owners aren’t in the loop; it is the directors [who] are in charge. The directors are the ones on [the] go but the owners are the ones who can put a brake on the project. The owner may switch the bandwagon—we have seen that a lot.
I think motivation was high but it dipped when it came to how to implement the project, because they weren’t quite sure what was going on and what happened. So, potentially, I think the motivation varied but now everybody seems pretty motivated. They were pretty jazzed and excited and had really good positive stories to share. I think motivation is back up top.
4.3.2. HFEH
4.4. Effects of Costs and Benefits on Motivation
4.4.1. Shape NC
I would like to do what [Ms.] R. [the key interventionist] has suggested. It seems like we'll have a cook for a while and then they are gone, but what I'd really like to do is have a tasting on a Friday afternoon and do some new recipe and let parents have a taste. Have parents come and taste the new recipes and ask them if they think their kid would like it and give them the recipe to make at home… That would be good advertisement.
4.4.2. HFEH
Everybody told me we were going to lose money, that the sales were going to hurt, because people want French fries; I said don’t worry about that. We actually increased revenue. It’s been pretty good…. We looked at it after six months and we were up about 18% on our growth. Overall since we took over [(took out the fryers)] five years ago we’ve been up to around $2,000,000 revenue of the year. And that’s just [for] serving better food, and brought in a whole new customer base. If you looked at the snapshot of the customers who were eating six years ago, it was heavy environmental services maintenance guys who want fried food, fried chicken, that kind of crowd. And when we introduced healthier food, we started seeing more doctors, more nurses, [and] more outside people who were eating, because it was a healthy way to go. So we brought in a new customer-base by adding healthier foods.
We did a whole renovation, and we were going to invest that money to get rid of the fried food, we certainly needed to be able to support that. [When] it comes down to money, you don’t want to do something that will really hurt your business and you’re just left hanging out there if this wasn’t a good idea. And we wanted to make sure that the idea we were doing was a good idea, both financially and nutritionally and all those things.
4.5. Self-Funding
4.5.1. Shape NC
A lot more money should be put into this than what is being put in now. I've always liked to break new ground, which is what I've done. But I've spent way more money than I received, but it has been well worth it to this point… I've put my own personal funds in and move money to this out of the budget. Not everybody can do that. But the more you put into a program the more you get out of it. They also need checks and balances—you need to make sure that the money that you are putting in is really doing what it needs to do. In some instances it is not, and that is a waste… I would say that I have spent probably three times the amount of my own money of the scholarship that we've received.
Ms. A. [the director] went way above and beyond that as far as spending. She built a well just to water the plants—it takes away from her water bill, but by the time you figure out how much she spent on that vs. the cost of the well, it was probably no comparison. But it is out there and it is wonderful. It is great the kids can turn it on and we don't get excited if the water is running a little longer than it should. They've learned to water their plants. So that little bit of a financial thing [initial grant] was like the carrot out there. Just kind of got us started. By no means did it support everything that we did.
4.5.2. HFEH
We really have had no resources to allocate. We don’t have a budget for wellness per se. Now, of course our department has a budget, but there never has been a particular amount set aside for employee wellness specifically. So all of the things that we have tried to do since the beginning have been low to really no cost movements.
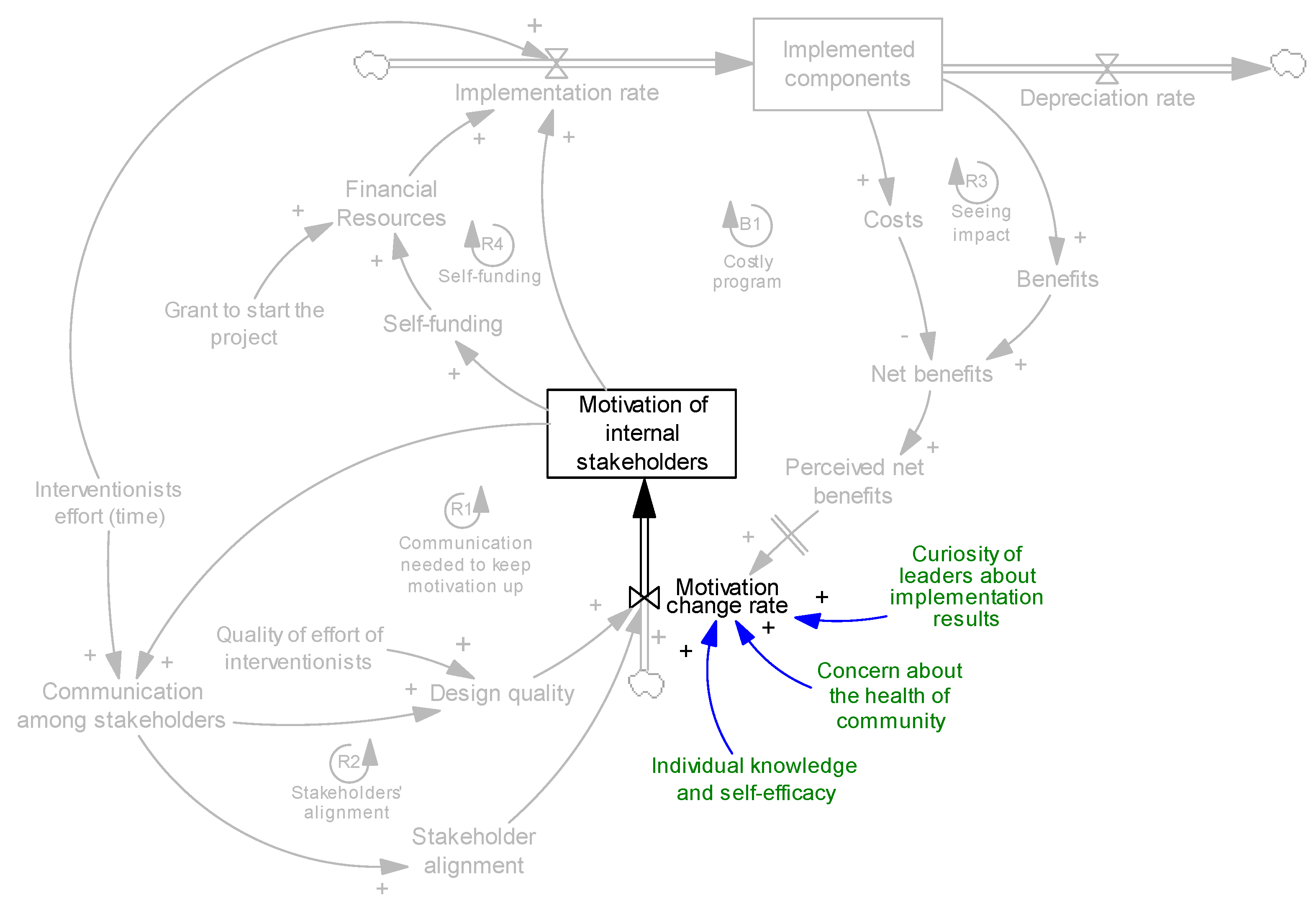
4.6. Non-Dynamic Factors Affecting Motivation
4.7. Depreciation and Maintenance
4.7.1. Shape NC
…the frustration and the motivation at the beginning and the lack of communication just sour it all and it never recovered. And when we select folks, there is this criterion but you have got centers, directors or owners who may not be that good at communicating.
Now with the garden, there's some enthusiasm, there's motivation from the teachers. Whereas some time back, I was not seeing much motivation from the teachers. After the training, now I'm seeing teachers like little bees running around outside with the kids. They are playing soccer and it is kind of weird how it happened. I saw a big shift when they opened up the fencing and allowed more space, more free spaces for kids and teachers to move.
4.7.2. HFEH
We’ve designed the program in order for them to easily maintain things over time, because one of the things that we encourage is that they continue to take the assessments to make sure that they’re maintaining that high level once they’ve achieved it.
[The main challenges to maintain the program is] just to keep people interested and excited. You want to do something that is different enough each year to keep them engaged, but you don’t want to change it so much that they go, ‘Uh, here we go again’, but something new, something completely different. We just learnt this one, now we’re starting something new.
[To be successful] I think you’ve got to have buy-in in that. I think that goes back to the culture, but I think you need to understand why you’re doing this, what’s the benefit of doing it, in that you stick with it, dig your heals in the ground, this is it, this is what we’re doing, this is our program, and then eventually it will become a culture thing.
Not really! Honestly, it’s just continued to grow bigger and bigger and bigger, and haven’t seen it backslide at all.
5. Analysis
5.1. Shape NC
We re-hauled the entire playground, added the trike path, planted fruit trees and other trees, [and] had parent work days. We come out on Saturdays some days. Just want needs to be done, step by step. We've had about four work days where we built things out here without the children... We try to keep the staff motivated, because at first they didn't really get it, but now they are adding it to their lesson plans and thinking about it all the time. They picking books that have fruits and vegetables and fresh foods in them—farm books and things like that, instead of your typical fantasy princess stuff.
…if you have a director X and center Y, and church you probably know this but [the] church based child care doesn’t have high requirements for profit and they give them a pass on certain things. So it’s different to see where the center director gets it and gets on board with it to where you have had a good relationship with the local partnership and they are prompt to do these kinds of things.
5.2. HFEH
Something that we require hospitals to do before they start working with us is to sign a CEO commitment form. That form basically says: ‘Yes, personally I support this but also I am going to put in my strategic plan, we’re going to work on this as an organization, and there are the people that want to work on it from my hospital.’ Having that leadership support is just so important, and as we go out and we visit hospitals and see what they’re doing on the ground, and seeing the CEO support, we definitely see those hospitals as moving forward more quickly than hospitals that have just mediocre or no support for the wellness program.
The wellness program is just a part of our life here. People are used to it, they’re very committed to completing their preventive items, and that is still a part of the wellness program with vitality, there is a prevention component to that.
I think it’s pretty easy to maintain [the program] once you get there. Getting there could be challenging for some people.
I really don’t know! I’ve never been able to find out the actual answer. I think it was just because somebody had brought it up in a meeting, and the CEO at that time was like, ‘Okay!’ and didn’t really know anything about it, because I actually went back to my HR director… maybe two years ago, around the end of the first year of the program, when I had been trying to offer a lot of proposals for things to do, and was not really getting anywhere, and she said, I’m talking about the CEO, said, ‘he doesn’t care. He doesn’t know what’s going on. He doesn’t have any interest in it.’… She was being nice to me, telling me that information. She just said, ‘You know, you do with it what you feel like you need to do.’
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Schiller, J.S.; Martinez, M.; Hao, C.; Barnes, P. Early Release of Selected Estimates Based on Data from the January–September 2004 National Health Interview Survey; National Center for Health Statistics: Atlanta, GA, USA, 2005.
- Ogden, C.L.; Carroll, M.D.; Curtin, L.R.; McDowell, M.A.; Tabak, C.J.; Flegal, K.M. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA-J. Am. Med. Assoc. 2006, 295, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Allender, S.; Millar, L.; Hovmand, P.; Bell, C.; Moodie, M.; Carter, R.; Swinburn, B.; Strugnell, C.; Lowe, J.; de la Haye, K.; et al. Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 1143. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Spadano, J.; Coakley, E.H.; Field, A.E.; Colditz, G.; Dietz, W.H. The disease burden associated with overweight and obesity. JAMA J. Am. Med. Assoc. 1999, 282, 1523–1529. [Google Scholar] [CrossRef]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef] [PubMed]
- World Development Indicators. Health Expenditure, Total (% of GDP); Online Databank; The World Bank: Washington, DC, USA, 2014; Available online: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS (accessed on 1 June 2015).
- Hammond, R.A.; Levine, R. The economic impact of obesity in the United States. Diabetes Metab. Syndr. Obes. Targets Ther. 2010, 3, 285–295. [Google Scholar] [CrossRef]
- Tremmel, M.; Gerdtham, U.G.; Nilsson, P.M.; Saha, S. Economic Burden of Obesity: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2017, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Begun, J.W.; Zimmerman, B.; Dooley, K. Health care organizations as complex adaptive systems. Adv. Health Care Organ. Theory 2003, 253, 288. [Google Scholar]
- Van Koperen, T.M.; de Kruif, A.; van Antwerpen, L.; Hendriks, A.M.; Seidell, J.C.; Schuit, A.J.; Renders, C.M. Barriers to and Facilitators of the Evaluation of Integrated Community-Wide Overweight Intervention Approaches: A Qualitative Case Study in Two Dutch Municipalities. Int. J. Environ. Res. Public Health 2016, 13, 390. [Google Scholar] [CrossRef] [PubMed]
- Plsek, P.E.; Greenhalgh, T. The challenge of complexity in health care. BMJ Clin. Res. Ed. 2001, 323, 625–628. [Google Scholar] [CrossRef]
- Rahmandad, H.; Repenning, N. Capability erosion dynamics. Strateg. Manag. J. 2015, 37, 649–672. [Google Scholar] [CrossRef]
- Stankov, I.; Howard, N.J.; Daniel, M.; Cargo, M. Policy, Research and Residents’ Perspectives on Built Environments Implicated in Heart Disease: A Concept Mapping Approach. Int. J. Environ. Res. Public Health 2017, 14, 17. [Google Scholar] [CrossRef] [PubMed]
- Addy, N.A.; Shaban-Nejad, A.; Buckeridge, D.L.; Dube, L. An Innovative Approach to Addressing Childhood Obesity: A Knowledge-Based Infrastructure for Supporting Multi-Stakeholder Partnership Decision-Making in Quebec, Canada. Int. J. Environ. Res. Public Health 2015, 12, 1314–1333. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, B.E.; Novotny, R.; Gittelsohn, J. Multi-Level, Multi-Component Approaches to Community Based Interventions for Healthy Living-A Three Case Comparison. Int. J. Environ. Res. Public Health 2016, 13, 1023. [Google Scholar] [CrossRef] [PubMed]
- Elias, A.A.; Jackson, L.S.; Cavana, R.Y. Changing positions and interests of stakeholders in environmental conflict: A New Zealand transport infrastructure case. Asia Pac. Viewp. 2004, 45, 87–104. [Google Scholar] [CrossRef]
- Davis, K. Different stakeholder groups and their perceptions of project success. Int. J. Proj. Manag. 2014, 32, 189–201. [Google Scholar] [CrossRef]
- De Schepper, S.; Dooms, M.; Haezendonck, E. Stakeholder dynamics and responsibilities in Public–Private Partnerships: A mixed experience. Int. J. Proj. Manag. 2014, 32, 1210–1222. [Google Scholar] [CrossRef]
- Repenning, N.P. A simulation-based approach to understanding the dynamics of innovation implementation. Organ. Sci. 2002, 13, 109–127. [Google Scholar] [CrossRef]
- Warren, K. Competitive Strategy Dynamics; Wiley: Chichester, UK, 2002; 330p. [Google Scholar]
- Levitt, B.; March, J.G. Organizational Learning. Annu. Rev. Sociol. 1988, 14, 319–340. [Google Scholar] [CrossRef]
- Leonard-Barton, D. Core Capabilities and Core Rigidities—A Paradox in Managing New Product Development. Strateg. Manag. J. 1992, 13, 111–125. [Google Scholar] [CrossRef]
- Rahmandad, H. Effect of delays on complexity of organizational learning. Manag. Sci. 2008, 54, 1297–1312. [Google Scholar] [CrossRef]
- Sterman, J.D. Learning in and about complex systems. Syst. Dyn. Rev. 1994, 10, 91–330. [Google Scholar] [CrossRef]
- Easton, G.S.; Jarrell, S.L. The effects of total quality management on corporate performance: An empirical investigation. J. Bus. 1998, 71, 253. [Google Scholar] [CrossRef]
- Hendricks, K.B.; Singhal, V.R. The Long-Run Stock Price Performance of Firms with Effective TQM Programs. Manag. Sci. 2001, 47, 359–368. [Google Scholar] [CrossRef]
- Repenning, N.P.; Sterman, J.D. Nobody ever gets credit for fixing problems that never happened: Creating and sustaining process improvement. Calif. Manag. Rev. 2001, 43, 64–88. [Google Scholar] [CrossRef]
- Sterman, J.K.; Repenning, N.P.; Kofman, F. Unanticipated side effects of successful quality programs: Exploring a paradox of organizational improvement. Manag. Sci. 1997, 43, 503–521. [Google Scholar] [CrossRef]
- Repenning, N.P. Understanding fire fighting in new product development. J. Prod. Innov. Manag. 2001, 18, 285–300. [Google Scholar] [CrossRef]
- Repenning, N.P.; Sterman, J.D. Capability traps and self-confirming attribution errors in the dynamics of process improvement. Adm. Sci. Q. 2002, 47, 265–295. [Google Scholar] [CrossRef]
- North Carolina Institute of Medicine. Promoting Healthy Weight for Young Children: A Blueprint for Preventing Early Childhood Obesity in North Carolina; North Carolina Institute of Medicine: Morrisville, NC, USA, 2013. [Google Scholar]
- Kolasa, K.M.; Dial, J.; Gaskins, S.; Currie, R. Moving toward healthier-eating environments in hospitals. Nutr. Today 2010, 45, 54–63. [Google Scholar] [CrossRef]
- Lee-Kwan, S.H.; Goedkoop, S.; Yong, R.; Batorsky, B.; Hoffman, V.; Jeffries, J.; Hamouda, M.; Gittelsohn, J. Development and implementation of the Baltimore healthy carry-outs feasibility trial: Process evaluation results. BMC Public Health 2013, 13, 638. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.S.; Rahmandad, H.; Bullock, S.L.; Lee-Kwan, S.H.; Gittelsohn, J.; Ammerman, A. Dynamics of intervention adoption, implementation, and maintenance inside organizations: The case of an obesity prevention initiative. Preprints 2017, 2017080043. [Google Scholar] [CrossRef]
- Jalali, S.M.J. Three Essays on Systems Thinking and Dynamic Modeling in Obesity Prevention Interventions; Virginia Tech.: Falls Church, VA, USA, 2015. [Google Scholar]
- Glaser, B.G.; Strauss, A.L. The Discovery of Grounded Theory: Strategies for Qualitative Research; Aldine Pub. Co.: Chicago, IL, USA, 1967; 271p. [Google Scholar]
- Patton, M.Q.; Patton, M.Q. Qualitative Research and Evaluation Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2002; 65p. [Google Scholar]
- Sterman, J. Business Dynamics: Systems Thinking and Modeling for a Complex World; Irwin/McGraw-Hill: Boston, MA, USA, 2000; 982p. [Google Scholar]
- Abdel-Hamid, T.; Ankel, F.; Battle-Fisher, M.; Gibson, B.; Gonzalez-Parra, G.; Jalali, M.; Kaipainen, K.; Kalupahana, N.; Karanfil, O.; Marathe, A. Public and health-professionals’ misconceptions about the dynamics of body weight gain/loss. Syst. Dyn. Rev. 2014, 30, 58–74. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.; Sharafi-Avarzaman, Z.; Rahmandad, H.; Ammerman, A. Social influence in childhood obesity interventions: A systematic review. Obes.Rev. 2016, 17, 820–832. [Google Scholar] [CrossRef] [PubMed]
- Fallah-Fini, S.; Rahmandad, H.; Huang, T.T.K.; Bures, R.M.; Glass, T.A. Modeling US Adult Obesity Trends: A System Dynamics Model for Estimating Energy Imbalance Gap. Am. J. Public Health 2014, 104, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Rahmandad, H.; Sabounchi, N.S. Modeling and estimating individual and population obesity dynamics. In Social Computing, Behavioral-Cultural Modeling and Prediction; Springer: Berlin/Heiderlberg, Germany, 2012; pp. 306–313. [Google Scholar]
- Struben, J.; Chan, D.; Dube, L. Policy insights from the nutritional food market transformation model: The case of obesity prevention. Ann. N. Y. Acad. Sci. 2014, 1331, 57–75. [Google Scholar] [CrossRef] [PubMed]
- Rahmandad, H. Human Growth and Body Weight Dynamics: An Integrative Systems Model. PLoS ONE 2014, 9, e114609. [Google Scholar] [CrossRef] [PubMed]
- Shoham, D.A.; Hammond, R.; Rahmandad, H.; Wang, Y.; Hovmand, P. Modeling Social Norms and Social Influence in Obesity. Curr. Epidemiol. Rep. 2015, 2, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Milstein, B.; Homer, J.; Hirsch, G. Analyzing national health reform strategies with a dynamic simulation model. Am. J. Public Health 2010, 100, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Ghaffarzadegan, N.; Ebrahimvandi, A.; Jalali, M.S. A Dynamic Model of Post-Traumatic Stress Disorder for Military Personnel and Veterans. PLoS ONE 2016, 11, e0161405. [Google Scholar] [CrossRef] [PubMed]
- Jalali, M.; Rahmandad, H.; Bullock, S.; Ammerman, A. Dynamics of Obesity Interventions inside Organizations. In Proceedings of the 32nd International Conference of the System Dynamics Society, Delf, The Netherlands, 20–24 July 2014; System Dynamics Society: Delf, The Netherlands, 2014; p. 69. [Google Scholar]
- Ghaffarzadegan, N.; Larson, R.C.; Fingerhut, H.; Jalali, M.; Ebrahimvandi, A.; Quaadgras, A.; Kochan, T. Model-Based Policy Analysis to Mitigate Post-Traumatic Stress Disorder. Available online: http://hdl.handle.net/1721.1/102662 (accessed on 1 November 2016).
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Levinthal, D.A. Adaptation on Rugged Landscapes. Manag. Sci. 1997, 43, 934–950. [Google Scholar] [CrossRef]
- Denrell, J.; Fang, C.; Winter, S.G. The economics of strategic opportunity. Strateg. Manag. J. 2003, 24, 977–990. [Google Scholar] [CrossRef]
- Argote, L.; Epple, D. Learning-Curves in Manufacturing. Science 1990, 247, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Arthur, W.B. Competing Technologies, Increasing Returns, and Lock In by Historical Events. Econ. J. 1989, 99, 116–131. [Google Scholar] [CrossRef]


| Organization | Interviewees | Number of Interviews | Interviews Length (min) |
|---|---|---|---|
| Healthy Food Environments in Hospitals (HFEH) | Interventionists and other stakeholders | 5 | 400 |
| Internal stakeholders—Case 1 (N1) * | 3 | 140 | |
| Internal stakeholders—Case 2 (N2) ** | 6 | 170 | |
| Shape North Carolina (Shape NC) | Interventionists and other stakeholders | 11 | 695 |
| Internal stakeholders—Case 1 (S1) * | 8 | 230 | |
| Internal stakeholders—Case 2 (S2) ** | 4 | 190 | |
| Baltimore Healthy Carry-outs (BHC)—presented in [34] | Interventionists and other stakeholders | 5 | 225 |
| Internal stakeholders—Case 1 | 1 | 50 | |
| Internal stakeholders—Case 2 | 1 | 60 | |
| Total | 44 | 2160 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jalali, M.S.; Rahmandad, H.; Bullock, S.L.; Ammerman, A. Dynamics of Implementation and Maintenance of Organizational Health Interventions. Int. J. Environ. Res. Public Health 2017, 14, 917. https://doi.org/10.3390/ijerph14080917
Jalali MS, Rahmandad H, Bullock SL, Ammerman A. Dynamics of Implementation and Maintenance of Organizational Health Interventions. International Journal of Environmental Research and Public Health. 2017; 14(8):917. https://doi.org/10.3390/ijerph14080917
Chicago/Turabian StyleJalali, Mohammad S., Hazhir Rahmandad, Sally Lawrence Bullock, and Alice Ammerman. 2017. "Dynamics of Implementation and Maintenance of Organizational Health Interventions" International Journal of Environmental Research and Public Health 14, no. 8: 917. https://doi.org/10.3390/ijerph14080917
APA StyleJalali, M. S., Rahmandad, H., Bullock, S. L., & Ammerman, A. (2017). Dynamics of Implementation and Maintenance of Organizational Health Interventions. International Journal of Environmental Research and Public Health, 14(8), 917. https://doi.org/10.3390/ijerph14080917






