The Association between Demographic Characteristics, Lifestyle Health Behaviours, and Quality of Life among Adolescents in Asia Pacific Region
Abstract
1. Introduction
2. Methods
2.1. Sampling
2.2. Sample Size Calculation
2.3. Study Tools
2.4. Ethical Approval
2.5. Data Collection
2.6. Statistical Analysis
3. Results
Demographics
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgements
Conflicts of Interest
References
- Barile, J.P.; Reeve, B.B.; Smith, A.W.; Zack, M.M.; Mitchell, S.A.; Kobau, R.; Cella, D.F.; Luncheon, C.; Thompson, W.W. Monitoring population health for Healthy People 2020: Evaluation of the NIH PROMIS® Global Health, CDC Healthy Days, and satisfaction with life instruments. Qual. Life Res. 2013, 22, 1201–1211. [Google Scholar] [CrossRef] [PubMed]
- Klein, J.D.; Alden, E.R. Children, gender, education, and health. Pediatrics 2017, 140, e20171322. [Google Scholar] [CrossRef] [PubMed]
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef]
- Aira, T.; Wang, W.; Riedel, M.; Witte, S.S. Reducing risk behaviors linked to noncommunicable diseases in Mongolia: A randomized controlled trial. Am. J. Public Health 2013, 103, 1555–1674. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.; Williams, J.; Townsend, N.; Mikkelsen, B. Roberts N4, Foster C1, Wickramasinghe, K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob. Health 2017, 5, E277–E289. [Google Scholar] [CrossRef]
- Varni, J.W.; Katz, E.R.; Seid, M.; Quiggins, D.J.; Friedman-Bender, A.; Castro, C.M. The Pediatric Cancer Quality of Life Inventory: Instrument development, descriptive statistics, and cross-informant variance. J. Behav. Med. 1998, 21, 179–204. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health for the World’s Adolescents: A Second Chance in the Second Decade; Department of Maternal, Child and Adolescent Health, Ed.; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Lehnert, T.; Sonntag, D.; Konnopka, A.; Riedel-Heller, S.; König, H.H. The long-term cost-effectiveness of obesity prevention interventions: Systematic literature review. Obes. Rev. 2012, 13, 537–553. [Google Scholar] [CrossRef]
- World Health Organization. Burden: Mortality, Morbidity and Risk Factors; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- UNICEF. Progress for Children: A Report Card on Adolescents; UNICEF: New York, NY, USA, 2012. [Google Scholar]
- Gielen, U.P.; Roopnarine, J.L. Childhood and Adolescence: Cross-Cultural Perspectives and Applications, 2nd ed.; Praeger: Santa Barbara, CA, USA, 2016. [Google Scholar]
- Arends-Kuenning, M.; Duryen, S. The effect of parental presence, parents’ education, and household hardship on adolescents’ schooling and work in Latin America. J. Fam. Econ. Issues 2006, 27, 263–286. [Google Scholar] [CrossRef]
- Bowker, J.C.; Ostrov, J.M.; Raja, R. Relational and overt aggression in urban India: Association with peer relations and best friends’ aggression. Int. J. Behav. Dev. Psychol. 2012, 36, 107–116. [Google Scholar] [CrossRef]
- Berg, N. Accumulation of Disadvantage from Adolescence to Midlife: A 26-Year Follow Up Study of 16-Year Old Adolescents; Faculty of Medicine, University of Helsinki: Helsinki, Finland, 2017. [Google Scholar]
- Lee, R.L.T.; Loke, A.Y. Lifestyle behaviours and psychosocial well-being of Chinese adolescents in Hong Kong and Guangzhou, China: A cross-sectional comparative survey. J. Clin. Nurs. 2011, 20, 2733–2743. [Google Scholar] [CrossRef]
- Rew, L.; Arheart, K.L.; Thompson, S.; Johnson, K. Predictors of adolescents’ health-promoting behaviours guided by primary socialization theory. J. Pediatric Nurs. 2013, 18, 277–288. [Google Scholar]
- Vingilis, E.R.; Wade, T.J.; Seeley, J.S. Predictors of adolescent self-rated health: Analysis of the National Population Health Survey. Can. J. Public Health 2002, 93, 193–197. [Google Scholar] [PubMed]
- Schwimmer, J.B.; Burwinkle, T.M.; Varni, J.W. Health-related quality of lie of severely obese children and adolescents. Am. Med Assoc. 2003, 37, 220–221. [Google Scholar]
- Kistler, K.D.; Molleston, J.; Unalp, A.; Abrams, S.H.; Behling, C.; Schwimmer, J.B. Symptoms and quality of life in obese children and adolescents with nonalcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2010, 31, 396–406. [Google Scholar] [CrossRef] [PubMed]
- McCarty, C.A.; Wymbs, B.T.; Mason, W.A.; King, K.M.; McCauley, E.; Baer, J.; Stoep, A.V. Early adolescent growth in depression and conduct problem symptoms as predictors of later substance use impairment. J. Abnorm. Child Psychol. 2013, 41, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Luszczynska, A.; Gibbons, F.X.; Piko, B.; Tekoze, M. Self-regulatory cognitions, social comparison, and perceived peer’s behaviors as predictors of nutrition and physical activity: A comparison among adolescents in Hungary, Poland, Turkey, and USA. Psychol. Health 2004, 19, 577–593. [Google Scholar] [CrossRef]
- Lacy, K.E.; Allender, S.; Kremer, P.; de Silva-Sanigorsk, A.; Millar, L.; Moodie, M. Screen time and physical activity behaviours are associated with health-related quality of life in Australian adolescents. Qual. Life Res. 2011, 21, 1085–1099. [Google Scholar] [CrossRef] [PubMed]
- Iversen, A.C.; Holsen, I. Inequality in health, psychosocial resources and health behaviour in early adolescence: The influence of different indicators of socioeconomic position. Child Indic. Res. 2008, 1, 291–302. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Framing Adolescent and Young Adult through Healthy People 2020 Webinar: Adolescent Health. Available online: https://www.healthypeople.gov/ (accessed on 25 June 2019).
- Office of Disease Prevention and Health Promotion. Healthy People 2020: Adolescent Health-Objectives. 2012. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/Adolescent-Health (accessed on 25 June 2019).
- Pender, N.J. Health Promotion Model Manual. 2011. Available online: http://deepbluelib.umich.edu/bitstream/2027.42/85350/1/heal (accessed on 25 June 2019).
- Aljasem, L.I.; Peyrot, M.; Wissow, L.; Rubin, R.R. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001, 27, 393–404. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Toobert, D.J.; Gillette, C.D. Psychosocial barriers to diabetes self-management and quality of life. Diabetes Spectr. 2001, 14, 33–41. [Google Scholar] [CrossRef]
- De Wulf, M. Population Pyramids of the World from 1950 to 2100: China, Hong Kong SAR 2017. 2017. Available online: https://www.populationpyramid.net/china-hong-kong-sar/2017/ (accessed on 25 June 2018).
- De Wulf, M. Population Pyramids of the World from 1950 to 2100: China 2017. 2017. Available online: https://www.populationpyramid.net/china/2017/ (accessed on 25 June 2018).
- De Wulf, M. Population Pyramids of the World from 1950 to 2100: Japan 2017. 2017. Available online: https://www.populationpyramid.net/japan/2017/ (accessed on 25 June 2018).
- De Wulf, M. Population Pyramids of the World from 1950 to 2100: Republic of Korea 2017. 2017. Available online: https://www.populationpyramid.net/republic-of-korea/2017/ (accessed on 25 June 2018).
- De Wulf, M. Population Pyramids of the World from 1950 to 2100: Thailand 2017. 2017. Available online: https://www.populationpyramid.net/thailand/2017/ (accessed on 25 June 2018).
- Population of 2017. Population oF Beijing 2017. 2017. Available online: http://populationof2017.com/population-of-beijing-2017.html (accessed on 25 June 2018).
- Population of 2017. Population oF Seoul 2017. 2017. Available online: http://populationof2017.com/population-of-seoul-2017.html (accessed on 25 June 2018).
- Population of 2017. Population of Bangkok 2017. 2017. Available online: http://populationof2017.com/population-of-bangkok-2017.html (accessed on 25 June 2018).
- Akashi city hall. [M1] Public information Akashi text version April 15, 2017. 2017. Available online: https://www.city.akashi.lg.jp/shise/koho/kohotext/h29/0415.html (accessed on 10 May 2019).
- Barlett, J.; Kotrlik, J.; Higgins, C. Organizational research: Determining appropriate sample size in survey research. Information Technology. Learn. Perform. J. 2001, 19, 43–50. [Google Scholar]
- Gillis, A.J. The Adolescent Lifestyle Questionnaire: Development and psychometric testing. Can. J. Nurs. Res. 1997, 29, 29–46. [Google Scholar] [PubMed]
- Guillemin, F.; Bombardier, C.; Beaton, D. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
- Feng, L.; Zhang, Y.; Chen, R.; Hao, Y. The Chinese version of the Pediaric Quality of Life Inventory 3.0 Asthma Module: Reliability and validity. Health Qual. Life Outcomes 2011, 9, 64. [Google Scholar] [CrossRef] [PubMed]
- Kook, S.H.; Varni, J.W. Validation of the Korean version of the pediatric quality of life inventory™ 4.0 (PedsQL™) generic core scales in school children and adolescents using the RASCH model. Health Qual. Life Outcomes 2008, 6, 41. [Google Scholar] [CrossRef] [PubMed]
- Iori, S.; Akiko, H.; Yanagisawa, T.; Mukasa, A.; Ida, K.; Sawamura, Y.; Sugiyama, K.; Saito, N.; Kumabe, T.; Terasaki, M.; et al. Development of the Japanese version of the Pediatric Quality of Life Inventory™ Brain Tumor Module. Health Qual. Life Outcomes 2010, 8, 38. [Google Scholar]
- Sritipsukho, P.; Wisai, M.; Thavorncharoensap, M. Reliability and validity of the Thai version of the Pediatric Quality of Life Inventory 4.0. Qual. Life Res. 2013, 22, 551–557. [Google Scholar] [CrossRef]
- World Health Organization. Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Nunes, C.; Hernando, A.; Lemos, I.; Ayala-Nunes, L.; Oliva, C.R.; Coronado, C.M. Quality of life of Portuguese and Spanish adolescents. A comparative study between natives and immigrants. Ciencia Saude Coletiva 2016, 21, 1137–1144. [Google Scholar] [CrossRef]
- World Health Organization. Improving the Quality of Paediatric Care: An Operational Guide for Facility-Based Audit and Reivew of Paediatric Mortality; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Damnjanovic, M.; Lakic, A.; Stevanovic, D.; Jovanovic, A. Effects of mental health on quality of life in children and adolescents living in residential and foster care: A cross-sectional study. Epidemiol. Psychiatr. Sci. 2011, 20, 257–262. [Google Scholar] [CrossRef]
- Magai, D.N.; Koot, H.M. Quality of life in children and adolescents in Central Kenya: Associations with emotional and behavioral problems. Qual. Life Res. 2019, 28, 1271–1279. [Google Scholar] [CrossRef]
- Krapels, S.H.; Grant, J. Exploring the effectiveness, efficiency and equity (3e’s) of research and research impact assessment. Palgrave Commun. 2016, 2, 16090. [Google Scholar] [CrossRef]
- Lerner, R.M.; Almerigi, J.; Theokas, C.; Lerner, J.V. Positive youth development: A view of the issues. J. Early Adolesc. 2005, 25, 10–16. [Google Scholar] [CrossRef]
- Schmidt, S.; Bullinger, M. Current Issues in Cross-Cultural Quality of Life Instrument Development. Arch. Phys. Med. Rehabil. 2003, 84 (Suppl. 2), S29–S34. [Google Scholar] [CrossRef] [PubMed]
- Social Determinants and The Health of Indigenous Peoples in Australia—A Human Rights Based Approach. 2017. Available online: https://www.humanrights.gov.au/about/news/speeches/social-determinants-and-health-indigenous-peoples-australia-human-rights-based (accessed on 25 June 2019).
| Source | F | df1 | df2 | p |
|---|---|---|---|---|
| Corrected Model | 224.022 | 4 | 1589 | <0.001 |
| City | 224.022 | 4 | 1589 | <0.001 |
| Age | 0.087 | 1 | 1589 | 0.768 |
| Gender | 0.621 | 1 | 1589 | 0.431 |
| Education level | 40.192 | 4 | 1589 | <0.001 |
| Religion | 3.855 | 4 | 1589 | 0.004 |
| Parents’ marital status | 0.655 | 1 | 1589 | 0.418 |
| ALQ physical participation | 6.013 | 1 | 1589 | 0.014 |
| ALQ nutrition | 27.710 | 1 | 1589 | <0.001 |
| ALQ social support | 6.327 | 1 | 1589 | 0.012 |
| ALQ stress management | 0.013 | 1 | 1589 | 0.910 |
| ALQ identity awareness | 501.718 | 1 | 1589 | <0.001 |
| ALQ health practices | 9.635 | 1 | 1589 | 0.002 |
| ALQ safety | 0.010 | 1 | 1589 | 0.921 |
| Model Term | Coefficient | SE | t | p | 95% CI | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Intercept | 2.843 | 0.1584 | 17.943 | 0.000 | 2.532 | 3.154 |
| Hong Kong | −0.010 | 0.0105 | −0.937 | 0.349 | −0.030 | 0.011 |
| Beijing | 0.182 | 0.0363 | 5.025 | 0.000 | 0.111 | 0.253 |
| Tokyo & Hyogo | 0.147 | 0.0334 | 4.404 | 0.000 | 0.082 | 0.212 |
| Seoul | 0.231 | 0.0135 | 17.182 | 0.000 | 0.205 | 0.258 |
| Bangkok | 0 b | . | . | . | . | . |
| Age | −0.004 | 0.0143 | −0.295 | 0.768 | −0.032 | 0.024 |
| Male | 0.015 | 0.0196 | 0.788 | 0.431 | −0.023 | 0.054 |
| Female | 0 b | . | . | . | . | . |
| Grade 4 | −0.124 | 0.0879 | −1.410 | 0.159 | −0.296 | 0.049 |
| Grade 5 | −0.092 | 0.0695 | −1.327 | 0.185 | −0.229 | 0.044 |
| Grade 6 | −0.094 | 0.0739 | −1.275 | 0.202 | −0.239 | 0.051 |
| Grade 7 | −0.151 | 0.0522 | −2.896 | 0.004 | −0.254 | −0.049 |
| Grade 8 | −0.024 | 0.0786 | −0.311 | 0.756 | −0.179 | 0.130 |
| Grade 9 | 0 b | . | . | . | . | . |
| Protestantism | −0.064 | 0.0223 | −2.863 | 0.004 | −0.107 | −0.020 |
| Catholic Church | −0.051 | 0.1616 | −0.313 | 0.754 | −0.368 | 0.266 |
| Buddhism | −0.098 | 0.0334 | −2.939 | 0.003 | −0.163 | −0.033 |
| Islam | −0.026 | 0.1071 | −0.239 | 0.811 | −0.236 | 0.184 |
| Other religion | −0.246 | 0.0166 | −14.785 | 0.000 | −0.279 | −0.213 |
| No religious belief | 0 b | . | . | . | . | . |
| Parents not living together | 0.027 | 0.0335 | 0.810 | 0.418 | −0.039 | 0.093 |
| Parents married and living together | 0 b | . | . | . | . | . |
| ALQ physical participation | 0.049 | 0.0198 | 2.452 | 0.014 | 0.010 | 0.087 |
| ALQ nutrition | 0.073 | 0.0138 | 5.264 | 0.000 | 0.046 | 0.100 |
| ALQ social support | 0.112 | 0.0445 | 2.515 | 0.012 | 0.025 | 0.199 |
| ALQ stress management | 0.002 | 0.0200 | 0.114 | 0.910 | −0.037 | 0.042 |
| ALQ identity awareness | 0.171 | 0.0077 | 22.399 | 0.000 | 0.156 | 0.186 |
| ALQ health practices | −0.034 | 0.0110 | −3.104 | 0.002 | −0.056 | −0.013 |
| ALQ safety | −0.001 | 0.0123 | −0.100 | 0.921 | −0.025 | 0.023 |
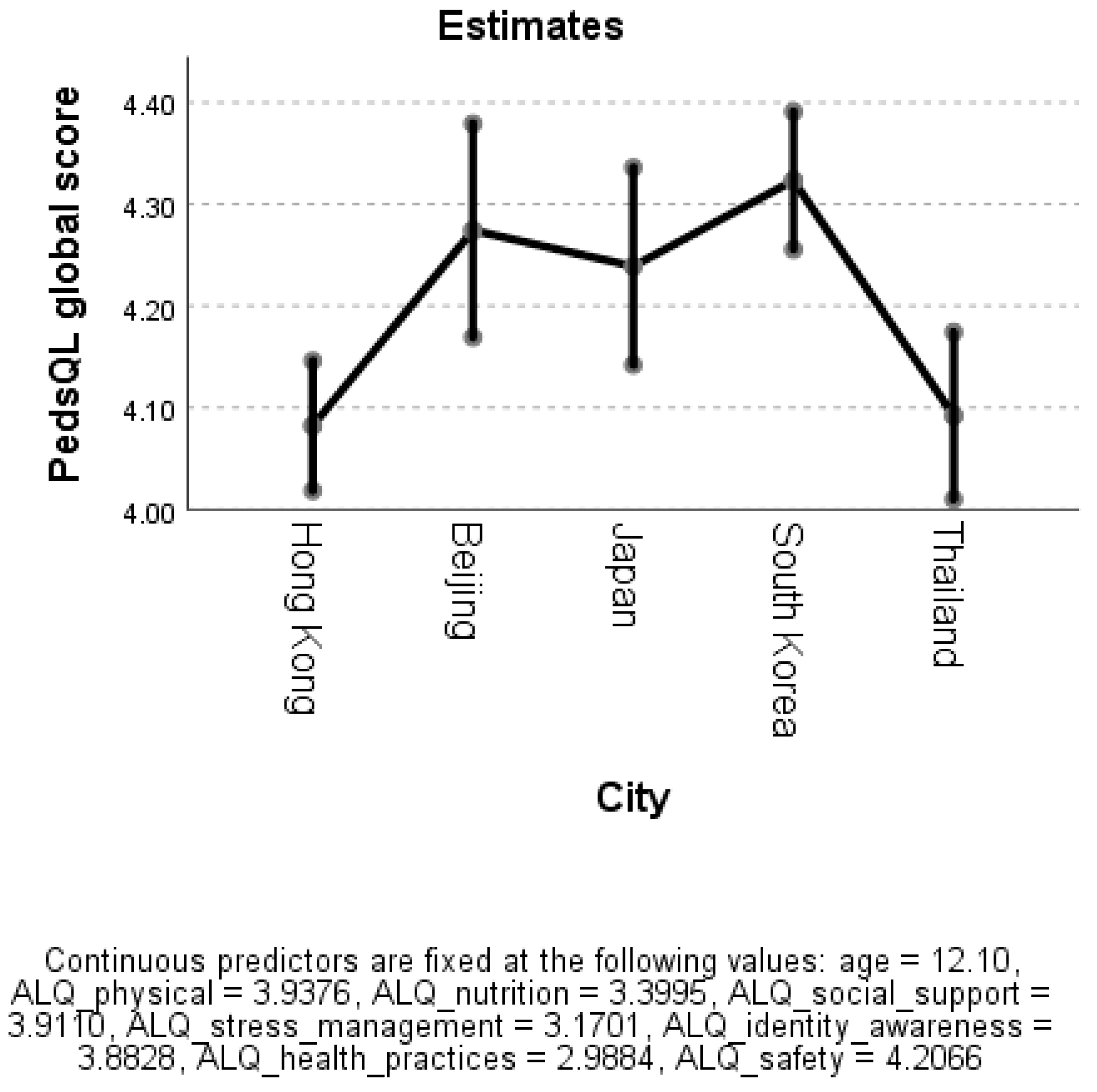
| City | Mean | SE | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower | Upper | |||
| Hong Kong | 4.082 | 0.033 | 4.018 | 4.146 |
| Beijing | 4.274 | 0.054 | 4.169 | 4.379 |
| Japan | 4.239 | 0.049 | 4.142 | 4.336 |
| South Korea | 4.323 | 0.035 | 4.255 | 4.391 |
| Thailand | 4.092 | 0.042 | 4.010 | 4.174 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, R.L.T.; Chien, W.T.; Tanida, K.; Takeuchi, S.; Rutja, P.; Kwok, S.W.H.; Lee, P.H. The Association between Demographic Characteristics, Lifestyle Health Behaviours, and Quality of Life among Adolescents in Asia Pacific Region. Int. J. Environ. Res. Public Health 2019, 16, 2324. https://doi.org/10.3390/ijerph16132324
Lee RLT, Chien WT, Tanida K, Takeuchi S, Rutja P, Kwok SWH, Lee PH. The Association between Demographic Characteristics, Lifestyle Health Behaviours, and Quality of Life among Adolescents in Asia Pacific Region. International Journal of Environmental Research and Public Health. 2019; 16(13):2324. https://doi.org/10.3390/ijerph16132324
Chicago/Turabian StyleLee, Regina L.T., Wai Tong Chien, Keiko Tanida, Sachi Takeuchi, Phuphaibul Rutja, Stephen W. H. Kwok, and Paul H. Lee. 2019. "The Association between Demographic Characteristics, Lifestyle Health Behaviours, and Quality of Life among Adolescents in Asia Pacific Region" International Journal of Environmental Research and Public Health 16, no. 13: 2324. https://doi.org/10.3390/ijerph16132324
APA StyleLee, R. L. T., Chien, W. T., Tanida, K., Takeuchi, S., Rutja, P., Kwok, S. W. H., & Lee, P. H. (2019). The Association between Demographic Characteristics, Lifestyle Health Behaviours, and Quality of Life among Adolescents in Asia Pacific Region. International Journal of Environmental Research and Public Health, 16(13), 2324. https://doi.org/10.3390/ijerph16132324







