Prevention of Common Mental Disorders in Employees. Perspectives on Collaboration from Three Health Care Professions
Abstract
:1. Introduction
2. Materials and Methods
- Experience of direct contact with the respective other professional groups (1 item, yes - no) and number of patients/employees.
- Reasons for non-conclusion in the case of active contact attempts (three items: contact partner could not be reached, contact/contact attempts were too time-consuming, patient/employee did not agree to contact).
- Evaluation of cooperation—two items: last cooperation and all experienced cooperation (rating from 1 = very good to 6 = very bad) and evaluating the importance of collaboration with the other two professions (four specified response options from very important to very unimportant).
- Evaluation of interest in further educational training (four specified response options from very high to very low interest).
Statistical Methods
- Occupational health physicians: age, sex.
- Primary care physicians: sex, size of the city (indicated by postal code).
- Psychotherapists: sex, size of the city, professional differences (psychological psychotherapist vs. physician working as a psychotherapist).
3. Results
3.1. Sample Description
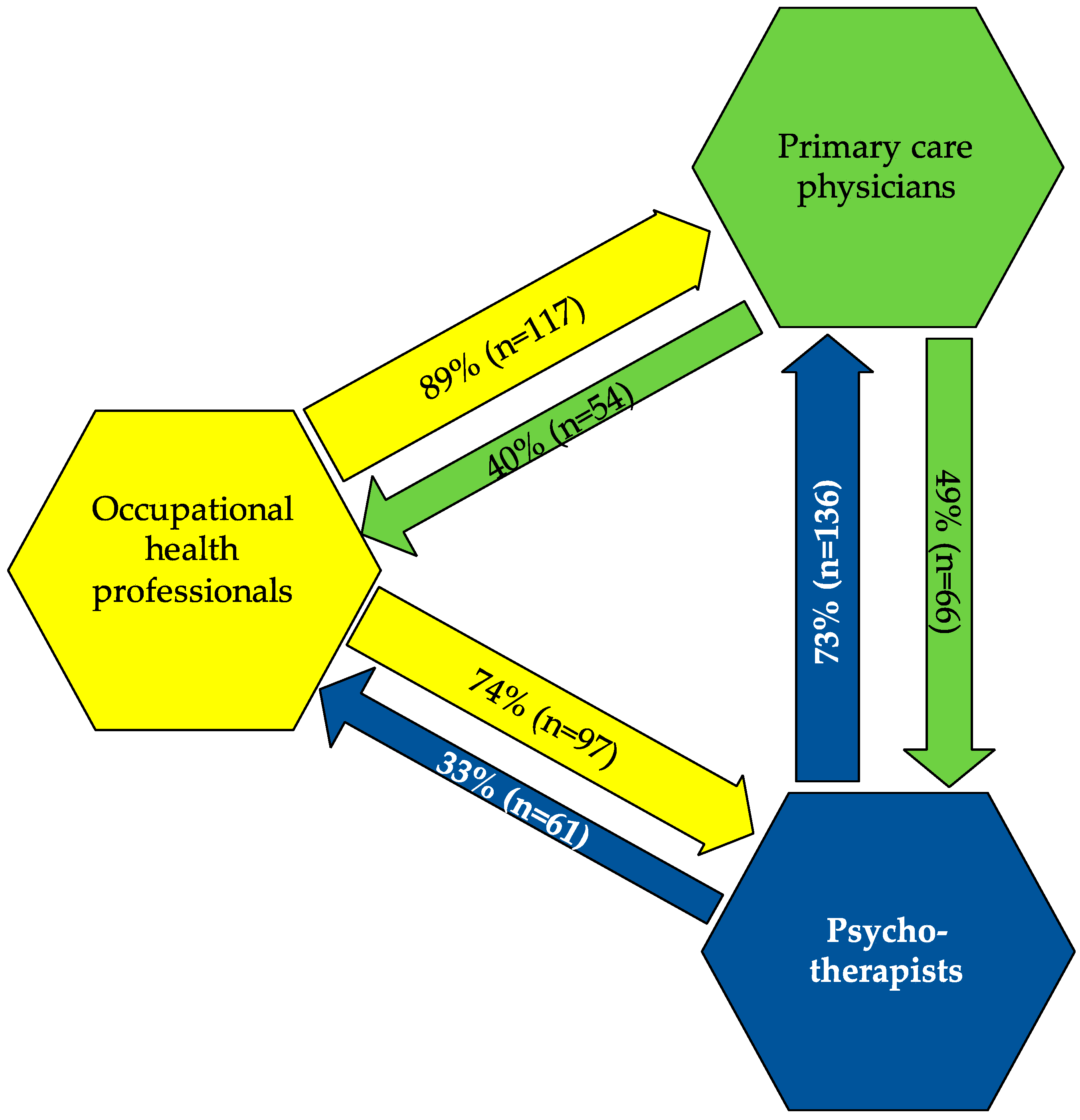
3.2. Extent of Collaborations between Three Professions to Prevent Common Mental Disorders in Employees
3.3. Barriers of Collaboration between Three Professions to Prevent Common Mental Disorders in Employees
3.4. Evaluation of Collaborations between Three Professions to Prevent Common Mental Disorders in Employees
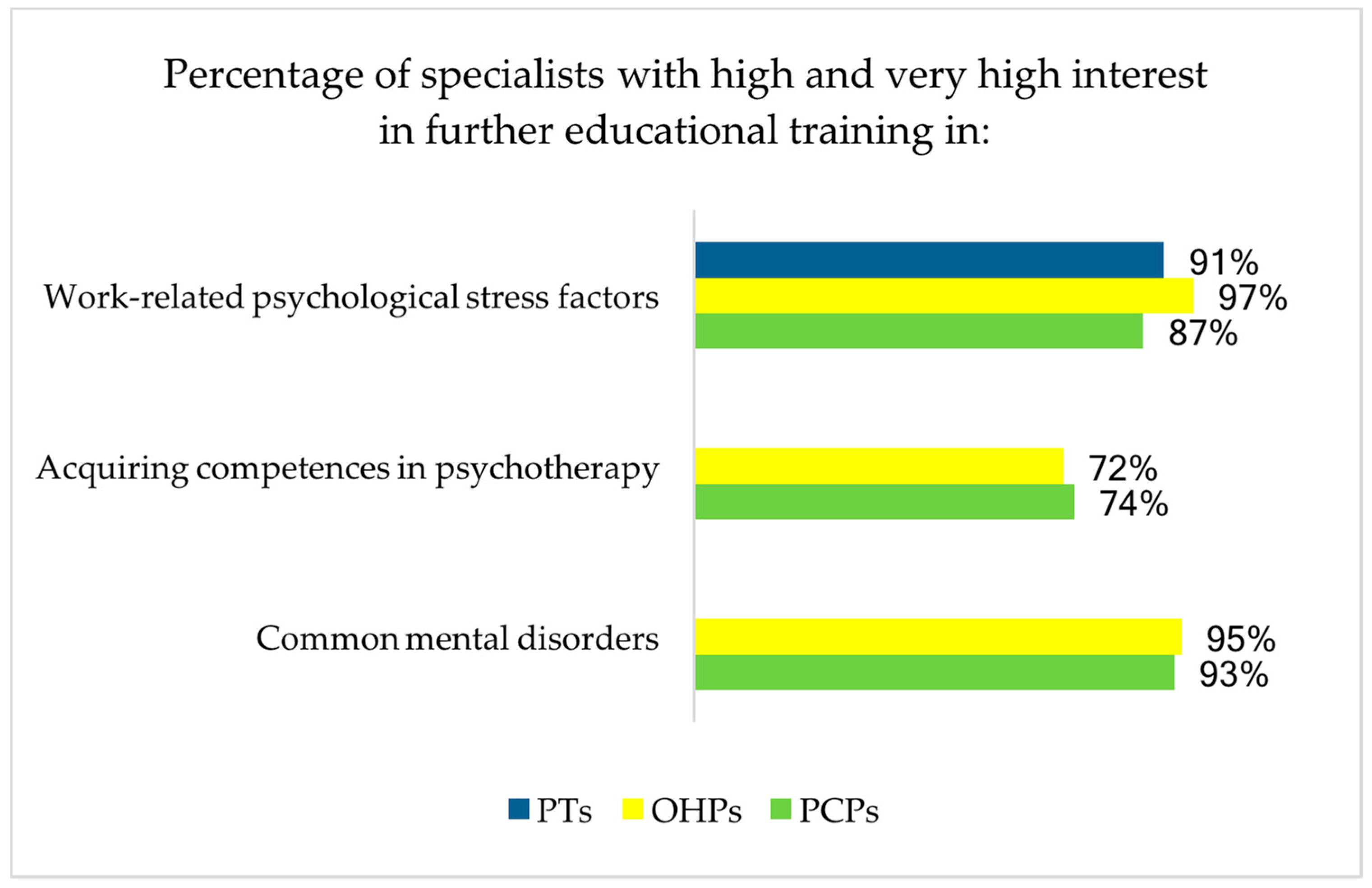
3.5. Significance of Further Educational Training at the Interface of Three Professions to Prevent Common Mental Disorders in Employees
4. Discussion
4.1. Cooperation between Occupational Health Physicians and Primary Care Physicians
4.2. Cooperation between Occupational Health Physicians and Psychotherapists
4.3. Cooperation between Primary Care Physicians and Psychotherapists
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Collaborator Study Group 2013. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar]
- Ferrari, A.J.; Charlson, F.J.; Norman, R.E.; Patten, S.B.; Freedman, G.; Murray, C.J.; Vos, T.; Whiteford, H.A. Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLoS Med. 2013, 10, e1001547. [Google Scholar] [CrossRef] [PubMed]
- OECD (Ed.) Sick on the Job? Myths and Realities about Mental Health and Work; OECD Publishing: Paris, France, 2012. [Google Scholar]
- Thornicroft, G.; Chatterji, S.; Evans-Lacko, S.; Gruber, M.; Sampson, N.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Andrade, L.; Borges, G.; et al. Under-treatment of people with major depressive disorder in 21 countries. Br. J. Psychiatry 2017, 210, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Mack, S.; Jacobi, F.; Gerschler, A.; Strehle, J.; Höfler, M.; Busch, M.A.; Maske, U.E.; Hapke, U.; Seiffert, I.; Gaebel, W.; et al. Self-reported utilization of mental health services in the adult German population—Evidence for unmet needs ? Results of the DEGS1-Mental Health Module (DEGS1-MH ). Int. J. Methods Psychiatr. Res. 2014, 23, 289–303. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Henriksen, C.A.; ten Have, M.; de Graaf, R.; Stein, M.B.; Enns, M.W.; Sareen, J. Common Mental Disorder Diagnosis and Need for Treatment are Not the Same: Findings from the NEMESIS Study. Adm. Policy Ment. Health Ment. Health Serv. Res. 2017, 44, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Harris, M.G.; McKeon, G.; Baxter, A.; Pennell, C.; Barendregt, J.J.; Wang, J. Estimating remission from untreated major depression: A systematic review and meta-analysis. Psychol. Med. 2013, 43, 1569–1585. [Google Scholar] [CrossRef] [PubMed]
- Ivandic, I.; Kamenov, K.; Rojas, D.; Cerón, G.; Nowak, D.; Sabariego, C. Determinants of work performance in workers with depression and anxiety: A cross-sectional study. Int. J. Environ. Res. Public Health 2017, 14, 466. [Google Scholar] [CrossRef] [PubMed]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rüsch, N.; Brown, J.S.L.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015, 45, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Bundespsychotherapeutenkammer (BPtK). BPtK-Studie zu Wartezeiten in der ambulanten psychotherapeutischen Versorgung; Umfrage der Landespsychotherapeutenkammern und der BPtK; Veröffentlichung der Bundespsychotherapeutenkammer: Berlin, Germany, 2011; p. 46. [Google Scholar]
- Magaard, J.L.; Seeralan, T.; Schulz, H.; Levke, A.; Tt, B. Factors associated with help-seeking behavior among individuals with major depression: A systematic review. PLoS ONE 2017, 12, e0176730. [Google Scholar] [CrossRef] [PubMed]
- Jacobi, F.; Becker, M.; Bretschneider, J.; Müllender, S.; Thom, J.; Hapke, U.; Maier, W. Ambulante fachärztliche Versorgung psychischer Störungen: Kleine regionale Unterschiede im Bedarf, große regionale Unterschiede in der Versorgungsdichte. [Provision of outpatient specialist care for mental disorders. Minor regional differences in treatment]. Nervenarzt 2016, 87, 1211–1221. [Google Scholar] [CrossRef] [PubMed]
- Munk-Jørgensen, P.; Allgulander, C.; Dahl, A.A.; Foldager, L.; Holm, M.; Rasmussen, I.; Virta, A.; Huuhtanen, M.-T.; Wittchen, H.-U. Prevalence of generalized anxiety disorder in general practice in Denmark, Finland, Norway, and Sweden. Psychiatr. Serv. 2006, 57, 1738–1744. [Google Scholar] [CrossRef] [PubMed]
- Wittchen, H.-U.; Härtling, S.; Dukes, E.; Morlock, R.; Edelsberg, J.; Oster, G.; Berger, A. Generalized anxiety disorder in primary care. Patterns of healthcare utilization in Germany. MMW Fortschr. Med. 2012, 154, 77–84. [Google Scholar] [PubMed]
- Bramesfeld, A.; Ungewitter, C.; Böttger, D.; El Jurdi, J.; Losert, C.; Kilian, R. What promotes and inhibits cooperation in mental health care across disciplines, services and service sectors? A qualitative study. Epidemiol. Psychiatr. Sci. 2012, 21, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Baumgardt, J.; Moock, J.; Rossler, W.; Kawohl, W. Aspects of sustainability: Cooperation, job satisfaction, and burnout among Swiss psychiatrists. Front. Public Health 2015, 3, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lasker, R.D.; Weiss, E.S.; Miller, R. Promoting collaborations that improve health. Educ. Health 2001, 14, 163–172. [Google Scholar] [CrossRef]
- Joosen, M.C.W.; Brouwers, E.P.M.; van Beurden, K.M.; Terluin, B.; Ruotsalainen, J.H.; Woo, J.-M.; Choi, K.-S.; Eguchi, H.; Moriguchi, J.; van der Klink, J.J.L.; et al. An international comparison of occupational health guidelines for the management of mental disorders and stress-related psychological symptoms. Occup. Environ. Med. 2015, 72, 313–322. [Google Scholar] [CrossRef] [PubMed]
- OECD. Fit Mind, Fit Job: From Evidence to Practice in Mental Health and Work, Mental Health and Work; OECD Publishing: Paris, France, 2015. [Google Scholar]
- Vlasveld, M.C.; van der Feltz-Cornelis, C.M.; Adèr, H.J.; Anema, J.R.; Hoedeman, R.; van Mechelen, W.; Beekman, A.T.F. Collaborative care for major depressive disorder in an occupational healthcare setting. Br. J. Psychiatry 2012, 200, 510–511. [Google Scholar] [CrossRef] [PubMed]
- Lugtenberg, M.; van Beurden, K.M.; Brouwers, E.P.M.; Terluin, B.; van Weeghel, J.; van der Klink, J.J.L.; Joosen, M.C.W. Occupational physicians’ perceived barriers and suggested solutions to improve adherence to a guideline on mental health problems: Analysis of a peer group training. BMC Health Serv. Res. 2016, 16, 271. [Google Scholar] [CrossRef] [PubMed]
- Van Beurden, K.M.; Brouwers, E.P.M.; Joosen, M.C.W.; de Boer, M.R.; van Weeghel, J.; Terluin, B.; van der Klink, J.J.L. Effectiveness of an intervention to enhance occupational physicians’ guideline adherence on sickness absence duration in workers with common mental disorders: A cluster-randomized controlled trial. J. Occup. Rehabil. 2017, 27, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Muschalla, B.; Fay, D.; Linden, M. Self-reported workplace perception as indicators of work anxieties. Occup. Med. 2016, 66, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Du Prel, J.-B.; March, S.; Schröder, H.; Peter, R. Berufliche Gratifikationskrisen und Arbeitsunfähigkeit in Deutschland. Bundesgesundheitsblatt Gesundheitsforsch. Gesundheitsschutz 2015, 58, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijsen, K.; Faber, B.; Verbeek, J.H.; Neumeyer-Gromen, A.; Hees, H.L.; Verhoeven, A.C.; van der Feltz-Cornelis, C.M.; Bültmann, U. Interventions to improve return to work in depressed people. Cochrane Database Syst. Rev. 2014, 12. [Google Scholar] [CrossRef] [PubMed]
- Moßhammer, D.; Natanzon, I.; Manske, I.; Grutschkowski, P.; Rieger, M.A. Deficiencies and barriers of the cooperation between German general practitioners and occupational health physicians? A qualitative content analysis of focus groups. Z. Evid. Fortbild. Qual. Gesundhwes. 2012, 106, 639–648. [Google Scholar] [CrossRef] [PubMed]
- Preiser, C.; Wittich, A.; Rieger, M.A. Psychosomatische Sprechstunde im Betrieb—Gestaltungsformen des Angebots Psychosomatic consultation in the workplace—Description and modeling of a new health-related service. Gesundheitswesen 2015, 77, 166–171. [Google Scholar] [CrossRef]
- Preiser, C.; Rothermund, E.; Wittich, A.; Gündel, H.; Rieger, M.A. Psychosomatic consultation in the workplace—Opportunities and limitations of the services offered. Results of a qualitative study. Int. Arch. Occup. Environ. Health 2016, 89, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Rothermund, E.; Gündel, H.; Kilian, R.; Hölzer, M.; Reiter, B.; Mauss, D.; Rieger, M.A.; Müller-Nübling, J.; Wörner, A.; von Wietersheim, J.; Beschoner, P. Behandlung psychosomatischer Beschwerden im Arbeitskontext—Konzept und erste Daten (Treatment of psychosomatic disorders occurring in the vocational context—Concept and first findings). Z. Psychosom. Med. Psychother. 2014, 60, 177–189. [Google Scholar] [PubMed]
- Kruse, J.; Larisch, A.; Hofmann, M.; Herzog, W. Ambulante psychosomatische und psychotherapeutische Versorgung in Deutschland—Versorgungsprofile abgebildet durch Daten der Kassenärztlichen Bundesvereinigung (KBV) (Psychosomatic and psychotherapeutic outpatient care in Germany—Capacity profile based). Z. Psychosom. Med. Psychother. 2013, 59, 254–272. [Google Scholar] [PubMed]
- Rothermund, E.; Kilian, R.; Rottler, E.; Hölzer, M.; Mayer, D.; Rieger, M.A.; Gündel, H. Improving access to mental health care by delivering psychotherapeutic car in the workplace: A cross-sectional exploratory trial. PLoS ONE 2017, 12, e0169559. [Google Scholar] [CrossRef] [PubMed]
- Rothermund, E.; Gündel, H.; Rottler, E.; Hölzer, M.; Mayer, D.; Rieger, M.; Kilian, R. Effectiveness of psychotherapeutic consultation in the workplace: A controlled observational trial. BMC Public Health 2016, 16, 891. [Google Scholar] [CrossRef] [PubMed]
- Evans-Lacko, S.; Koeser, L.; Knapp, M.; Longhitano, C.; Zohar, J.; Kuhn, K. Evaluating the economic impact of screening and treatment for depression in the workplace. Eur. Neuropsychopharmacol. 2016, 26, 1004–1013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinchin, I.; Doran, C.M. The economic cost of suicide and non-fatal suicide behavior in the Australian workforce and the potential impact of a workplace suicide prevention strategy. Int. J. Environ. Res. Public Health 2017, 14, 347. [Google Scholar] [CrossRef] [PubMed]
- Yelin, E.; Mathias, S.D.; Buesching, D.P.; Rowland, C.; Calucin, R.Q.; Fifer, S. The impact on employment of an intervention to increase recognition of previously untreated anxiety among primary care physicians. Soc. Sci. Med. 1996, 42, 1069–1075. [Google Scholar] [CrossRef]
- Michaelis, M.; Lange, R.; Junne, F.; Rothermund, E.; Zipfel, S.; Gündel, H.; Rieger, M.A. Prevention of common mental disorders in employees—Conception, study design and sample characteristics of a multi-target survey. Ment. Health Prev. 2016, 4, 88–95. [Google Scholar] [CrossRef]
- Burgess, S.; Rieger, M.A.; Junne, F.; Rothermund, E.; Gündel, H.; Zipfel, S.; Michaelis, M. Prevention of common mental disorders in working age: Perceptions of employees towards causes and prevention. Arbeitsmedizin Sozialmedizin Umweltmedizin 2017, 52. [Google Scholar] [CrossRef]
- Moßhammer, D.; Natanzon, I.; Manske, I.; Grutschkowski, P.; Rieger, M.A. Cooperation between general practitioners and occupational health physicians in Germany: How can it be optimized? A qualitative study. Int. Arch. Occup. Environ. Health 2014, 87, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Moßhammer, D.; Michaelis, M.; Mehne, J.; Wilm, S.; Rieger, M.A. General practitioners’ and occupational health physicians’ views on their cooperation: A cross-sectional postal survey. Int. Arch. Occup. Environ. Health 2015. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Ménard, C.; Richard, J.-B.; Demortière, G.; Beck, F. Collaboration between general practitioners and occupational physicians: A comparison of the results of two national surveys in France. J. Occup. Environ. Med. 2014, 56, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Brohan, E.; Henderson, C.; Wheat, K.; Malcolm, E.; Clement, S.; Barley, E.; Slade, M.; Thornicroft, G. Systematic review of beliefs, behaviors and influencing factors associated with disclosure of a mental health problem in the workplace. BMC Psychiatry 2012, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Völter-Mahlknecht, S.; Rieger, M.A. Patient care at the interface between rehabilitation and occupational health physicians—A systematic review focusing health care organizations. Dtsch. Medizinische Wochenschrift 2014, 139, 1609–1614. [Google Scholar]
- Dewa, C.S.; Hoch, J.S.; Goering, P. “Using financial incentives to promote shared mental health care”: Comment. Can. J. Psychiatry La Rev. Can. Psychiatr. 2001, 46, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Arbeitsgemeinschaft der wissenschaftlichen medizinischen Fachgesellschaften (AWMF). S 3 Leitlinie: Umgang mit Patienten mit Nicht-Spezifischen, Funktionellen und Somatoformen Körperbeschwerden (S3-Guideline ’Management of Patients with Non-Specific, Functional and Somatoform Body Disorders); Schattauer: Stuttgart, Germany, 2012; Volume 109, pp. 1–232. [Google Scholar]
- Burman-Roy, S.; Butterworth, M.; Madan, I.; Henderson, M.; Harvey, S.B. Which patients are seen by an occupational psychiatry service? Occup. Med. Lond. 2013, 63, 507–509. [Google Scholar] [CrossRef] [PubMed]
- Joisten, H. Disease Management Programme—Wie es weiterging. Forum Psychother. Prax. 2002, 2, 175–198. [Google Scholar] [CrossRef]
- Bühring, P. Bessere Versorgung durch strukturierte Zusammenarbeit. Dtsch. Arztebl. 2015, 112, 120–121. [Google Scholar]
- Wiesemann, A. Nutritional counseling in German general practices: A holistic approach. Am. J. Clin. Nutr. 1997, 65, 1957S–1962S. [Google Scholar] [CrossRef] [PubMed]
- Oriol-Zerbe, C.; Abholz, H.H. Primary prevention of cardiovascular diseases by lipid-lowering treatment in German general practice: Results from GPs ignoring guidelines and risk calculators. Eur. J. Gen. Pract. 2007, 13, 27–34. [Google Scholar] [CrossRef] [PubMed]

| OHP 1 (n = 133) | PCP 2 (n = 136) | PT 3 (n = 186) | Differences between Groups, Stat. Test | |
|---|---|---|---|---|
| Age (years, SD), n valid | 54.9 (8.0), 133 | 53.7 (8.6), 130 | 53.9 (8.6), 183 | n.s., MW-U-test |
| Gender (male, n/n valid) | 52.6% (70/133) | 59.6% (81/136) | 30.1% (56/186) | OHP-PCP n.s., OHP-PT p = 0.000, phi = 0.23, PCP-PT p = 0.000, phi = 0.29, Chi2 test |
| Professional experience (years working within that specialization or in own practice, SD), n valid | 26.7 (8.5), 114 | 18.3 (9.3), 127 | 13.6 (8.2),182 | n.s., MW-U-test |
| Practicing in urban centers | 57.0% (73/128) | 30.9% (42/136) | 60.0% (111/185) | OHP-PCP p = 0.000, phi = 0.26, PCP-PT p = 0.000, phi = 0.29; OHP-PT n.s., Chi-2 test |
| Responding Group | Addressed Collaboration Group | ||
|---|---|---|---|
| OHPs | PCPs | PTs | |
| OHP | - | 4 13.4 (45.5) n = 117/118 | 2 10.4 (43.7) n = 97/97 |
| PCP | 2 2.3 (3.0) n = 54/54 | - | 2 4.6 (7.2) n = 65/66 |
| PT | 1 2.4 (5.2) n = 61/61 | 3 9.5 (41.1) n = 61/61 | - |
| Contact Attempts between… | Reasons for Unsuccessful Contact | |||
|---|---|---|---|---|
| n | Contact Partner Was Not Available % (n) | Contact Attempt Was Too Time-Consuming % (n) | Patient/Employee Did Not Agree to Contact % (n) | |
| occupational health physicians and primary care physicians | 115 | 14% (16) | 13% (15) | 12% (14) |
| occupational health physicians and psychotherapists | 95 | 33% (31) | 14% (13) | 17% (16) |
| primary care physicians and occupational health physicians | 54 | 9% (5) | 7% (4) | 2% (1) |
| primary care physicians and psychotherapists | 67 | 15% (10) | 9% (6) | 0% (0) |
| psychotherapists and occupational health physicians | 60 | 3% (2) | 2% (1) | 3% (2) |
| psychotherapists and primary care physicians | 135 | 2% (3) | 2% (3) | 0% (0) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rothermund, E.; Michaelis, M.; Jarczok, M.N.; Balint, E.M.; Lange, R.; Zipfel, S.; Gündel, H.; Rieger, M.A.; Junne, F. Prevention of Common Mental Disorders in Employees. Perspectives on Collaboration from Three Health Care Professions. Int. J. Environ. Res. Public Health 2018, 15, 278. https://doi.org/10.3390/ijerph15020278
Rothermund E, Michaelis M, Jarczok MN, Balint EM, Lange R, Zipfel S, Gündel H, Rieger MA, Junne F. Prevention of Common Mental Disorders in Employees. Perspectives on Collaboration from Three Health Care Professions. International Journal of Environmental Research and Public Health. 2018; 15(2):278. https://doi.org/10.3390/ijerph15020278
Chicago/Turabian StyleRothermund, Eva, Martina Michaelis, Marc N. Jarczok, Elisabeth M. Balint, Rahna Lange, Stephan Zipfel, Harald Gündel, Monika A. Rieger, and Florian Junne. 2018. "Prevention of Common Mental Disorders in Employees. Perspectives on Collaboration from Three Health Care Professions" International Journal of Environmental Research and Public Health 15, no. 2: 278. https://doi.org/10.3390/ijerph15020278





