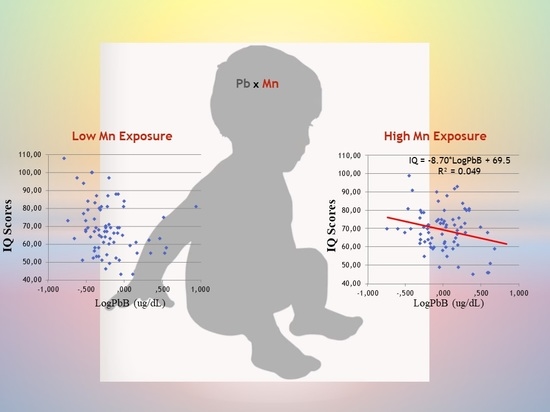
Environmental Co-Exposure to Lead and Manganese and Intellectual Deficit in School-Aged Children
Abstract
:1. Introduction
2. Materials and Methods
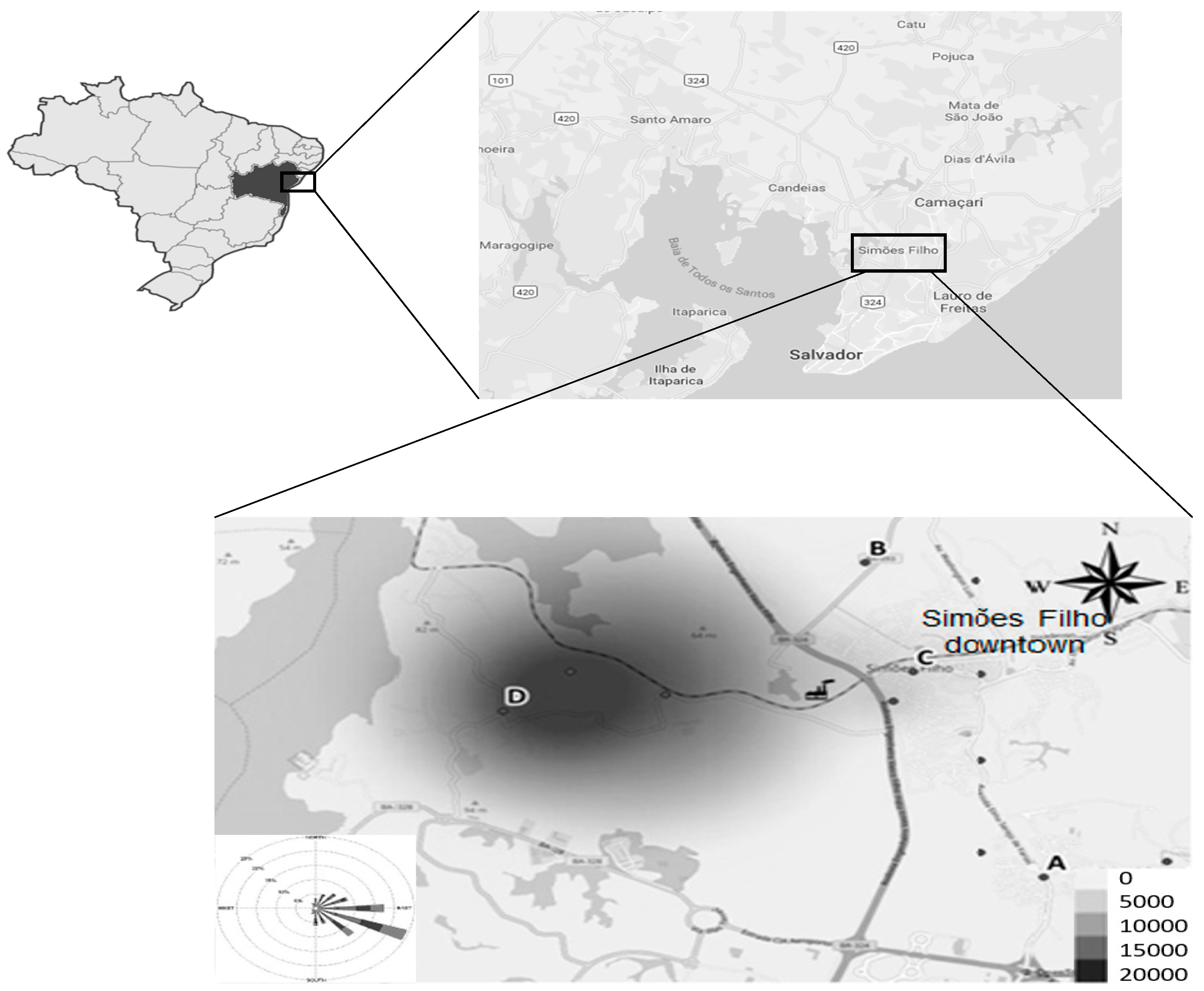
2.1. Study Design and Population
2.2. Questionnaires and Anthropometric Measurements
2.3. Exposure Biomarkers
2.4. Neuropsychological Assessment
2.5. Statistical Analysis
3. Results
3.1. Population Characteristics
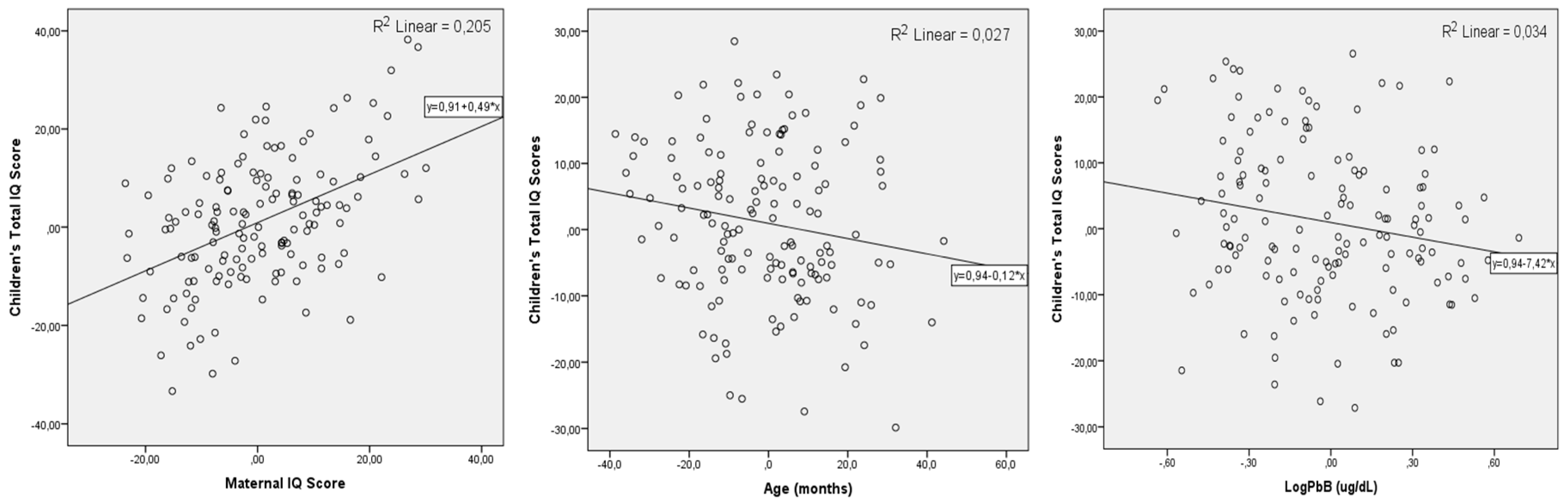
3.2. Biomarkers of Exposure and Bivariate Analysis
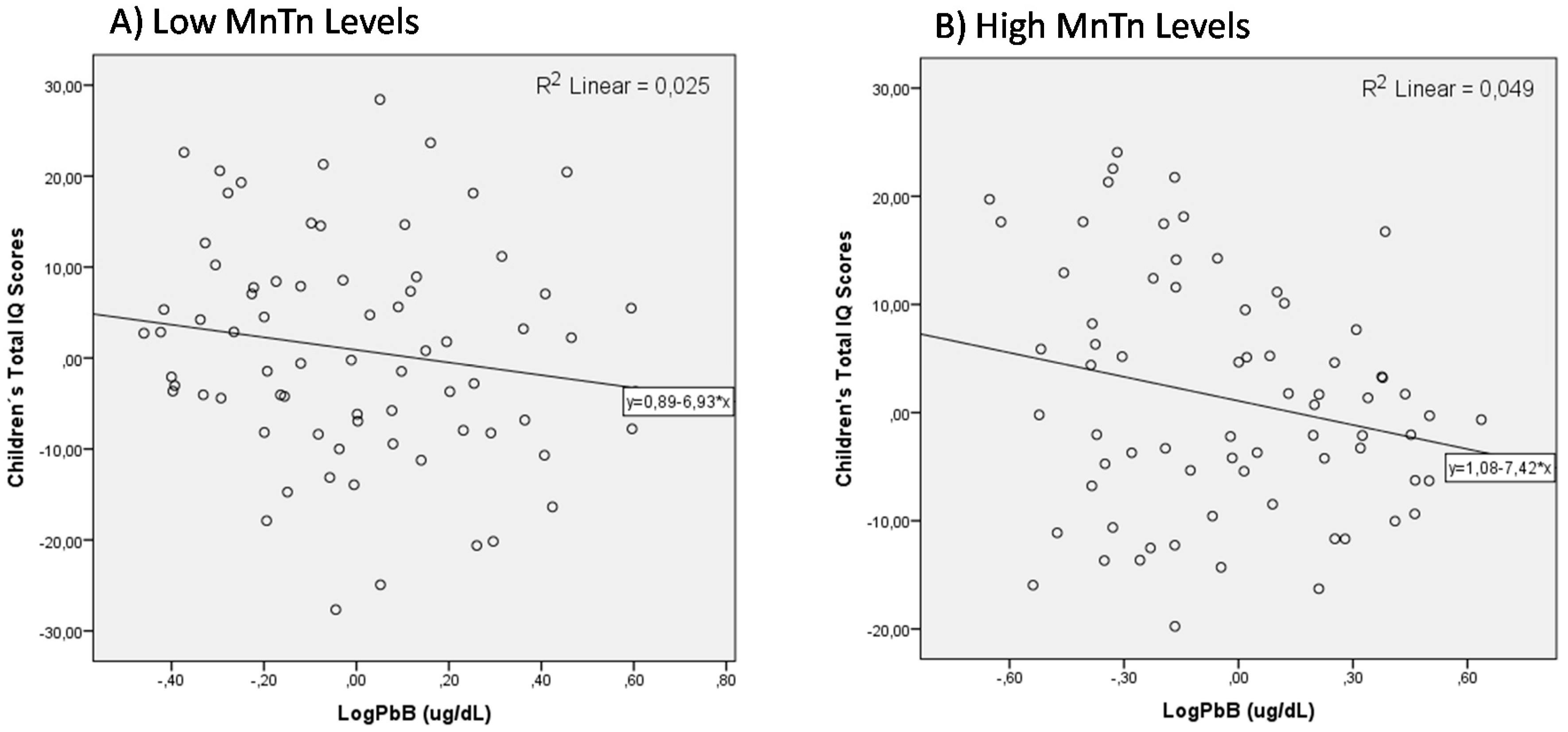
3.3. MLR Models for Children’s Total IQ Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- UNEP (United Nations Environment Program). 2012 Partnership for Clean Fuels and Vehicles. Available online: http://staging.unep.org/transport/pcfv/PDF/Brochurelead.pdf (accessed on 29 August 2018).
- Trasande, L.; Liu, Y. Reducing the staggering costs of environmental disease in children, estimated at $76.6 billion in 2008. Health Aff. 2011, 30, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Gould, E. Childhood lead poisoning: Conservative estimates of the social and economic benefits of lead hazard control. Environ. Health Perspect. 2009, 117, 1162–1167. [Google Scholar] [CrossRef] [PubMed]
- CDC (Centers for Disease Control and Prevention). Interpreting and Managing Blood Lead Levels <10 ug/dl in Children and Reducing Childhood Exposures to Lead: Recommendations of CDC’s Advisory Committee on Childhood Lead Poisoning Prevention. Available online: http://www.cdc.gov/mmwr/PDF/rr/rr5608.pdf (accessed on 21 April 2018).
- Obeng-Gyasi, E. Lead Exposure and Oxidative Stress—A Life Course Approach in US Adults. Toxics 2018, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Ide, L.S.; Parker, D.L. Hazardous Child Labor: Lead and Neurocognitive Development. Public Health Rep. 2005, 120, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Lo, Y.C.; Dooyema, C.A.; Neri, A.; Durant, J.; Jefferies, T.; Medina-Marino, A.; de Ravello, L.; Thoroughman, D.; Davis, L.; Dankoli, R.S.; et al. Childhood lead poisoning associated with goldore processing: A village-level investigation-Zamfara State, Nigeria. Environ Health Perspect. 2012, 120, 1450–1455. [Google Scholar] [CrossRef] [PubMed]
- ATSDR—Agency for Toxic Substances and Disease Registry. Toxicological Profile for Lead; Department of Health and Human Services: Atlanta, GA, USA, 2010. Available online: https://www.atsdr.cdc.gov/ToxProfiles/tp.asp?id = 96&tid = 22 (accessed on 12 September 2018).
- World Health Organization (WHO). Summary of Principles for Evaluating Health Risks in Children Associated with Exposure to Chemicals; World Health Organization: Geneva, Switzerland, 2011; Available online: www.who.int/ceh/health_risk_children.pdf (accessed on 6 September 2018).
- Lidsky, T.I.; Schneider, J.S. Lead neurotoxicity in children: Basic mechanisms and clinical correlates. Brain 2003, 126, 5–19. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Childhood Lead Poisoning. Available online: http://www.who.int/ceh/publications/leadguidance.pdf (accessed on 31 August 2018).
- AAP Council on Environmental Health. Prevention of Childhood Lead Toxicity. Pediatrics 2016, 138, e20161493. [Google Scholar] [CrossRef] [PubMed]
- Menezes-Filho, J.A.; Viana, G.F.S.; Paes, C.R. Determinants of lead exposure in children on the outskirts of Salvador, Brazil. Environ. Monit. Assess. 2012, 184, 2593–2603. [Google Scholar] [CrossRef] [PubMed]
- Needleman, H.L.; Riess, J.A.; Tobin, M.J.; Biesecker, G.E.; Greenhouse, J.B. Bone lead levels and delinquent behavior. JAMA 1996, 275, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Nigg, J.T.; Knottnerus, G.M.; Martel, M.M.; Nikolas, M.; Cavanagh, K.; Karmaus, W.; Rappley, M.D. Low blood lead levels associated with clinically diagnosed attention deficit/hyperactivity disorder and mediated by weak cognitive control. Biol. Psychiatry 2008, 63, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Lanphear, B.P.; Hornung, R.; Khoury, J.; Yolton, K.; Baghurst, P.; Bellinger, D.C.; Canfield, R.L.; Dietrich, K.N.; Bornschein, R.; Greene, T. Low-level environmental lead exposure and children’s intellectual function: An international pooled analysis. Environ. Health Perspect. 2005, 113, 894–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Froehlich, T.E.; Lanphear, B.P.; Auinger, P.; Hornung, R.; Epstein, J.N.; Braun, J.; Kahn, R.S. The association of tobacco and lead exposure with attention-deficit/hyperactivity disorder. Pediatrics 2009, 124, e1054. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.H. Development of human brain functions. Biol. Psychiatry 2003, 15, 1312–1316. [Google Scholar] [CrossRef]
- Casey, B.J.; Tottenham, N.; Liston, C.; Durston, S. Imaging the developing brain: What have we learned about cognitive development? Trends Cogn. Sci. 2005, 9, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Suszkiw, J.B. Presynaptic Disruption of Transmitter Release by Lead. Neurotoxicology 2004, 25, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Karri, V.; Schuhmacher, M.; Kumar, V. Heavy metals (Pb, Cd, As and MeHg) as risk factors for cognitive dysfunction: A general review of metal mixture mechanism in brain. Environ. Toxicol. Pharmacol. 2016, 48, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Guilarte, T.R.; McGlothan, J.L.; Degaonkar, M.; Chen, M.K.; Barker, P.B.; Syversen, T.; Schneider, J.S. Evidence for cortical dysfunction and widespread manganese accumulation in the nonhuman primate brain following chronic manganese exposure: A 1HMRS and MRI study. Toxicol. Sci. 2006, 94, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Aschner, M.; Guilarte, T.R.; Zheng, W. Manganese: Recent advances in understanding its transport and neurotoxicity. Toxicol. Appl. Pharmacol. 2007, 221, 131–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guilarte, T.R. A decade of studies on manganese neurotoxicity in non-human primates: Novel findings and future directions. In Manganese in Health and Disease; Costa, L.G., Aschner, M., Eds.; The Royal Society of Chemistry: London, UK, 2015; pp. 459–476. [Google Scholar]
- Chen, P.; Chakraborty, S.; Mukhopadhyay, S.; Lee, E.; Paoliello, M.M.; Bowman, A.B.; Aschner, M. Manganese homeostasis in the nervous system. J. Neurochem. 2015, 134, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Bouabid, S.; Tinakoua, A.; Lakhdar’Ghazal, N.; Benazzouz, A. Manganese neurotoxicity: Behavioral disorders associated with dysfunctions in the basal ganglia and neurochemical transmission. J. Neurochem. 2016, 136, 677–691. [Google Scholar] [CrossRef] [PubMed]
- Guilarte, T.R. Manganese neurotoxicity: New perspectives from behavioral, neuroimaging, and neuropathological studies in humans and non-human primates. Front. Aging Neurosci. 2013, 5, 23. [Google Scholar] [CrossRef] [PubMed]
- Lucchini, R.G.; Zoni, S.; Guazzetti, S.; Bontempi, E.; Micheletti, S.; Broberg, K.; Parrinello, G.; Smith, D.R. Inverse association of intellectual function with very low blood lead but not with manganese exposure in Italian adolescents. Environ. Res. 2012, 118, 65–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Claus Henn, B.; Schnaas, L.; Ettinger, A.S.; Schwartz, J.; Lamadrid-Figueroa, H.; Hernandez-Avila, M.; Amarasiriwardena, C.; Hu, H.; Bellinger, D.C.; Wright, R.O.; et al. Associations of early childhood manganese and lead coexposure with neurodevelopment. Environ. Health Perspect. 2012, 120, 126–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodrigues, E.G.; Bellinger, D.C.; Valeri, L.; Hasan, M.O.S.I.; Quamruzzaman, Q.; Golam, M.; Kile, M.K.; Christiani, D.C.; Wright, R.O.; Mazumdar, M. Neurodevelopmental outcomes among 2- to 3-year-old children in Bangladesh with elevated blood lead and exposure to arsenic and manganese in drinking water. Environ. Health 2016, 15, 44. [Google Scholar] [PubMed]
- Valeri, L.; Mazumdar, M.M.; Bobb, J.F.; Claus Henn, B.; Rodrigues, E.; Sharif, O.I.A.; Kile, M.L.; Quamruzzaman, Q.; Afroz, S.; Golam, M.; et al. The Joint Effect of Prenatal Exposure to Metal Mixtures on Neurodevelopmental Outcomes at 20–40 Months of Age: Evidence from Rural Bangladesh. Environ. Health Perspect. 2017, 26, 067015. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Chen, Y.C.; Su, F.C.; Lin, C.M.; Liao, H.F.; Hwang, Y.H.; Hsieh, W.S.; Jeng, S.F.; Su, Y.N.; Chen, P.C. In utero exposure to environmental lead and manganese and neurodevelopment at 2 years of age. Environ. Res. 2013, 123, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.L.G.; Bandeira, M.J.; Araújo, C.F.S.; Santos, N.R.; Anjos, A.L.S.; Koin, N.L.; Pereira, L.C.; Oliveira, S.S.P.; Mergler, D.; Menezes-Filho, J.A. Manganese and lead levels in settled dust in elementary schools are correlated with biomarkers of exposure in school-aged children. Environ. Pollut. 2017, 238, 1004–1013. [Google Scholar] [CrossRef] [PubMed]
- Menezes-Filho, J.A.; de Souza, K.O.F.; Rodrigues, J.L.G.; dos Santos, N.R.; de Jesus Bandeira, M.; Koin, N.G.; Mergler, D. Manganese and lead in dust fall accumulation in elementary schools near a ferromanganese alloy plant. Environ. Res. 2016, 148, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Associação Brasileira de Empresas de Pesquisa—ABEP. Critério de Classificação Econômica Brasil. 2011. Available online: http://www.tendencia.inf.br/cceb.pdf (accessed on 25 August 2018).
- World Health Origination WHO. AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Wechsler, D. Escala de Inteligência Wechsler para Crianças, (WISC-III): Manual; Adaptação e Padronização de uma Amostra Brasileira; Casa do Psicólogo: São Paulo, Brasil, 2002. [Google Scholar]
- CDC (Centers for Disease Control and Prevention). Blood Lead Levels in Children. Available online: http://www.cdc.gov/nceh/lead/ACCLPP/Lead_Levels_in_Children_Fact_Sheet.pdf (accessed on 29 August 2018).
- Olivero-Verbel, J.; Duarte, D.; Echenique, M.; Guette, J.; Johnson-Restrepo, B.; Parsons, P.J. Blood lead levels in children aged 5–9 years living in Cartagena, Colombia. Sci. Total Environ. 2017, 372, 707–716. [Google Scholar] [CrossRef] [PubMed]
- Zaida, F.; Chadrame, S.; Sedki, A.; Lekouch, N.; Bureau, F.; Arhan, P.; Bougle, D. Lead and aluminium levels in infants’ hair, diet, and the local environment in the Moroccan city of Marrakech. Sci. Total Environ. 2007, 377, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Ji, J.S.; Schwartz, J.S.; Sparrow, D.; Hu, H.; Weisskopf, M.G. Occupational Determinants of Cumulative Lead Exposure: Analysis of Bone Lead among Men in the VA Normative Aging Study. J. Occup. Environ. Med. 2014, 56, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Menezes-Filho, J.A.; Novaes, C.O.; Moreira, J.C.; Sarcinelli, P.N.; Mergler, D. Elevated manganese and cognitive performance in school-aged children and their mothers. Environ. Res. 2011, 111, 156–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucas, E.L.; Bertrand, P.; Guazzetti, S.; Donna, F.; Peli, M.; Jursa, T.P.; Lucchini, R.; Smith, D.R. Impact of ferromanganese alloy plants on household dust manganese levels: Implications for childhood exposure. Environ. Res. 2015, 138, 279–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haynes, E.N.; Sucharew, H.; Hilbert, T.J.; Kuhnell, P.; Spencer, A.; Newman, N.C.; Burns, R.; Wright, R.; Parsons, P.J.; Dietrich, K.N. Impact of air manganese on child neurodevelopment in East Liverpool, Ohio. Neurotoxicology 2018, 64, 94–102. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n | %/Mean (Min-Max) |
|---|---|---|
| Gender | ||
| Boys | 111 | 49.1% |
| Girls | 115 | 50.9% |
| Age (months) | 224 | 116.8 (84.0–156.9) |
| BMI (kg/m2) | 211 | 17.62 (12.70–44.75) |
| H/A z-score | 212 | 0.065 (−3.03–3.93) |
| Anemia | 186 | 10 (5.5%) |
| Main caregiver | ||
| Mother | 148 | 83.6% |
| Father | 11 | 6.2% |
| Other | 18 | 10.2% |
| Gestational period in the region | 216 | 170 (75.2%) |
| Smoker at home | 215 | 39 (18.1%) |
| Maternal schooling | ||
| Completed high school | 215 | 50 (24.0%) |
| Less than high school | 208 | 158 (76.0%) |
| Brazilian socioeconomic classification | ||
| B | 5 | 2.4% |
| C | 93 | 41.2% |
| D/E | 155 | 52.8% |
| Children’s IQ | 217 | 75.5 (42–116) |
| Maternal IQ | 174 | 68.9 (43–108) |
| Biomarker | n | Median | Min.–Max. | Mean | SD | P25–P75 |
|---|---|---|---|---|---|---|
| PbB (µg/dL) | 219 | 1.15 | 0.2–15.6 | 1.64 | 1.56 | 0.6–2.1 |
| MnH (µg/g) | 208 | 0.74 | 0.16–8.79 | 1.14 | 1.19 | 0.50–1.32 |
| MnTn (µg/g) | 198 | 0.84 | 0.15–13.30 | 1.43 | 1.75 | 0.51–1.77 |
| Children’s IQ | Maternal IQ | Sex | Age (months) | H/A z-Score | PbB (µg/dL) | MnH (µg/g) | MnTn (µg/g) | Hb (g/dL) | |
|---|---|---|---|---|---|---|---|---|---|
| Children’s IQ | 1.000 | 0.413 ** | 0.008 | −0.287 ** | 0.038 | −0.264 ** | −0.169 * | −0.018 | 0.110 |
| 0.000 | 0.906 | 0.000 | 0.591 | 0.000 | 0.017 | 0.807 | 0.111 | ||
| Maternal IQ | 1.000 | 0.098 | −0.117 | 0.044 | −0.070 | −0.216 ** | 0.016 | 0.126 | |
| 0.198 | 0.128 | 0.567 | 0.367 | 0.006 | 0.846 | 0.102 | |||
| Sex | 1.000 | 0.007 | −0.021 | 0.088 | 0.099 | 0.122 | 0.020 | ||
| 0.917 | 0.760 | 0.193 | 0.153 | 0.087 | 0.766 | ||||
| Age (months) | 1.000 | −0.099 | 0.229 ** | 0.005 | 0.133 | −0.013 | |||
| 0.150 | 0.001 | 0.946 | 0.063 | 0.851 | |||||
| H/A z-score | 1.000 | −0.164 * | −0.050 | 0.115 | −0.029 | ||||
| 0.019 | 0.490 | 0.117 | 0.677 | ||||||
| PbB | 1.000 | 0.185 ** | 0.244 ** | −0.178 ** | |||||
| 0.008 | 0.001 | 0.008 | |||||||
| MnH | 1.000 | 0.394 ** | −0.133 | ||||||
| 0.000 | 0.058 | ||||||||
| MnTn | 1.000 | −0.164 * | |||||||
| 0.022 | |||||||||
| Hb (g/dL) | 1.000 |
| Model A: Unadjusted for Parent. IQ | Beta | Std. Error | T-Stat | p-value |
| Constant | 98.118 | 6.334 | 15.492 | <0.001 |
| Age (months) | −0.195 | 0.053 | −3.659 | <0.001 |
| Sex | 0.958 | 1.910 | 0.501 | 0.617 |
| H/A z-score | −0.662 | 0.901 | −0.735 | 0.464 |
| LogPbB | −9.915 | 3.041 | −3.261 | 0.001 |
| LogMnH | −8.093 | 3.041 | −2.576 | 0.011 |
| LogMnTn | 6.961 | 2.935 | 2.372 | 0.019 |
| Models’ statistics: n = 186, r2 = 0.167, F = 6.00, p < 0.001 | ||||
| Model B: Adjusted for Maternal IQ | Beta | Std. Error | T-Stat | p-value |
| Constant | 61.404 | 8.834 | 6.951 | <0.001 |
| Age (months) | −0.140 | 0.053 | −2.631 | 0.009 |
| LogPbB | −8.609 | 2.965 | −2.904 | 0.004 |
| LogMnH | −2.589 | 3.234 | −0.801 | 0.425 |
| LogMnTn | 4.372 | 2.854 | 1.523 | 0.128 |
| ParentMaternal IQ | 0.452 | 0.078 | 5.799 | <0.001 |
| Models’ statistics: n = 155, r2 = 0.316, F = 13.88, p < 0.001 | ||||
| Model C: Interactions | Beta | Std. Error | T-Stat | p-value |
| Constant | 59.016 | 8.899 | 6.632 | <0.001 |
| Age (months) | −0.131 | 0.054 | −2.420 | 0.017 |
| LogPbB | −9.008 | 3.121 | −2.288 | 0.005 |
| LogMnH | −0.279 | 3.121 | −0.089 | 0.929 |
| Maternal IQ | 0.473 | 0.079 | 5.961 | <0.001 |
| LogPbB*LogMnH | −14.317 | 10.868 | −1.317 | 0.190 |
| LogPbB*LogMnTn | 6.412 | 8.657 | 0.741 | 0.460 |
| Models’ statistics: n = 149, r2 = 0.286, F = 10.93, p < 0.001 | ||||
| Model D: Effect modif. Low MnTn | Beta | Std. Error | T-Stat | p-value |
| Constant | 54.282 | 12.450 | 4.360 | <0.001 |
| Age (months) | −0.050 | 0.083 | −0.610 | 0.544 |
| LogPbB | −6.801 | 4.927 | −1.380 | 0.172 |
| LogMnH | −5.329 | 4.675 | −1.140 | 0.258 |
| Maternal IQ | 0.383 | 0.106 | 3.632 | 0.001 |
| Models’ statistics: n = 73, r2 = 0.256, F = 5.90, p < 0.001 | ||||
| Model E: Effect modif. High MnTn | Beta | Std. Error | T-Stat | p-value |
| Constant | 55.445 | 13.843 | 4.005 | <0.001 |
| Age (months) | −0.170 | 0.073 | −2.336 | 0.022 |
| LogPbB | −8.699 | 4.064 | −2.140 | 0.036 |
| LogMnH | 3.078 | 4.277 | 0.720 | 0.4474 |
| Maternal IQ | 0.598 | 0.124 | 4.812 | <0.001 |
| Models’ statistics: n = 74, r2 = 0.381, F = 12.38, p < 0.001. | ||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menezes-Filho, J.A.; Carvalho, C.F.; Rodrigues, J.L.G.; Araújo, C.F.S.; Dos Santos, N.R.; Lima, C.S.; Bandeira, M.J.; Marques, B.L.d.S.; Anjos, A.L.S.; Bah, H.A.F.; et al. Environmental Co-Exposure to Lead and Manganese and Intellectual Deficit in School-Aged Children. Int. J. Environ. Res. Public Health 2018, 15, 2418. https://doi.org/10.3390/ijerph15112418
Menezes-Filho JA, Carvalho CF, Rodrigues JLG, Araújo CFS, Dos Santos NR, Lima CS, Bandeira MJ, Marques BLdS, Anjos ALS, Bah HAF, et al. Environmental Co-Exposure to Lead and Manganese and Intellectual Deficit in School-Aged Children. International Journal of Environmental Research and Public Health. 2018; 15(11):2418. https://doi.org/10.3390/ijerph15112418
Chicago/Turabian StyleMenezes-Filho, José A., Chrissie F. Carvalho, Juliana L. G. Rodrigues, Cecília F. S. Araújo, Nathália R. Dos Santos, Cássio S. Lima, Matheus J. Bandeira, Breno L. de S. Marques, Ana Laura S. Anjos, Homegnon A. F. Bah, and et al. 2018. "Environmental Co-Exposure to Lead and Manganese and Intellectual Deficit in School-Aged Children" International Journal of Environmental Research and Public Health 15, no. 11: 2418. https://doi.org/10.3390/ijerph15112418