1. Introduction
On-call or stand-by is a form of scheduling whereby an employee can be called into work under emergency or unpredictable circumstances [
1]. On-call arrangements typically allow for 24/7 work coverage, without the financial burden of providing 24/7 active coverage or when fixed rostering is not possible [
1,
2]. The industries that typically utilise on-call working arrangements include health care, emergency services, maintenance, and information technology [
1]. In Australia and Europe, 20–25% of the workforce are required to do on-call work as part of their regular employment [
3,
4]. Furthermore, on-call work scheduling is becoming increasingly prevalent, for example from 2005 to 2015 the proportion of on-call workers in the United States (US) increased from 2% to 17% [
3,
5].
On-call arrangements are often utilised when workloads may be low; as such they typically occur outside of normal working hours, particularly at night [
6]. When on-call periods occur overnight, there is likely to be a significant reduction in sleep [
6]. For example, railroad engineers [
7] and gas and electricity supply company supervisors [
8] reported obtaining 0.5–1.5 h less sleep per night during on-call periods compared with not on-call. There is also evidence to suggest that being on-call, regardless of whether an employee is actually called, can also adversely impact sleep duration [
9]. For example, in a study of hospital doctors, shorter sleep was reported when on-call compared with not on-call, even when no calls were actually received [
10]. The major difference between on-call work and other irregular work schedules (e.g., shift work) is the inherent unpredictability of whether or not a worker will receive a call, and secondly whether or not they will be required to return to work.
Adults should regularly sleep seven hours or more per night to support optimal health [
11]. Inadequate sleep (less than seven hours) is associated with a plethora of adverse health impacts on a range of physiological and psychological functions, including neurobehavioural performance [
12], metabolism [
13], appetite regulation [
14], and immune function [
15]. It is particularly concerning that inadequate sleep is linked with an increased risk of workplace injuries. For example, workers with excessive daytime sleepiness (as a result of chronic inadequate sleep) or those who often reported trouble sleeping had a 1.40–2.20 fold increased risk of sustaining an occupational injury [
16,
17]. Furthermore, on-call nurses involved in weekly or more frequent ‘call ins’ to work have been found to have an almost two-fold increase in back and shoulder musculoskeletal injuries [
18]. The relationship between working on-call, inadequate sleep, and injury risk is particularly concerning for on-call workers given the crucial roles (e.g., doctors, firefighters) these workers play in communities.
Inadequate sleep impacts up to 40% of Australians at an annual economic cost of
$66 billion, comprising
$26.2 billion in financial costs (e.g., health system, productivity, informal care), and
$40.1 billion in the loss of well-being [
19]. Furthermore, the costs of other irregular work hours exert acute effects on sleep and alertness which can lead to considerable human and economic costs due to fatigue-related accidents and reduced productivity [
20]. For example, road and workplace accidents, related to excessive sleepiness, are estimated to cost
$71–93 billion per annum in the United States [
21].
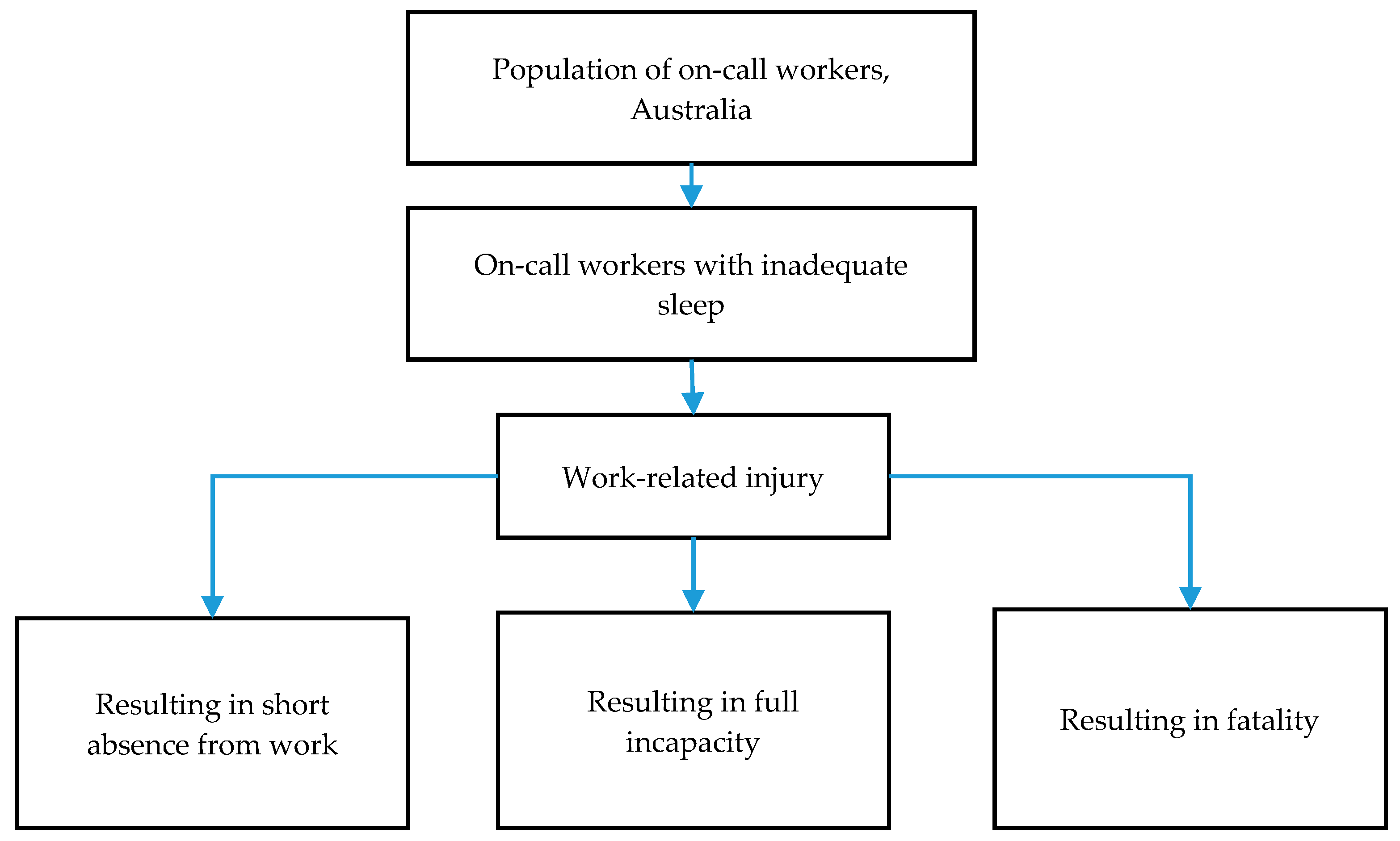
To the authors’ knowledge the economic cost of inadequate sleep in on-call work is yet to be investigated. On-call work is particularly common in industries where it is more cost-effective for an employer to have staff on-call at relevant times, rather than having employees rostered on when they are not needed. However, the economic benefits of implementing on-call arrangements should depend on worker health and safety risks being maintained at an acceptable level. As a first step into investigating the economic cost of on-call work, the objective of this study is to draw upon past research and validated costing methodology to quantify the economic cost of injury due to inadequate sleep of Australian on-call workers over one year.
4. Discussion
To the best of our knowledge this is the first study to quantify the economic cost of workplace injury due to inadequate sleep in on-call workers. Two-thirds of Australia’s on-call population (66%) reported obtaining inadequate sleep on weekdays (work days) and over 80% reported inadequate sleep while on-call. The resulting cost of injury is estimated at $2.25 billion per year ($1.71–2.73 billion). This equates to $1222 per person per incident involving a short-term absence from work, $2.53 million per incident classified as full incapacity, and $1.78 million for each fatality.
The annual cost of inadequate sleep due to workplace injury to on-call employees is $136.88 million ($103.70–165.91 million). Employers bear the largest share of the cost when injuries result in short absence from work (72%). This cost mainly relates to medical compensations as part of employer excess provisions (57%), and the value of lost production and staff turnover cost such as overtime and over-employment (42%). Meanwhile, the burden of cost associated with full incapacity and fatality is largely borne by the government: 98% and 96%, respectively. The annual cost of workplace injuries associated with inadequate sleep among on-call workers to the government and the economy as a whole is $2.11 billion ($1.60–2.56 billion). This includes costs in providing welfare benefits, falls in tax revenue, and costs to the health care system. Lost output alone costs the economy $1.88 billion ($1.42–2.28 billion). At a time when there is a national focus on productivity, the inescapable conclusion is that it is in the interest of both employers and the government to prioritize and invest far more in management of inadequate sleep.
The estimated cost of workplace injury reported in this study is comparable to the available national and international evidence from other populations. A recent report on inadequate sleep among the Australian general population estimated nearly 40% of Australian adults experience inadequate sleep leading to the financial loss of
$26.2 billion, or
$3548 per person/year [
19]. A US study found that inadequate sleep among healthcare, manufacturing, and transportation workers cost
$3174 per employee per year in fatigue-related productivity losses (converted to 2016 Australian dollars using AU/US PPP conversion factor of 1.50 and CPI of 1.14) [
33].
The current study provided an initial insight into the potential impact of inadequate sleep of on-call workers by examining the cost of injuries classified as a short absence from work, full incapacity, or fatality. However, there are other adverse impacts of inadequate sleep for this population which have not been considered in this costing analysis. The current study did not assess the cost of inadequate sleep on well-being. In the general Australian population, well-being loss imposes an extra cost of $5419 per person annually. In addition, the impact of inadequate sleep on other household members including spouses and children has also not been considered, nor were other potential impacts from a personal or societal viewpoint. Further research is needed to understand how being called can, for example, disturb an on-call worker’s spouse’s sleep, and the subsequent cost resulting from inadequate sleep.
Furthermore, 22% of on-call workers in the current study indicated that on-call work was not part of their primary employment (e.g., on-call role as volunteer firefighter). Therefore, the cost of injury for these individuals may be greater than estimated in the current study because an injury to these workers has the potential to impact not only their capacity in their voluntary (on-call) role but also their main place of employment, both with associated costs. Therefore, the overall cost of inadequate sleep to the individuals, their families, workplaces, government, and society in general is likely to be greater than estimated in the current study.
It is of great concern that 80% of the on-call population in this study reported obtaining inadequate sleep when on-call. Regulations in many countries, for example in Europe [
34], state that on-call periods when no calls are received are just as restful as time off, despite evidence demonstrating that this is often not the case [
7,
35]. For time off to be fully restorative and for workers to be well-rested, it is recommended that workers be provided with the opportunity to disengage from the work [
36]. To alleviate the burden of inadequate sleep, it is essential that employers recognize that on-call and time off are not equivalent when managing employees. This may involve developing work schedules which account for the demands of on-call work, particularly for instances where workers have not actually been called-in. For example, if a worker is on-call across a weekend but is not actually called, then it may be appropriate for them to have some extra time off. Furthermore, when an on-call worker obtains inadequate sleep, employers should perhaps consider additional control measures to minimize the potential fatigue-related risk.
Well-rested employees are critical to safe and productive operations, especially in on-call industries (e.g., healthcare, emergency services) where the risk of a fatigue-related error can have serious consequences to the workers themselves and the communities they serve. Our estimates of the cost of inadequate sleep in the Australian on-call workforce reinforce the importance of preventive measures to reduce fatigue-related errors. Organisations and workers are dually responsible for the management of inadequate sleep. For example, workplaces could provide sleep education to increase knowledge of how inadequate sleep can impact worker health and safety, and ways to obtain good sleep. While it is essential that workplaces provide fatigue-risk management strategies (including appropriate rosters that facilitate workers’ sleep and recovery), workers are also responsible for managing fatigue risk e.g., utilizing a sleep opportunity for sleep. Notably, across workplaces, there can be a culture of underreporting of injuries [
37,
38] and workers may not report sleeping poorly out of fear of a punitive response.
Determining whether sleep-related fatigue underlies or is a contributing factor to injury is often difficult, as a sleep-related fatigue injury is the endpoint of a fatigue-risk trajectory (or ‘error trajectory’) [
39]. For example, the fatigued state of a worker is preceded by insufficient recovery sleep or excessive wakefulness, which could be caused by various reasons, such as failure to obtain sufficient sleep for reasons beyond the workers control (e.g., the roster did not provide an adequate sleep opportunity) or the worker choosing to engage in non-sleep activities [
39]. Therefore, it is important to acknowledge that there are a multitude of factors [
40] that precede a fatigue-related injury. In addition, individuals lacking sleep are often unaware of their own level of associated performance impairment [
41] and therefore may not recognise lack of sleep as a contributing factor to injury.
This study has some limitations which should be acknowledged. Firstly, self-report measures were used to estimate the prevalence of inadequate sleep among on-call workers. Self-report data allowed for a large number of on-call workers to be surveyed from various industries at low cost [
42]. The literature comparing self-reported sleep duration with objective measures (actigraphy and/or polysomnography) is mixed. Some studies show that, when compared to objective measures, individuals can underestimate [
43,
44], or overestimate [
45] total sleep duration by as much as 30–40 min. In addition, the current study exclusively utilised sleep duration as a measure of inadequate sleep. Future studies need to assess a broad range of sleep variables (such as quality and timing) to determine to what extent these factors contribute to sleep-related injury risk and subsequent economic cost.
Given that the survey was advertised as research into the impact of on-call work on health and well-being it is possible that a disproportionate number of workers who felt that on-call work was impacting their health and well-being undertook the survey. In addition, participants were included in the study if any of their work included an on-call component, regardless of the amount of time workers were on-call. Therefore, the number and distribution (e.g., consecutive) of on-call shifts, as well as the likelihood of receiving a call (high vs. low), would likely impact upon sleep and subsequently upon the risk of injury; that is, a greater amount of on-call means a greater risk of injury. Further research is needed to determine the implications of on-call workload on injury risk. During on-call work periods, workers may not be called (i.e., not called into work). In these circumstances, there is no immediate risk of a workplace injury, because the worker is not at work. However, given that workers report inadequate sleep during on-call periods, even when no calls are received [
9], if adequate sleep following an on-call shift is not obtained, the next scheduled work shift could be impacted, regardless of whether this shift is classified as ‘on-call’. Lastly, the costing analysis relied on population averages (e.g., weekly earnings, age when injury occurred). These data may mask the potential variance in economic cost per full incapacity and fatality; for example, older workers having a lower economic cost than younger workers [
26].