Socio-Demographic and Lifestyle Factors Predict 5-Year Changes in Adiposity among a Group of Black South African Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.2.1. Questionnaires
2.2.2. Socio-Economic Status Index
2.2.3. Anthropometric Measurements
2.3. Statistical Analysis
3. Results
3.1. Descriptive Baseline Data for the Sample Stratified According to Sex
3.2. Five-Year Dietary and Adiposity Changes of Men and Women Stratified by Residence
3.2.1. Changes in Dietary Intake
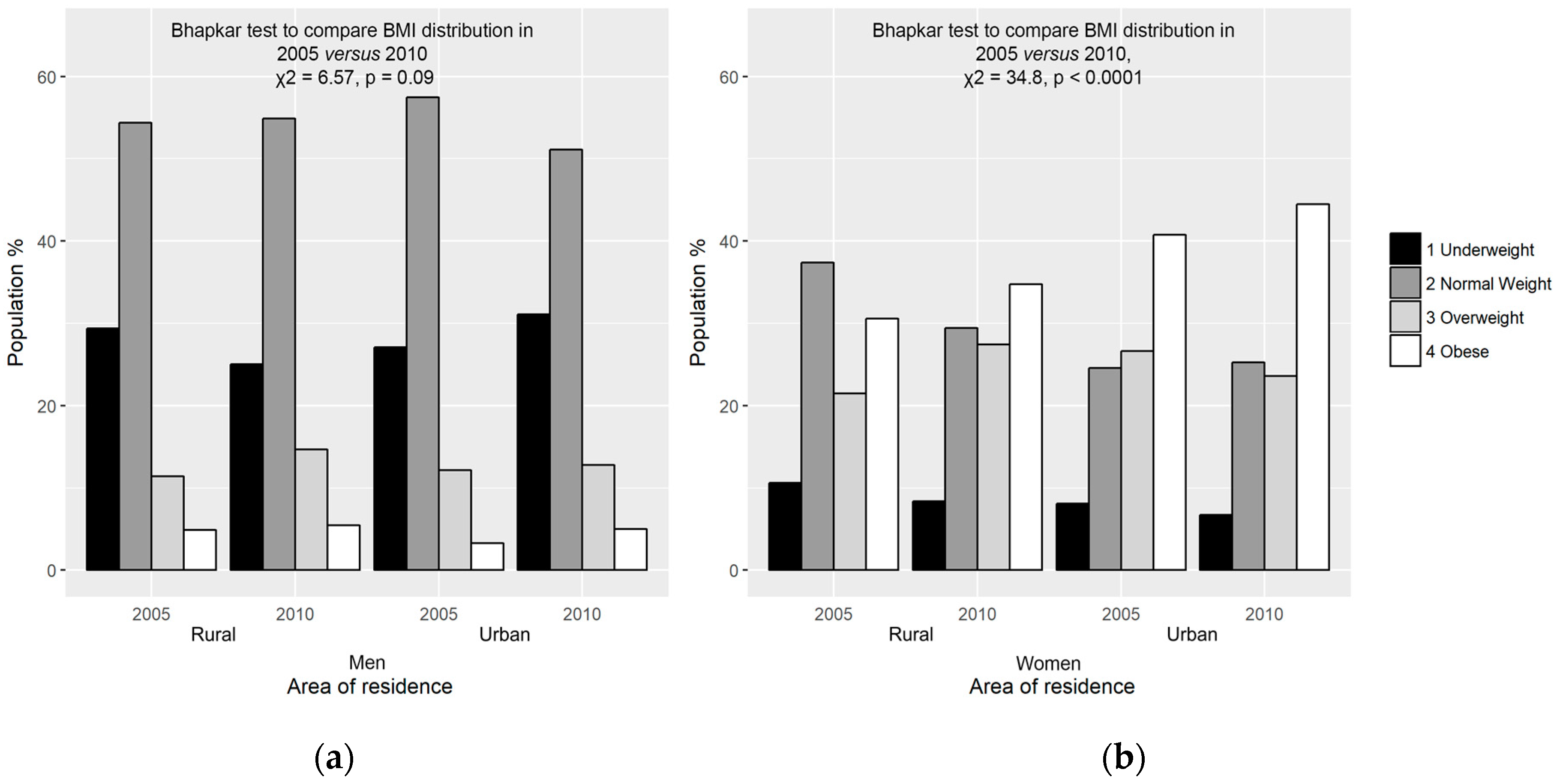
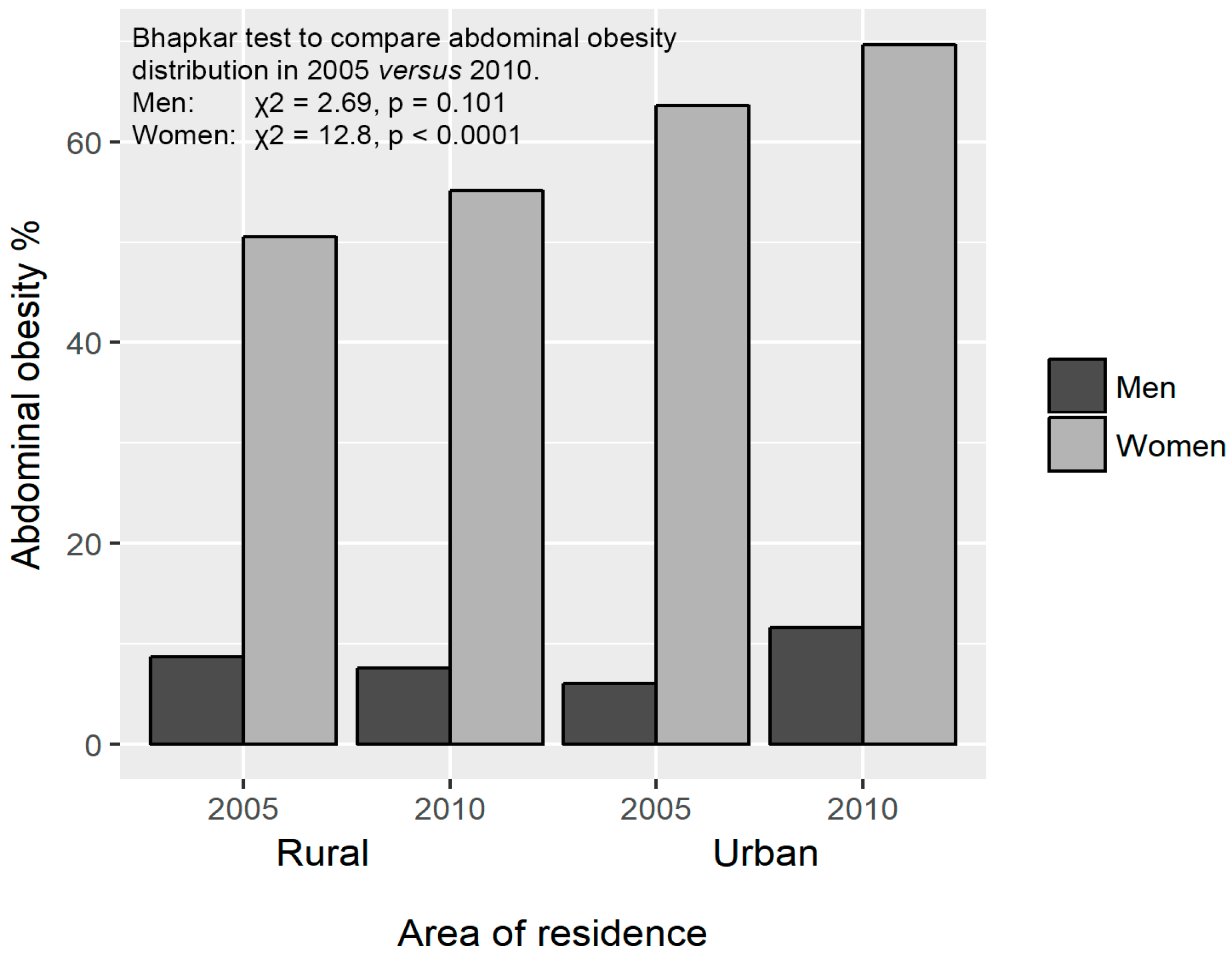
3.2.2. Changes in Adiposity
3.3. Association between Changes in Adiposity with Demographic, Socio-Economic and Lifestyle Variables
3.4. Multivariate Analysis of Changes in Adiposity (Dependent) and Predictor (Baseline Socio-Economic and Lifestyle) Variables
3.5. Marital Transitions and Changes in Adiposity
3.6. Smoking Status Changes and Changes in Adiposity
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 22 June 2017).
- Micklesfield, L.K.; Lambert, E.V.; Hume, D.J.; Chantler, S.; Pienaar, P.R.; Dickie, K.; Goedecke, J.H.; Puoane, T. Socio-cultural, environmental and behavioural determinants of obesity in black South African women: Review articles. Cardiovasc. J. Afr. 2013, 24, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P. The South African National Health and Nutrition Examination Survey, 2012: Sanhanes-1: The Health and Nutritional Status of the Nation; HSRC Press: Cape Town, South Africa, 2014. [Google Scholar]
- Statistics South Africa. South African Demographic and Health Survey Key Indicator Report; Statistics South Africa: Pretoria, South Africa, 2016.
- Alaba, O.; Chola, L. Socioeconomic inequalities in adult obesity prevalence in South Africa: A decomposition analysis. Int. J. Environ. Res. Public Health 2014, 11, 3387–3406. [Google Scholar] [CrossRef] [PubMed]
- Christensen, D.L.; Eis, J.; Hansen, A.W.; Larsson, M.W.; Mwaniki, D.L.; Kilonzo, B.; Tetens, I.; Boit, M.K.; Kaduka, L.; Borch-Johnsen, K. Obesity and regional fat distribution in Kenyan populations: Impact of ethnicity and urbanization. Ann. Hum. Biol. 2008, 35, 232–249. [Google Scholar] [CrossRef] [PubMed]
- Sundquist, J.; Johansson, S.E. The influence of socioeconomic status, ethnicity and lifestyle on body mass index in a longitudinal study. Int. J. Epidemiol. 1998, 27, 57–63. [Google Scholar] [CrossRef] [PubMed]
- McLaren, L. Socioeconomic status and obesity. Epidemiol. Rev. 2007, 29, 29–48. [Google Scholar] [CrossRef] [PubMed]
- Roskam, A.J.; Kunst, A.E.; Van Oyen, H.; Demarest, S.; Klumbiene, J.; Regidor, E.; Helmert, U.; Jusot, F.; Dzurova, D.; Mackenbach, J.P. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int. J. Epidemiol. 2009, 39, 392–404. [Google Scholar] [CrossRef] [PubMed]
- Abrahams, Z.; Mchiza, Z.; Steyn, N.P. Diet and mortality rates in Sub-Saharan Africa: Stages in the nutrition transition. BMC Public Health 2011, 11, 801. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Melanson, E.L.; Wyatt, H.T. Dietary fat intake and regulation of energy balance: Implications for obesity. Nutrition 2000, 130, 284S–288S. [Google Scholar]
- Vorster, H.H.; Kruger, A.; Margetts, B.M. The nutrition transition in Africa: Can it be steered into a more positive direction? Nutrients 2011, 3, 429–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Devanathan, R.; Esterhuizen, T.M.; Govender, R.D. Overweight and obesity amongst Black women in Durban, KwaZulu-Natal: A “disease” of perception in an area of high HIV prevalence. Afr. J. Primary Health Care Fam. Med. 2013, 5, 1–7. [Google Scholar] [CrossRef]
- Irwin, M.L.; Yasui, Y.; Ulrich, C.M.; Bowen, D.; Rudolph, R.E.; Schwartz, R.S.; Yukawa, M.; Aiello, E.; Potter, J.D.; McTiernan, A. Effect of exercise on total and intra-abdominal body fat in postmenopausal women: A randomized controlled trial. JAMA 2003, 289, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Chiolero, A.; Faeh, D.; Paccaud, F.; Cornuz, J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am. J. Clin. Nutr. 2008, 87, 801–809. [Google Scholar] [PubMed]
- Sartorius, B.; Veerman, L.J.; Manyema, M.; Chola, L.; Hofman, K. Determinants of obesity and associated population attributability, South Africa: Empirical evidence from a national panel survey, 2008–2012. PLoS ONE 2015, 10, e130218. [Google Scholar] [CrossRef] [PubMed]
- Cois, A.; Day, C. Obesity trends and risk factors in the South African adult population. BMC Obes. 2015, 2, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abubakari, A.R.; Lauder, W.; Agyemang, C.; Jones, M.; Kirk, A.; Bhopal, R. Prevalence and time trends in obesity among adult West African populations: A meta-analysis. Obes. Rev. 2008, 9, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Cleland, V.; Hume, C.; Crawford, D.; Timperio, A.; Hesketh, K.; Baur, L.; Welch, N.; Salmon, J.; Ball, K. Urban–rural comparison of weight status among women and children living in socioeconomically disadvantaged neighbourhoods. Med. J. Australia 2010, 192, 137–140. [Google Scholar] [PubMed]
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): A prospective cohort study. Lancet 2017. [Google Scholar] [CrossRef]
- Bourne, L.T.; Lambert, E.V.; Steyn, K. Where does the black population of South Africa stand on the nutrition transition? Public Health Nutr. 2002, 5, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Pillay-van Wyk, V.; Msemburi, W.; Laubscher, R.; Dorrington, R.E.; Groenewald, P.; Glass, T.; Nojilana, B.; Joubert, J.D.; Matzopoulos, R.; Prinsloo, M. Mortality trends and differentials in South Africa from 1997 to 2012: Second National Burden of Disease Study. Lancet Global Health 2016, 4, e642–e653. [Google Scholar] [CrossRef]
- Hajian-Tilaki, K.; Heidari, B. Prevalence of obesity, central obesity and the associated factors in urban population aged 20–70 years, in the north of Iran: A population-based study and regression approach. Obes. Rev. 2007, 8, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Sobal, J.; Rauschenbach, B.; Frongillo, E.A. Marital status changes and body weight changes: A U.S. longitudinal analysis. Soc. Sci. Med. 2003, 56, 1543–1555. [Google Scholar] [CrossRef]
- Umberson, D.; Liu, H.; Powers, D. Marital Status, Marital Transitions, and Body Weight. J. Health Soc. Behav. 2009, 50, 327–343. [Google Scholar] [CrossRef] [PubMed]
- Sobal, J.; Rauschenbach, B.S.; Frongillo, E.A. Marital status, fatness and obesity. Soc. Sci. Med. 1992, 35, 915–923. [Google Scholar] [CrossRef]
- Brown, D.E.; Hampson, S.E.; Dubanoski, J.P.; Murai, A.S.; Hillier, T.A. Effects of ethnicity and socioeconomic status on body composition in an admixed, multiethnic population in Hawaii. Am. J. Hum. Biol. 2009, 21, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Segal, K.R.; Dunaif, A.; Gutin, B.; Albu, J.; Nyman, A.; Pi-Sunyer, F.X. Body composition, not body weight, is related to cardiovascular disease risk factors and sex hormone levels in men. Eur. J. Clin. Investig. 1987, 80, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Stensland, S.; Margolis, S. Simplifying the calculation of body mass index for quick reference. J. Am. Diet. Assoc. 1990, 90, 856. [Google Scholar] [PubMed]
- Conway, J.M.; Yanovski, S.Z.; Avila, N.A.; Hubbard, V.S. Visceral adipose tissue differences in black and white women. Am. J. Clin. Nutr. 1995, 61, 765–771. [Google Scholar] [PubMed]
- Lohman, T.G. Skinfolds and body density and their relation to body fatness: A review. Hum. Biol. 1981, 53, 181–225. [Google Scholar] [PubMed]
- Meeuwsen, S.; Horgan, G.; Elia, M. The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin. Nutr. 2010, 29, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Kruger, H.S.; Botha-Ravyse, C.; Havemann-Nel, L.; Doubell, M.; van Rooyen, J.M. Agreement between specific measures of adiposity and associations with high blood pressure in black South African women. Am. J. Hum. Biol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Teo, K.; Chow, C.K.; Vaz, M.; Rangarajan, S.; Yusuf, S. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am. Heart J. 2009, 158, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Vorster, H.H.; Kruger, A.; Wentzel-Viljoen, E.; Kruger, H.S.; Margetts, B.M. Added sugar intake in South Africa: Findings from the Adult Prospective Urban and Rural Epidemiology cohort study. Am. J. Clin. Nutr. 2014, 99, 1479–1486. [Google Scholar] [CrossRef] [PubMed]
- Wentzel-Viljoen, E.; Laubscher, R.; Kruger, A. Using different approaches to assess the reproducibility of a culturally sensitive quantified food frequency questionnaire. S. Afr. J. Clin. Nutr. 2011, 24, 143–148. [Google Scholar] [CrossRef]
- Wolmarans, P.; Danster, N.; Dalton, A.; Rossouw, K.; Schönfeldt, H. Condensed Food Composition Tables for South Africa; Medical Research Council: Cape Town, South Africa, 2010. [Google Scholar]
- Kruger, M.C.; Kruger, I.M.; Wentzel-Viljoen, E.; Kruger, A. Urbanization of black South African women may increase risk of low bone mass due to low vitamin D status, low calcium intake, and high bone turnover. Nutr. Res. 2011, 31, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Kruger, H.S.; Venter, C.S.; Vorster, H.H.; Margetts, B.M. Physical inactivity is the major determinant of obesity in black women in the North West Province, South Africa: The THUSA study. Nutrition 2002, 18, 422–427. [Google Scholar] [CrossRef]
- Filmer, D.; Pritchett, L.H. Estimating wealth effects without expenditure data—Or tears: An application to educational enrollments in states of India. Demography 2001, 38, 115–132. [Google Scholar] [PubMed]
- Alberti, M.; Eckel, R.; Grundy, S.; Zimmet, P.; Cleeman, J.; Donato, K.; Fruchart, J.; Philip, W.; James, T.; Loria, C. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the Association for the Study of Obesity Heart Federation; International Atherosclerosis Society; and International National Heart, Lung, and Blood Institute; American Heart Association; World International Diabetes Federation Task Force on Epidemiology and Prevention. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Sullivan, G.; Feinn, R. Using effect size—Or Why the p value is not enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Amoah, A. Obesity in adult residents of Accra, Ghana. Ethn. Dis. 2003, 13, S97–S101. [Google Scholar] [PubMed]
- Ejike, C.E.; Ijeh, I.I. Obesity in young-adult Nigerians: Variations in prevalence determined by anthropometry and bioelectrical impedance analysis, and the development of % body fat prediction equations. Int. Arch. Med. 2012, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A. Obesity and the built environment: Changes in environmental cues cause energy imbalances. Int. J. Obes. 2008, 32, S137–S142. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, R.W.; French, S.A.; Forster, J.L.; Spry, V.M. Socioeconomic status differences in health behaviors related to obesity: The Healthy Worker Project. Int. J. Obes. 1991, 15, 689–696. [Google Scholar] [PubMed]
- Baxter-Jones, A.D.; Eisenmann, J.C.; Mirwald, R.L.; Faulkner, R.A.; Bailey, D.A. The influence of physical activity on lean mass accrual during adolescence: A longitudinal analysis. J. Appl. Physiol. 2008, 105, 734–741. [Google Scholar] [CrossRef] [PubMed]
- Molarius, A.; Seidell, J.; Sans, S.; Tuomilehto, J.; Kuulasmaa, K. Waist and hip circumferences, and waist-hip ratio in 19 populations of the WHO MONICA Project. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Motala, A.A.; Esterhuizen, T.; Pirie, F.J.; Omar, M.A. The prevalence of metabolic syndrome and determination of the optimal waist circumference cutoff points in a rural South African community. Diabetes Care 2011, 34, 1032–1037. [Google Scholar] [CrossRef] [PubMed]

| Variables | Men (n = 365 *) | Women (n = 693 *) | p a | ||
|---|---|---|---|---|---|
| Age at baseline (year), mean ±SD | 51.9 ± 10.1 | 51.8 ± 10.2 | 0.95 | ||
| Marital status % (n) | Living single | 42.2 (152) | 47.5 (317) | 0.11 | |
| Married/cohabiting | 57.8 (208) | 52.5 (351) | |||
| Socio-economic variables | Stratum of urbanization % (n) | Urban | 49.6 (181) | 42.9 (297) | 0.04 |
| Rural | 50.4 (184) | 57.1 (396) | |||
| Education % (n) | No formal education | 41.5 (149) | 38.4 (257) | 0.59 | |
| Low (1–7 years) | 42.1 (151) | 44.5 (298) | |||
| Intermediate (8–12 years) | 15.3 (55) | 16.6 (111) | |||
| High (>12 years) | 1.1 (4) | 0.6 (4) | |||
| Employed full-time | 59.7 (218) | 57.4 (398) | 0.77 | ||
| Occupation % (n) | Domestic/informal worker | 89.0 (325) | 88.0 (610) | 0.23 | |
| Formally trained/skilled | 4.1 (15) | 2.6 (18) | |||
| Professionals | 0.8 (3) | 0.6 (4) | |||
| No answer | 6.0 (22) | 8.8 (61) | |||
| Type of roofing | Tiles, slates or reinforced concrete | 3.6 (13) | 3.2 (22) | 0.82 | |
| Galvanized iron | 79.7 (291) | 82.0 (568) | |||
| Asbestos | 14.2 (52) | 12.4 (86) | |||
| Scrap material | 2.5 (9) | 2.5 (17) | |||
| Electricity % (n) | 88.5 (323) | 91.3 (633) | 0.23 | ||
| Piped water in house % (n) | 45.5 (166) | 36.4 (252) | 0.004 | ||
| SES index score | 7.83 ± 1.27 | 7.77 ± 1.13 | 0.43 | ||
| Life style | Tobacco use % (n) | 63.2 (230) | 47.2 (325) | <0.001 | |
| Physical activity score, median (interquartile range) | 2.83 (2.52–3.23) | 2.90 (2.57–3.25) | 0.40 | ||
| Energy intake (kg), mean ±SD | 8563 ± 3625 | 7413 ± 3512 | <0.001 | ||
| Fat intake (g), mean ±SD | 50.1 ± 29.5 | 48.0 ± 32.3 | 0.33 | ||
| Adiposity parameters | BMI (kg/m2) | 21.0 ± 4.32 | 27.6 ± 7.41 | <0.001 | |
| Height (cm) | 167 ± 6.75 | 157 ± 6.25 | <0.001 | ||
| Weight (kg) | 58.7 ± 12.7 | 67.9 ± 18.8 | <0.001 | ||
| WC (cm) | 77.1 ± 10.6 | 82.9 ± 13.8 | <0.001 | ||
| Triceps SFT (mm) | 9.32 ± 6.09 | 22.3 ± 9.30 | <0.001 | ||
| Obese: BMI >30 kg/m2, % (n) | 4.1 (15) | 34.9 (242) | <0.001 | ||
| Abdominal obesity ¥, % (n) | 7.4 (27) | 56.1 (389) | <0.001 | ||
| Anthropometric Variables | Residence | Men | Women | ||||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Δ | Baseline | Follow-Up | Δ | ||
| Weight (kg) | Urban | 58.5 ± 12.6 | 58.9 ± 14.1 | 0.46 ± 5.00 | 70.6 ± 19.5 | 71.7 ± 20.6 | 1.09 ± 6.36 |
| Rural | 59.0 ± 13.0 | 60.1 ± 13.3 | 1.04 ± 4.98 | 65.7 ± 18.1 | 68.4 ± 18.5 | 2.52 ± 6.37 | |
| BMI (kg/m2) | Urban | 20.9 ± 4.18 | 21.3 ± 4.90 | 0.34 ± 2.15 | 28.7 ± 7.58 | 29.4 ± 8.06 | 0.62 ± 2.80 |
| Rural | 21.1 ± 4.47 | 21.6 ± 4.67 | 0.50 ± 1.77 | 26.7 ± 7.17 | 27.9 ± 7.34 | 1.11 ± 2.82 | |
| WC (cm) | Urban | 76.6 ± 10.3 | 78.4 ± 11.5 | 1.83 ± 5.95 | 84.7 ± 3.45 | 88.2 ± 1.56 | 3.45 ± 7.65 |
| Rural | 77.5 ± 10.9 | 77.8 ± 10.5 | 0.27 ± 4.13 | 81.4 ± 14.0 | 82.7 ± 13.2 | 1.13 ± 6.18 | |
| Triceps SFT (cm) | Urban | 8.6 ± 5.50 | 9.2 ± 5.87 | −0.6 ± 3.69 | 21.1 ± 8.50 | 23.8 ± 11.4 | 0.81 ± 8.17 |
| Rural | 10.1 ± 6.81 | 9.4 ± 6.41 | 0.7 ± 4.79 | 23.1 ± 9.77 | 24.4 ± 9.98 | −0.37 ± 7.98 | |
| Variable | Men | Women | |||||
|---|---|---|---|---|---|---|---|
| Δ BMI (kg/m2) | Δ WC (cm) | Δ Triceps SFT (mm) | Δ BMI (kg/m2) | Δ WC (cm) | Δ Triceps SFT (mm) | ||
| (n = 364) | (n = 363) | (n = 358) | (n = 691) | (n = 685) | (n = 569) | ||
| Age (year) | 0.04 | 0.07 | 0.002 | −0.16 ** | −0.07 | −0.12 ** | |
| Socio-economic | Education level | −0.02 | 0.03 | 0.01 | 0.0 | 0.11 * | 0.08 |
| Occupation (graded) | 0.04 | 0.04 | −0.02 | 0.03 | 0.03 | −0.03 | |
| SES index | −0.04 | 0.05 | 0.04 | 0.04 | 0.14 ** | 0.07 | |
| Lifestyle | Physical activity score | 0.10 | 0.05 | −0.02 | 0.13 * | −0.02 | 0.08 |
| Energy intake (kJ) | −0.08 | 0.02 | 0.05 | −0.06 | 0.09 * | −0.05 | |
| Fat intake (g) | −0.03 | 0.08 | 0.10 | −0.05 | 0.09 * | 0.02 | |
| Predictor Variables | ∆ BMI | ∆ WC | ∆ Triceps SFT | |||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| Model 1: Full model with all variables | ||||||
| Baseline BMI | −0.07 | −0.08 | N/A | N/A | N/A | N/A |
| Baseline WC | N/A | N/A | −0.28 ** | −0.26 ** | N/A | N/A |
| Baseline triceps SFT | N/A | N/A | N/A | N/A | −0.48 ** | −0.36 ** |
| Baseline age | −0.08 | −0.09 | 0.02 | −0.05 | −0.02 | −0.06 |
| Baseline SES index | 0.003 | 0.05 | 0.13 * | 0.09 * | 0.10 | 0.10 * |
| Baseline physical activity score | 0.11 | 0.05 | 0.02 | 0.02 | −0.04 | 0.05 |
| Baseline fat intake (g) | 0.09 | −0.01 | −0.005 | −0.04 | 0.06 | 0.06 |
| Baseline tobacco use 0 = never used, 1 = ever used | −0.07 | −0.02 | −0.09 | 0.01 | −0.10 | −0.10 * |
| Baseline marital status 0 = single, 1 = married/cohabiting | 0.22 ** | 0.03 | 0.27 ** | 0.07 | 0.14 * | −0.06 |
| Stratum of urbanization 0 = rural, 1 = urban | −0.07 | 0.00 | 0.15 * | 0.23 ** | 0.09 | 0.02 |
| Baseline menopausal status 0 = premenopausal, 1 = postmenopausal | N/A | −0.09 | N/A | −0.03 | N/A | −0.10 * |
| Adjusted R2 | 0.054 | 0.024 | 0.131 | 0.100 | 0.228 | 0.129 |
| Model 2: Model with best fit | ||||||
| Baseline BMI | -- | −0.08 | N/A | N/A | N/A | N/A |
| Baseline WC | N/A | N/A | −0.28 ** | −0.26 ** | N/A | N/A |
| Baseline triceps SFT | N/A | N/A | N/A | N/A | −0.48 ** | −0.36 ** |
| Baseline age | −0.09 | −0.09 | -- | −0.07 | -- | −0.06 |
| Baseline SES index | -- | 0.05 | 0.12 * | 0.09 * | 0.12 * | 0.09 * |
| Baseline marital status 0 = single, 1 = married/cohabiting | 0.22 ** | -- | 0.27 ** | -- | 0.13 * | -- |
| Stratum of urbanization 0 = rural, 1 = urban | -- | -- | 0.15 * | 0.22 ** | 0.12 * | |
| Baseline physical activity score | 0.12 * | 0.05 | -- | -- | -- | -- |
| Baseline menopausal status 0 = premenopausal, 1 = postmenopausal | N/A | −0.08 | N/A | -- | N/A | −0.11 * |
| Baseline tobacco use 0 = never used, 1 = ever used | -- | -- | −0.09 | -- | -- | −0.10 * |
| Adjusted R2 | 0.057 | 0.030 | 0.138 | 0.107 | 0.231 | 0.132 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nienaber-Rousseau, C.; Sotunde, O.F.; Ukegbu, P.O.; Myburgh, P.H.; Wright, H.H.; Havemann-Nel, L.; Moss, S.J.; Kruger, I.M.; Kruger, H.S. Socio-Demographic and Lifestyle Factors Predict 5-Year Changes in Adiposity among a Group of Black South African Adults. Int. J. Environ. Res. Public Health 2017, 14, 1089. https://doi.org/10.3390/ijerph14091089
Nienaber-Rousseau C, Sotunde OF, Ukegbu PO, Myburgh PH, Wright HH, Havemann-Nel L, Moss SJ, Kruger IM, Kruger HS. Socio-Demographic and Lifestyle Factors Predict 5-Year Changes in Adiposity among a Group of Black South African Adults. International Journal of Environmental Research and Public Health. 2017; 14(9):1089. https://doi.org/10.3390/ijerph14091089
Chicago/Turabian StyleNienaber-Rousseau, Cornelie, Olusola F. Sotunde, Patricia O. Ukegbu, P. Hermanus Myburgh, Hattie H. Wright, Lize Havemann-Nel, Sarah J. Moss, Iolanthé M. Kruger, and H. Salomé Kruger. 2017. "Socio-Demographic and Lifestyle Factors Predict 5-Year Changes in Adiposity among a Group of Black South African Adults" International Journal of Environmental Research and Public Health 14, no. 9: 1089. https://doi.org/10.3390/ijerph14091089








