Comparative Study between a Novel In Vivo Method and CBCT for Assessment of Ridge Alterations after Socket Preservation—Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Study Protocol
2.3. Surgical Technique
2.4. Postoperative Care
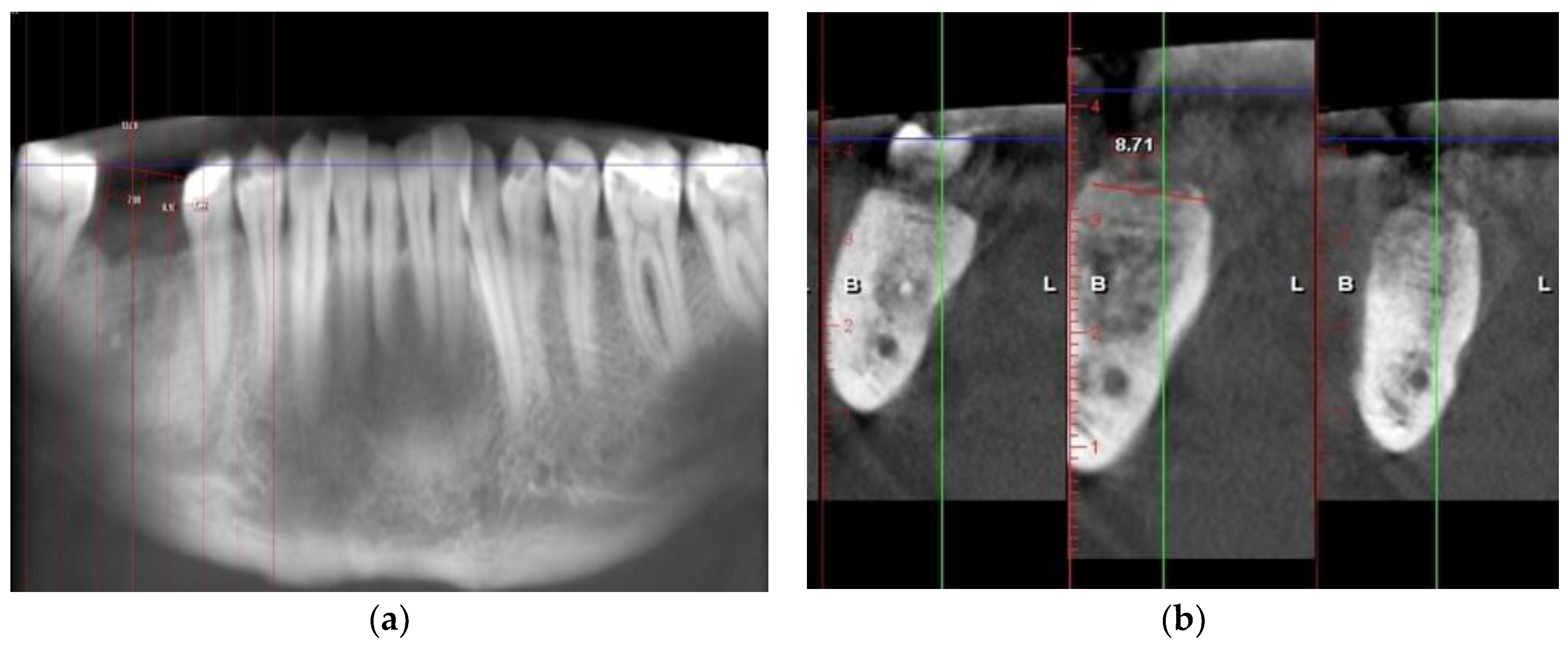
2.5. Radiographic Examination on CBCTs
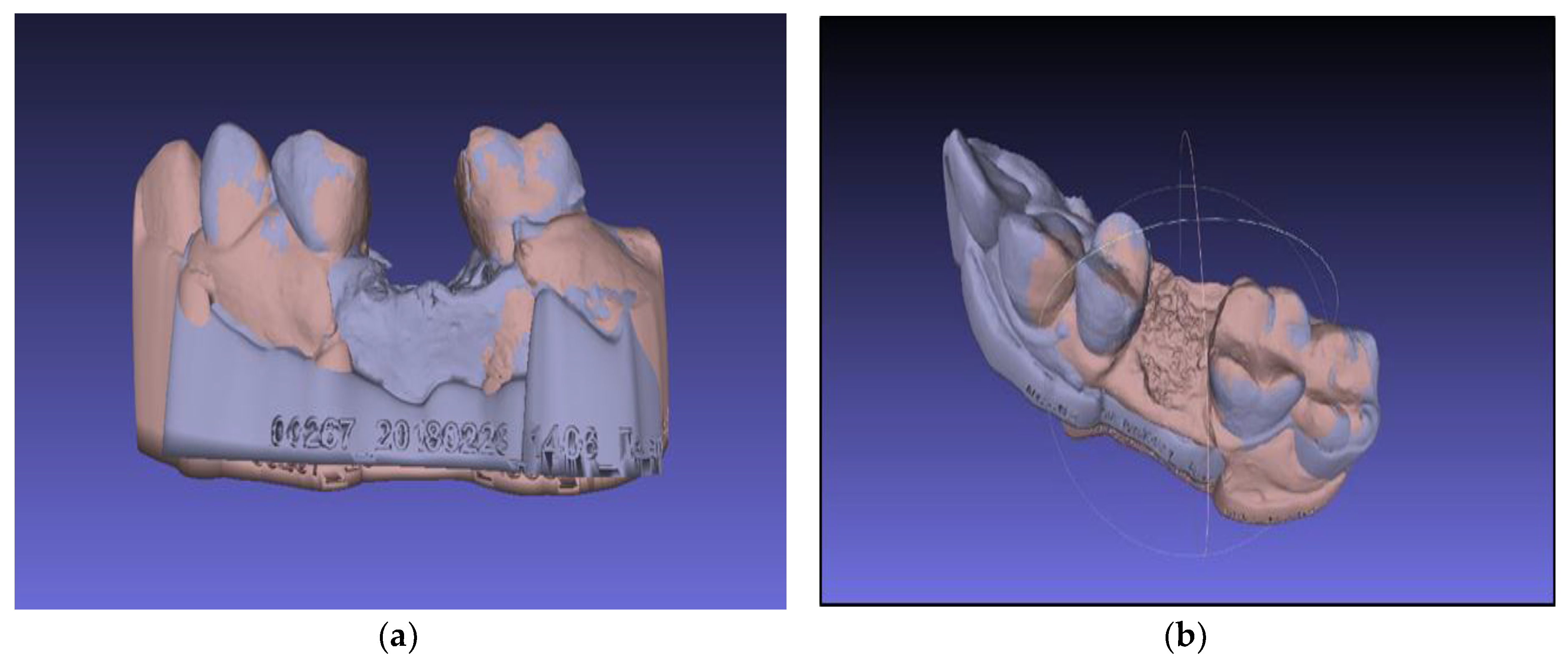
2.6. Three-Dimensional Virtual Models Evaluation
- Selection of the base model—choose a model that is tightly oriented at the base of the work area defined by the axes “x” and “y”
- Fix the selected model using the “Glue mesh here” command
- Equation of points with the point-based gluing function
- Selection of the “processing” function, by which the models are finely tuned by the “ICP—iterative closest point” method
3. Results
3.1. Radiographic Analysis
3.2. Virtual Models Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Zhao, J.H.; Tsai, C.H.; Chang, Y.C. Clinical and histologic evaluations of healing in an extraction socket filled with platelet-rich fibrin. J. Dent. Sci. 2011, 6, 116–122. [Google Scholar] [CrossRef]
- Iasella, J.M.; Greenwell, H.; Miller, R.L.; Hill, M.; Dsisko, C.; Bohra, A.A.; Scheetz, J.P. Ridge Preservation with Freeze-Dried Bone Allograft and a Collagen Membrane Compared to Extraction Alone for Implant Site Development: A Clinical and Histologic Study in Humans. J. Periodontol. 2003, 74, 990–999. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Chaturvedi, R.; Pahuja, B. Comparative Evaluation of the Efficacy of Calcium Sulfate Bone Grafts in Crystalline and Nano-Crystalline Forms in Fresh Extraction Socket Sites: A Radiographic and Histological Pilot Study. Int. J. Oral Implantol. Clin. Res. 2012, 3, 58–61. [Google Scholar] [CrossRef]
- Anwandter, A.; Bohmann, S.; Nally, M.; Castro, A.B.; Quirynen, M.; Pinto, N. Dimensional changes of the post extraction alveolar ridge, preserved with Leukocyte- and Platelet Rich Fibrin: A Clinical Pilot Study. J. Dent. 2016, 52, 23–29. [Google Scholar] [CrossRef]
- Lekovic, V.; Camargo, P.M.; Klokkevold, P.R.; Weinlaender, M.; Kenney, E.B.; Dimitrijevic, B.; Nedic, M. Preservation of Alveolar Bone in Extraction Sockets Using Bioabsorbable. J. Periodontol. 1998, 69, 1044–1049. [Google Scholar] [CrossRef]
- Baniasadi, B.; Evrard, L. Alveolar Ridge Preservation After Tooth Extraction with DFDBA and Platelet Concentrates: A Radiographic Retrospective Study. Open Dent. J. 2017, 11, 99–108. [Google Scholar] [CrossRef]
- Zlatev, S.; Ivanova, V.; Chenchev, I. A Method for Volumetric Evaluation of Post-Extraction Site’s Alveolar Bone Change in Human Subjects. IOSR J. Dent. Med. Sci. 2017, 16, 76–78. [Google Scholar]
- Mangano, F.; Shibli, J.A.; Fortin, T. Digital Dentistry: New Materials and Techniques. Int. J. Dent. 2016, 2016, 2–4. [Google Scholar] [CrossRef]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Renne, W.; Ludlow, M.; Fryml, J.; Schurch, Z.; Mennito, A.; Kessler, R.; Lauer, A. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J. Prosthet. Dent. 2017, 118, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of four intraoral scanners in oral implantology: A comparative in vitro study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Veronesi, G.; Hauschild, U.; Mijiritsky, E.; Mangano, C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. PLoS ONE 2016, 11, e0163107. [Google Scholar] [CrossRef] [PubMed]
- Benn, D.K. A review of the reliability of radiographic measurements in estimating alveolar bone changes. J. Clin. Periodontol. 1990, 17, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Larsen, C.; Barendregt, D.S.; Slot, D.E.; Van der Velden, U.; Van der Weijden, F. Probing pressure, a highly undervalued unit of measure in periodontal probing: A systematic review on its effect on probing pocket depth. J. Clin. Periodontol. 2009, 36, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Preus, H.R.; Torgersen, G.R.; Koldsland, O.C.; Hansen, B.F.; Aass, A.M.; Larheim, T.A.; Sandvik, L. A new digital tool for radiographic bone level measurements in longitudinal studies. BMC Oral Health 2015, 15, 2–7. [Google Scholar] [CrossRef]
- Bagoff, R.S.; Mamidwar, I.; Chesnoiu-Matei, J.L.; Alexander, R.H.; Tovar, N.M. Socket Preservation and Sinus Augmentation Using a Medical Grade Calcium Sulfate Hemihydrate and Mineralized Irradiated Cancellous Bone Allograft Composite. J. Oral Implantol. 2013, 39, 363–371. [Google Scholar] [CrossRef]
- Ten Heggeler, J.M.; Slot, D.E.; Van der Weijden, G.A. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: A systematic review. Clin. Oral Implants Res. 2011, 22, 779–788. [Google Scholar] [CrossRef]
- Walker, C.J.; Prihoda, T.J.; Mealey, B.L.; Lasho, D.J.; Huynh-ba, G.; Antonio, S. Evaluation of Healing at Molar Extraction Sites With and Without Ridge Preservation: A Randomized Controlled Clinical Trial. J. Periodontol. 2017, 88, 241–249. [Google Scholar] [CrossRef]
- Horowitz, R.; Holtzclaw, D.; Rosen, P.S. A review on alveolar ridge preservation following tooth extraction. J. Evid. Based Dent. Pract. 2012, 12 (Suppl. S3), 149–160. [Google Scholar] [CrossRef]
- Van der Weijden, F.; Dell’Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Chappuis, V.; Engel, O.; Reyes, M.; Shahim, K.; Nolte, L.P.; Buser, D. Ridge alterations post-extraction in the esthetic zone: A 3D analysis with CBCT. J. Dent. Res. 2013, 92 (Suppl. S12), 195S–201S. [Google Scholar] [CrossRef] [PubMed]
- Gultekin, B.A.; Bedeloglu, E.; Kose, T.E.; Mijiritsky, E. Comparison of Bone Resorption Rates after Intraoral Block Bone and Guided Bone Regeneration Augmentation for the Reconstruction of Horizontally Deficient Maxillary Alveolar Ridges. Biomed. Res. Int. 2016, 2016, 4987437. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 1–16. [Google Scholar] [CrossRef]
- Yuzbasioglu, E.; Kurt, H.; Turunc, R.; Bilir, H. Comparison of digital and conventional impression techniques: Evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Hack, G.D.; Sebastian, B.M. Evaluation of the Accuracy of Six Intraoral Scanning. Am. Dent. Assoc. 2015, 10, 1–5. [Google Scholar]
- Chappuis, V.; Engel, O.; Shahim, K.; Reyes, M.; Katsaros, C.; Buser, D. Soft Tissue Alterations in Esthetic Postextraction Sites: A 3-Dimensional Analysis. J. Dent. Res. 2015, 94 (Suppl. S9), 187S–193S. [Google Scholar] [CrossRef]
- Mangano, F.G.; Luongo, F.; Picciocchi, G.; Mortellaro, C.; Park, K.B.; Mangano, C. Soft Tissue Stability around Single Implants Inserted to Replace Maxillary Lateral Incisors: A 3D Evaluation. Int. J. Dent. 2016, 4, 1–9. [Google Scholar] [CrossRef]





| Method | CBCT | Virtual Model (.stl) | ||
|---|---|---|---|---|
| Direction | Horizontal (mm) | Vertical (mm) | Horizontal (mm) | Vertical (mm) |
| Case Number | ||||
| 1 | 0.8 | 1.4 | 3.64 | 2.10 |
| 2 | 0.6 | 1.6 | 2.63 | 1.15 |
| 3 | 1.1 | 1.1 | 2.28 | 1.84 |
| 4 | 0.1 | 1.16 | 2.43 | 0.805 |
| 5 | 0.8 | 2.7 | 2.68 | 1.84 |
| 6 | 0.8 | 0.46 | 2.49 | 1.14 |
| 7 | 1.2 | 0.5 | 1.92 | 0.95 |
| 8 | 2.4 | 2.8 | 3.64 | 1.68 |
| 9 | 0.3 | 1.7 | 2.63 | 0.657 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanova, V.; Chenchev, I.; Zlatev, S.; Iordanov, G.; Mijiritsky, E. Comparative Study between a Novel In Vivo Method and CBCT for Assessment of Ridge Alterations after Socket Preservation—Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 127. https://doi.org/10.3390/ijerph16010127
Ivanova V, Chenchev I, Zlatev S, Iordanov G, Mijiritsky E. Comparative Study between a Novel In Vivo Method and CBCT for Assessment of Ridge Alterations after Socket Preservation—Pilot Study. International Journal of Environmental Research and Public Health. 2019; 16(1):127. https://doi.org/10.3390/ijerph16010127
Chicago/Turabian StyleIvanova, Vasilena, Ivan Chenchev, Stefan Zlatev, Georgi Iordanov, and Eitan Mijiritsky. 2019. "Comparative Study between a Novel In Vivo Method and CBCT for Assessment of Ridge Alterations after Socket Preservation—Pilot Study" International Journal of Environmental Research and Public Health 16, no. 1: 127. https://doi.org/10.3390/ijerph16010127
APA StyleIvanova, V., Chenchev, I., Zlatev, S., Iordanov, G., & Mijiritsky, E. (2019). Comparative Study between a Novel In Vivo Method and CBCT for Assessment of Ridge Alterations after Socket Preservation—Pilot Study. International Journal of Environmental Research and Public Health, 16(1), 127. https://doi.org/10.3390/ijerph16010127






