Differences in Autonomy and Health-Related Quality of Life between Resilient and Non-Resilient Individuals with Mild Cognitive Impairment
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.2.1. Brief Resilient Coping Scale (BRCS)
2.2.2. The Short Form-12 Health Survey (SF-12)
2.2.3. Barthel Index
2.2.4. The Lawton Instrumental Activities of Daily Living
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Relationships between Resilience, ADLs, IADLs and HRQOL
3.2. Scores in ADLs and IADLs in Each Group
3.3. Scores in HRQOL in Each Group
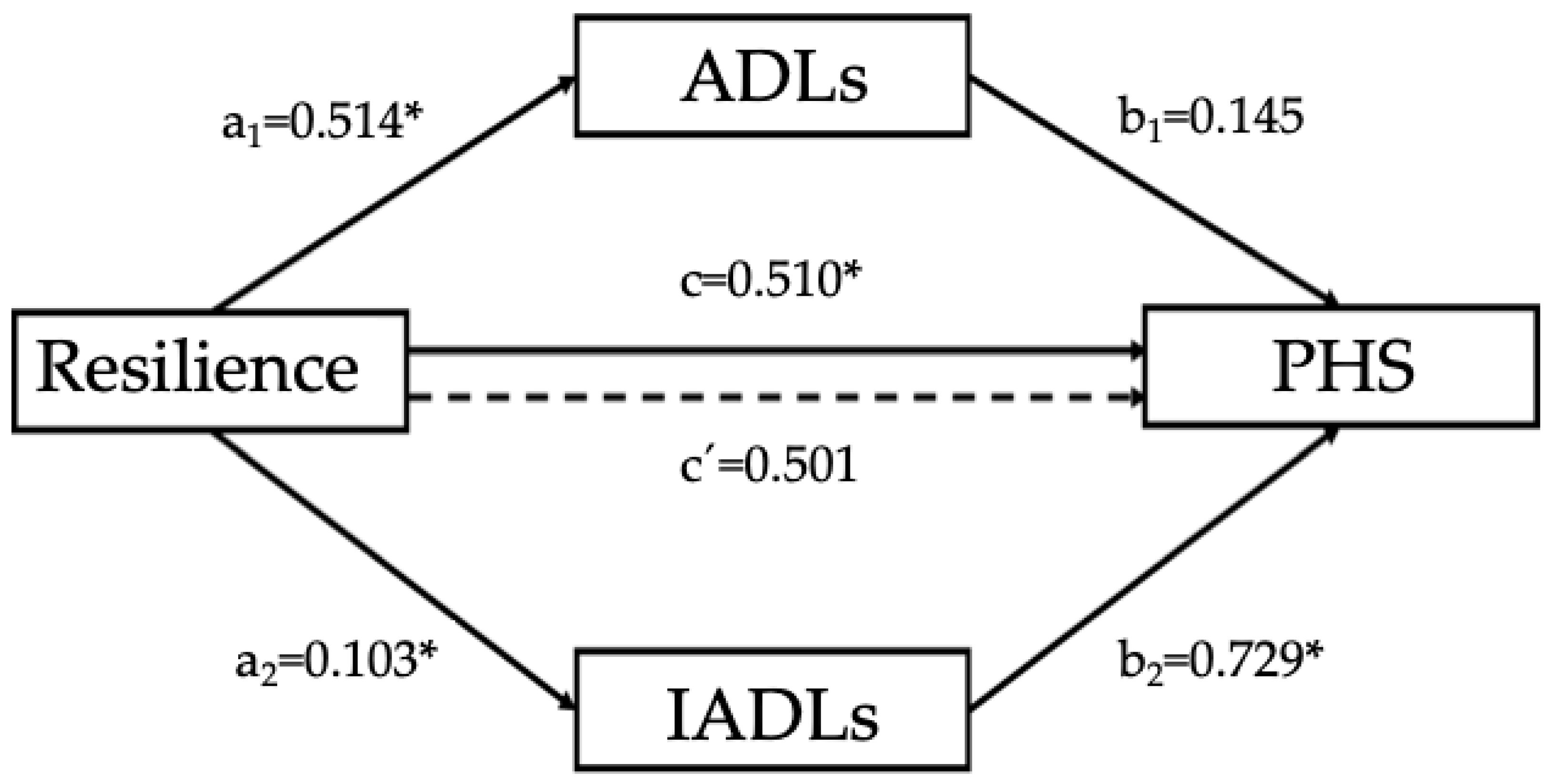
3.4. Mediation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Petersen, R.C. Mild cognitive impairment. Contin. Lifelong Learn. Neurol. 2016, 22, 404–418. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Caracciolo, B.; Brayne, C.; Gauthier, S.; Jelic, V.; Fratiglioni, L. Mild cognitive impairment: A concept in evolution. J. Intern. Med. 2014, 275, 214–228. [Google Scholar] [CrossRef] [PubMed]
- Oltra-Cucarella, J.; Ferrer-Cascales, R.; Alegret, M.; Gasparini, R.; Díaz-Ortiz, L.M.; Ríos, R.; Martínez-Nogueras, A.; Luis, I.; Pérez-Vicente, J.A.; Cabello-Rodríguez, L.; et al. Risk of progression to Alzheimer’s disease for different neuropsychological Mild Cognitive Impairment subtypes: A hierarchical meta-analysis of longitudinal studies. Psychol. Aging 2018, 33, 1007–1021. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Smith, G.E.; Waring, S.C.; Ivnik, R.J.; Tangalos, E.G.; Kokmen, E. Mild Cognitive Impairment: Clinical Characterization and Outcome. Arch. Neurol. 1999, 56, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Roberts, R.O.; Knopman, D.S.; Geda, Y.E.; Cha, R.H.; Pankratz, V.S.; Boeve, B.F.; Tangalos, E.G.; Ivnik, R.J.; Rocca, W.A. Prevalence of mild cognitive impairment is higher in men. Neurology 2010, 75, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Plassman, B.L. Prevalence of Cognitive Impairment without Dementia in the United States. Ann. Intern. Med. 2008, 148, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.M.; Cohen, A.; Ein-Mor, E.; Maaravi, Y.; Stessman, J. Frailty, cognitive impairment and mortality among the oldest old. J. Nutr. Health Aging 2011, 15, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Purser, J.L.; Fillenbaum, G.G.; Pieper, C.F.; Wallace, R.B. Mild Cognitive Impairment and 10-Year Trajectories of Disability in the Iowa Established Populations for Epidemiologic Studies of the Elderly Cohort. J. Am. Geriatr. Soc. 2005, 53, 1966–1972. [Google Scholar] [CrossRef]
- Royall, D.R.; Chiodo, L.K.; Polk, M.J. Correlates of Disability among Elderly Retirees with “Subclinical” Cognitive Impairment. J. Gerontol. Ser. A 2000, 55, M541–M546. [Google Scholar] [CrossRef]
- Artero, S.; Touchon, J.; Ritchie, K. Disability and mild cognitive impairment: A longitudinal population-based study. Int. J. Geriatr. Psychiatry 2001, 16, 1092–1097. [Google Scholar] [CrossRef]
- Nygård, L. Instrumental activities of daily living: A stepping-stone towards Alzheimer’s disease diagnosis in subjects with mild cognitive impairment? Acta Neurol. Scand. 2003, 107, 42–46. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Perneczky, R.; Pohl, C.; Sorg, C.; Hartmann, J.; Komossa, K.; Alexopoulos, P.; Wagenpfeil, S.; Kurz, A. Complex activities of daily living in mild cognitive impairment: Conceptual and diagnostic issues. Age Ageing 2006, 35, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Marshall, G.A.; Rentz, D.M.; Frey, M.T.; Locascio, J.J.; Johnson, K.A.; Sperling, R.A. Executive function and instrumental activities of daily living in mild cognitive impairment and Alzheimer’s disease. Alzheimers Dement. 2011, 7, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.K.; Wittrup-Jensen, K.U.; Lolk, A.; Andersen, K.; Kragh-Sørensen, P. Ability to perform activities of daily living is the main factor affecting quality of life in patients with dementia. Health Qual. Life Outcomes 2004, 2, 52. [Google Scholar] [CrossRef] [PubMed]
- Hill, N.L.; McDermott, C.; Mogle, J.; Munoz, E.; DePasquale, N.; Wion, R.; Whitaker, E. Subjective cognitive impairment and quality of life: A systematic review. Int. Psychogeriatr. 2017, 29, 1965–1977. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.P.; Weinborn, M.; Li, Y.R.; Hodgson, E.; Ng, A.R.J.; Bucks, R.S. Does prospective memory influence quality of life in community-dwelling older adults? Aging Neuropsychol. Cogn. 2015, 22, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Rickenbach, E.H.; Condeelis, K.L.; Haley, W.E. Daily stressors and emotional reactivity in individuals with mild cognitive impairment and cognitively healthy controls. Psychol. Aging 2015, 30, 420–431. [Google Scholar] [CrossRef]
- Kim, S.W.; Shin, I.S. Patients’ versus caregivers’ reports of quality of life in Alzheimer’s disease. J. Korean Soc. Biol. Ther. Psychiatry 2006, 12, 224–230. [Google Scholar]
- Tomaszewski Farias, S.; Schmitter-Edgecombe, M.; Weakley, A.; Harvey, D.; Denny, K.G.; Barba, C.; Gravano, J.T.; Giovannetti, T.; Willis, S. Compensation Strategies in Older Adults: Association With Cognition and Everyday Function. Am. J. Alzheimers Dis. Dementias 2018, 33, 184–191. [Google Scholar] [CrossRef]
- Levy, B.R.; Slade, M.D.; Kunkel, S.R.; Kasl, S.V. Longevity increased by positive self-perceptions of aging. J. Pers. Soc. Psychol. 2002, 83, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, U.M.; Fleeson, W. Self and personality in old and very old age: A sample case of resilience? Dev. Psychopathol. 1996, 8, 867–885. [Google Scholar] [CrossRef]
- Cosco, T.D.; Kaushal, A.; Hardy, R.; Richards, M.; Kuh, D.; Stafford, M. Operationalising resilience in longitudinal studies: A systematic review of methodological approaches. J. Epidemiol. Community Health 2017, 71, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Hertzog, C.; Jopp, D.S. Resilience in the face of cognitive aging: Experience, adaptation, and compensation. In New Frontiers in Resilient Aging: Life-Strengths and Well-Being in Late Life; Fry, P., Keyes, C., Eds.; Cambridge University Press: New York, NY, USA, 2010; pp. 130–161. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. Mini-mental state. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Blesa, R.; Pujol, M.; Aguilar, M.; Santacruz, P.; Bertran-Serra, I.; Hernández, G.; Sol, J.M.; Peña-Casanova, J. Clinical validity of the ‘mini-mental state’ for Spanish speaking communities. Neuropsychologia 2001, 39, 1150–1157. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Moret-Tatay, C.; Fernández-Muñoz, J.J.; Civera-Mollá, C.; Navarro-Pardo, E.; Alcover-de-la-Hera, C. Psychometric properties and Factor structure of the BRCS in an elderly Spanish sample. An. Psicol. Ann. Psychol. 2015, 31, 1030–1034. [Google Scholar] [CrossRef]
- Vilagut, G.; María Valderas, J.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretación de los cuestionarios de salud SF-36 y SF-12 en España: Componentes físico y mental. Med. Clínica. 2008, 130, 726–735. [Google Scholar] [CrossRef]
- Baztán, J.; Pérez del Molino, J.; Alarcón, T.; San Cristóbal, E.; Izquierdo, G.; Manzarbeitia, J. Índice de Barthel: Instrumento válido para la valoración funcional de pacientes con enfermedad cerebrovascular. Rev. Esp. Geriatr. Gerontol. 1993, 28, 32–40. [Google Scholar]
- Vergara, I.; Bilbao, A.; Orive, M.; Garcia-Gutierrez, S.; Navarro, G.; Quintana, J.M. Validation of the Spanish version of the Lawton IADL Scale for its application in elderly people. Health Qual. Life Outcomes 2012, 10, 130. [Google Scholar] [CrossRef]
- Hayes, A.F.; Rockwood, N.J. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behav. Res. Ther. 2017, 98, 39–57. [Google Scholar] [CrossRef] [PubMed]
- Meléndez, J.C.; Satorres, E.; Redondo, R.; Escudero, J.; Pitarque, A. Wellbeing, resilience, and coping: Are there differences between healthy older adults, adults with mild cognitive impairment, and adults with Alzheimer-type dementia? Arch. Gerontol. Geriatr. 2018, 77, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Perna, L.; Mielck, A.; Lacruz, M.E.; Emeny, R.T.; Holle, R.; Breitfelder, A.; Ladwig, K.H. Socioeconomic position, resilience, and health behaviour among elderly people. Int. J. Public. Health 2012, 57, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Kemper, K.J.; Mo, X.; Khayat, R.; Cramer, H. Are mindfulness and self-compassion associated with sleep and resilience in health professionals? Dtsch. Z. Für Akupunkt 2016, 59, 28–29. [Google Scholar] [CrossRef] [PubMed]
- Ezeamama, A.E.; Elkins, J.; Simpson, C.; Smith, S.L.; Allegra, J.C.; Miles, T.P. Indicators of resilience and healthcare outcomes: Findings from the 2010 health and retirement survey. Qual. Life Res. 2016, 25, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Pruchno, R.; Carr, D. Successful Aging 2.0: Resilience and Beyond. J. Gerontol. Ser. B 2017, 72, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Meerow, S.; Newell, J.P.; Stults, M. Defining urban resilience: A review. Landsc. Urban Plan. 2016, 147, 38–49. [Google Scholar] [CrossRef]
- Pusswald, G.; Tropper, E.; Kryspin-Exner, I.; Moser, D.; Klug, S.; Auff, E.; Dal-Bianco, P.; Lehrner, J. Health-Related Quality of Life in Patients with Subjective Cognitive Decline and Mild Cognitive Impairment and its Relation to Activities of Daily Living. J. Alzheimers Dis. 2015, 47, 479–486. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Tsai, W.-C.; Chiu, M.-J.; Tang, L.-Y.; Lee, H.-J.; Shyu, Y.-I.L.; Wang, W.S. Relationships Between Cognitive Dysfunction and Health-Related Quality of Life among Older Persons in Taiwan: A Nationwide Population-Based Survey. Am. J. Alzheimers Dis. Other Demen. 2019, 34, 41–48. [Google Scholar] [CrossRef]
- León-Salas, B.; Ayala, A.; Blaya-Nováková, V.; Avila-Villanueva, M.; Rodríguez-Blázquez, C.; Rojo-Pérez, F.; Fernández-Mayoralas, G.; Martínez-Martín, P.; Forjaz, M.J. Quality of life across three groups of older adults differing in cognitive status and place of residence. Geriatr. Gerontol. Int. 2015, 15, 627–635. [Google Scholar] [CrossRef]
- Nikmat, A.W.; Al-Mashoor, S.H.; Hashim, N.A. Quality of life in people with cognitive impairment: Nursing homes versus home care. Int. Psychogeriatr. 2015, 27, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Lee, E. Quality of Life and Its Factors in Korean Elderly with Mild Cognitive Impairment. Clin. Nurs. Res. 2018, 27, 871–889. [Google Scholar] [CrossRef] [PubMed]
- Bárrios, H.; Narciso, S.; Guerreiro, M.; Maroco, J.; Logsdon, R.; de Mendonça, A. Quality of life in patients with mild cognitive impairment. Aging Ment. Health 2013, 17, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Baltes, P.B.; Baltes, M.M. Optimierung durch Selektion und Kompensation. Z Für Pädagog. 1989, 35, 85–105. [Google Scholar]
- Baltes, P.B.; Baltes, M.M. Successful Aging: Perspectives from the Behavioral Sciences; Cambridge University Press: New York, NY, USA, 1993; p. 418. [Google Scholar]
- Baltes, P.B.; Smith, J. New Frontiers in the Future of Aging: From Successful Aging of the Young Old to the Dilemmas of the Fourth Age. Gerontology 2003, 49, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Bäckman, L.; Dixon, R.A. Psychological compensation: A theoretical framework. Psychol. Bull. 1992, 112, 259–283. [Google Scholar] [CrossRef] [PubMed]
- García, A.J.; García, M.Á. Nuevas formas de envejecer activamente: Calidad de vida y actividad física desde una perspectiva psicosocial. Escr. Psicol. Internet 2013, 6, 1–5. [Google Scholar] [CrossRef]
- Jopp, D.; Smith, J. Resources and life-management strategies as determinants of successful aging: On the protective effect of selection, optimization, and compensation. Psychol. Aging 2006, 21, 253–265. [Google Scholar] [CrossRef]
- Uriarte Arciniega, J.D. Resiliencia y Envejecimiento. Eur. J. Invest. Health Psychol. Educ. 2014. [Google Scholar] [CrossRef]
- Jekel, K.; Damian, M.; Wattmo, C.; Hausner, L.; Bullock, R.; Connelly, P.J.; Dubois, B.; Eriksdotter, M.; Ewers, M.; Graessel, E.; et al. Mild cognitive impairment and deficits in instrumental activities of daily living: A systematic review. Alzheimers Res. Ther. 2015, 7, 17. [Google Scholar] [CrossRef]
- Rodakowski, J.; Becker, A.M.; Golias, K.W. Activity-Based Goals Generated by Older Adults with Mild Cognitive Impairment. OTJR Occup. Particip. Health 2018, 38, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Ciro, C.A.; Anderson, M.P.; Hershey, L.A.; Prodan, C.I.; Holm, M.B. Instrumental Activities of Daily Living Performance and Role Satisfaction in People With and Without Mild Cognitive Impairment: A Pilot Project. Am. J. Occup. Ther. 2015, 69, 1–10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dixon, R.A.; de Frias, C.M. Mild memory deficits differentially affect 6-year changes in compensatory strategy use. Psychol. Aging. 2007, 22, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Navarro, A.B.; Bueno, B. Afrontamiento de problemas de salud en personas muy mayores. An. Psicol. 2015, 31, 1008. [Google Scholar] [CrossRef]

| Variable/Characteristics | All Sample n = 62 | Non-Resilient n = 32 | Resilient n = 30 | |
|---|---|---|---|---|
| Sex | Male | 21 (33.9%) | 14 (43.8%) | 7 (23.3%) |
| Female | 41 (66.1%) | 18 (56.2%) | 23 (76.7%) | |
| Age | 77.52 ± 8.26 | 78.78 ± 8.22 | 76.17 ± 8.23 | |
| Marital status | Single | 2 (3.2%) | 1 (3.1%) | 1 (3.3%) |
| Married | 27 (43.5%) | 13 (40.6%) | 14 (46.7%) | |
| Divorced | 3 (4.8%) | 1 (3.1%) | 2 (6.7%) | |
| Widowed | 30 (48.4%) | 17 (53.1%) | 13 (43.3%) | |
| Cognitive status | MMSE | 22.91 ± 2.21 | 23.09 ± 2.16 | 22.73 ± 2.30 |
| Variable | Scale | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Resilience | 1 | 0.279 * | 0.320 * | 0.314 * | 0.096 | 0.318 * | 0.137 | 0.316 * | 0.249 * | 0.075 | 0.201 | 0.287 * | 0.144 | |
| 2. ADLs | 1 | 0.595 ** | 0.466 ** | 0.275 * | 0.185 | 0.097 | 0.138 | 0.310 * | 0.039 | 0.149 | 0.399 ** | 0.030 | ||
| 3. IADLs | 1 | 0.548 ** | 0.153 | 0.204 | 0.001 | 0.185 | 0.127 | −0.106 | −0.038 | 0.460 ** | −0.187 | |||
| HRQOL | 4. Physical Function | 1 | 0.460 ** | 0.490 ** | 0.156 | 0.252 * | 0.486 ** | 0.167 | 0.278 * | 0.800 ** | 0.040 | |||
| 5. Role Physical | 1 | 0.419 ** | 0.360 ** | 0.312 * | 0.584 ** | 0.471 ** | 0.532 ** | 0.609 ** | 0.427 ** | |||||
| 6. Body Pain | 1 | 0.305 * | 0.304 * | 0.481 ** | 0.289 * | 0.381 ** | 0.663 ** | 0.236 | ||||||
| 7. General Health | 1 | 0.407 ** | 0.358 ** | 0.082 | 0.273 * | 0.507 ** | 0.188 | |||||||
| 8. Vitality | 1 | 0.378 ** | 0.102 | 0.447 ** | 0.363 ** | 0.435 ** | ||||||||
| 9. Social Function | 1 | 0.246 | 0.525 ** | 0.572 ** | 0.483 ** | |||||||||
| 10. Role Emotional | 1 | 0.597 ** | −0.048 | 0.799 ** | ||||||||||
| 11. Mental Health | 1 | 0.153 | 0.869 ** | |||||||||||
| 12. Physical Health Summary | 1 | −0.106 | ||||||||||||
| 13. Mental Health Summary | 1 |
| Variable | Scale | Non-Resilient | Resilient | p |
|---|---|---|---|---|
| n = 32 | n = 30 | |||
| ADLs | Feeding | 9.38 ± 1.68 | 9.50 ± 1.52 | 0.761 |
| Bathing | 4.38 ± 1.68 | 4.83 ± 0.91 | 0.185 | |
| Dressing | 9.38 ± 1.68 | 9 ± 2.42 | 0.479 | |
| Grooming * | 4.38 ± 1.68 | 5 ± 0.00 | 0.044 | |
| Bowels | 10 ± 0.00 | 10 ± 0.00 | - | |
| Bladder * | 8.75 ± 2.84 | 10 ± 1.31 | 0.030 | |
| Toilet use | 9.69 ± 1.23 | 10 ± 1.31 | 0.337 | |
| Transfers (bed to chair and back) * | 12.97 ± 3.07 | 14.33 ± 2.17 | 0.047 | |
| Mobility (on levels surfaces) | 13.13 ± 3.30 | 14.20 ± 3.08 | 0.191 | |
| Stairs * | 6.56 ± 3.68 | 8.37 ± 3.22 | 0.045 | |
| IADLs | Ability to use telephone | 0.94 ± 0.24 | 0.93 ± 0.25 | 0.948 |
| Shopping * | 0.34 ± 0.48 | 0.63 ± 0.49 | 0.022 | |
| Food preparation * | 0.41 ± 0.49 | 0.67 ± 0.47 | 0.041 | |
| Housekeeping | 0.47 ±0.50 | 0.60 ± 0.49 | 0.308 | |
| Laundry | 0.50 ± 0.50 | 0.70 ± 0.46 | 0.111 | |
| Mode of transportation ** | 0.34 ± 0.48 | 0.73 ± 0.45 | 0.002 | |
| Responsibility for own medications | 0.50 ± 0.50 | 0.73 ± 0.45 | 0.060 | |
| Ability to handle finances | 0.56 ± 0.50 | 0.70 ± 0.46 | 0.269 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clement-Carbonell, V.; Ferrer-Cascales, R.; Ruiz-Robledillo, N.; Rubio-Aparicio, M.; Portilla-Tamarit, I.; Cabañero-Martínez, M.J. Differences in Autonomy and Health-Related Quality of Life between Resilient and Non-Resilient Individuals with Mild Cognitive Impairment. Int. J. Environ. Res. Public Health 2019, 16, 2317. https://doi.org/10.3390/ijerph16132317
Clement-Carbonell V, Ferrer-Cascales R, Ruiz-Robledillo N, Rubio-Aparicio M, Portilla-Tamarit I, Cabañero-Martínez MJ. Differences in Autonomy and Health-Related Quality of Life between Resilient and Non-Resilient Individuals with Mild Cognitive Impairment. International Journal of Environmental Research and Public Health. 2019; 16(13):2317. https://doi.org/10.3390/ijerph16132317
Chicago/Turabian StyleClement-Carbonell, Violeta, Rosario Ferrer-Cascales, Nicolás Ruiz-Robledillo, María Rubio-Aparicio, Irene Portilla-Tamarit, and María José Cabañero-Martínez. 2019. "Differences in Autonomy and Health-Related Quality of Life between Resilient and Non-Resilient Individuals with Mild Cognitive Impairment" International Journal of Environmental Research and Public Health 16, no. 13: 2317. https://doi.org/10.3390/ijerph16132317
APA StyleClement-Carbonell, V., Ferrer-Cascales, R., Ruiz-Robledillo, N., Rubio-Aparicio, M., Portilla-Tamarit, I., & Cabañero-Martínez, M. J. (2019). Differences in Autonomy and Health-Related Quality of Life between Resilient and Non-Resilient Individuals with Mild Cognitive Impairment. International Journal of Environmental Research and Public Health, 16(13), 2317. https://doi.org/10.3390/ijerph16132317






