Safety and Effectiveness of Monochloramine Treatment for Disinfecting Hospital Water Networks
Abstract
:1. Introduction
2. Material and Methods
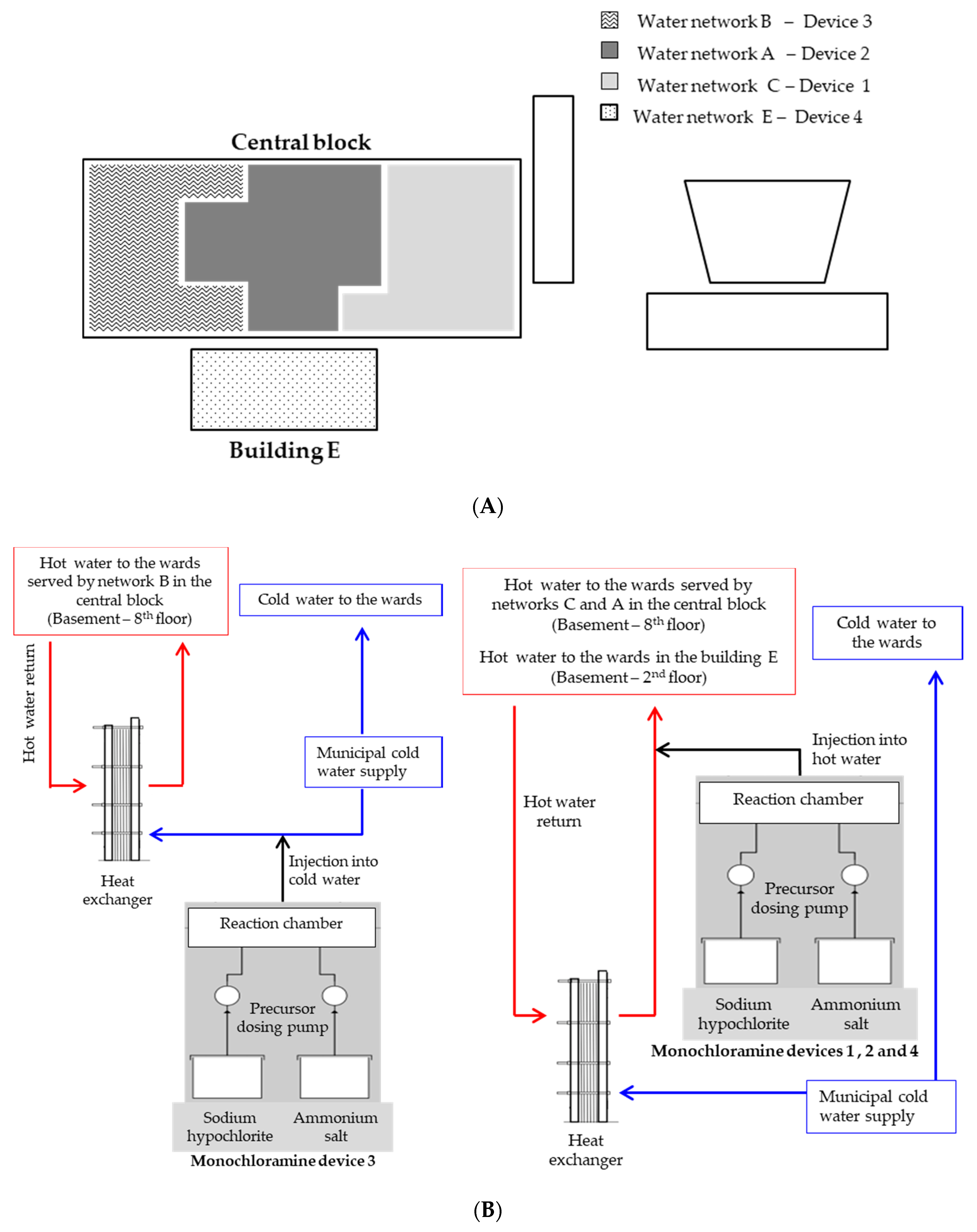
2.1. Hospital Setting
2.2. Sample Collection
2.3. Laboratory Methods
2.3.1. Microbiological Analysis
2.3.2. Chemical Analysis
2.3.3. Corrective Actions
2.3.4. Statistical Analysis
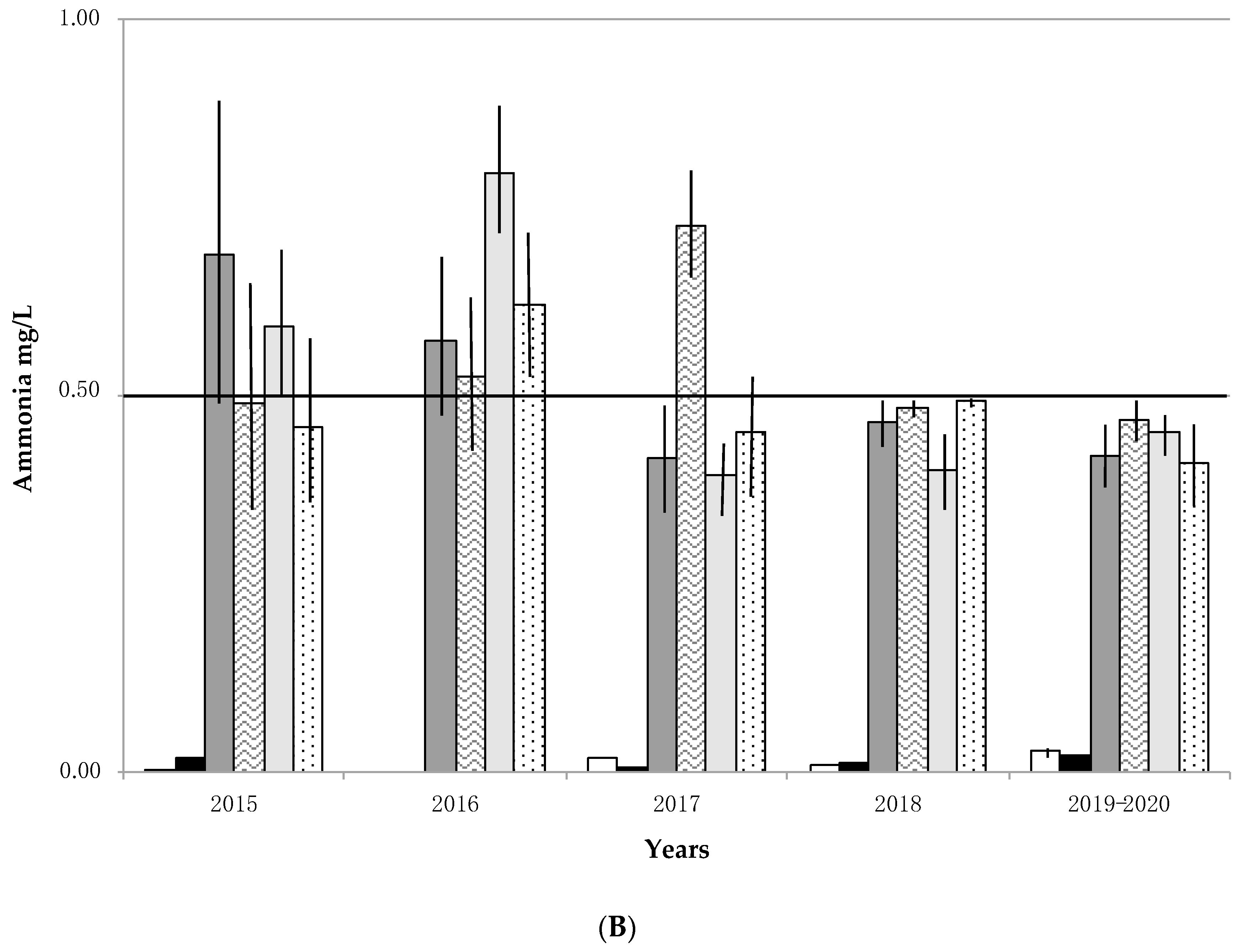
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lin, Y.E.; Stout, J.E.; Yu, V.L. Prevention of hospital-acquired legionellosis. Curr. Opin. Infect. Dis. 2011, 24, 350–356. [Google Scholar] [CrossRef]
- Superior Institute of Health. Italian Guidelines for Prevention and Control of Legionellosis; Approvate in Conferenza Stato-Regioni nella seduta del 7 maggio 2015; Superior Institute of Health: Rome, Italy, 2015. [Google Scholar]
- WHO. Legionella and the Prevention of Legionellosis; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Borella, P.; Bargellini, A.; Marchegiano, P.; Vecchi, E.; Marchesi, I. Hospital-acquired Legionella infections: An update on the procedures for controlling environmental contamination. Ann. Ig. 2016, 28, 98–108. [Google Scholar] [PubMed]
- Ngwenya, N.; Ncube, E.J.; Parsons, J. Recent advances in drinking water disinfection: Successes and challenges. Rev. Environ. Contam. Toxicol. 2013, 222, 111–170. [Google Scholar] [PubMed]
- Nieuwenhuijsen, M.J.; Smith, R.; Golfinopoulos, S.; Best, N.; Bennett, J.; Aggazzotti, G.; Righi, E.; Fantuzzi, G.; Bucchini, L.; Cordier, S.; et al. Health impacts of long-term exposure to disinfection by-products in drinking water in Europe: HIWATE. J. Water Health 2009, 7, 185–207. [Google Scholar] [CrossRef] [PubMed]
- Plewa, M.J.; Richardson, S.D. Water treatment and disinfection by-products. J. Environ. Sci. 2017, 58, 1–350. [Google Scholar] [CrossRef]
- Pule, D. Conventional and alternative disinfection methods of Legionella in water distribution systems—Review. Constr. Sci. 2016, 19, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Giovanardi, R.; Bononi, M.; Messori, M.; Bargellini, A.; Paduano, S.; Borella, P.; Marchesi, I. Corrosion resistance of commonly used plumbing materials for water distribution systems exposed to disinfection treatments. Corros. Eng. Sci. Technol 2020, 1–8. [Google Scholar] [CrossRef]
- Dice, J.C. Denver’s seven decades of experience with chloramination. J. Am. Water Works Assoc. 1985, 77, 34–37. [Google Scholar] [CrossRef]
- Kool, J.L.; Carpenter, J.C.; Fields, B.S. Effect of monochloramine disinfection of municipal drinking water on risk of nosocomial Legionnaires’ disease. Lancet 1999, 353, 272–277. [Google Scholar] [CrossRef]
- Heffelfinger, J.D.; Kool, J.L.; Fridkin, S.; Fraser, V.J.; Hageman, J.; Carpenter, J.; Whitney, C.G. Society for Healthcare Epidemiology of America. Risk of hospital-acquired legionnaires’ disease in cities using monochloramine versus other water disinfectants. Infect. Control Hosp. Epidemiol. 2003, 24, 569–574. [Google Scholar] [CrossRef] [Green Version]
- Flannery, B.; Gelling, L.B.; Vugia, D.J.; Weintraub, J.M.; Salerno, J.J.; Conroy, M.J.; Stevens, V.A.; Rose, C.E.; Moore, M.R.; Fields, B.S.; et al. Reducing Legionella colonization in water systems with monochloramine. Emerg. Infect. Dis. 2006, 12, 588–596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, M.R.; Pryor, M.; Fields, B.; Lucas, C.; Phelan, M.; Besser, R.E. Introduction of monochloramine into a municipal water system: Impact on colonization of buildings by Legionella spp. Appl. Environ. Microbiol. 2006, 72, 378–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marchesi, I.; Ferranti, G.; Bargellini, A.; Marchegiano, P.; Predieri, G.; Stout, J.E.; Borella, P. Monochloramine and chlorine dioxide for controlling Legionella pneumophila contamination: Biocide levels and disinfection by-products formation in hospital water networks. J. Water Health 2013, 11, 738–747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duda, S.; Kandiah, S.; Stout, J.E.; Baron, J.L.; Yassin, M.; Fabrizio, M.; Ferrelli, J.; Hariri, R.; Wagener, M.M.; Goepfert, J.; et al. Evaluation of a new monochloramine generation system for controlling Legionella in building hot water systems. Infect. Control Hosp. Epidemiol. 2014, 35, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Marchesi, I.; Ferranti, G.; Mansi, A.; Marcelloni, A.M.; Proietto, A.R.; Saini, N.; Borella, P.; Bargellini, A. Control of Legionella contamination and risk of corrosion in hospital water networks following various disinfecting procedures. Appl. Environ. Microbiol. 2016, 82, 2959–2965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coniglio, M.A.; Ferrante, M.; Yassin, M.H. Preventing Healthcare-Associated Legionellosis: Results after 3 Years of Continuous Disinfection of Hot Water with Monochloramine and an Effective Water Safety Plan. Int. J. Environ. Res. Public Health 2018, 15, 1594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simoes, L.C.; Simoes, M. Biofilms in drinking water: Problems and solutions. RSC Adv. 2013, 3, 2520–2533. [Google Scholar] [CrossRef] [Green Version]
- Nawrocki, J.; Andrzejewski, P. Nitrosamines and water. J. Hazard. Mater. 2011, 189, 1–18. [Google Scholar] [CrossRef]
- Kadmi, Y.; Favier, L.; Wolbert, D. N-nitrosamines, emerging disinfection by-products of health concern: An overview of occurrence, mechanisms of formation, control and analysis in water. Water Sci. Technol. 2015, 15, 11–25. [Google Scholar] [CrossRef]
- West, D.M.; Wu, Q.; Donovan, A.; Shi, H.; Ma, Y.; Jiang, H.; Wang, J. N-nitrosamine formation by monochloramine, free chlorine, and peracetic acid disinfection with presence of amine precursors in drinking water system. Chemosphere 2016, 153, 521–527. [Google Scholar] [CrossRef]
- Qiu, Y.; Bei, E.; Wang, Y.; Wang, J.; Zhang, X.; Chen, C. One representative water supply system in China with nitrosamine concern: Challenges and treatment strategies. J. Environ. Sci. 2020, 88, 12–20. [Google Scholar] [CrossRef] [PubMed]
- US Environmental Protection Agency (EPA). Drinking Water Standards and Health Advisories; 822-S-12-001; EPA: Washington, DC, USA, 2012.
- Krasner, S.W.; Kostopoulou, M.; Toledano, M.B.; Wright, J.; Patelarou, E.; Kogevinas, M.; Villanueva, C.M.; Carrasco-Turigas, G.; Santa Marina, L.; Fernández-Somoano, A.; et al. Occurrence of DBPs in Drinking Water of European Regions for Epidemiology Studies. J. Am. Water Works Assoc. 2016, 108, E501–E512. [Google Scholar] [CrossRef]
- Mitch, W.A.; Gerecke, A.C.; Sedlak, D.L. A N-Nitrosodimethylamine (NDMA) precursor analysis for chlorination of water and wastewater. Water Res. 2003, 37, 3733–3741. [Google Scholar] [CrossRef]
- Decreto Legislativo 2 Febbraio 2001 n. 31, e Successive Modifiche. Attuazione della Direttiva 98/83/CE Relativa alla Qualità delle Acque Destinate al Consumo Umano. Gazzetta Ufficiale n. 52 del 3.3.2001, Supplemento Ordinario n. 41. Available online: https://www.gazzettaufficiale.it/eli/id/2001/03/03/001G0074/sg (accessed on 1 July 2020).
- Council Directive 98/83/EC of 3 November 1998 on the quality of water intended for human consumption. Off. J. Eur. Union 1998, 330, 32–54.
- WHO. Guidelines for Drinking-Water Quality. In Incorporating the First Addendum, 4th ed.; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Marchesi, I.; Cencetti, S.; Marchegiano, P.; Frezza, G.; Borella, P.; Bargellini, A. Control of Legionella contamination in a hospital water distribution system by monochloramine. Am. J. Infect. Control 2012, 40, 279–281. [Google Scholar] [CrossRef]
- Paduano, S.; Marchesi, I.; Casali, M.E.; Valeriani, F.; Frezza, G.; Vecchi, E.; Sircana, L.; Romano Spica, V.; Borella, P.; Bargellini, A. Characterisation of microbial community associated with different disinfection treatments in hospital hot water networks. Int. J. Environ. Res. Public Health 2020, 17, 2158. [Google Scholar] [CrossRef] [Green Version]
- White, G.C. Handbook of Chlorination for Potable Water, Wastewater, Cooling Water, Industrial Processes, and Swimming Pools; Van Nostrand Reinhold: New York, NY, USA, 1972. [Google Scholar]
- Melada, S.; Coniglio, M.A. Monochloramine for remediation of Legionella only in domestic hot water systems: An iron fist in a velvet glove. Open J. Prev. Med. 2015, 5, 143–150. [Google Scholar] [CrossRef] [Green Version]
- Qi, W.; Fang Yee, L.; Jiangyong, H. Relationship between organic precursors and N-nitrosodimethylamine (NDMA) formation in tropical water sources. J. Water Health 2014, 12, 736–746. [Google Scholar] [CrossRef] [Green Version]
- Righi, E.; Bechtold, P.; Tortorici, D.; Lauriola, P.; Calzolari, E.; Astolfi, G.; Nieuwenhuijsen, M.J.; Fantuzzi, G.; Aggazzotti, G. Trihalomethanes, chlorite, chlorate in drinking water and risk of congenital anomalies: A population-based case-control study in Northern Italy. Environ. Res. 2012, 116, 66–73. [Google Scholar] [CrossRef]
- Casini, B.; Baggiani, A.; Totaro, M.; Mansi, A.; Costa, A.L.; Aquino, F.; Miccoli, M.; Valentini, P.; Bruschi, F.; Lopalco, P.L.; et al. Detection of viable but non-culturable legionella in hospital water network following monochloramine disinfection. J. Hosp. Infect. 2018, 98, 46–52. [Google Scholar] [CrossRef]
- Vu, T.N.; Kimura, S.Y.; Plewa, M.J.; Richardson, S.D.; Marinas, B.J. Predominant N-haloacetamide and haloacetonitrile formation in drinking water via the aldehyde reaction pathway. Environ. Sci. Technol. 2019, 53, 850–859. [Google Scholar] [CrossRef] [PubMed]

| Water Pipework | Samples Number | Legionella spp. Positives | Physical-Chemical Parameters | |||
|---|---|---|---|---|---|---|
| n/Total (%) a | Geometric Mean cfu/L (Range) | Monochloramine Mean ± SD mg/L | T (°C) Mean ± SD | pH Mean ± SD | ||
| A | 172 | 4/172 (2.3) | 1.3 × 102 (25–2.9 × 103) | 2.84 ±1.18 | 45.3 ± 4.5 b | 7.4 ± 0.3 |
| B | 136 | 6/136 (4.4) | 7.2 × 10 (25–3.0 × 102) | 2.98 ± 1.10 | 39.1 ± 6.6 | 7.5 ± 0.4 |
| C | 121 | 1/121 (0.8) | 2.5 × 103 | 2.82 ± 0.95 | 40.9 ± 5.0 | 7.4 ± 0.2 |
| E | 121 | 11/121 (9.1) | 2.9 × 102 (25–3.2 × 103) | 2.93 ± 0.90 | 40.7 ± 8.1 | 7.5 ± 0.2 |
| Total | 550 | 22/550 (4.0) | 1.9 × 102 (25–3.2 × 103) | 2.89 ± 1.05 | 41.8 ± 6.6 | 7.4 ± 0.3 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchesi, I.; Paduano, S.; Frezza, G.; Sircana, L.; Vecchi, E.; Zuccarello, P.; Oliveri Conti, G.; Ferrante, M.; Borella, P.; Bargellini, A. Safety and Effectiveness of Monochloramine Treatment for Disinfecting Hospital Water Networks. Int. J. Environ. Res. Public Health 2020, 17, 6116. https://doi.org/10.3390/ijerph17176116
Marchesi I, Paduano S, Frezza G, Sircana L, Vecchi E, Zuccarello P, Oliveri Conti G, Ferrante M, Borella P, Bargellini A. Safety and Effectiveness of Monochloramine Treatment for Disinfecting Hospital Water Networks. International Journal of Environmental Research and Public Health. 2020; 17(17):6116. https://doi.org/10.3390/ijerph17176116
Chicago/Turabian StyleMarchesi, Isabella, Stefania Paduano, Giuseppina Frezza, Luca Sircana, Elena Vecchi, Pietro Zuccarello, Gea Oliveri Conti, Margherita Ferrante, Paola Borella, and Annalisa Bargellini. 2020. "Safety and Effectiveness of Monochloramine Treatment for Disinfecting Hospital Water Networks" International Journal of Environmental Research and Public Health 17, no. 17: 6116. https://doi.org/10.3390/ijerph17176116





