Weather Woes? Exploring Potential Links between Precipitation and Age-Related Cognitive Decline
Abstract
:1. Introduction
2. Methods
2.1. Study Sample
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fu, P.; Guo, X.; Cheung, F.M.H.; Yung, K.K.L. The association between PM2.5 exposure and neurological disorders: A systematic review and meta-analysis. Sci. Total Environ. 2019, 655, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Kwong, J.C.; Copes, R.; Tu, K.; Villeneuve, P.J.; van Donkelaar, A.; Wilton, A.S. Living near major roads and the incidence of dementia, Parkinson’s disease, and multiple sclerosis: A population-based cohort study. Lancet 2017, 389, 718–726. [Google Scholar] [CrossRef]
- Chen, J.C.; Schwartz, J. Neurobehavioral effects of ambient air pollution on cognitive performance in US adults. Neurotoxicology 2009, 30, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Costafreda, S.G. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Cedeno Laurent, J.G.; Williams, A.; Oulhote, Y.; Zanobetti, A.; Allen, J.G.; Spengler, J.D. Reduced cognitive function during a heat wave among residents of non-air-conditioned buildings: An observational study of young adults in the summer of 2016. PLoS Med. 2018, 15, e1002605. [Google Scholar] [CrossRef]
- Schlader, Z.J.; Gagnon, D.; Adams, A.; Rivas, E.; Cullum, C.M.; Crandall, C.G. Cognitive and perceptual responses during passive heat stress in younger and older adults. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 308, R847–R854. [Google Scholar] [CrossRef] [Green Version]
- Mazloumi, A.; Golbabaei, F.; Mahmood Khani, S.; Kazemi, Z.; Hosseini, M.; Abbasinia, M.; Dehghan, S.F. Evaluating Effects of Heat Stress on Cognitive Function among Workers in a Hot Industry. Health Promot. Perspect. 2014, 4, 240–246. [Google Scholar] [CrossRef]
- Kent, S.T.; McClure, L.A.; Crosson, W.L.; Arnett, D.K.; Wadley, V.G.; Sathiakumar, N. Effect of sunlight exposure on cognitive function among depressed and non-depressed participants: A REGARDS cross-sectional study. Environ. Health 2009, 8, 34. [Google Scholar] [CrossRef] [Green Version]
- Kent, S.T.; Kabagambe, E.K.; Wadley, V.G.; Howard, V.J.; Crosson, W.L.; Al-Hamdan, M.Z.; McClure, L.A. The relationship between long-term sunlight radiation and cognitive decline in the REGARDS cohort study. Int. J. Biometeorol. 2014, 58, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Keller, M.; Frederickson, B.; Ybarra, O.; Cote, S.; Johnson, K.; Mikels, J.; Wager, T. A Warm Heart and a Clear Head: The Contingent Effects of Weather on Mood and Cognition. Psychol. Sci. 2005, 16, 724–731. [Google Scholar] [CrossRef]
- Lim, A.S.P.; Gaiteri, C.; Yu, L.; Sohail, S.; Swardfager, W.; Tasaki, S.; Black, S.E. Seasonal plasticity of cognition and related biological measures in adults with and without Alzheimer disease: Analysis of multiple cohorts. PLoS Med. 2018, 15, e1002647. [Google Scholar] [CrossRef] [PubMed]
- Major, S.U.S. Cities with the Most Days of More Than 0.01 Inches of Rainfall per Year between 1981 and 2010. 2011. Available online: https://www-statista-com.proxy.lib.umich.edu/statistics/226747/us-cities-with-the-most-rainy-days/ (accessed on 5 February 2020).
- Klinenberg, E. Heat Wave: A Social Autopsy of Disaster in Chicago; The University of Chicago Press: Chicago, IL, USA, 2002. [Google Scholar]
- Malik, S.; Lee, D.C.; Doran, K.M.; Grudzen, C.R.; Worthing, J.; Portelli, I.; Smith, S.W. Vulnerability of Older Adults in Disasters: Emergency Department Utilization by Geriatric Patients After Hurricane Sandy. Disaster Med. Public Health Prep. 2018, 12, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Gronlund, C.J.; Zanobetti, A.; Schwartz, J.D.; Wellenius, G.A.; O’Neill, M.S. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ. Health Perspect. 2014, 122, 1187–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, P.; Hirsch, J.A.; Melendez, R.; Winters, M.; Sims Gould, J.; Ashe, M.; McKay, H. Snow and Rain Modify Neighbourhood Walkability for Older Adults. Can. J. Aging 2017, 36, 159–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, P.J.; Yan, T.; Keusch, F.; Gallagher, N.A. The Impact of Weather on Mobility and Participation in Older U.S. Adults. Am. J. Public Health 2015, 105, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Hsu, J.A.; Fernie, G. Aging and the use of pedestrian facilities in winter-the need for improved design and better technology. J. Urban Health 2013, 90, 602–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallagher, N.A.; Clarke, P.J.; Ronis, D.L.; Cherry, C.L.; Nyquist, L.; Gretebeck, K.A. Influences on neighborhood walking in older adults. Res. Gerontol. Nurs. 2012, 5, 238–250. [Google Scholar] [CrossRef] [Green Version]
- Rantakokko, M.; Iwarsson, S.; Vahaluoto, S.; Portegijs, E.; Viljanen, A.; Rantanen, T. Perceived environmental barriers to outdoor mobility and feelings of loneliness among community-dwelling older people. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1562–1568. [Google Scholar] [CrossRef] [Green Version]
- Hjorthol, R. Winter weather—An obstacle to older people’s activities? J. Transp. Geogr. 2013, 28, 186–191. [Google Scholar] [CrossRef]
- Finlay, J.M. ‘Walk like a penguin’: Older Minnesotans’ experiences of (non)therapeutic white space. Soc. Sci. Med. 2017, 198, 77–84. [Google Scholar] [CrossRef]
- Howard, V.J.; Cushman, M.; Pulley, L.; Gomez, C.R.; Go, R.C.; Prineas, R.J.; Howard, G. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology 2005, 25, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.A.; Galecki, A.T.; Langa, K.M.; Unverzagt, F.W.; Kabeto, M.U.; Giordani, B.; Wadley, V.G. Trajectory of Cognitive Decline After Incident Stroke. JAMA 2015, 314, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Fillenbaum, G.G.; van Belle, G.; Morris, J.C.; Mohs, R.C.; Mirra, S.S.; Davis, P.C.; Tariot, P.N.; Silverman, J.M.; Clark, C.M.; Welsh-Bohmer, K.A.; et al. Consortium to Establish a Registry for Alzheimer’s Disease (CERAD): The first twenty years. Alzheimer’s Dement. 2008, 4, 96–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, J.C.; Heyman, A.; Mohs, R.C.; Hughes, J.P.; Van Belle, G.; Fillenbaum, G.; Clark, C. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD): Part, I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 1989, 39, 1159. [Google Scholar] [CrossRef]
- Hachinski, V.; Iadecola, C.; Petersen, R.C.; Breteler, M.M.; Nyenhuis, D.L.; Black, S.E.; Vinters, H.V. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 2006, 37, 2220–2241. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. JAGS 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Zhu, W.; Howard, V.J.; Wadley, V.G.; Hutto, B.; Blair, S.N.; Vena, J.E.; Hooker, S.P. Association Between Objectively Measured Physical Activity and Cognitive Function in Older Adults-The Reasons for Geographic and Racial Differences in Stroke Study. J. Am. Geriatr. Soc. 2015, 63, 2447–2454. [Google Scholar] [CrossRef] [Green Version]
- Weuve, J.; Proust-Lima, C.; Power, M.C.; Gross, A.L.; Hofer, S.M.; Thiebaut, R.; MELODEM Initiative. Guidelines for reporting methodological challenges and evaluating potential bias in dementia research. Alzheimer’s Dement. 2015, 11, 1098–1109. [Google Scholar] [CrossRef]
- Wilson, R.S.; Segawa, E.; Boyle, P.A.; Anagnos, S.E.; Hizel, L.P.; Bennett, D.A. The natural history of cognitive decline in Alzheimer’s disease. Psychol. Aging 2012, 27, 1008–1017. [Google Scholar] [CrossRef] [Green Version]
- National Oceanic and Atmospheric Administration. Land-Based Station Data. 2019. Available online: https://www.ncdc.noaa.gov/data-access/land-based-station-data (accessed on 9 January 2020).
- Chen, D.; Chen, H.W. Using the Köppen classification to quantify climate variation and change: An example for 1901–2010. Environ. Dev. 2013, 6, 69–79. [Google Scholar] [CrossRef]
- Singer, J.D.; Willet, J.B. Applied Longitudinal Data Analysis; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Burnham, K.P.; Anderson, D.R. Multimodel Inference: Understanding AIC and BIC in Model Selection. Sociol. Methods Res. 2004, 33, 261–304. [Google Scholar] [CrossRef]
- Pinheiro, J.; Bates, D.; DebRoy, S.; Sarkar, D.; R Core Team. nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-141. 2019. Available online: https://CRAN.R-project.org/package=nlme (accessed on 5 February 2020).
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Leone, M. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Goldberg, M.S.; Gasparrini, A.; Armstrong, B.; Valois, M.F. The short-term influence of temperature on daily mortality in the temperate climate of Montreal, Canada. Environ. Res. 2011, 111, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A. Onebasis. 2019. Available online: https://www.rdocumentation.org/packages/dlnm/versions/2.3.9/topics/onebasis (accessed on 5 February 2020).
- Clarke, P.J.; Ailshire, J.A.; House, J.S.; Morenoff, J.D.; King, K.; Melendez, R.; Langa, K.M. Cognitive function in the community setting: The neighbourhood as a source of ‘cognitive reserve’? J. Epidemiol. Community Health 2012, 66, 730–736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Y.T.; Prina, A.M.; Jones, A.P.; Barnes, L.E.; Matthews, F.E.; Brayne, C. Community environment, cognitive impairment and dementia in later life: Results from the Cognitive Function and Ageing Study. Age Ageing 2015, 44, 1005–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Keijzer, C.; Gascon, M.; Nieuwenhuijsen, M.J.; Dadvand, P. Long-Term Green Space Exposure and Cognition Across the Life Course: A Systematic Review. Curr. Environ. Health Rep. 2016, 3, 468–477. [Google Scholar] [CrossRef]
- Besser, L.M.; McDonald, N.C.; Song, Y.; Kukull, W.A.; Rodriguez, D.A. Neighborhood Environment and Cognition in Older Adults: A Systematic Review. Am. J. Prev. Med. 2017, 53, 241–251. [Google Scholar] [CrossRef] [Green Version]
- Besser, L.M.; Rodriguez, D.A.; McDonald, N.; Kukull, W.A.; Fitzpatrick, A.L.; Rapp, S.R.; Seeman, T. Neighborhood built environment and cognition in non-demented older adults: The Multi-Ethnic Study of Atherosclerosis. Soc. Sci. Med. 2018, 200, 27–35. [Google Scholar] [CrossRef]
- Besser, L.; Galvin, J.E.; Rodriguez, D.; Seeman, T.; Kukull, W.; Rapp, S.R.; Smith, J. Associations between neighborhood built environment and cognition vary by apolipoprotein E genotype: Multi-Ethnic Study of Atherosclerosis. Health Place 2019, 60, 102188. [Google Scholar] [CrossRef]
- Cerin, E. Building the evidence for an ecological model of cognitive health. Health Place 2019, 60. [Google Scholar] [CrossRef]
- Finlay, J.; Esposito, M.; Tang, S.; Gomez-Lopez, I.; Sylvers, D.; Judd, S.; Clarke, P. Fast-food for thought: Retail food environments as resources for cognitive health and wellbeing among aging Americans? Health Place 2020, 64, 102379. [Google Scholar] [CrossRef]
- Read, S.; Comas-Herrera, A.; Grundy, E. Social Isolation and Memory Decline in Later-life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 367–376. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerland, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Cooper, C. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef] [Green Version]
- Ardon-Dryer, K.; Huang, Y.W.; Cziczo, D.J. Laboratory studies of collection efficiency of sub-micrometer aerosol particles by cloud droplets on a single-droplet basis. Atmos. Chem. Phys. 2015, 15, 9159–9171. [Google Scholar] [CrossRef] [Green Version]
- Feng, X.; Wang, S. Influence of different weather events on concentrations of particulate matter with different sizes in Lanzhou, China. J. Environ. Sci. 2011, 24, 665–674. [Google Scholar] [CrossRef]
- Shukla, J.B.; Misra, A.K.; Sundar, S.; Naresh, R. Effect of rain on removal of a gaseous pollutant and two different particulate matters from the atmosphere of a city. Math. Comput. Model. 2008, 48, 832–844. [Google Scholar] [CrossRef]
- Finlay, J.; Franke, T.; McKay, H.; Sims-Gould, J. Therapeutic landscapes and wellbeing in later life: Impacts of blue and green spaces for older adults. Health Place 2015, 34, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Killin, L.O.; Starr, J.M.; Shiue, I.J.; Russ, T.C. Environmental risk factors for dementia: A systematic review. BMC Geriatr. 2016, 16, 175. [Google Scholar] [CrossRef] [Green Version]
- Baumgart, M.; Snyder, H.M.; Carrillo, M.C.; Fazio, S.; Kim, H.; Johns, H. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimer’s Dement. 2015, 11, 718–726. [Google Scholar] [CrossRef] [Green Version]
- Schoenbaum, M.; Butler, B.; Kataoka, S.; Norquist, G.; Springgate, B.; Sullivan, G.; Wells, K. Promoting Mental Health Recovery After Hurricanes Katrina and Rita. Arch. Gen. Psychiatry 2009, 66, 906–914. [Google Scholar] [CrossRef]
- Kessler, R.C.; Galea, S.; Gruber, M.J.; Sampson, N.A.; Ursano, R.J.; Wessely, S. Trends in mental illness and suicidality after Hurricane Katrina. Mol. Psychiatry 2008, 13, 374–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heid, A.R.; Pruchno, R.; Cartwright, F.P.; Wilson-Genderson, M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment. Health 2017, 21, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Long, D.L.; Howard, G.; Long, D.M.; Judd, S.; Manly, J.J.; McClure, L.A.; Glymour, M.M. An Investigation of Selection Bias in Estimating Racial Disparity in Stroke Risk Factors. Am. J. Epidemiol. 2019, 188, 587–597. [Google Scholar] [CrossRef] [PubMed]
- USGCRP. Climate Science Special Report: Fourth National Climate Assessment; USGCRP: Washington, DC, USA, 2017; Volume I.


| (Mean ± SD or %) | |
|---|---|
| Cognitive health factor score (baseline) | 0.0009 ± 2.34 |
| Age (years) at baseline assessment | 64.38 ± 8.71 |
| Year of Baseline interview | |
| 2003 | 18.23% |
| 2004 | 31.25% |
| 2005 | 22.61% |
| 2006 | 16.20% |
| 2007 | 11.71% |
| Black | 39.23% |
| Female | 56.16% |
| Education | |
| Less than high school | 10.84% |
| High school | 25.58% |
| Some college | 26.90% |
| College or more | 36.63% |
| Precipitation percent of days in past year | 30.99 ± 9.05 |
| Köppen climate region at baseline residence | |
| Dry | 2.21% |
| Continental | 24.32% |
| Tropical | 65.76% |
| Mediterranean/Oceanic | 7.71% |
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Unconditional Growth Model | + Precipitation | + Covariates | |
| Fixed Effects | Beta (SE) | Beta (SE) | Beta (SE) |
| Intercept | −5.99 (0.40) *** | −5.27 (0.59) *** | −5.39 (0.57) *** |
| Precipitation (% days in past year) ¶ | |||
| 19% of days in past year | 0.04 (0.02) * | −0.04 (0.02) * | |
| 41% of days in past year | 0.09 (0.01) * | 0.05 (0.01) * | |
| Black (ref White) | 1.05 (0.02) *** | ||
| Female (ref Male) | −0.33 (0.02) *** | ||
| Education (ref College or More) | |||
| Less than High School | −2.00 (0.04) *** | ||
| High School | −1.33 (0.02) *** | ||
| Some College | −0.78 (0.02) *** | ||
| Baseline Interview Year (ref 2003) | |||
| 2004 | 0.09 (0.03) ** | ||
| 2005 | 0.10 (0.03) ** | ||
| 2006 | 0.18 (0.04) *** | ||
| 2007 | 0.17 (0.04) *** | ||
| Köppen Climate Regions (ref Dry) | |||
| Continental | 0.12 (0.08) | ||
| Mediterranean/Oceanic | 0.12 (0.07) | ||
| Tropical | −0.25 (0.07) *** | ||
| Rate of Change | |||
| Age (years) | 0.26 (0.01) *** | 0.25 (0.01) *** | 0.25 (0.01) *** |
| Age2 | −0.002 (0.0001) *** | −0.002 (0.0001) *** | −0.002 (0.0001) *** |
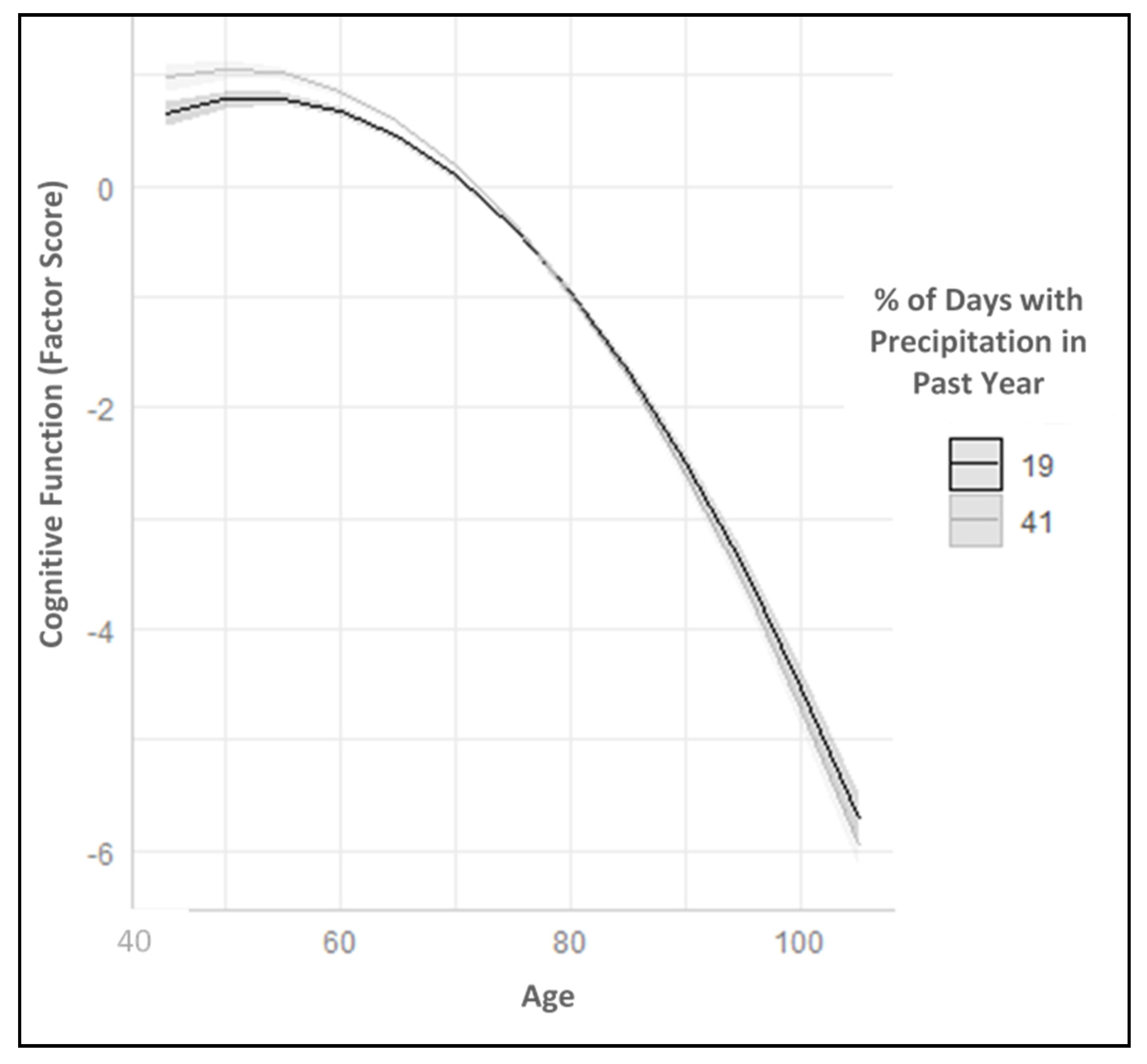
| Age (80 years) × Precipitation (19% days) § | 0.07 (0.02) * | 0.07 (0.02) * | |
| Age (80 years) × Precipitation (41% days) § | −0.04 (0.01) * | −0.03 (0.01) * | |
| Age (60 years) × Precipitation (19% days) § | −0.07 (0.02) * | −0.07 (0.02) * | |
| Age (60 years) × Precipitation (41% days) § | 0.04 (0.01) * | 0.03 (0.01) * | |
| Random Effects | |||
| Intercept | 2.096 | 2.072 | 2.614 |
| Slope (Age) | 0.028 | 0.028 | 0.045 |
| Slope (Age2) | 0.001 | 0.001 | 0.000 |
| Residual | 1.308 | 1.295 | 1.296 |
| Goodness of Fit Statistics | |||
| AIC | 347,347.4 | 347,242.5 | 339,931.3 |
| BIC | 347,450.4 | 347,401.8 | 340,203.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Finlay, J.; Khan, A.; Gronlund, C.; Sol, K.; Jang, J.; Melendez, R.; Judd, S.; Clarke, P. Weather Woes? Exploring Potential Links between Precipitation and Age-Related Cognitive Decline. Int. J. Environ. Res. Public Health 2020, 17, 9011. https://doi.org/10.3390/ijerph17239011
Finlay J, Khan A, Gronlund C, Sol K, Jang J, Melendez R, Judd S, Clarke P. Weather Woes? Exploring Potential Links between Precipitation and Age-Related Cognitive Decline. International Journal of Environmental Research and Public Health. 2020; 17(23):9011. https://doi.org/10.3390/ijerph17239011
Chicago/Turabian StyleFinlay, Jessica, Anam Khan, Carina Gronlund, Ketlyne Sol, Joy Jang, Robert Melendez, Suzanne Judd, and Philippa Clarke. 2020. "Weather Woes? Exploring Potential Links between Precipitation and Age-Related Cognitive Decline" International Journal of Environmental Research and Public Health 17, no. 23: 9011. https://doi.org/10.3390/ijerph17239011





