Can Periodical Examinations of Employees Be Useful in Detection of Glycaemia Impairment and Improving Patients’ Adherence to Medical Recommendations?
Abstract
1. Introduction
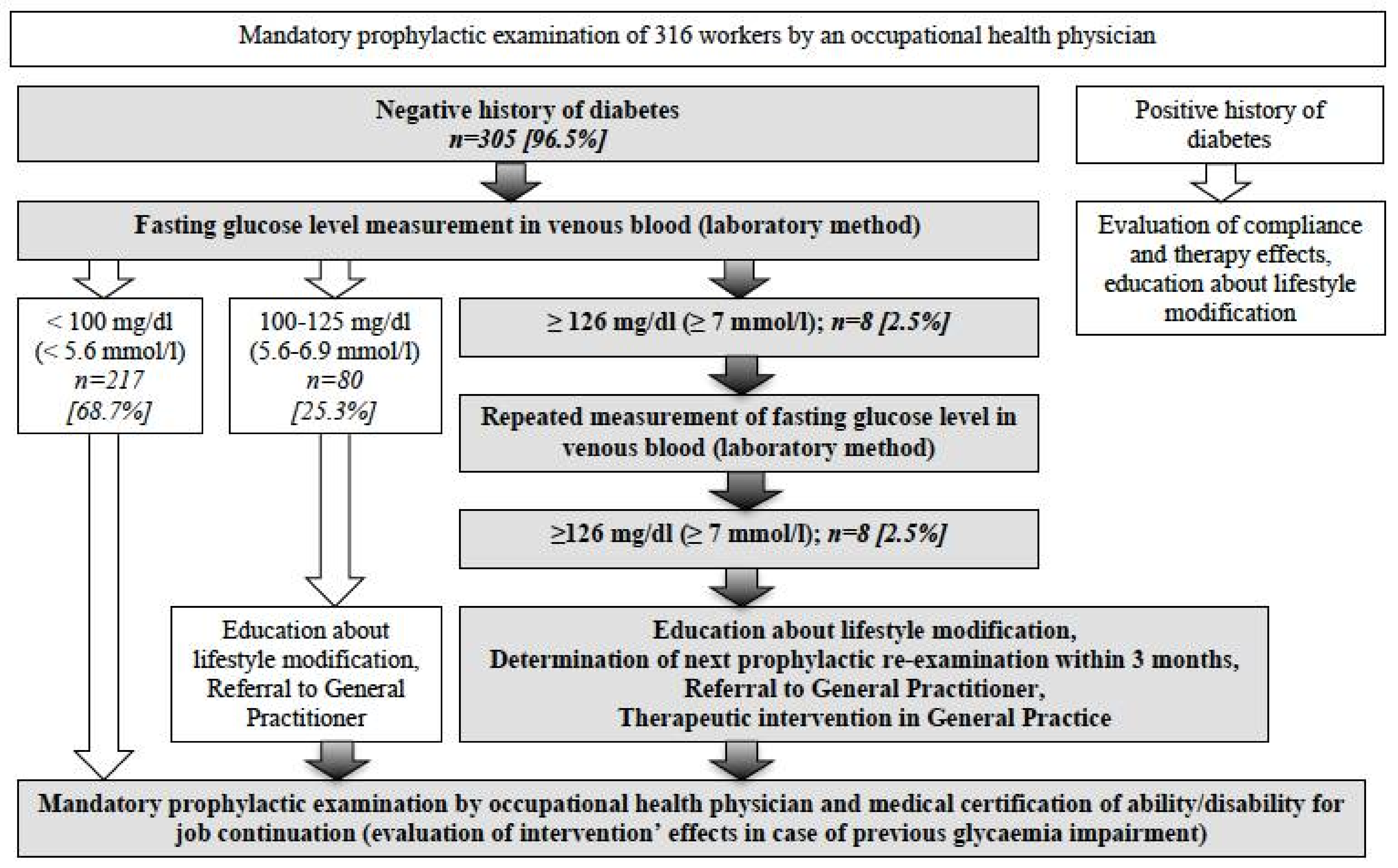
2. Materials and Methods
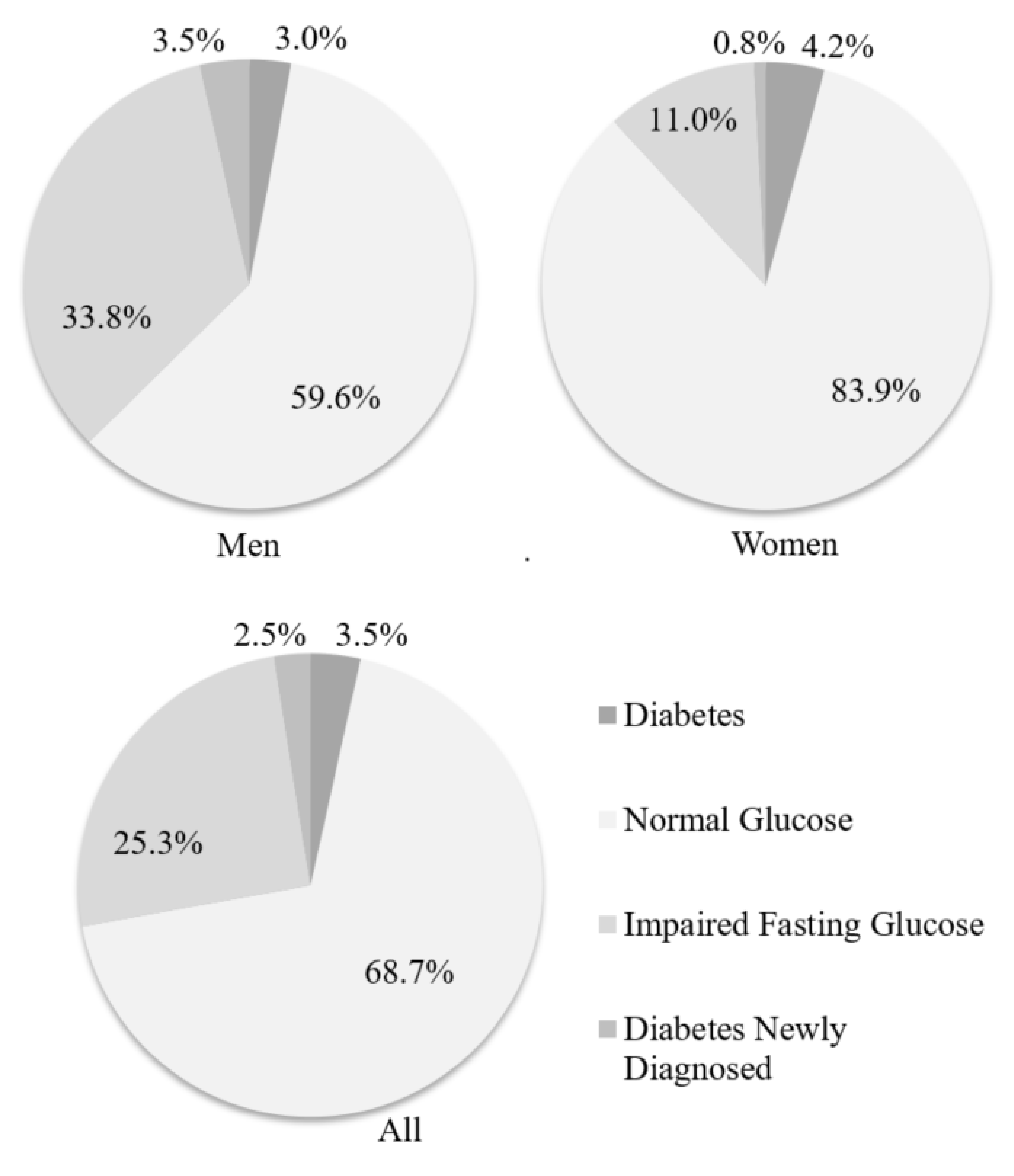
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas-Seventh Edition. 2015. Available online: http://www.diabetesatlas.org (accessed on 15 February 2017).
- Marcinkiewicz, A.; Wojda, M.; Walusiak-Skorupa, J.; Hanke, W.; Rydzyński, K. The analysis of tasks realized by occupational health services in Poland from 1997 to 2014. Do we exploit the full potential of prophylactic examinations of workers? Med. Pr. 2017, 68, 105–119. (In Polish) [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vrijens, B.; De Geest, S.; Hughes, D.A.; Kardas, P.; Demonceau, J.; Ruppar, T.; Dobbels, F.; Fargher, E.; Morrison, V.; Lewek, P.; et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 2012, 73, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Polish Diabetes Association. Guidelines on the management of diabetic patients. A position of Polish Diabetes Association. Clin. Diabetol. 2015, 4 (Suppl. A), A1–A73. (In Polish) [Google Scholar]
- Lindstrom, J.; Tuomilehto, J. The diabetes risk score: A practical tool to predict type 2 diabetes risk. Diabetes Care 2003, 26, 725–731. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing, version 3.3; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- Wittek, A.; Sokalski, B.; Grzeszczak, W.; Strojek, K. Prevalence of Diabetes and Cardiovascular Risk Factors of Industrial Area in Southern Poland. Exp. Clin. Endocrinol. Diabetes 2009, 117, 350–353. [Google Scholar] [CrossRef] [PubMed]
- Biela, U.; Pająk, A.; Kaczmarczyk-Chałas, K.; Głuszek, J.; Tendera, M.; Waśkiewicz, A.; Kurjata, P.; Wyrzykowski, B. Incidence of overweight and obesity in women and men between the ages of 20–74. Results of the WOBASZ program. Kardiol. Pol. 2005, 63 (Suppl. 4), 1–4. (In Polish) [Google Scholar]
- Krogsbøll, L.T.; Jørgensen, K.J.; Larsen, C.G.; Gøtzsche, P.C. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ 2012, 345, e7191. [Google Scholar] [CrossRef] [PubMed]
- Rodrigez-Jareno, M.C.; Molinero, E.; de Montserrat, J.; Valles, A.; Aymerich, M. How much do workers’ health examinations add to health and safety at the workplace? Occupational preventive usefulness of routine health examinations. Gac. Sanit. 2015, 29, 266–273. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sluiter, J.K. The new why when designing mandatory medical examinations. Occup. Med. 2017, 67, 325–327. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, L.E.; Alvarez, M.; Dilla, T.; Gil-Guillén, V.; Orozco-Beltrán, D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013, 4, 175–194. [Google Scholar] [CrossRef] [PubMed]
- Kobuszewska, L.; Sokołowska, B.; Kobus, G.; Urbańczuk, M. Level of knowledge of patients referred for coronary angiography on prevention of secondary coronary heart disease. Probl. Hig. Epidemiol. 2014, 95, 165–169. (In Polish) [Google Scholar]
- Viitasalo, K.; Lindström, J.; Hemiö, K.; Puttonen, S.; Koho, A.; Härmä, M.; Peltonen, M. Occupational health care identifies risk for type 2 diabetes and cardiovascular disease. Prim. Care Diabetes 2012, 6, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Tankova, T.; Chakarova, N.; Atanassova, I.; Dakovska, L. Evaluation of the Finnish Diabetes Risk Score as a screening tool for impaired fasting glucose, impaired glucose tolerance and undetected diabetes. Diabetes Res. Clin. Pract. 2011, 92, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Salinero-Fort, M.A.; Burgos-Lunar, C.; Lahoz, C.; Mostaza, J.M.; Abánades-Herranz, J.C.; Laguna-Cuesta, F.; Estirado-de Cabo, E.; García-Iglesias, F.; González-Alegre, T.; Fernández-Puntero, B.; et al. Performance of the Finnish Diabetes Risk Score and a Simplified Finnish Diabetes Risk Score in a Community-Based, Cross-Sectional Programme for Screening of Undiagnosed Type 2 Diabetes Mellitus and Dysglycaemia in Madrid, Spain: The SPREDIA-2 Study. PLoS ONE 2016, 11, 7, e0158489. [Google Scholar] [CrossRef] [PubMed]
- Vandersmissen, G.J.M.; Godderis, L. Evaluation of the Finnish Diabetes Risk Score (FINDRISC) for diabetes screening in occupational health care. Int. J. Occup. Med. Environ. Health 2015, 28, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Bergman, A.; Li, J.; Wang, L.; Schulze, J.; Bornstein, S.R.; Schwarz, P.E. A simplified Finnish diabetes risk score to predict type 2 diabetes risk and disease evolution in a German population. Horm. Metab. Res. 2007, 39, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Witte, D.R.; Shipley, M.J.; Marmot, M.G.; Brunner, E.J. Performance of existing risk scores in screening for undiagnosed diabetes: An external validation study. Diabet. Med. 2010, 27, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Kennedy-Martin, T.; Boye, K.S.; Peng, X. Cost of medication adherence and persistence in type 2 diabetes mellitus: A literature review. Patient Prefer. Adherence 2017, 11, 1103–1117. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.K.; Molenaar, D.M.; Arena, V.C.; Venditti, E.M.; Meehan, R.J.; Miller, R.G.; Vanderwood, K.K.; Eaglehouse, Y.; Kriska, A.M. Improving employee health: Evaluation of a worksite lifestyle change program to decrease risk factors for diabetes and cardiovascular disease. J. Occup. Environ. Med. 2015, 57, 284–291. [Google Scholar] [CrossRef]
- Elshatarat, R.A.; Burgel, B.J. Cardiovascular risk factors of taxi drivers. J. Urban Health 2016, 93, 589–606. [Google Scholar] [CrossRef] [PubMed]
| Risk Factor | Males n = 192 (%) | Females n = 113 (%) | Both n = 305 (%) |
|---|---|---|---|
| Age > 45 years | 68 (35) | 33 (29) | 101 (33) |
| BMI > 25kg/m2 | 137 (71) | 38 (34) | 175 (57) |
| Abdominal obesity: M > 94 cm of WC, F > 80 cm of WC | 116 (60) | 58 (51) | 174 (57) |
| Low daily physical activity * | 81 (42) | 57 (50) | 138 (45) |
| Improper diet ** | 82 (43) | 30 (26) | 112 (37) |
| History of arterial hypertension | 46 (24) | 14 (12) | 60 (20) |
| Family history of diabetes | 65 (34) | 51 (45) | 116 (38) |
| Positive history of glycaemia impairment | 31 (16) | 10 (9) | 41 (13) |
| Lack of glycaemia impairment control *** | 18 (9) | 4 (3) | 22 (7) |
| Lack of previous glycaemia testing | 64 (33) | 33 (29) | 97 (32) |
| Risk Factor | Males (n = 192) | Females (n = 113) | ||||
|---|---|---|---|---|---|---|
| FGL at Reference Range <100 mg/dL n = 118 (%) | FGL ≥ 100 mg/dL n = 74 (%) | OR (95% CI) | FGL at Reference Range <100 mg/dL n = 99 (%) | FGL ≥ 100 mg/dL n = 14 (%) | OR (95% CI) | |
| Age > 45 years | 24 (20.3) | 44 (59.5) | 5.74 (3.01–10.95) | 26 (26.3) | 7 (50) | 2.81 (0.9–8.77) |
| BMI ≥ 25 kg/m2 | 74 (62.7) | 63 (85.1) | 3.41 (1.62–7.15) | 28 (28.3) | 10 (71.4) | 6.34 (1.84–21.89) |
| Abdominal obesity * | 55 (46.6) | 61 (82.4) | 5.37 (2.67–10.82) | 46 (46.5) | 12 (85.2) | 6.91 (1.47–32.51) |
| Low daily physical activity ** | 41 (34.47) | 40 (54.1) | 2.26 (1.25–4.09) | 46 (46.5) | 11 (78.6) | 4.22 (1.11–16.07) |
| Improper diet *** | 52 (44.1) | 30 (40.5) | 0.87 (0.48–1.56) | 27 (27.3) | 3 (21.4) | 0.73 (0.19–2.81) |
| History of AH | 16 (13.6) | 30 (40.5) | 4.35 (2.15–8.77) | 10 (10.1) | 4 (28.6) | 3.56 (0.94–13.48) |
| Family history of DM | 40 (33.9) | 25 (33.8) | 0.99 (0.54–1.84) | 43 (43.4) | 8 (57.1) | 1.74 (0.56–5.38) |
| Positive history of glycaemia impairment | 8 (7) | 23 (31) | 6.20 (2.59–14.81) | 5 (5) | 5 (36) | 10.44 (2.53–43.02) |
| Lack of glycaemia impairment control *** | 4 (3) | 14 (19) | 6.65 (2.09–21.09) | 2 (2) | 2 (14) | 8.08 (1.04–62.76) |
| Lack of previous glycaemia testing | 45 (38) | 19 (26) | 0.56 (0.29–1.06) | 31 (31) | 2 (14) | 0.36 (0.07–1.73) |
| 10 Years Risk of DM Type 2 Development | All n = 305 (%) | Fasting Glucose Level in Venous Blood | ||
|---|---|---|---|---|
| 70–99 mg/dL (3.9–5.5 mmol/L) n = 217 (%) | 100–125 mg/dL (5.6–6.9 mmol/L) n = 80 (%) | ≥126 mg/dL (7.0 mmol/L) n = 8 (%) | ||
| Low (<1%) | 141 (46.2) | 123 (87.2) | 18 (12.8) | 0 |
| Slightly elevated (4%) | 80 (26.2) | 60 (75) | 19 (23.8) | 1 (1.3) |
| Moderate (16.6%) | 34 (11.1) | 16 (47.1) | 15 (44.1) | 3 (8.8) |
| High (33%) | 44 (14.4) | 16 (36.4) | 26 (59.1) | 2 (4.5) |
| Very high (50%) | 6 (2.0) | 2 (33.3) | 2 (33.3) | 2 (33.3) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcinkiewicz, A.; Hanke, W.; Kałużny, P.; Lipińska-Ojrzanowska, A.; Wiszniewska, M.; Walusiak-Skorupa, J. Can Periodical Examinations of Employees Be Useful in Detection of Glycaemia Impairment and Improving Patients’ Adherence to Medical Recommendations? Int. J. Environ. Res. Public Health 2018, 15, 638. https://doi.org/10.3390/ijerph15040638
Marcinkiewicz A, Hanke W, Kałużny P, Lipińska-Ojrzanowska A, Wiszniewska M, Walusiak-Skorupa J. Can Periodical Examinations of Employees Be Useful in Detection of Glycaemia Impairment and Improving Patients’ Adherence to Medical Recommendations? International Journal of Environmental Research and Public Health. 2018; 15(4):638. https://doi.org/10.3390/ijerph15040638
Chicago/Turabian StyleMarcinkiewicz, Andrzej, Wojciech Hanke, Paweł Kałużny, Agnieszka Lipińska-Ojrzanowska, Marta Wiszniewska, and Jolanta Walusiak-Skorupa. 2018. "Can Periodical Examinations of Employees Be Useful in Detection of Glycaemia Impairment and Improving Patients’ Adherence to Medical Recommendations?" International Journal of Environmental Research and Public Health 15, no. 4: 638. https://doi.org/10.3390/ijerph15040638
APA StyleMarcinkiewicz, A., Hanke, W., Kałużny, P., Lipińska-Ojrzanowska, A., Wiszniewska, M., & Walusiak-Skorupa, J. (2018). Can Periodical Examinations of Employees Be Useful in Detection of Glycaemia Impairment and Improving Patients’ Adherence to Medical Recommendations? International Journal of Environmental Research and Public Health, 15(4), 638. https://doi.org/10.3390/ijerph15040638





