Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up
Abstract
:1. Introduction
2. Methods
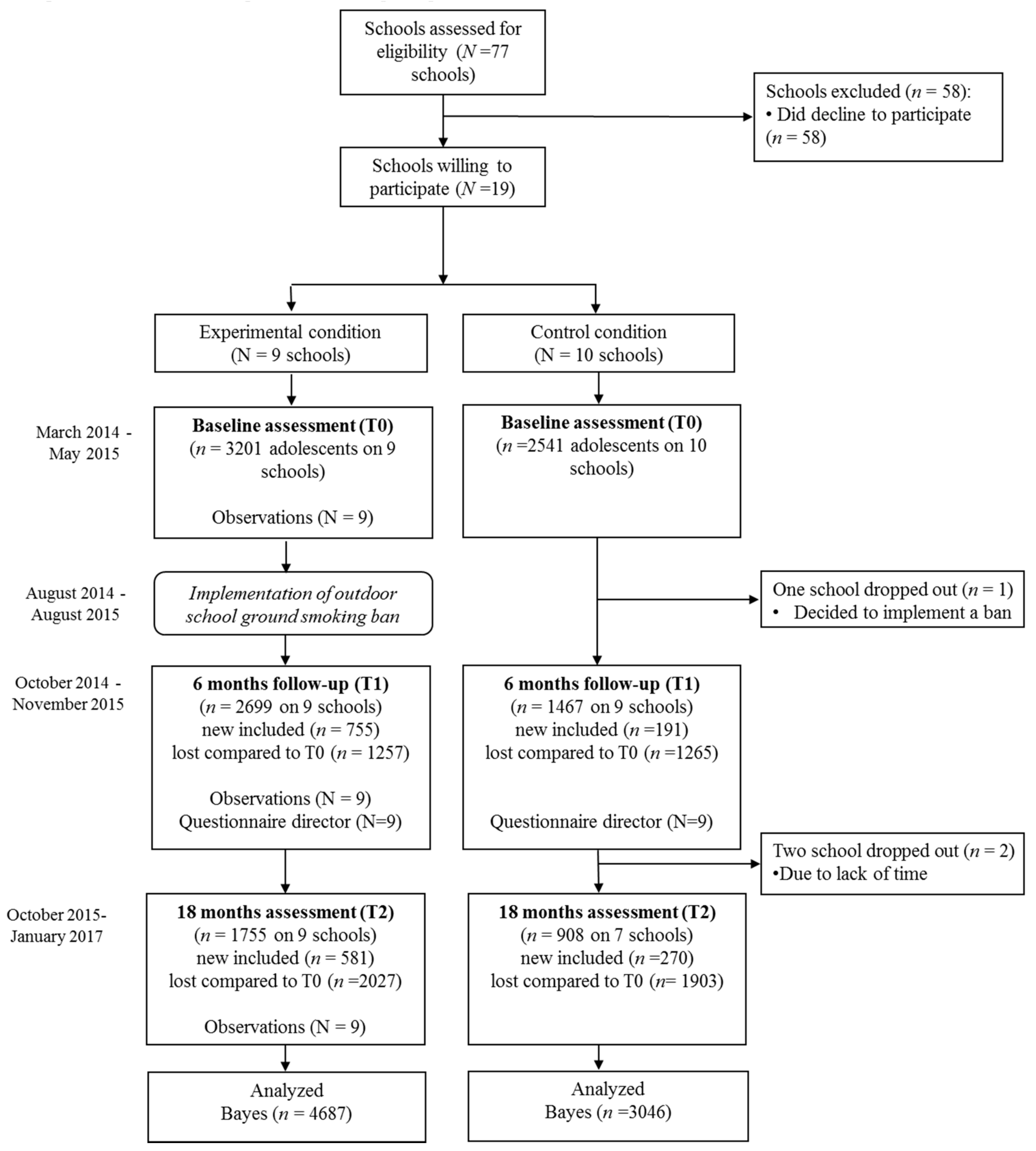
2.1. Procedure and Participants
2.2. Implementation Fidelity of the Ban
2.3. Measures
2.3.1. Conventional Cigarettes
2.3.2. Alternative Tobacco Products (E-Cigarettes with/without Nicotine and Water Pipe)
2.3.3. Sociodemographics
2.3.4. Smoking Policy Variables to Assess Implementation
2.4. Statistical Analysis
3. Results
3.1. Multilevel Analysis
3.2. Implementation Fidelity of the Ban
4. Discussion
5. Strengths and Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Current Tobacco Smoking in Europe. 2017. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/tobacco/data-and-statistics (accessed on 7 September 2017).
- Kraus, L.; Leifman, H.; Vicente, J. The 2015 ESPAD Report: Results from the European School Survey Project on Alcohol and Other Drugs. 2015. Available online: http://www.espad.org/ (accessed on 17 June 2017).
- Welte, J.W.; Barnes, G.M.; Tidwell, M.O.; Hoffman, J.H. Tobacco Use, Heavy use, and dependence among adolescents and young adults in the United States. Subst. Use Misuse 2011, 46, 1090–1098. [Google Scholar] [CrossRef] [PubMed]
- Greenhill, R.; Dawkins, L.; Notley, C.; Finn, M.D.; Turner, J.J.D. Adolescent awareness and use of electronic cigarettes: A review of emerging trends and findings. J. Adolesc. Health 2016, 59, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Van Dorsselaer, S.; Tuithof, M.; Verdurmen, J.; Spit, M.; van Laar, M.; Monshouwer, K. Jeugd en Riskant Gedrag. 2015. Available online: https://assets.trimbos.nl/docs/8e6ef71f-d74e-4696-a67b-98ef82fb2235.pdf (accessed on 17 June 2017).
- Voigt, K. Smoking Norms and the Regulation of E-Cigarettes. Am. J. Pub. Health 2015, 105, 1967–1972. [Google Scholar] [CrossRef] [PubMed]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 1985, 14, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, K.; Alzghoul, B.; Innabi, A.; Meena, N. Is vaping a gateway to smoking: A review of the longitudinal studies. Int. J. Adolesc. Med. Health 2016. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, A.M.; Strong, D.R.; Kirkpatrick, M.G.; Unger, J.B.; Sussman, S.; Riggs, N.R.; Stone, M.D.; Khoddam, R.; Samet, J.M.; Audrain-McGovern, J. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA 2015, 314, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Wills, T.A.; Knight, R.; Sargent, J.; Gibbons, F.; Pagano, I.; Williams, R. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob. Control 2017, 26, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Veeranki, S.P.; Alzyoud, S.; Kheirallah, K.A.; Pbert, L. Waterpipe Use and Susceptibility to Cigarette Smoking among Never-Smoking Youth. Am. J. Prev. Med. 2015, 49, 502–511. [Google Scholar] [CrossRef] [PubMed]
- Soneji, S.; Barrington-Trimis, J.L.; Wills, T.A.; Leventhal, A.M.; Unger, J.B.; Gibson, L.A.; Yang, J.; Primack, B.A.; Andrews, J.A.; Miech, R.A.; et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: A systematic review and meta-analysis. JAMA Pediatr. 2017, 171, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Goniewicz, M.L.; Knysak, J.; Gawron, M.; Kosmider, L.; Sobczak, A.; Kurek, J.; Prokopowicz, A.; Jablonska-Czapla, M.; Rosik-Dulewska, C.; Havel, C.; et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob. Control 2014, 23, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Hajek, P.; Etter, J.-F.; Benowitz, N.; Eissenberg, T.; McRobbie, H. Electronic cigarettes: Review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction 2014, 109, 1801–1810. [Google Scholar] [CrossRef] [PubMed]
- Kienhuis, A.S.; Soeteman-Hernandez, L.G.; Bos, P.M.J.; Cremers, H.W.; Klerx, W.N.; Talhout, R. Potential harmful health effects of inhaling nicotine-free shisha-pen vapor: A chemical risk assessment of the main components propylene glycol and glycerol. Tob. Induc. Dis. 2015, 13, 15. [Google Scholar] [CrossRef] [PubMed]
- Haddad, L.; Kelly, D.L.; Weglicki, L.S.; Barnett, T.E.; Ferrell, A.V.; Ghadban, R. A Systematic Review of Effects of Waterpipe Smoking on Cardiovascular and Respiratory Health Outcomes. Tob. Use Insights 2016, 9, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Rijksinstituut voor Volksgezondheid en Milieu. Waterpijp: Risico op Koolmonoxide-Vergiftiging bij Gebruik. 2016. Available online: https://waterpijp-risico-op-koolmonoxidevergiftiging-bij-gebruik.pdf (accessed on 7 September 2017).
- Joossens, L.; Raw, M. The Tobacco Control Scale 2016. 2017. Available online: http://www.tobaccocontrolscale.org/wp-content/uploads/2017/03/TCS-2016-in-Europe-COMPLETE-LoRes.pdf (accessed on 27 March 2017).
- Lowrie, C.; Pearson, A.L.; Thomson, G. Inequities in coverage of smokefree space policies within the United States. BMC Public Health 2017, 17, 456. [Google Scholar] [CrossRef] [PubMed]
- Breedveld, K.; Lammertink, N. Rookvrije Schoolterreinen. 2016. Available online: http://www.kennisbanksportenbewegen.nl/?file=7409&m=1479732680&action=file.download (accessed on 22 March 2017).
- Longfonds: Stappenplan voor een Rookvrij Schoolterrein. 2017. Available online: https://www.longfonds.nl/schoolterrein (accessed on 22 March 2017).
- Piontek, D.; Buehler, A.; Donath, C.; Floeter, S.; Rudolph, U.; Metz, K.; Gradl, S.; Kroeger, C. School context variables and students’ smoking. Testing a mediation model through multilevel analysis. Eur. Addict. Res. 2008, 14, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Barnett, T.A.; Gauvin, L.; Lambert, M.; O’Loughlin, J.; Paradis, G.; McGrath, J.J. The influence of school smoking policies on student tobacco use. Arch. Pediatr. Adolesc. Med. 2007, 161, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.L.; Chen, F.L.; Hsu, C.C.; Yen, Y.Y.; Chen, T.; Huang, C.M.; Shi, H.Y.; Hu, C.Y.; Lee, C.H. A multilevel-based study of school policy for tobacco control in relation to cigarette smoking among children in elementary schools: Gender differences. Health Educ. Res. 2010, 25, 451–463. [Google Scholar] [CrossRef] [PubMed]
- Pentz, M.A.; Brannon, B.R.; Charlin, V.L.; Barrett, E.J.; Mackinnon, D.P.; Flay, B.R. The power of policy—The relationship of smoking policy to adolescent smoking. Am. J. Public Health 1989, 79, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Kuipers, M.A.G.; de Korte, R.; Soto, V.E.; Richter, M.; Moor, I.; Rimpelä, A.H.; Perelman, J.; Federico, B.; Kunst, A.E.; Lorant, V. School smoking policies and educational inequalities in smoking behaviour of adolescents aged 14–17 years in Europe. J. Epidemiol. Community Health 2015, 70, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Poulin, C.C. School smoking bans: Do they help/do they harm? Drug Alcohol Rev. 2007, 26, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Coppo, A.; Galanti, M.R.; Giordano, L.; Buscemi, D.; Bremberg, S.; Faggiano, F. School policies for preventing smoking among young people. Cochrane Database Syst. Rev. 2014, 10, CD009990. [Google Scholar] [CrossRef] [PubMed]
- Galanti, M.R.; Coppo, A.; Jonsson, E.; Bremberg, S.; Faggiano, F. Anti-tobacco policy in schools: Upcoming preventive strategy or prevention myth? A review of 31 studies. Tob. Control 2014, 23, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Lung Foundation. Monitoring Outdoor School Ground Smoking Bans. 2014. Available online: http://www.alliantienederlandrookvrij.nl/wp-content/uploads/2014/01/Rapportage-Onderzoek-Longfonds-Monitor-2014.pdf (accessed on 7 December 2017).
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2015. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus Statistical Modeling Software: Release 7.0; Muthén & Muthén: Los Angeles, CA, USA, 2012. [Google Scholar]
- Muthén, B.O. Bayesian analysis in Mplus: A brief introduction. Unpublished work. 2010. [Google Scholar]
- Asparouhov, T.; Muthén, B.O. Bayesian Analysis Using Mplus: Technical Implementation. Available online: http://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.310.3903 (accessed on 23 January 2018).
- Peugh, J.L.; Heck, R.H. Conducting three-level longitudinal analyses. J. Early Adolesc. 2017, 37, 7–58. [Google Scholar] [CrossRef]
- Schreuders, M.; Nuyts, P.A.W.; van den Putte, B.; Kunst, A.E. Understanding the impact of school tobacco policies on adolescent smoking behaviour: A realist review. Soc. Sci. Med. 2017, 183, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.W.; Lovato, C.Y.; Card, A.; Manske, S.R. Do students’ perceptions of school smoking policies influence where students smoke? Canada’s Youth Smoking Survey. Cancer Causes Control 2010, 21, 2085–2092. [Google Scholar] [CrossRef] [PubMed]
- Radwan, G.N.; Loffredo, C.A.; Aziz, R.; Abdel-Aziz, N.; Labib, N. Implementation, barriers and challenges of smoke-free policies in hospitals in Egypt. BMC Res. Notes 2012, 5, 568. [Google Scholar] [CrossRef] [PubMed]
- Ashley, M.J.; Northrup, D.A.; Ferrence, R. The Ontario ban on smoking on school property: Issues and challenges in enforcement. Can. J. Public Health 1998, 89, 229–232. [Google Scholar] [PubMed]
- Jancey, J.; Bowser, N.; Burns, S.; Crawford, G.; Portsmouth, L.; Smith, J. No Smoking Here: Examining Reasons for Noncompliance with a Smoke-Free Policy in a Large University. Nicotine Tob. Res. 2014, 16, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Rozema, A.D.; Mathijssen, J.J.P.; Jansen, M.W.J.; van Oers, J.A.M. Sustainability of outdoor school ground smoking bans at secondary schools: A mixed-method study. Eur. J. Public Health 2018, 28, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Burns, S.; Hart, E.; Jancey, J.; Hallett, J.; Crawford, G.; Portsmouth, L. A cross sectional evaluation of a total smoking ban at a large Australian university. BMC Res. Notes 2016, 9, 288. [Google Scholar] [CrossRef] [PubMed]
- Gërxhani, K.; Bruggeman, J. Time lag and communication in changing unpopular norms. PLoS ONE 2015, 10, e0124715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nederlandse Voedsel en Warenautoriteit. Naleving Rookverbod. 2015. Available online: Https://www.nvwa.nl/over-de-nvwa/organisatie/jaarverslagen-en-jaarplannen-nvwa/jaarverslag-2015/naleving-rookverbod (accessed on 22 August 2017).
- Hiemstra, J.M.; de Leeuw, R.N.H.; Engels, R.C.M.E.; Otten, R. What parents can do to keep their children from smoking: A systematic review on smoking-specific parenting strategies and smoking onset. Addict. Behav. 2017, 70, 107–128. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, A.H.; Collins, D.; Parsons, M. ‘A place for healthy activity’: Parent and caregiver perspectives on smokefree playgrounds. Health Place 2015, 31, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Wiium, N.; Wold, B. Family and school influences on adolescent smoking behaviour. Health Educ. 2006, 106, 465–479. [Google Scholar] [CrossRef]
- Thomas, R.E.; McLellan, J.; Perera, R. School-based programmes for preventing smoking. Cochrane Database Syst. Rev. 2013, 4, CD001293. [Google Scholar]
- Brown, T.; Platt, S.; Amos, A. Equity impact of interventions and policies to reduce smoking in youth: Systematic review. Tob. Control 2014, 23, e98–e105. [Google Scholar] [CrossRef] [PubMed]
- Gorber, S.C.; Schofield-Hurwitz, S.; Hardt, J.; Levasseur, G.; Tremblay, M. The accuracy of self-reported smoking: A systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob. Res. 2009, 11, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Dolcini, M.M.; Adler, N.E.; Ginsberg, D. Factors Influencing Agreement between Self-Reports and Biological Measures of Smoking among Adolescents. J. Res. Adolesc. 1996, 6, 515–542. [Google Scholar]
| Experimental Condition (E) (n = 4687) | Control Condition (C) (n = 3046) | Significant Difference between E and C + | ||
|---|---|---|---|---|
| Sex | χ2 = 10.985 (1), p = 0.001 | |||
| Boy | 2355 (50.7) | 1647 (54.5) | ||
| Girl | 2293 (49.3) | 1373 (45.5) | ||
| Migration background | χ2 = 40.53 (1), p < 0.001 | |||
| Native | 3815 (83.5) | 2317 (77.6) | ||
| Migrant descent ! | 755 (16.5) | 668 (22.4) | ||
| Age in years (mean (SD) | 13.9 (1.06) | 13.5 (1.10) | t(5623) = −15.763, p < 0.001 | |
| Education level * | χ2 = 1087.36 (3), p < 0.001 | |||
| Low | 1557 (49.2) | 283 (11.3) | ||
| Average | 979 (31.0) | 891 (35.7) | ||
| Middle | 297 (9.4) | 763 (30.6) | ||
| High | 329 (10.4) | 559 (22.4) | ||
| Grade | χ2 = 172.47 (5), p < 0.001 | |||
| 7th | 1003 (21.5) | 839 (27.7) | ||
| 8th | 1351 (29.0) | 933 (30.8) | ||
| 9th | 1707 (36.6) | 1116 (36.8) | ||
| 10th | 566 (12.1) | 118 (3.9) | ||
| 11th | 12 (0.3) | 8 (0.3) | ||
| 12th | 21 (0.5) | 18 (0.6) | ||
| Total Sample | Experimental Condition ‘Ever Users’ | Control Condition ‘Ever Users’ | Total ‘Ever Users’ | ||
|---|---|---|---|---|---|
| Smoking prevalence | n | n (%) | n (%) | n (%) | |
| T0 | 5695 | 745 (23.4) | 485 (19.3) | 1230 (21.6) | |
| T1 | 4690 | 1120 (37.6) | 655 (38.2) | 1775 (37.8) | |
| T2 | 4020 | 1547 (59.6) | 771 (54.2) | 2318 (57.7) | |
| Smoking onset | |||||
| T0 | 4465 | - | - | - | |
| T1 | 2347 | 132 (6.7) | 84 (7.4) | 216 (7.0) | |
| T2 | 1473 | 279 (21.0) | 122 (15.8) | 401 (19.1) | |
| E-cigarette with nicotine | |||||
| T0 | 5517 | 481 (15.6) | 260 (10.7) | 741 (13.4) | |
| T1 | 4069 | 402 (15.3) | 208 (14.5) | 610 (15.0) | |
| T2 | 2568 | 346 (20.5) | 142 (16.1) | 488 (16.3) | |
| E-cigarette without nicotine | |||||
| T0 | 5514 | 921 (29.8) | 654 (26.9) | 1575 (28.6) | |
| T1 | 4061 | 846 (32.2) | 414 (28.9) | 1260 (31.0) | |
| T2 | 2559 | 580 (34.5) | 251 (28.6) | 831 (32.5) | |
| Water pipe | |||||
| T0 | 5517 | 725 (23.4) | 455 (18.8) | 1180 (21.4) | |
| T1 | 4066 | 673 (25.6) | 266 (18.5) | 939 (23.1) | |
| T2 | 2561 | 560 (33.3) | 191 (21.7) | 751 (29.3) | |
| Smoking Prevalence | Smoking Onset | ||||||
|---|---|---|---|---|---|---|---|
| Median Estimate (Posterior SD) + | One-Tailed p-Value | Bayesian 95% Credibility Interval * | Median Estimate (Posterior SD) + | One-Tailed p-Value | Bayesian 95% Credibility Interval * | ||
| Regression | |||||||
| coefficients | Sex | −2.56 (0.70) | 0.000 | −4.05–−1.27 * | −0.06 (0.41) | 0.44 | −0.092–0.74 |
| Migration background | 2.24 (0.91) | 0.005 | 0.54–4.11 * | −0.66 (0.63) | 0.14 | −1.95–0.53 | |
| Grade | 5.89 (0.72) | 0.000 | 4.69–7.48 * | 0.048 (0.26) | 0.43 | −0.49–0.054 | |
| Educational level | −4.20 (0.71) | 0.000 | −5.77–−3.00 * | −0.20 (0.33) | 0.26 | −0.90–0.42 | |
| Time | 3.64 (1.15) | 0.000 | 1.85–6.24 * | 2.90 (1.26) | 0.000 | 1.00–5.82 * | |
| Condition | −2.80 (1.75) | 0.06 | −6.22–0.68 | −1.24 (1.31) | 0.15 | −4.18–0.99 | |
| Condition*time | 0.52 (0.57) | 0.17 | −0.58–1.66 | 1.42 (0.70) | 0.01 | 0.21–2.96 * | |
| Variance | Intercept variance individual level | 331.74 (86.68) | 0.000 | 213.79–547.02 * | 39.15 (13.09) | 0.000 | 17.40–69.44 * |
| components | Slope variance individual level | 0.14 (0.20) | 0.000 | 0.004–0.75 * | 0.15 (0.23) | 0.000 | 0.01–0.83 * |
| Intercept variance school level | 41.39 (34.91) | 0.000 | 15.50–143.52 * | 7.31 (8.11) | 0.000 | 2.09–30.38 * | |
| Slope variance school level | 1.26 (1.03) | 0.000 | 0.44–4.19 * | 0.47 (0.94) | 0.000 | 0.11–3.28 * | |
| Covariance between school level intercept and slope | 5.15 (5.12) | 0.005 | 1.03–19.92 * | −1.08 (2.48) | 0.17 | −7.94–1.21 | |
| Fit index | School ICC | 0.11 | 0.16 | ||||
| Iterations ~ | 419,300 | 757,600 | |||||
| E-Cigarettes with Nicotine | E-Cigarettes without Nicotine | Water Pipe | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median Estimate (Posterior SD) + | One-Tailed p-Value | Bayesian 95% Credibility Interval * | Median Estimate (Posterior SD) + | One-Tailed p-Value | Bayesian 95% Credibility Interval * | Median Estimate (Posterior SD) + | One-Tailed p-Value | Bayesian 95% Credibility Interval * | ||
| Regression | ||||||||||
| coefficients | Sex | −0.93 (0.12) | 0.000 | −1.17–−0.700 * | −0.94 (0.09) | 0.000 | −1.11–−0.7700 * | −0.93 (0.03) | 0.000 | −1.19–−0.69 * |
| Migration Background | 0.33 (0.14) | 0.007 | 0.07–0.600 * | 0.27 (0.13) | 0.02 | 0.02–0.5100 * | 0.75 (0.17) | 0.000 | 0.43–1.11 * | |
| Grade | 0.66 (0.08) | 0.000 | 0.51–0.820 * | 0.48 (0.06) | 0.000 | 0.37–0.6100 * | 1.15 (0.11) | 0.000 | 0.94–1.36 * | |
| Educational level | −0.036 (0.08) | 0.000 | −0.51–−0.210 * | −0.45 (0.06) | 0.000 | −0.57–−0.3300 * | −0.57 (0.10) | 0.000 | −0.077–−0.40 * | |
| Time | 1.09 (0.26) | 0.000 | 0.59–1.610 * | 0.40 (0.24) | 0.05 | −0.06–0.89 | 0.20 (0.25) | 0.21 | −0.31–0.70 | |
| Condition | −0.19 (0.41) | 0.31 | −1.01–0.59 | −0.03 (0.32) | 0.46 | −0.67–0.59 | 0.32 (0.39) | 0.20 | −0.43–1.10 | |
| Condition*time | −0.42 (0.23) | 0.03 | −0.88–0.02 | −0.15 (0.20) | 0.24 | −0.55–0.26 | 0.20 (0.25) | 0.21 | −0.30–0.69 | |
| Variance | Intercept variance individual level | 5.42 (0.83) | 0.000 | 3.77–6.810 * | 5.34 (0.54) | 0.000 | 4.43–6.6100 * | 9.08 (1.41) | 0.000 | 6.52–11.98 * |
| components | Slope variance individual level | 0.49 (0.17) | 0.000 | 0.24–0.890 * | 0.44 (0.12) | 0.000 | 0.20–0.6700 * | 0.58 (0.22) | 0.000 | 0.19–1.04 * |
| Intercept variance school level | 0.64 (0.31) | 0.000 | 0.31–1.480 * | 0.37 (0.19) | 0.000 | 0.17–0.8800 * | 0.55 (0.29) | 0.000 | 0.25–1.36 * | |
| Slope variance school level | 0.13 (0.07) | 0.000 | 0.06–0.320 * | 0.12 (0.06) | 0.000 | 0.06–0.2700 * | 0.15 (0.08) | 0.000 | 0.07–0.38 * | |
| Covariance between school level intercept and slope | 0.002 (0.12) | 0.49 | −0.23–0.25 | 0.004 (0.07) | 0.47 | −0.13–0.15 | −0.04 (0.11) | 0.33 | −0.29–0.15 | |
| Fit index | School ICC | 0.11 | 0.06 | 0.06 | ||||||
| Iterations ~ | 13,000 | 5700 | 4800 | |||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rozema, A.D.; Hiemstra, M.; Mathijssen, J.J.P.; Jansen, M.W.J.; Van Oers, H.J.A.M. Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up. Int. J. Environ. Res. Public Health 2018, 15, 205. https://doi.org/10.3390/ijerph15020205
Rozema AD, Hiemstra M, Mathijssen JJP, Jansen MWJ, Van Oers HJAM. Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up. International Journal of Environmental Research and Public Health. 2018; 15(2):205. https://doi.org/10.3390/ijerph15020205
Chicago/Turabian StyleRozema, Andrea D., Marieke Hiemstra, Jolanda J. P. Mathijssen, Maria W. J. Jansen, and Hans J. A. M. Van Oers. 2018. "Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up" International Journal of Environmental Research and Public Health 15, no. 2: 205. https://doi.org/10.3390/ijerph15020205
APA StyleRozema, A. D., Hiemstra, M., Mathijssen, J. J. P., Jansen, M. W. J., & Van Oers, H. J. A. M. (2018). Impact of an Outdoor Smoking Ban at Secondary Schools on Cigarettes, E-Cigarettes and Water Pipe Use among Adolescents: An 18-Month Follow-Up. International Journal of Environmental Research and Public Health, 15(2), 205. https://doi.org/10.3390/ijerph15020205





