Neck Circumference Positively Relates to Cardiovascular Risk Factors in College Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Test Sample
2.2. Anthropometry
2.3. Statistical Analysis
2.4. Ethical Statement
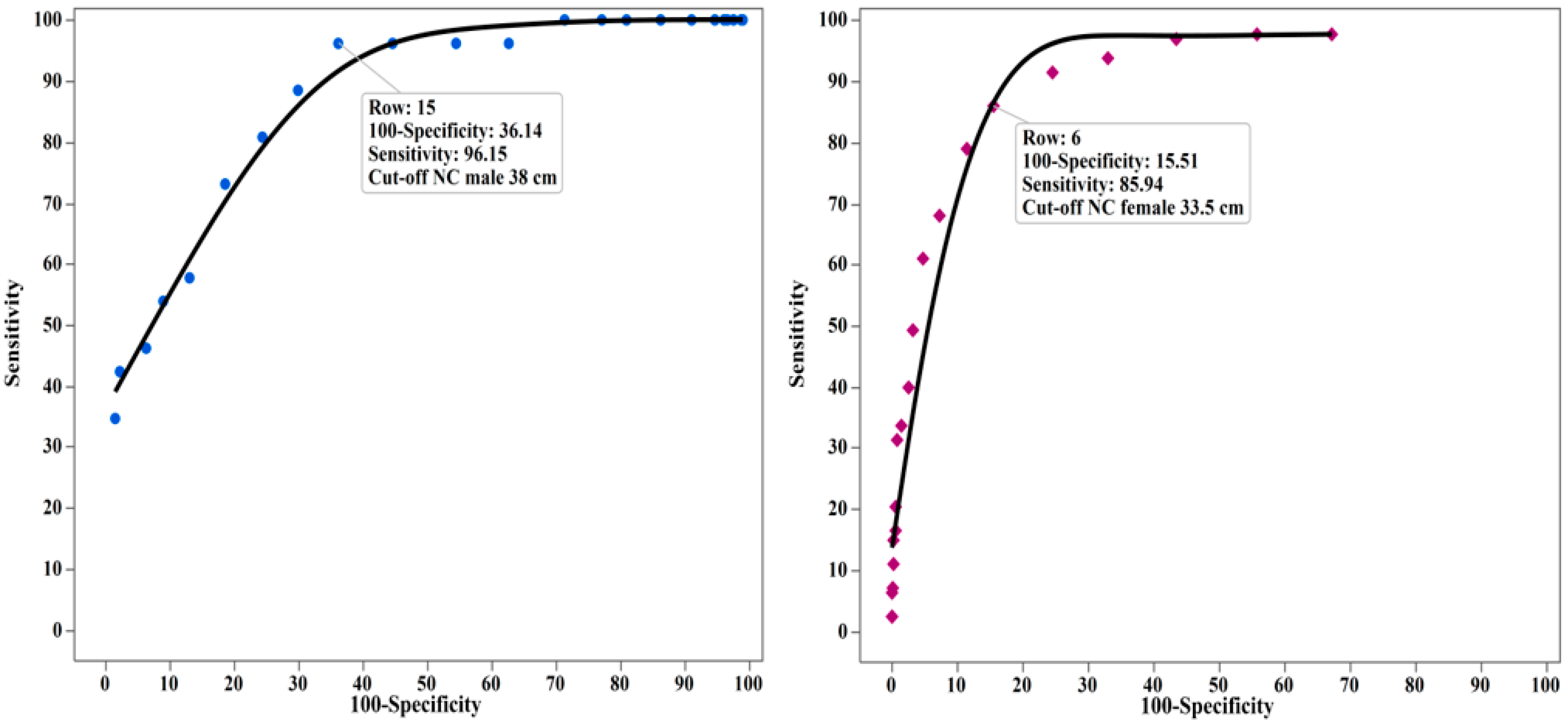
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Materials
Abbreviations
| NC | Neck circumference |
| BMI | Body mass index |
| WC | waist circumference |
| HC | hip circumference |
| SBP | systolic blood pressure |
| U.S. | United States |
| HDL | high-density lipoprotein |
| WHR | waist-to-hip ratio |
| ROC | receiving operating characteristic curve |
References
- Wang, Y.C.; McPherson, K.; Marsh, T.; Gortmaker, S.L.; Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011, 378, 815–825. [Google Scholar] [CrossRef]
- Hubert, H.B.; Feinleib, M.; Mcnamara, P.M.; Castelli, W.P. Obesity as an independent risk factor for cardiovascular-disease—A 26-year follow-up of participants in the Framingham Heart-Study. Circulation 1983, 67, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Spadano, J.; Coakley, E.H.; Field, A.E.; Colditz, G.; Dietz, W.H. The disease burden associated with overweight and obesity. JAMA 1999, 282, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Mendlein, J.; Resnicow, K.; Frank, E.; Cullen, K.W.; Baranowski, J. Physical activity and nutrition in children and youth: An overview of obesity prevention. Prev. Med. 2000, 31, S1–S10. [Google Scholar] [CrossRef]
- Strong, J.P.; Malcom, G.T.; McMahan, C.A.; Tracy, R.E.; Newman, W.P., III; Herderick, E.E.; Cornhill, J.F. Prevalence and extent of atherosclerosis in adolescents and young adults: Implications for prevention from the pathobiological determinants of atherosclerosis in youth study. JAMA 1999, 281, 727–735. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Rothman, K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008, 32, S56–S59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallagher, D.; Visser, M.; Sepulveda, D.; Pierson, R.N.; Harris, T.; Heymsfield, S.B. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am. J. Epidemiol. 1996, 143, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Gastaldelli, A. Abdominal fat: Does it predict the development of type 2 diabetes? Am. J. Clin. Nutr. 2008, 87, 1118–1119. [Google Scholar] [CrossRef] [PubMed]
- Després, J.-P. Abdominal obesity: The most prevalent cause of the metabolic syndrome and related cardiometabolic risk. Eur. Heart J. Suppl. 2006, 8, B4–B12. [Google Scholar] [CrossRef]
- Vague, J. The degree of masculine differentiation of obesities a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am. J. Clin. Nutr. 1956, 4, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Kissebah, A.H.; Vydelingum, N.; Murray, R.; Evans, D.J.; Kalkhoff, R.K.; Adams, P.W. Relation of body fat distribution to metabolic complications of obesity. J. Clin. Endocrinol. Metab. 1982, 54, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Vallianou, N.G.; Evangelopoulos, A.A.; Bountziouka, V.; Vogiatzakis, E.D.; Bonou, M.S.; Barbetseas, J.; Avgerinos, P.C.; Panagiotakos, D.B. Neck circumference is correlated with triglycerides and inversely related with HDL cholesterol beyond BMI and waist circumference. Diabetes/Metab. Res. Rev. 2013, 29, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Cizza, G.; de Jonge, L.; Piaggi, P.; Mattingly, M.; Zhao, X.; Lucassen, E.; Rother, K.I.; Sumner, A.E.; Csako, G. Neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab. Syndr. Relat. Disord. 2014, 12, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Stabe, C.; Vasques, A.C.J.; Lima, M.M.O.; Tambascia, M.A.; Pareja, J.C.; Yamanaka, A.; Geloneze, B. Neck circumference as a simple tool for identifying the metabolic syndrome and insulin resistance: Results from the brazilian metabolic syndrome study. Clin. Endocrinol. 2013, 78, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Hingorjo, M.R.; Qureshi, M.A.; Mehdi, A. Neck circumference as a useful marker of obesity: A comparison with body mass index and waist circumference. JPMA 2012, 62, 36–40. [Google Scholar]
- Yang, G.R.; Yuan, S.Y.; Fu, H.J.; Wan, G.; Zhu, L.X.; Bu, X.L.; Zhang, J.D.; Du, X.P.; Li, Y.L.; Ji, Y.; et al. Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing community diabetes study 4. Diabetes Care 2010, 33, 2465–2467. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Van Leer, E.; Seidell, J.; Lean, M. Waist circumference action levels in the identification of cardiovascular risk factors: Prevalence study in a random sample. BMJ 1995, 311, 1401–1405. [Google Scholar] [CrossRef] [PubMed]
- Ben-Noun, L.L.; Laor, A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp. Clin. Cardiol. 2006, 11, 14–20. [Google Scholar] [PubMed]
- Lean, M.; Han, T.; Morrison, C. Waist circumference as a measure for indicating need for weight management. Bmj 1995, 311, 158–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashwell, M. Obesity in men and women. Int. J. Obes. Relat. Metab. Disord. 1994, 18, S1–S7. [Google Scholar] [PubMed]
- Pouliot, M.-C.; Després, J.-P.; Lemieux, S.; Moorjani, S.; Bouchard, C.; Tremblay, A.; Nadeau, A.; Lupien, P.J. Waist circumference and abdominal sagittal diameter: Best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am. J. Cardiol. 1994, 73, 460–468. [Google Scholar] [CrossRef]
- Janssen, I.; Heymsfield, S.B.; Allison, D.B.; Kotler, D.P.; Ross, R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am. J. Clin. Nutr. 2002, 75, 683–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunkley, A.J.; Stone, M.A.; Patel, N.; Davies, M.J.; Khunti, K. Waist circumference measurement: Knowledge, attitudes and barriers in patients and practitioners in a multi-ethnic population. Fam. Pract. 2009, 26, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Onat, A.; Hergenç, G.; Yüksel, H.; Can, G.; Ayhan, E.; Kaya, Z.; Dursunoğlu, D. Neck circumference as a measure of central obesity: Associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin. Nutr. 2009, 28, 46–51. [Google Scholar] [CrossRef] [PubMed]
| Variables | Males | Females |
|---|---|---|
| Age (years) | 19.6 ± 1.4 (18–27) | 19.8 ± 1.4 (18–28) |
| Weight (kg) | 76.2 ± 15.7 (42.5–153.6) | 65.7 ± 15.3 (39.3–146.2) |
| Height (cm) | 175.3 ± 7.7 (146.5–197.5) | 164.6 ± 7.1 (141.2–191.2) |
| BMI (kg/m2) | 24.7 ± 4.3 (14.7–41.8) | 24.2 ± 4.9 (16.3–49.7) |
| Waist Circumference (cm) | 83.3 ± 11.1 (61.5–139.5) | 76.8 ± 11.2 (56.0–156.3) |
| Hip Circumference (cm) | 101.1 ± 9.7 (69.4–144.0) | 99.8 ± 10.4 (63.4–149.0) |
| Neck Circumference (cm) | 37.4 ± 2.7 (29.4–48.5) | 32.3 ± 2.4 (26.8–50.0) |
| Systolic Blood Pressure (mm/Hg) | 118 ± 13 (74–162) | 106 ± 11 (69–166) |
| Diastolic Blood Pressure (mm/Hg) | 68 ± 9 (46–96) | 68 ± 9 (43–107) |
| Variables | Males | Females | ||
|---|---|---|---|---|
| ρ | p-Value | ρ | p-Value | |
| Age (years) | 0.04 | 0.45 | −0.06 | 0.07 * |
| Weight (kg) | 0.69 | <0.0001 ** | 0.71 | <0.0001 ** |
| Height (cm) | 0.26 | <0.0001 ** | 0.28 | <0.0001 ** |
| BMI (kg/m2) | 0.70 | <0.0001 ** | 0.69 | <0.0001 ** |
| Waist Circumference (cm) | 0.69 | <0.0001 ** | 0.72 | <0.0001 ** |
| Hip Circumference (cm) | 0.64 | <0.0001 ** | 0.69 | <0.0001 ** |
| Waist-to-Hip Ratio | 0.46 | <0.0001 ** | 0.41 | <0.0001 ** |
| Systolic Blood Pressure (mm/Hg) | 0.25 | <0.0001 ** | 0.31 | <0.0001 ** |
| Diastolic Blood Pressure (mm/Hg) | 0.04 | 0.42 | 0.22 | <0.0001 ** |
| Males | Females | |||
|---|---|---|---|---|
| Cut-Off (cm) | Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) |
| 31 | 100 | 1.0 | 97.7 | 32.8 |
| 31.5 | 100 | 1.2 | 97.7 | 44.2 |
| 32 | 100 | 2.4 | 96.9 | 56.6 |
| 32.5 | 100 | 3.4 | 93.8 | 67.0 |
| 33 | 100 | 3.9 | 91.4 | 75.5 |
| 33.5 | 100 | 5.3 | 85.9 | 84.5 |
| 34 | 100 | 8.9 | 78.9 | 88.6 |
| 34.5 | 100 | 13.7 | 68.0 | 92.7 |
| 35 | 100 | 19.0 | 60.9 | 95.3 |
| 35.5 | 100 | 22.9 | 49.2 | 96.8 |
| 36 | 100 | 28.7 | 39.8 | 97.5 |
| 36.5 | 96.2 | 37.4 | 33.6 | 98.6 |
| 37 | 96.2 | 45.5 | 31.3 | 99.2 |
| 37.5 | 96.2 | 55.4 | 20.3 | 99.5 |
| 38 | 96.2 | 63.9 | 16.4 | 99.5 |
| 38.5 | 88.5 | 70.1 | 14.8 | 99.8 |
| 39 | 80.8 | 75.7 | 10.9 | 99.8 |
| 39.5 | 73.1 | 81.5 | 7.0 | 99.8 |
| 40 | 57.7 | 87.0 | 6.3 | 100 |
| 40.5 | 53.9 | 91.1 | 2.3 | 100 |
| 41 | 46.2 | 93.7 | 2.3 | 100 |
| 41.5 | 42.3 | 97.8 | 2.3 | 100 |
| 42 | 34.6 | 98.6 | 2.3 | 100 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Famodu, O.A.; Barr, M.L.; Colby, S.E.; Zhou, W.; Holásková, I.; Leary, M.P.; Byrd-Bredbenner, C.; Mathews, A.E.; Olfert, M.D. Neck Circumference Positively Relates to Cardiovascular Risk Factors in College Students. Int. J. Environ. Res. Public Health 2018, 15, 1480. https://doi.org/10.3390/ijerph15071480
Famodu OA, Barr ML, Colby SE, Zhou W, Holásková I, Leary MP, Byrd-Bredbenner C, Mathews AE, Olfert MD. Neck Circumference Positively Relates to Cardiovascular Risk Factors in College Students. International Journal of Environmental Research and Public Health. 2018; 15(7):1480. https://doi.org/10.3390/ijerph15071480
Chicago/Turabian StyleFamodu, Oluremi A., Makenzie L. Barr, Sarah E. Colby, Wenjun Zhou, Ida Holásková, Miriam P. Leary, Carol Byrd-Bredbenner, Anne E. Mathews, and Melissa D. Olfert. 2018. "Neck Circumference Positively Relates to Cardiovascular Risk Factors in College Students" International Journal of Environmental Research and Public Health 15, no. 7: 1480. https://doi.org/10.3390/ijerph15071480





