Peri-Implant Surgical Treatment Downregulates the Expression of sTREM-1 and MMP-8 in Patients with Peri-Implantitis: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Peri-Implant Treatment
2.3. Saliva Collection
2.4. sTREM-1, PGLYRP1, MMP-8, and TIMP-1 Immunoassays
2.5. Statistical Analysis
3. Results
3.1. Demographics and Clinical Parameters
3.2. Salivary Parameters
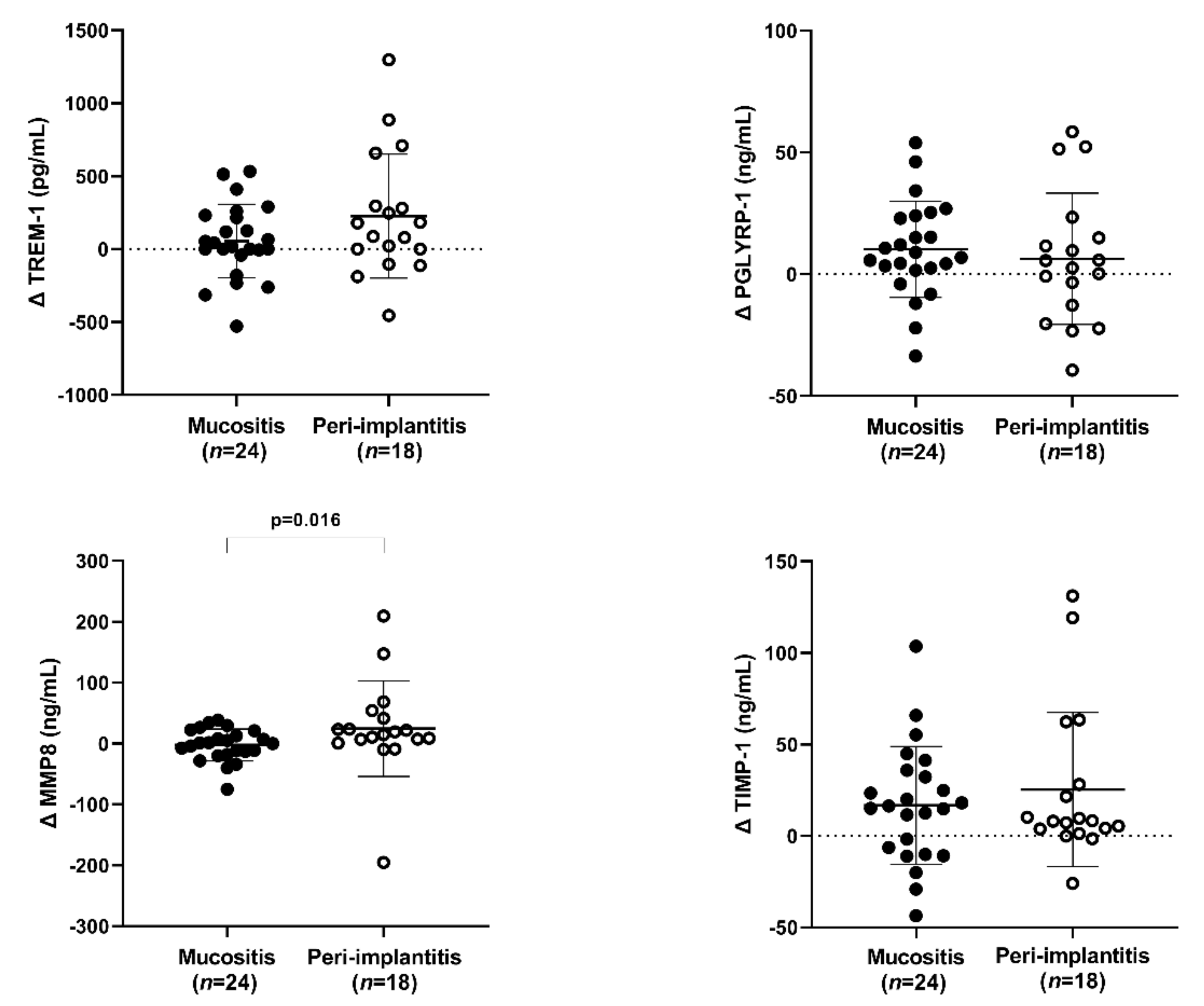
3.2.1. The Variation between before and after (Delta)
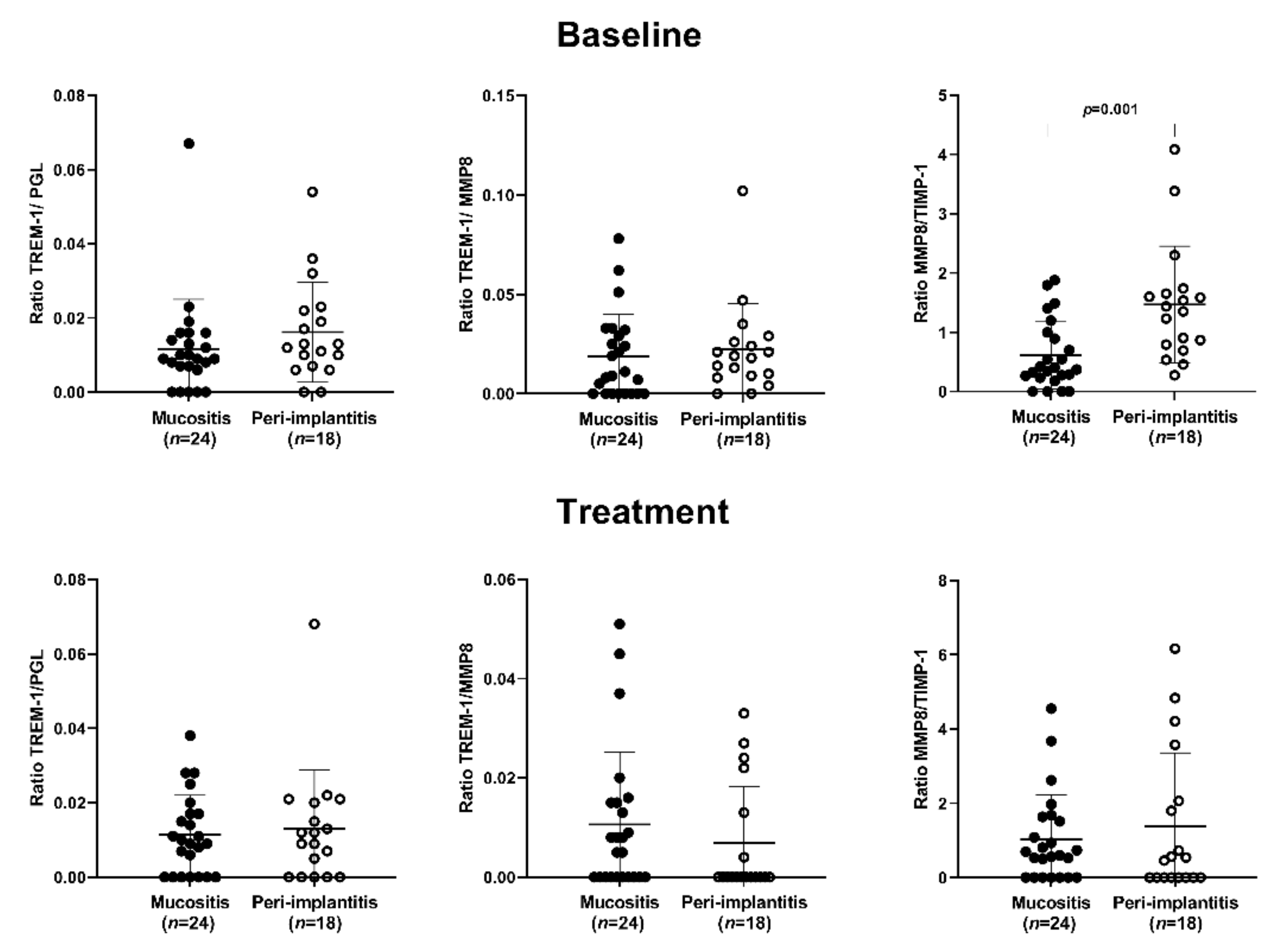
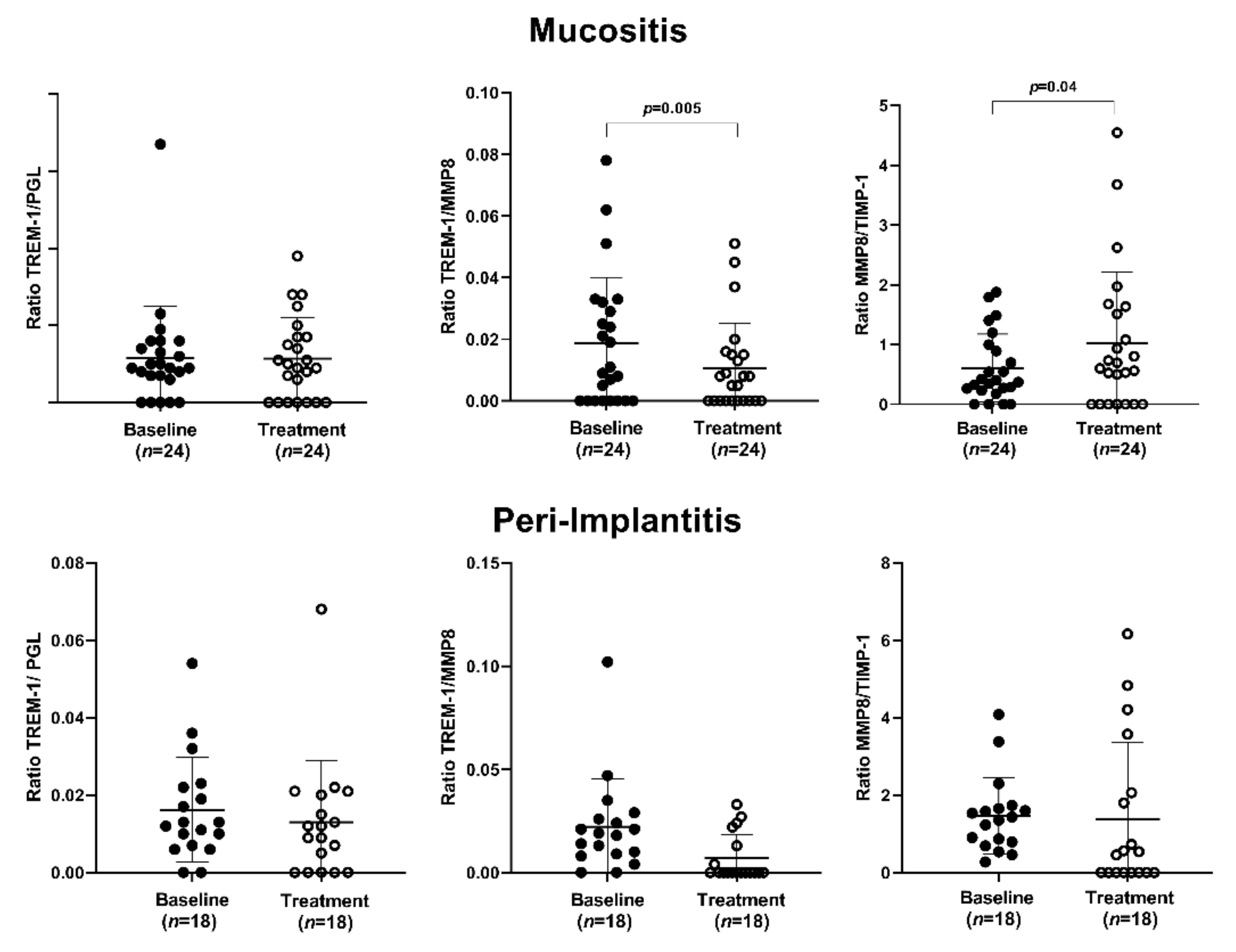
3.2.2. The Ratio Analysis
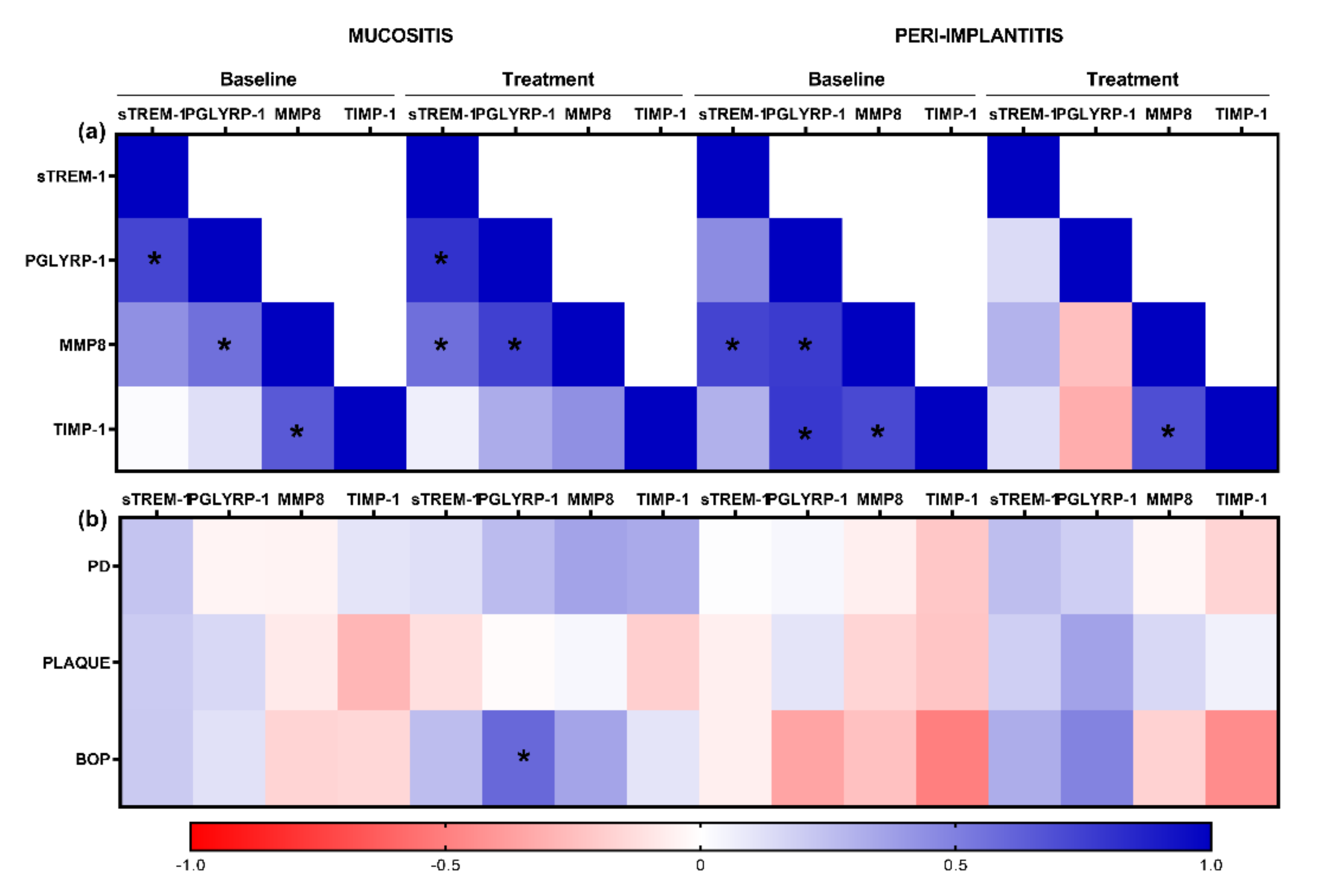
3.2.3. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.A.; Salvi, G.E. Peri-implant mucositis. J. Clin. Periodontol. 2018, 45, S237–S245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Clin. Periodontol. 2018, 45, S246–S266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Derks, J.; Tomasi, C. Peri-implant health and disease. A systematic review of current epidemiology. J. Clin. Periodontol. 2015, 42, S158–S171. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, W.; Zhang, L.; Yan, X.; Shi, D.; Meng, H. A nomogram prediction of peri-implantitis in treated severe periodontitis patients: A 1-5-year prospective cohort study. Clin. Implant. Dent. Relat. Res. 2018, 20, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.H.; Wang, H.L. Breaking the wave of peri-implantitis. Periodontol. 2000 2020, 84, 145–160. [Google Scholar] [CrossRef]
- Berglundh, T.; Zitzmann, N.; Donati, M. Are peri-implantitis lesions different from periodontitis lesions? J. Clin. Periodontol. 2011, 38, 188–202. [Google Scholar] [CrossRef]
- Berglundh, T.; Gislason, O.; Lekholm, U.; Sennerby, L.; Lindhe, J. Histopathological observations of human periimplantitis lesions. J. Clin. Periodontol. 2004, 31, 341–347. [Google Scholar] [CrossRef]
- Nguyen Vo, T.N.; Hao, J.; Chou, J.; Oshima, M.; Aoki, K.; Kuroda, S.; Kaboosaya, B.; Kasugai, S. Ligature induced peri-implantitis: Tissue destruction and inflammatory progression in a murine model. Clin. Oral. Implant. Res. 2017, 28, 129–136. [Google Scholar] [CrossRef]
- Bleharski, J.R.; Kiessler, V.; Buonsanti, C.; Sieling, P.A.; Stenger, S.; Colonna, M.; Modlin, R.L. A role for triggering receptor expressed on myeloid cells-1 in host defense during the early-induced and adaptive phases of the immune response. J. Immunol. 2003, 170, 3812–3818. [Google Scholar] [CrossRef]
- Bouchon, A.; Dietrich, J.; Colonna, M. Cutting edge: Inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes. J. Immunol. 2000, 164, 4991–4995. [Google Scholar] [CrossRef] [PubMed]
- Varanat, M.; Haase, E.M.; Kay, J.G.; Scannapieco, F.A. Activation of the TREM-1 pathway in human monocytes by periodontal pathogens and oral commensal bacteria. Mol. Oral. Microbiol. 2017, 32, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Piña, V.; Soares-Schanoski, A.; Rodríguez-Rojas, A.; Del Fresno, C.; García, F.; Vallejo-Cremades, M.T.; Fernández-Ruiz, I.; Arnalich, F.; Fuentes-Prior, P.; López-Collazo, E. Metalloproteinases shed TREM-1 ectodomain from lipopolysaccharide-stimulated human monocytes. J. Immunol. 2007, 179, 4065–4073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, G.; Lai, C.; Fife, M.E.; Grabiec, A.M.; Tildy, B.; Snelgrove, R.J.; Xin, G.; Lloyd, C.M.; Hussell, T. Reversal of TREM-1 ectodomain shedding and improved bacterial clearance by intranasal metalloproteinase inhibitors. Mucosal. Immunol. 2017, 10, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Bostanci, N.; Oztürk, V.; Emingil, G.; Belibasakis, G.N. Elevated oral and systemic levels of soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) in periodontitis. J. Dent. Res. 2013, 92, 161–165. [Google Scholar] [CrossRef] [Green Version]
- Bisson, C.; Massin, F.; Lefevre, P.A.; Thilly, N.; Miller, N.; Gibot, S. Increased gingival crevicular fluid levels of soluble triggering receptor expressed on myeloid cells (sTREM)-1 in severe periodontitis. J. Clin. Periodontol. 2012, 39, 1141–1148. [Google Scholar] [CrossRef]
- Belibasakis, G.N.; Öztürk, V.; Emingil, G.; Bostanci, N. Soluble triggering receptor expressed on myeloid cells 1 (sTREM-1) in gingival crevicular fluid: Association with clinical and microbiologic parameters. J. Periodontol. 2014, 85, 204–210. [Google Scholar] [CrossRef]
- Dubar, M.; Frippiat, J.P.; Remen, T.; Boufenzer, A.; Alauzet, C.; Baumann, C.; Gibot, S.; Bisson, C. Comparison of sTREM-1 and associated periodontal and bacterial factors before/after periodontal therapy, and impact of psychosocial factors. J. Clin. Periodontol. 2020, 47, 1064–1078. [Google Scholar] [CrossRef]
- Bostanci, N.; Abe, T.; Belibasakis, G.N.; Hajishengallis, G. TREM-1 Is Upregulated in Experimental Periodontitis, and Its Blockade Inhibits IL-17A and RANKL Expression and Suppresses Bone loss. J. Clin. Med. 2019, 1, 1579. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, M.K.S.; Lira-Junior, R.; Lourenço, E.J.V.; Telles, D.M.; Boström, E.A.; Figueredo, C.M.; Bostanci, N. The modulation of the TREM-1/PGLYRP1/MMP-8 axis in peri-implant diseases. Clin. Oral. Investig. 2020, 24, 1837–1844. [Google Scholar] [CrossRef]
- Royet, J.; Dziarski, R. Peptidoglycan recognition proteins: Pleiotropic sensors and effectors of antimicrobial defenses. Nat. Rev. Microbiol. 2007, 5, 264–277. [Google Scholar] [CrossRef]
- Dziarski, R.; Gupta, D. Review: Mammalian peptidoglycan recognition proteins (PGRPs) in innate immunity. Innate. Immun. 2010, 16, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Read, C.B.; Kuijper, J.L.; Hjorth, S.A.; Heipel, M.D.; Tang, X.; Fleetwood, A.J.; Dantzler, J.L.; Grell, S.N.; Kastrup, J.; Wang, C.; et al. Cutting Edge: Identification of neutrophil PGLYRP1 as a ligand for TREM-1. J. Immunol. 2015, 15, 1417–1421. [Google Scholar] [CrossRef] [PubMed]
- Nylund, K.M.; Ruokonen, H.; Sorsa, T.; Heikkinen, A.M.; Meurman, J.H.; Ortiz, F.; Tervahartiala, T.; Furuholm, J.; Bostanci, N. Association of the Salivary Triggering Receptor Expressed on Myeloid Cells/its Ligand Peptidoglycan Recognition Protein 1 Axis With Oral Inflammation in Kidney Disease. J. Periodontol. 2017, 28, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Smeets, R.; Henningsen, A.; Jung, O.; Heiland, M.; Hammächer, C.; Stein, J.M. Definition, etiology, prevention and treatment of peri-implantitis—A review. Head Face Med. 2014, 10, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindhe, J.; Meyle, J.; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [Green Version]
- Crespi, R.; Marconcini, S.; Crespi, G.; Giammarinaro, E.; Menchini Fabris, G.B.; Barone, A.; Covani, U. Nonsurgical Treatment of Peri-implantitis Without Eliminating Granulation Tissue: A 3-Year Study. Implant. Dent. 2019, 28, 4–10. [Google Scholar] [CrossRef]
- Valderrama, P.; Wilson, T.G., Jr. Detoxification of implant surfaces affected by peri-implant disease: An overview of surgical methods. Int. J. Dent. 2013, 2013, 740680. [Google Scholar] [CrossRef] [Green Version]
- Bhavsar, I.; Miller, C.S.; Ebersole, J.L.; Dawson, D.R., 3rd; Thompson, K.L.; Al-Sabbagh, M. Biological response to peri-implantitis treatment. J. Periodontal. Res. 2019, 54, 720–728. [Google Scholar] [CrossRef]
- Duarte, P.M.; de Mendonça, A.C.; Máximo, M.B.; Santos, V.R.; Bastos, M.F.; Nociti, F.H. Effect of anti-infective mechanical therapy on clinical parameters and cytokine levels in human peri-implant diseases. J. Periodontol. 2009, 80, 234–243. [Google Scholar] [CrossRef]
- Renvert, S.; Widen, C.; Persson, R.G. Cytokine and microbial profiles in relation to the clinical outcome following treatment of peri-implantitis. Clin. Oral. Implant. Res. 2017, 28, 1127–1132. [Google Scholar] [CrossRef] [PubMed]
- de Mello-Neto, J.M.; Teixeira, M.K.S.; Teixeira, G.S.; Lourenço, E.J.V.; Telles, D.M.; Lira-Junior, R.; Ipe, D.; Nair, R.G.; Boström, E.A.; Figueredo, C.M. Peri-implant treatment reduces the salivary levels of Colony stimulator factor-1 and S100A8/A9. Odontology 2021, 109, 540–546. [Google Scholar] [CrossRef]
- Albrektsson, T.; Jansson, T.; Lekholm, U. Osseointegrated dental implants. Dent Clin. N. Am. 1986, 30, 151–174. [Google Scholar]
- Hentenaar, D.F.M.; De Waal, Y.C.M.; Vissink, A.; Van Winkelhoff, A.J.; Meijer, H.J.A.; Liefers, S.C.; Kroese, F.G.M.; Raghoebar, G.M. Biomarker levels in peri-implant crevicular fluid of healthy implants, untreated and non-surgically treated implants with peri-implantitis. J. Clin. Periodontol. 2021, 48, 590–601. [Google Scholar] [CrossRef] [PubMed]
- Ziebolz, D.; Schmalz, G.; Gollasch, D.; Eickholz, P.; Rinke, S. Microbiological and aMMP-8 findings depending on peri-implant disease in patients undergoing supportive implant therapy. Diagn. Microbiol. Infect. Dis. 2017, 88, 47–52. [Google Scholar] [CrossRef]
- Sorsa, T.; Gursoy, U.K.; Nwhator, S.; Hernandez, M.; Tervahartiala, T.; Leppilahti, J.; Gursoy, M.; Könönen, E.; Emingil, G.; Pussinen, P.J.; et al. Analysis of matrix metalloproteinases, especially MMP-8, in gingival creviclular fluid, mouthrinse and saliva for monitoring periodontal diseases. Periodontol. 2000. 2016, 70, 142–163. [Google Scholar] [CrossRef] [PubMed]
- Costa-Junior, F.R.; Alvim-Pereira, C.C.; Alvim-Pereira, F.; Trevilatto, P.C.; de Souza, A.P.; Santos, M.C. Influence of MMP-8 promoter polymorphism in early osseointegrated implant failure. Clin. Oral. Investig. 2013, 17, 311–316. [Google Scholar] [CrossRef]
- Ramseier, C.A.; Eick, S.; Brönnimann, C.; Buser, D.; Brägger, U.; Salvi, G.E. Host-Derived Biomarkers at Teeth and Implants in Partially Edentulous Patients. A 10-Year Retrospective Study. Clin. Oral. Implant. Res. 2016, 27, 211–217. [Google Scholar] [CrossRef]
- Rudick, C.P.; Miyamoto, T.; Lang, M.S.; Agrawal, D.K. Triggering receptor expressed on myeloid cells in the pathogenesis of periodontitis: Potential novel treatment strategies. Expert Rev. Clin. Immunol. 2017, 13, 1189–1197. [Google Scholar] [CrossRef]
- Arakawa, H.; Uehara, J.; Hara, E.S.; Sonoyama, W.; Kimura, A.; Kanyama, M.; Matsuka, Y.; Kuboki, T. Matrix metalloproteinase-8 is the major potential collagenase in active peri-implantitis. J. Prosthodont. Res. 2012, 56, 249–255. [Google Scholar] [CrossRef] [Green Version]
- Hiyari, S.; Naghibi, A.; Wong, R.; Sadreshkevary, R.; Yi-Ling, L.; Tetradis, S.; Camargo, P.M.; Pirih, F.Q. Susceptibility of different mouse strains to peri-implantitis. J. Periodontal Res. 2018, 53, 107–116. [Google Scholar] [CrossRef]
- Silbereisen, A.; Hallak, A.K.; Nascimento, G.G.; Sorsa, T.; Belibasakis, G.N.; Lopez, R.; Bostanci, N. Regulation of PGLYRP1 and TREM-1 during Progression and Resolution of Gingival Inflammation. JDR Clin. Trans. Res. 2019, 4, 352–359. [Google Scholar] [CrossRef]
- Äyräväinen, L.; Heikkinen, A.M.; Kuuliala, A.; Ahola, K.; Koivuniemi, R.; Moilanen, E.; Hämäläinen, M.; Tervahartiala, T.; Meurman, J.H.; Leirisalo-Repo, M.; et al. Anti-rheumatic medication and salivary MMP-8, a biomarker for periodontal disease. Oral. Dis. 2018, 24, 1562–1571. [Google Scholar] [CrossRef]
- Górska, R.; Nedzi-Góra, M. The effects of the initial treatment phase and of adjunctive low-dose doxycycline therapy on clinical parameters and MMP-8, MMP-9, and TIMP-1 levels in the saliva and peripheral blood of patients with chronic periodontitis. Arch. Immunol. Exp. 2006, 54, 419–426. [Google Scholar] [CrossRef]
- Fenol, A.; Peter, M.R.; Perayil, J.; Vyloppillil, R.; Bhaskar, A. Comparison of Salivary TIMP-1 Levels in Periodontally Involved and Healthy Controls and the Response to Nonsurgical Periodontal Therapy. Int. J. Chronic Dis. 2014, 2014, 363581. [Google Scholar] [CrossRef] [PubMed]
- Marcaccini, A.M.; Meschiari, C.A.; Zuardi, L.R.; de Sousa, T.S.; Taba, M., Jr.; Teofilo, J.M.; Jacob-Ferreira, A.L.; Tanus-Santos, J.E.; Novaes, A.B., Jr.; Gerlach, R.F. Gingival crevicular fluid levels of MMP-8, MMP-9, TIMP-2, and MPO decrease after periodontal therapy. J. Clin. Periodontol. 2010, 37, 180–190. [Google Scholar] [CrossRef]
- İnce, G.; Gürsoy, H.; İpçi, Ş.D.; Cakar, G.; Emekli-Alturfan, E.; Yılmaz, S. Clinical and Biochemical Evaluation of Lozenges Containing Lactobacillus reuteri as an Adjunct to Nonsurgical Periodontal Therapy in Chronic Periodontitis. J. Periodontol. 2015, 86, 746–754. [Google Scholar] [CrossRef]
- Raeeszadeh-Sarmazdeh, M.; Do, L.D.; Hritz, B.G. Metalloproteinases and Their Inhibitors: Potential for the Development of New Therapeutics. Cells 2020, 25, 1313. [Google Scholar] [CrossRef]
- Barootchi, S.; Ravidà, A.; Tavelli, L.; Wang, H.L. Nonsurgical treatment for peri-implant mucositis: A systematic review and meta-analysis. Int. J. Oral. Implantol. 2020, 13, 123–139. [Google Scholar]
- Roccuzzo, M.; Layton, D.M.; Roccuzzo, A.; Heitz-Mayfield, L.J. Clinical outcomes of peri-implantitis treatment and supportive care: A systematic review. Clin. Oral. Implant. Res. 2018, 29, 331–350. [Google Scholar] [CrossRef]
- Zhang, Y.; Sun, J.; Lin, C.C.; Abemayor, E.; Wang, M.B.; Wong, D.T. The emerging landscape of salivary diagnostics. Periodontol. 2000. 2016, 70, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Rathnayake, N.; Gieselmann, D.R.; Heikkinen, A.M.; Tervahartiala, T.; Sorsa, T. Salivary Diagnostics-Point-of-Care diagnostics of MMP-8 in dentistry and medicine. Diagnostics 2017, 20, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kc, S.; Wang, X.Z.; Gallagher, J.E. Diagnostic sensitivity and specificity of host-derived salivary biomarkers in periodontal disease amongst adults: Systematic review. J. Clin. Periodontol. 2020, 47, 289–308. [Google Scholar] [CrossRef] [PubMed]
- Diesch, T.; Filippi, C.; Fritschi, N.; Filippi, A.; Ritz, N. Cytokines in saliva as biomarkers of oral and systemic oncological or infectious diseases: A systematic review. Cytokine 2021, 143, 155506. [Google Scholar] [CrossRef]

| Mucositis (n = 24) | Peri-Implantitis (n = 18) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Baseline | p1 | 3 Months | p2 | Baseline | p3 | 3 Months | p4 |
| Peri-implant parameters | ||||||||
| Mean PPD | 3.8 (0.7) | 0.002 | 3.1 (0.9) | <0.001 | 5.04 (1.0) | 0.005 | 4.0 (1.2) | 0.016 |
| % Plaque | 74.3 (33.0) | 0.019 | 49.1 (36.6) | 0.726 | 70.3(33.1) | 0.017 | 35.1 (47.8) | 0.154 |
| % BOP | 88.2 (21.7) | 0.001 | 47 (38.9) | 0.489 | 93.44 (15.4) | 0.004 | 49.0 (42.5) | 0.906 |
| Full mouth periodontal parameters | ||||||||
| Mean PPD | 2.3 (0.3) | 0.001 | 2.1 (0.3) | 0.006 | 2.6 (0.3) | <0.001 | 2.3 (0.3) | 0.021 |
| Mean CAL | 1.5 (1.0) | 0.617 | 1.5 (0.9) | 0.431 | 1.6 (0.8) | 0.571 | 1.6 (0.8) | 0.263 |
| % Plaque | 80.2(16.3) | 0.010 | 69.2 (20.5) | 0.060 | 68.6 (19.7) | 0.218 | 61.4 (27.1) | 0.237 |
| % BOP | 52 (22.6) | <0.001 | 35.4 (21.9) | 0.303 | 58.2 (21.8) | 0.002 | 34.6 (20.8) | 0.970 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teixeira Neves, G.S.; Elangovan, G.; Teixeira, M.K.S.; Mello-Neto, J.M.d.; Tadakamadla, S.K.; Lourenço, E.J.V.; Telles, D.M.; Figueredo, C.M. Peri-Implant Surgical Treatment Downregulates the Expression of sTREM-1 and MMP-8 in Patients with Peri-Implantitis: A Prospective Study. Int. J. Environ. Res. Public Health 2022, 19, 3627. https://doi.org/10.3390/ijerph19063627
Teixeira Neves GS, Elangovan G, Teixeira MKS, Mello-Neto JMd, Tadakamadla SK, Lourenço EJV, Telles DM, Figueredo CM. Peri-Implant Surgical Treatment Downregulates the Expression of sTREM-1 and MMP-8 in Patients with Peri-Implantitis: A Prospective Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3627. https://doi.org/10.3390/ijerph19063627
Chicago/Turabian StyleTeixeira Neves, Glaucia Schuindt, Gayathiri Elangovan, Mayla Kezy Silva Teixeira, João Martins de Mello-Neto, Santosh Kumar Tadakamadla, Eduardo José Veras Lourenço, Daniel Moraes Telles, and Carlos Marcelo Figueredo. 2022. "Peri-Implant Surgical Treatment Downregulates the Expression of sTREM-1 and MMP-8 in Patients with Peri-Implantitis: A Prospective Study" International Journal of Environmental Research and Public Health 19, no. 6: 3627. https://doi.org/10.3390/ijerph19063627






