Occupation-Induced Fatigue and Impacts on Emergency First Responders: A Systematic Review
Abstract
:1. Introduction
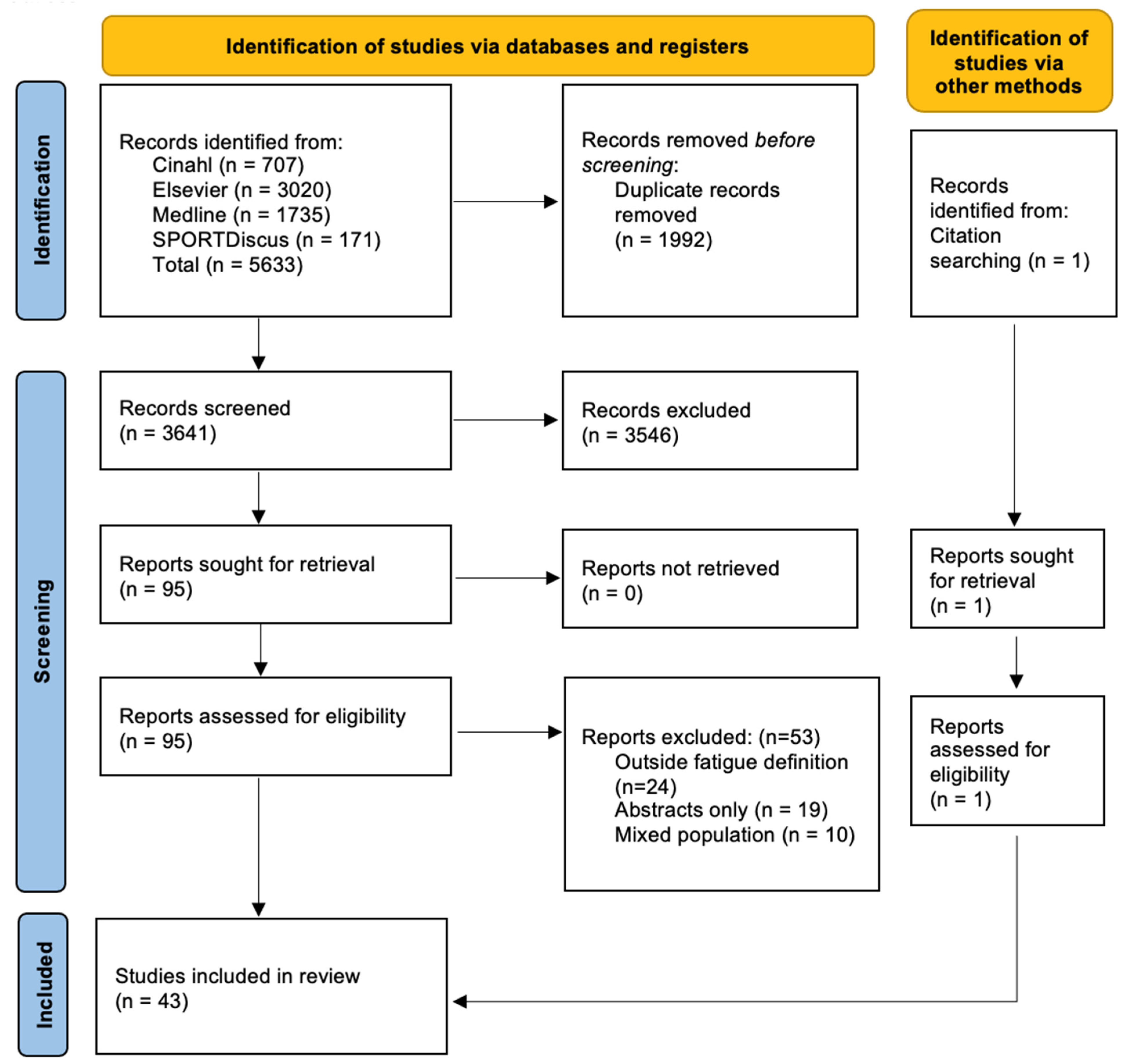
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy and Selection
2.4. Outcome Measures and Synthesis Methods
2.5. Risk of Bias Assessment
2.6. Effect Measures
3. Results
3.1. Risk of Bias
3.2. Outcome Measures of Fatigue
3.3. Direct Contributors
3.3.1. Sleep Practices
3.3.2. Fatigue Questionnaires and Interviews
3.3.3. Physiological Measurements
3.3.4. Cognitive Reaction Test
3.3.5. Self-Rated Measures
3.3.6. Physical Activity
3.3.7. Workload and Safety
3.3.8. Balance and Strength
3.4. Indirect Contributors
3.4.1. Mental Health
3.4.2. Recovery Practices
4. Discussion
4.1. Outcome Measures for Fatigue Assessment
4.2. Causes of Fatigue
4.3. Impacts of Fatigue
4.4. Fatigue Mitigation Strategies
4.4.1. Shift Cycles
4.4.2. Sleep Hygiene
4.4.3. Cold Water Immersion
4.4.4. Exercise
4.5. Strengths and Limitations
4.6. Implications for Practice and Policy
4.7. Future Research
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Arble, E.; Arnetz, B.B. A Model of First-responder Coping: An Approach/Avoidance Bifurcation. Stress Health 2017, 33, 223–232. [Google Scholar] [CrossRef]
- Jones, S. Describing the Mental Health Profile of First Responders—A Systematic Review. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 200–214. [Google Scholar] [CrossRef] [PubMed]
- Billings, J.; Focht, W. Firefighter Shift Schedules Affect Sleep Quality. J. Occup. Environ. Med. 2016, 58, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.L.; Sinden, K.E.; MacPhee, R.S.; Ottawa Paramedic Service Research Team. Identifying the critical physical demanding tasks of paramedic work: Towards the development of a physical employment standard. Appl. Ergon. 2017, 65, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Sofianopoulos, S.; Williams, B.; Archer, F. Paramedics and the effects of shift work on sleep: A literature review. Emerg. Med. J. 2012, 29, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Higgins, J.S.; Van Dongen, H.P.A.; Buysse, D.J.; Thackery, R.W.; Kupas, D.F.; Becker, D.S.; Dean, B.E.; Lindbeck, G.H.; Guyette, F.X.; et al. Evidence-Based Guidelines for Fatigue Risk Management in Emergency Medical Services. Prehosp. Emerg. Care 2018, 22, 89–101. [Google Scholar] [CrossRef]
- Yung, M.; Du, B.; Gruber, J.; Yazdani, A. Developing a Canadian fatigue risk management standard for first responders: Defining the scope. Saf. Sci. 2021, 134, 105044. [Google Scholar] [CrossRef]
- Dawson, D.; Ferguson, S.A.; Vincent, G.E. Safety implications of fatigue and sleep inertia for emergency services personnel. Sleep Med. Rev. 2021, 55, 101386. [Google Scholar] [CrossRef]
- Corrigan, S.L.; Roberts, S.; Warmington, S.; Drain, J.; Main, L.C. Monitoring stress and allostatic load in first responders and tactical operators using heart rate variability: A systematic review. BioMed Cent. Public Health 2021, 21, 1701. [Google Scholar] [CrossRef]
- Satterfield, B.C.; Van Dongen, H.P.A. Occupational fatigue, underlying sleep and circadian mechanisms, and approaches to fatigue risk management. Fatigue: Biomed. Health Behav. 2013, 1, 118–136. [Google Scholar] [CrossRef]
- Enoka, R.M.; Duchateau, J. Translating Fatigue to Human Performance. Med. Sci. Sports Exerc. 2016, 48, 2228–2238. [Google Scholar] [CrossRef] [PubMed]
- Gurubhagavatula, I.; Barger, L.K.; Barnes, C.M.; Basner, M.; Boivin, D.B.; Dawson, D.; Drake, C.L.; Flynn-Evans, E.E.; Mysliwiec, V.; Patterson, P.D.; et al. Guiding principles for determining work shift duration and addressing the effects of work shift duration on performance, safety, and health: Guidance from the American Academy of Sleep Medicine and the Sleep Research Society. J. Clin. Sleep Med. 2021, 17, 2283–2306. [Google Scholar] [CrossRef]
- Ferris, M.; Bowles, K.A.; Bray, M.; Bosley, E.; Rajaratnam, S.M.W.; Wolkow, A.P. The impact of shift work schedules on PVT performance in naturalistic settings: A systematic review. Int. Arch. Occup. Environ. Health 2021, 94, 1475–1494. [Google Scholar] [CrossRef] [PubMed]
- Fullagar, H.H.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and athletic performance: The effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015, 45, 161–186. [Google Scholar] [CrossRef]
- Park, S.; Hong, H.; Kim, R.Y.; Ma, J.; Lee, S.; Ha, E.; Yoon, S.; Kim, J. Firefighters Have Cerebral Blood Flow Reductions in the Orbitofrontal and Insular Cortices That are Associated with Poor Sleep Quality. Nat. Sci. Sleep 2021, 13, 1507–1517. [Google Scholar] [CrossRef]
- Stout, J.W.; Beidel, D.C.; Brush, D.; Bowers, C. Sleep disturbance and cognitive functioning among firefighters. J. Health Psychol. 2021, 26, 2248–2259. [Google Scholar] [CrossRef] [PubMed]
- Suminska, S.; Nowak, K.; Lukomska, B.; Cygan, H.B. Cognitive functions of shift workers: Paramedics and firefighters—An electroencephalography study. Int. J. Occup. Saf. Ergon. 2021, 27, 686–697. [Google Scholar] [CrossRef]
- Yung, M.; Kolus, A.; Wells, R.; Neumann, W.P. Examining the fatigue-quality relationship in manufacturing. Appl. Ergon. 2020, 82, 102919. [Google Scholar] [CrossRef]
- Orr, R.; Simas, V.; Canetti, E.; Schram, B. A Profile of Injuries Sustained by Firefighters: A Critical Review. Int. J. Environ. Res. Public Health 2019, 16, 3931. [Google Scholar] [CrossRef]
- Kearney, J.; Muir, C.; Smith, K. Occupational injury among paramedics: A systematic review. Inj. Prev. 2022, 28, 175–184. [Google Scholar] [CrossRef]
- Uehli, K.; Mehta, A.J.; Miedinger, D.; Hug, K.; Schindler, C.; Holsboer-Trachsler, E.; Leuppi, J.D.; Kunzli, N. Sleep problems and work injuries: A systematic review and meta-analysis. Sleep Med. Rev. 2014, 18, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.-H.; Kim, Y.-K.; Kim, K.S.; Ahn, Y.-S. Characteristics of Workplace Injuries among Nineteen Thousand Korean Firefighters. J. Korean Med. Sci. 2016, 31, 1546–1552. [Google Scholar] [CrossRef]
- Gray, S.E.; Collie, A. The nature and burden of occupational injury among first responder occupations: A retrospective cohort study in Australian workers. Injury 2017, 48, 2470–2477. [Google Scholar] [CrossRef]
- Campbell, R. Firefighter Injuries on the Fireground; National Fiire Protection Associiaton: Quincy, MA, USA, 2022; pp. 1–11. [Google Scholar]
- Butry, D.T.; Webb, D.; Gilbert, S.; Taylor, J. TriData. The Economic Consequences of Firefighter Injuries and Their Prevention; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2019. [CrossRef]
- Maguire, B.J.; Al Amiry, A.; O’Neill, B.J. Occupational Injuries and Illnesses among Paramedicine Clinicians: Analyses of US Department of Labor Data (2010–2020). Prehosp. Disaster Med. 2023, 38, 581–588. [Google Scholar] [CrossRef]
- Maguire, B.J.; O’Meara, P.F.; Brightwell, R.F.; O’Neill, B.J.; Fitzgerald, G.J. Occupational injury risk among Australian paramedics: An analysis of national data. Med. J. Aust. 2014, 200, 477–480. [Google Scholar] [CrossRef]
- Hillman, D.; Mitchell, S.; Streatfeild, J.; Burns, C.; Bruck, D.; Pezzullo, L. The economic cost of inadequate sleep. Sleep 2018, 41, zsy083. [Google Scholar] [CrossRef]
- Khoshakhlagh, A.H.; Al Sulaie, S.; Yazdanirad, S.; Orr, R.M.; Dehdarirad, H.; Milajerdi, A. Global prevalence and associated factors of sleep disorders and poor sleep quality among firefighters: A systematic review and meta-analysis. Heliyon 2023, 9, e13250. [Google Scholar] [CrossRef]
- Sawyer, S.; Cowlishaw, S.; Kendrick, K.; Boyle, M.; Dicker, B.; Lord, B. Systematic Review of Incidence, Prevalence, and Trends in Health Outcomes for Australian and New Zealand Paramedics. Prehosp. Emerg. Care 2022, 27, 398–412. [Google Scholar] [CrossRef]
- Parker, R.S.; Parker, P. The impact of sleep deprivation in military surgical teams: A systematic review. J. R. Army Med. Corps 2017, 163, 158–163. [Google Scholar] [CrossRef] [PubMed]
- International Civil Aviation Organisation (ICAO). Fatigue Management Guide for Airline Operators, 2nd ed.; International Civil Aviation Organisation: Montreal, QC, Canada, 2015. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- International Civil Aviation Organisation (ICAO). Fatigue Management Guide for Air Traffic Service Providers, 1st ed.; International Civil Aviation Organisation: Montreal, QC, Canada, 2016. [Google Scholar]
- Systematic Review Accelerator. SearchRefinery. Available online: https://sr-accelerator.com/#/ (accessed on 20 October 2021).
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. Br. Med. J. 2021, 372, n160. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Kwong, J.S.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.L.; Wang, Y.Y.; Yang, Z.H.; Huang, D.; Weng, H.; Zeng, X.T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Viera, A.J.; Garret, J.M. Understanding interobserver agreement- the kappa statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar] [PubMed]
- Courtney, J.; Francis, A.; Paxton, S. Caring for the Country: Fatigue, Sleep and Mental Health in Australian Rural Paramedic Shiftworkers. J. Community Health 2013, 38, 178–186. [Google Scholar] [CrossRef]
- Courtney, J.B.; Lipsey, T.; Braun, B.; Henry, K.; Nelson, T.L.; Kaigang, L. Using Ecological Momentary Assessment to Examine the Effects of Duty Status on Acute Stress and Tiredness in Firefighters: A Pilot Study. J. Occup. Environ. Med. 2020, 62, 859–870. [Google Scholar] [CrossRef] [PubMed]
- Cvirn, M.A.; Dorrian, J.; Smith, B.P.; Jay, S.M.; Vincent, G.E.; Ferguson, S.A. The sleep architecture of Australian volunteer firefighters during a multi-day simulated wildfire suppression: Impact of sleep restriction and temperature. Accid. Anal. Prev. 2017, 99 Pt B, 389–394. [Google Scholar] [CrossRef]
- Dawson, D.; Mayger, K.; Thomas, M.J.; Thompson, K. Fatigue risk management by volunteer fire-fighters: Use of informal strategies to augment formal policy. Accid. Anal. Prev. 2015, 84, 92–98. [Google Scholar] [CrossRef]
- de Carvalho Dutra, K.L. Nursing Diagnosis Related to Military Fire Fighters. J. Nurs. UFPE/Rev. Enferm. UFPE 2017, 11, 196–205. [Google Scholar]
- Dennison, K.J.; Mullineaux, D.R.; Yates, J.W.; Abel, M.G. The effect of fatigue and training status on firefighter performance. J. Strength Cond. Res. 2012, 26, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, E.A.; Bradford, P.; Davis, M.; Hedges, C.; Socha, D.; Morassutti, P. Fatigue and Safety in Paramedicine. Can. J. Emerg. Med. 2019, 21, 762–765. [Google Scholar] [CrossRef]
- Donnelly, E.A.; Bradford, P.; Davis, M.; Hedges, C.; Socha, D.; Morassutti, P.; Pichika, S.C. What influences safety in paramedicine? Understanding the impact of stress and fatigue on safety outcomes. J. Am. Coll. Emerg. Physicians Open 2020, 1, 460–473. [Google Scholar] [CrossRef]
- Ferguson, S.A.; Smith, B.P.; Browne, M.; Rockloff, M.J. Fatigue in emergency services operations: Assessment of the optimal objective and subjective measures using a simulated wildfire deployment. Int. J. Environ. Res. Public Health 2016, 13, 171. [Google Scholar] [CrossRef] [PubMed]
- Fullagar, H.H.K.; Schwarz, E.; Richardson, A.; Notley, S.R.; Lu, D.; Duffield, R. Australian firefighters perceptions of heat stress, fatigue and recovery practices during fire-fighting tasks in extreme environments. Appl. Ergon. 2021, 95, 103449. [Google Scholar] [CrossRef]
- Games, K.E.; Winkelmann, Z.K.; Eberman, L.E. Physical Exertion Diminishes Static and Dynamic Balance in Firefighters. Int. J. Athl. Ther. Train. 2020, 25, 318–322. [Google Scholar] [CrossRef]
- Gerstner, G.R.; Mota, J.A.; Giuliani, H.K.; Weaver, M.A.; Shea, N.W.; Ryan, E.D. The impact of repeated bouts of shiftwork on rapid strength and reaction time in career firefighters. Ergonomics 2022, 65, 1086–1094. [Google Scholar] [CrossRef]
- Ghasemi, F.; Zarei, H.; Babamiri, M.; Kalatpour, O. Fatigue profile among petrochemical firefighters and its relationship with safety behavior: The moderating and mediating roles of perceived safety climate. Int. J. Occup. Saf. Ergon. JOSE 2021, 28, 1822–1828. [Google Scholar] [CrossRef]
- Giuliani, H.K.; Gerstner, G.R.; Mota, J.A.; Ryan, E.D. Influence of Demographic Characteristics and Muscle Strength on the Occupational Fatigue Exhaustion Recovery Scale in Career Firefighters. J. Occup. Environ. Med. 2020, 62, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.S.; Chen, Y.C.; Tsai, S.Y.; Huang, Y.E.; Guo, Y.L. Incomplete off-duty work hours and sleep quality among firefighters: A cross-sectional study, Taiwan. Int. Arch. Occup. Environ. Health 2022, 96, 247–257. [Google Scholar] [CrossRef]
- Jeklin, A.T.; Davies, H.W.; Bredin, S.S.D.; Hives, B.A.; Meanwell, L.E.; Perrotta, A.S.; Warburton, D.E.R. Fatigue and sleep patterns among Canadian wildland firefighters during a 17-day fire line deployment. J. Occup. Environ. Hyg. 2020, 17, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Jeklin, A.T.; Perrotta, A.S.; Davies, H.W.; Bredin, S.S.D.; Paul, D.A.; Warburton, D.E.R. The association between heart rate variability, reaction time, and indicators of workplace fatigue in wildland firefighters. Int. Arch. Occup. Environ. Health 2021, 94, 823–831. [Google Scholar] [CrossRef]
- Jeong, K.S.; Ahn, Y.S.; Jang, T.W.; Lim, G.; Kim, H.D.; Cho, S.W.; Sim, C.S. Sleep Assessment During Shift Work in Korean Firefighters: A Cross-Sectional Study. Saf. Health Work. 2019, 10, 254–259. [Google Scholar] [CrossRef]
- Kaikkonen, P.; Lindholm, H.; Lusa, S. Physiological Load and Psychological Stress During a 24-hour Work Shift Among Finnish Firefighters. J. Occup. Environ. Med. 2017, 59, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.A.A.; Conduit, R.; Kennedy, G.A.; Jackson, M.L. The relationship between shift-work, sleep, and mental health among paramedics in Australia. Sleep Health 2020, 6, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.A.A.; Jackson, M.L.; Kennedy, G.A.; Conduit, R. A field investigation of the relationship between rotating shifts, sleep, mental health and physical activity of Australian paramedics. Sci. Rep. 2021, 11, 866. [Google Scholar] [CrossRef]
- Kujawski, S.; Słomko, J.; Tafil-Klawe, M.; Zawadka-Kunikowska, M.; Szrajda, J.; Newton, J.L.; Zalewski, P.; Klawe, J.J. The impact of total sleep deprivation upon cognitive functioning in firefighters. Neuropsychiatr. Dis. Treat. 2018, 14, 1171–1181. [Google Scholar] [CrossRef]
- Kwak, K.; Kim, B.K.; Jang, T.W.; Sim, C.S.; Ahn, Y.S.; Choi, K.S.; Jeong, K.S. Association between Shift Work and Neurocognitive Function among Firefighters in South Korea: A Prospective Before-After Study. Int. J. Environ. Res. Public Health 2020, 17, 4647. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.H.; Huang, Y.C.; Chen, W.K.; Wang, J.Y. Sleepiness and injury risk in emergency medical service workers in Taiwan. PLoS ONE 2020, 15, e0229202. [Google Scholar] [CrossRef] [PubMed]
- Marcel-Millet, P.; Groslambert, A.; Ravier, G. Effects on Firefighters’ Nocturnal Cardiac Autonomic Activity and Sleep Quality of On-Call Nights With and Without Simulated Firefighting Interventions. J. Occup. Environ. Med. 2020, 62, e644–e650. [Google Scholar] [CrossRef] [PubMed]
- McGillis, Z.; Dorman, S.C.; Robertson, A.; Lariviere, M.; Leduc, C.; Eger, T.; Oddson, B.E.; Lariviere, C. Sleep Quantity and Quality of Ontario Wildland Firefighters Across a Low-Hazard Fire Season. J. Occup. Environ. Med. 2017, 59, 1188–1196. [Google Scholar] [CrossRef]
- Nowak, K.; Łukomska, B. The impact of shift work on the wellbeing and subjective levels of alertness and sleepiness in firefighters and rescue service workers. Int. J. Occup. Saf. Ergon. JOSE 2021, 27, 1056–1063. [Google Scholar] [CrossRef]
- Paterson, J.L.; Aisbett, B.; Ferguson, S.A. Sound the alarm: Health and safety risks associated with alarm response for salaried and retained metropolitan firefighters. Saf. Sci. 2016, 82, 174–181. [Google Scholar] [CrossRef]
- Paterson, J.L.; Sofianopoulos, S.; Williams, B. What paramedics think about when they think about fatigue: Contributing factors. Emerg. Med. Australas. 2014, 26, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Klapec, S.E.; Weaver, M.D.; Guyette, F.X.; Platt, T.E.; Buysse, D.J. Differences in Paramedic Fatigue before and after Changing from a 24-hour to an 8-hour Shift Schedule: A Case Report. Prehosp. Emerg. Care 2016, 20, 132–136. [Google Scholar] [CrossRef]
- Patterson, P.D.; Weaver, M.D.; Frank, R.C.; Warner, C.W.; Martin-Gill, C.; Guyette, F.X.; Fairbanks, R.J.; Hubble, M.W.; Songer, T.J.; Callaway, C.W.; et al. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp. Emerg. Care 2012, 16, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Kim, S.; Nussbaum, M.A. Fatigue-induced balance alterations in a group of Italian career and retained firefighters. Int. J. Ind. Ergon. 2014, 44, 615–620. [Google Scholar] [CrossRef]
- Pyper, Z.; Paterson, J.L. Fatigue and mental health in Australian rural and regional ambulance personnel. Emerg. Med. Australas. 2016, 28, 62–66. [Google Scholar] [CrossRef]
- Rodríguez-Marroyo, J.A.; López-Satue, J.; Pernía, R.; Carballo, B.; García-López, J.; Foster, C.; Villa, J.G. Physiological work demands of Spanish wildland firefighters during wildfire suppression. Int. Arch. Occup. Environ. Health 2012, 85, 221–228. [Google Scholar] [CrossRef]
- Smith, B.P.; Browne, M.; Armstrong, T.A.; Ferguson, S.A. The accuracy of subjective measures for assessing fatigue related decrements in multi-stressor environments. Saf. Sci. 2016, 86, 238–244. [Google Scholar] [CrossRef]
- Sofianopoulos, S.; Williams, B.; Archer, F.; Thompson, B. The exploration of physical fatigue, sleep and depression in paramedics: A pilot study. J. Emerg. Prim. Health Care 2011, 9, 1–33. [Google Scholar] [CrossRef]
- Toyokuni, Y.; Ishimaru, T.; Honno, K.; Kubo, T.; Matsuda, S.; Fujino, Y. Near-miss incidents owing to fatigue and irregular lifestyles in ambulance personnel. Arch. Environ. Occup. Health 2022, 77, 46–50. [Google Scholar] [CrossRef]
- Vincent, G.E.; Aisbett, B.; Hall, S.; Ferguson, S. Sleep quantity and quality is not compromised during planned burn shifts < 12 H. Sleep 2016, 39, A71. [Google Scholar]
- Vincent, G.E.; Aisbett, B.; Hall, S.J.; Ferguson, S.A. Fighting fire and fatigue: Sleep quantity and quality during multi-day wildfire suppression. Ergonomics 2016, 59, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Vincent, G.E.; Aisbett, B.; Larsen, B.; Ridgers, N.D.; Snow, R.; Ferguson, S.A. The impact of heat exposure and sleep restriction on firefighters’work performance and physiology during simulated wildfire suppression. Int. J. Environ. Res. Public Health 2017, 14, 180. [Google Scholar] [CrossRef]
- Vincent, G.E.; Ferguson, S.; Larsen, B.; Ridgers, N.D.; Snow, R.; Aisbett, B. Adding sleep restriction to the equation: Impact on wildland firefighters’ work performance and physiology in hot conditions. Int. Arch. Occup. Environ. Health 2018, 91, 601–611. [Google Scholar] [CrossRef]
- Vincent, G.E.; Ferguson, S.A.; Tran, J.; Larsen, B.; Wolkow, A.; Aisbett, B. Sleep restriction during simulated wildfire suppression: Effect on physical task performance. PLoS ONE 2015, 10, e115329. [Google Scholar] [CrossRef]
- Jeklin, A.T.; Davies, H.W.; Bredin, S.S.D.; Perrotta, A.S.; Hives, B.A.; Meanwell, L.; Warburton, D.E.R. Using a biomathematical model to assess fatigue risk and scheduling characteristics in Canadian wildland firefighters. Int. J. Wildland Fire 2021, 30, 467–473. [Google Scholar] [CrossRef]
- Braude, D.; Goldsmith, T.; Weiss, S.J. Assessing air medical crew real-time readiness to perform critical tasks. Prehosp. Emerg. Care 2011, 15, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Bushmaker, R.; Corey, K.; Dunn, J.; Lalonde, T.; Estrada, S. Evaluation of a New Helicopter Crew Transport Fatigue Assessment. Air Med. J. 2019, 38, 198–201. [Google Scholar] [CrossRef]
- Guyette, F.X.; Morley, J.L.; Weaver, M.D.; Patterson, P.D.; Hostler, D. The effect of shift length on fatigue and cognitive performance in air medical providers. Prehosp. Emerg. Care 2013, 17, 23–28. [Google Scholar] [CrossRef]
- Mehta, R.K.; Nuamah, J.; Peres, S.C.; Murphy, R.R. Field Methods to Quantify Emergency Responder Fatigue: Lessons Learned from sUAS Deployment at the 2018 Kilauea Volcano Eruption. IISE Trans. Occup. Ergon. Hum. Factors 2020, 8, 166–174. [Google Scholar] [CrossRef]
- Nix, S.; Gossett, K.; Shepherd, A.D. An investigation of pilot fatigue in helicopter emergency medical services. Air Med. J. 2013, 32, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Buysse, D.J.; Weaver, M.D.; Suffoletto, B.P.; McManigle, K.L.; Callaway, C.W.; Yealy, D.M. Emergency healthcare worker sleep, fatigue, and alertness behavior survey (SFAB): Development and content validation of a survey tool. Accid. Anal. Prev. 2014, 73, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Patterson, P.D.; Weaver, M.D.; Markosyan, M.A.; Moore, C.G.; Guyette, F.X.; Doman, J.M.; Sequeira, D.J.; Werman, H.A.; Swanson, D.; Hostler, D.; et al. Impact of shift duration on alertness among air-medical emergency care clinician shift workers. Am. J. Ind. Med. 2019, 62, 325–336. [Google Scholar] [CrossRef]
- Radstaak, M.; Geurts, S.A.; Beckers, D.G.; Brosschot, J.F.; Kompier, M.A. Work stressors, perseverative cognition and objective sleep quality: A longitudinal study among Dutch Helicopter Emergency Medical Service (HEMS) Pilots. J. Occup. Health 2014, 56, 469–477. [Google Scholar] [CrossRef]
- Sedlár, M. Work-related factors, cognitive skills, unsafe behavior and safety incident involvement among emergency medical services crew members: Relationships and indirect effects. Int. J. Occup. Saf. Ergon. JOSE 2021, 28, 1281–1290. [Google Scholar] [CrossRef]
- Smellie, W.S. Testing pitfalls and summary of guidance in lipid management. BMJ 2006, 333, 83–86. [Google Scholar] [CrossRef]
- Rajendra Acharya, U.; Paul Joseph, K.; Kannathal, N.; Lim, C.M.; Suri, J.S. Heart rate variability: A review. Med. Biol. Eng. Comput. 2006, 44, 1031–1051. [Google Scholar] [CrossRef]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Louise, W.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Friesen, L.D.; Vidyarthi, A.R.; Baron, R.B.; Katz, P.P. Factors associated with intern fatigue. J. Gen. Intern. Med. 2008, 23, 1981–1986. [Google Scholar] [CrossRef] [PubMed]
- Flo, E.; Bjorvatn, B.; Folkard, S.; Moen, B.E.; Gronli, J.; Nordhus, I.H.; Pallesen, S. A reliability and validity study of the Bergen Shift Work Sleep Questionnaire in nurses working three-shift rotations. Chronobiol. Int. 2012, 29, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Grech, M.R.; Neal, A.; Yeo, G.; Smith, S.; Humphreys, M. An examination of the relationship between workload and fatigue within and across consecutive days of work: Is the relationship static or dynamic? J. Occup. Health Psychol. 2009, 14, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Winwood, P.C.; Lushington, K.; Winefield, A.H. Further development and validation of the Occupational Fatigue Exhaustion Recovery (OFER) scale. J. Occup. Environ. Med. 2006, 48, 381–389. [Google Scholar] [CrossRef]
- Patterson, P.D.; Buysse, D.J.; Weaver, M.D.; Callaway, C.W.; Yealy, D.M. Recovery between Work Shifts among Emergency Medical Services Clinicians. Prehosp. Emerg. Care 2015, 19, 365–375. [Google Scholar] [CrossRef]
- Sharot, T. The optimism bias. Curr. Biol. 2011, 21, R941–R945. [Google Scholar] [CrossRef] [PubMed]
- Hao, C.; Li, M.; Luo, W.; Ma, N. Dissociation of Subjective and Objective Alertness During Prolonged Wakefulness. Nat. Sci. Sleep 2021, 13, 923–932. [Google Scholar] [CrossRef]
- Boardman, J.M.; Bei, B.; Mellor, A.; Anderson, C.; Sletten, T.L.; Drummond, S.P.A. The ability to self-monitor cognitive performance during 60 h total sleep deprivation and following 2 nights recovery sleep. J. Sleep Res. 2018, 27, e12633. [Google Scholar] [CrossRef]
- Dorrian, J.; Lamond, N.; Holmes, A.; Burgess, H.; Roach, G.; Fletcher, A.; Dawson, D. The ability to self-monitor performance during a week of simulated night shifts. Sleep 2003, 26, 871–877. [Google Scholar] [CrossRef]
- Bustos, D.; Guedes, J.C.; Vaz, M.P.; Pombo, E.; Fernandes, R.J.; Costa, J.T.; Baptista, J.S. Non-Invasive Physiological Monitoring for Physical Exertion and Fatigue Assessment in Military Personnel: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8815. [Google Scholar] [CrossRef]
- Frone, M.R.; Tidwell, M.O. The meaning and measurement of work fatigue: Development and evaluation of the Three-Dimensional Work Fatigue Inventory (3D-WFI). J. Occup. Health Psychol. 2015, 20, 273–288. [Google Scholar] [CrossRef]
- Sun, J.; Stewart, P.; Chiew, A.; Becker, T.; Siu, W.; Varndell, W.; Chan, B.S. Association between shift work and cognitive performance on the Trail Making Test in emergency department health officers. Emerg. Med. Australas. 2021, 33, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.M.; Feyer, A.-M. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup. Environ. Med. 2000, 57, 649–655. [Google Scholar] [CrossRef]
- Doran, S.M.; Van Dongen, H.P.; Dinges, D.F. Sustained attention performance during sleep deprivation- evidence of state instability. Arch. Ital. Biol. 2001, 139, 253–267. [Google Scholar] [PubMed]
- Williamson, A.; Lombardi, D.A.; Folkard, S.; Stutts, J.; Courtney, T.K.; Connor, J.L. The link between fatigue and safety. Accid. Anal. Prev. 2011, 43, 498–515. [Google Scholar] [CrossRef] [PubMed]
- Vanttola, P.; Puttonen, S.; Karhula, K.; Oksanen, T.; Härmä, M. Employees with shift work disorder experience excessive sleepiness also on non-work days: A cross-sectional survey linked to working hours register in Finnish hospitals. Ind. Health 2020, 58, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Committee on Sleep Medicine and Research Board on Health Sciences Policy. Sleep Disorders and Sleep Deprivation—An Unmet Public Health Problem; National Academies Press: Washington, DC, USA, 2006; p. 424. [Google Scholar]
- Frost, C.; Toczko, M.; Merrigan, J.J.; Martin, J.R. The effects of sleep on firefighter occupational performance and health: A systematic review and call for action. Sleep Epidemiol. 2021, 1, 100014. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- D’Emanuele, S.; Maffiuletti, N.A.; Tarperi, C.; Rainoldi, A.; Schena, F.; Boccia, G. Rate of Force Development as an Indicator of Neuromuscular Fatigue: A Scoping Review. Front. Hum. Neurosci. 2021, 15, 701916. [Google Scholar] [CrossRef]
- Orr, R.; Pope, R.; Peterson, S.; Hinton, B.; Stierli, M. Leg Power As an Indicator of Risk of Injury or Illness in Police Recruits. Int. J. Environ. Res. Public Health 2016, 13, 237. [Google Scholar] [CrossRef]
- Holtzer, R.; Shuman, M.; Mahoney, J.R.; Lipton, R.; Verghese, J. Cognitive fatigue defined in the context of attention networks. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn. 2011, 18, 108–128. [Google Scholar] [CrossRef]
- Banks, S.; Landon, L.B.; Dorrian, J.; Waggoner, L.B.; Centofanti, S.A.; Roma, P.G.; Van Dongen, H.P.A. Effects of fatigue on teams and their role in 24/7 operations. Sleep Med. Rev. 2019, 48, 101216. [Google Scholar] [CrossRef] [PubMed]
- Sorengaard, T.A.; Olsen, A.; Langvik, E.; Saksvik-Lehouillier, I. Associations between Sleep and Work-Related Cognitive and Emotional Functioning in Police Employees. Saf. Health Work. 2021, 12, 359–364. [Google Scholar] [CrossRef]
- Akerstedt, T.; Wright, K.P., Jr. Sleep Loss and Fatigue in Shift Work and Shift Work Disorder. Sleep Med. Clin. 2009, 4, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.W.; Sletten, T.L. The Impact of Shift Work on Sleep, Alertness and Performance in Healthcare Workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef] [PubMed]
- Rice, V.J.B.; Schroeder, P.J. Self-Reported Sleep, Anxiety, and Cognitive Performance in a Sample of U.S. Military Active Duty and Veterans. Mil. Med. 2019, 184, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Vrijkotte, S.; Roelands, B.; Meeusen, R.; Pattyn, N. Sustained Military Operations and Cognitive Performance. Aerosp. Med. Hum. Perform. (AMHP) 2016, 87, 718–727. [Google Scholar] [CrossRef]
- Van Cutsem, J.; Marcora, S.; De Pauw, K.; Bailey, S.; Meeusen, R.; Roelands, B. The Effects of Mental Fatigue on Physical Performance: A Systematic Review. Sports Med. 2017, 47, 1569–1588. [Google Scholar] [CrossRef]
- Lucas, S.J.; Anson, J.G.; Palmer, C.D.; Hellemans, I.J.; Cotter, J.D. The impact of 100 hours of exercise and sleep deprivation on cognitive function and physical capacities. J. Sports Sci. 2009, 27, 719–728. [Google Scholar] [CrossRef]
- Knufinke, M.; Nieuwenhuys, A.; Maase, K.; Moen, M.H.; Geurts, S.A.E.; Coenen, A.M.L.; Kompier, M.A.J. Effects of Natural Between-Days Variation in Sleep on Elite Athletes’ Psychomotor Vigilance and Sport-Specific Measures of Performance. J. Sports Sci. Med. 2018, 17, 515–524. [Google Scholar]
- Smith, E.; Dean, G.; Holmes, L. Supporting the Mental Health and Well-Being of First Responders from Career to Retirement: A Scoping Review. Prehosp. Disaster Med. 2021, 36, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Lee, T.Y.; Banda, K.J.; Pien, L.C.; Jen, H.J.; Chen, R.; Liu, D.; Hsiao, S.S.; Chou, K.R. Prevalence of sleep disorders among first responders for medical emergencies: A meta-analysis. J. Glob. Health 2022, 12, 04092. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Drake, C. Occupational Sleep Medicine. Sleep Med. Clin. 2016, 11, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Marsh, S.M.; Gwilliam, M.; Konda, S.; Tiesman, H.M.; Fahy, R. Nonfatal Injuries to Firefighters Treated in U.S. Emergency Departments, 2003–2014. Am. J. Prev. Med. 2018, 55, 353–360. [Google Scholar] [CrossRef]
- Di Muzio, M.; Diella, G.; Di Simone, E.; Pazzaglia, M.; Alfonsi, V.; Novelli, L.; Cianciulli, A.; Scarpelli, S.; Gorgoni, M.; Giannini, A.; et al. Comparison of Sleep and Attention Metrics Among Nurses Working Shifts on a Forward- vs Backward-Rotating Schedule. JAMA Netw. Open 2021, 4, e2129906. [Google Scholar] [CrossRef]
- Bambra, C.L.; Whitehead, M.M.; Sowden, A.J.; Akers, J.; Petticrew, M.P. Shifting schedules: The health effects of reorganizing shift work. Am. J. Prev. Med. 2008, 34, 427–434. [Google Scholar] [CrossRef]
- Arsintescu, L.; Pradhan, S.; Chachad, R.G.; Gregory, K.B.; Mulligan, J.B.; Flynn-Evans, E.E. Early starts and late finishes both reduce alertness and performance among short-haul airline pilots. J. Sleep Res. 2022, 31, e13521. [Google Scholar] [CrossRef]
- Yung, M..; Gruber, J.; Du, B.; Yazdani, A. Fatigue Risk Management for First Responders: Current Landscape of Perspectives, Policies, and Practices; Canadian Institute for Safety, Wellness, & Performance (CISWP): Kitchener, ON, Canada, 2020.
- Shriane, A.E.; Ferguson, S.A.; Jay, S.M.; Vincent, G.E. Sleep hygiene in shift workers: A systematic literature review. Sleep Med. Rev. 2020, 53, 101336. [Google Scholar] [CrossRef]
- Patterson, P.D.; Martin, S.E.; Brassil, B.N.; Hsiao, W.H.; Weaver, M.D.; Okerman, T.S.; Seitz, S.N.; Patterson, C.G.; Robinson, K. The Emergency Medical Services Sleep Health Study: A cluster-randomized trial. Sleep Health 2022, 9, 64–76. [Google Scholar] [CrossRef]
- Nunes, R.F.H.; Duffield, R.; Nakamura, F.Y.; Bezerra, E.S.; Sakugawa, R.L.; Loturco, I.; Bobinski, F.; Martins, D.F.; Guglielmo, L.G.A. Recovery following Rugby Union matches: Effects of cold water immersion on markers of fatigue and damage. Appl. Physiol. Nutr. Metab. 2019, 44, 546–556. [Google Scholar] [CrossRef]
- Bouchiba, M.; Bragazzi, N.L.; Zarzissi, S.; Turki, M.; Zghal, F.; Grati, M.A.; Daab, W.; Ayadi, F.; Rebai, H.; Ibn Hadj Amor, H.; et al. Cold Water Immersion Improves the Recovery of Both Central and Peripheral Fatigue Following Simulated Soccer Match-Play. Front. Physiol. 2022, 13, 860709. [Google Scholar] [CrossRef] [PubMed]
- Dupuy, O.; Douzi, W.; Theurot, D.; Bosquet, L.; Dugue, B. An Evidence-Based Approach for Choosing Post-exercise Recovery Techniques to Reduce Markers of Muscle Damage, Soreness, Fatigue, and Inflammation: A Systematic Review With Meta-Analysis. Front. Physiol. 2018, 9, 403. [Google Scholar] [CrossRef] [PubMed]
- Nema, J.; Zdara, J.; Lasak, P.; Bavlovic, J.; Bures, M.; Pejchal, J.; Schvach, H. Impact of cold exposure on life satisfaction and physical composition of soldiers. BMJ Mil. Health 2023, e002237. [Google Scholar] [CrossRef]
- Wolkow, A.P.; Barger, L.K.; O’Brien, C.S.; Sullivan, J.P.; Qadri, S.; Lockley, S.W.; Czeisler, C.A.; Rajaratnam, S.M.W. Associations between sleep disturbances, mental health outcomes and burnout in firefighters, and the mediating role of sleep during overnight work: A cross-sectional study. J. Sleep Res. 2019, 28, e12869. [Google Scholar] [CrossRef]
- Peterson, S.A.; Wolkow, A.P.; Lockley, S.W.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Czeisler, C.A.; Rajaratnam, S.M.W.; Barger, L.K. Associations between shift work characteristics, shift work schedules, sleep and burnout in North American police officers: A cross-sectional study. Br. Med. J. Open 2019, 9, e030302. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.J.E.; Maley, M.J.; Minett, G.M.; Stewart, I.B. Occupational cooling practices of emergency first responders in the United States: A survey. Temperature 2018, 5, 348–358. [Google Scholar] [CrossRef]
- van Drongelen, A.; Boot, C.R.; Hlobil, H.; Smid, T.; van der Beek, A.J. Risk factors for fatigue among airline pilots. Int. Arch. Occup. Environ. Health 2017, 90, 39–47. [Google Scholar] [CrossRef]
- Song, B.; Yang, Y.; Bai, W.; Li, Z.; Wan, J.; Teng, X.; Shao, J.; Ji, F.; Dong, H.; Zhu, J. Effect of physical exercise on young anesthesiologists with on-call-related fatigue. Psychol. Health Med. 2019, 24, 1055–1062. [Google Scholar] [CrossRef]
- Das, B.M.; Adams, B.C. Nurses’ physical activity exploratory study: Caring for you so you can care for others. Work 2021, 68, 461–471. [Google Scholar] [CrossRef]
- Mikkelsen, K.; Stojanovska, L.; Polenakovic, M.; Bosevski, M.; Apostolopoulos, V. Exercise and mental health. Maturitas 2017, 106, 48–56. [Google Scholar] [CrossRef]
- Herbert, C.; Meixner, F.; Wiebking, C.; Gilg, V. Regular Physical Activity, Short-Term Exercise, Mental Health, and Well-Being Among University Students: The Results of an Online and a Laboratory Study. Front. Psychol. 2020, 11, 509. [Google Scholar] [CrossRef]
- Banno, M.; Harada, Y.; Taniguchi, M.; Tobita, R.; Tsujimoto, H.; Tsujimoto, Y.; Kataoka, Y.; Noda, A. Exercise can improve sleep quality: A systematic review and meta-analysis. PeerJ 2018, 6, e5172. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, G.; Fullick, S.; Grindey, C.; Maclaren, D.; Waterhouse, J. Exercise, Energy Balance and the Shift Worker. Sports Med. 2008, 38, 671–685. [Google Scholar] [CrossRef]
- Reilly, T.; Waterhouse, J. Sports performance: Is there evidence that the body clock plays a role? Eur. J. Appl. Physiol. 2009, 106, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Supples, M.W.; Rivard, M.K.; Cash, R.E.; Chrzan, K.; Panchal, A.R.; McGinnis, H.D. Barriers to Physical Activity Among Emergency Medical Services Professionals. J. Phys. Acti Health 2021, 18, 304–309. [Google Scholar] [CrossRef]
- Pronk, N.P.; Martinson, B.; Kessler, R.C.; Beck, A.L.; Simon, G.E.; Wang, P. The association between work performance and physical activity, cardiorespiratory fitness, and obesity. J. Occup. Environ. Med. 2004, 46, 19–25. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.W.; Brand, R.A.; Dunn, W.; Spindler, K.P. How to write a systematic review. Clin. Orthop. Relat. Res. 2007, 455, 23–29. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Terms |
|---|---|
| Medline | (((“exertion” [Title/Abstract] OR “no rest” [Title/Abstract] OR “exhaustion” [Title/Abstract] OR “strain” [Title/Abstract] OR “muscle fatigue” [Title/Abstract] OR “Sleep deprivation” [Title/Abstract] OR “rest” [Title/Abstract] OR “wakefulness” [Title/Abstract] OR “fatigue*” [Title/Abstract] OR “muscle fatigue” [MESH] OR “Sleep Deprivation” [MESH] OR “Rest” [Mesh] OR “Wakefulness”[Mesh] OR “fatigue” [Mesh])) AND ((“Fire*” [Title/Abstract] OR “paramed*” [Title/Abstract] OR “call centers” [Title/Abstract] OR “Ambulance” [Title/Abstract] OR “first responder” [Title/Abstract] OR “EMS” [Title/Abstract] OR “emergency medical technicians” [Title/Abstract] OR “emergency medical dispatch” [Title/Abstract] OR “Emergency Medical Technicians” [Mesh] OR “Firefighters” [Mesh] OR “Call Centers” [Mesh] OR “Emergency Medical Dispatch” [Mesh] OR “Ambulances” [Mesh]))) NOT ((“Animals” [Mesh] NOT (“Animals” [Mesh] AND “Humans” [Mesh]))) |
| Embase | (exertion:ti,ab OR ‘no rest’:ti,ab OR exhaustion:ti,ab OR strain:ti,ab OR ‘muscle fatigue’:ti,ab OR ‘sleep deprivation’:ti,ab OR rest:ti,ab OR wakefulness:ti,ab OR fatigue*:ti,ab OR ‘muscle fatigue’/exp OR ‘sleep deprivation’/exp OR ‘rest’/exp OR ‘wakefulness’/exp OR ‘fatigue’/exp) AND (fire*:ti,ab OR paramed*:ti,ab OR ‘call centers’:ti,ab OR ambulance:ti,ab OR ‘first responder’:ti,ab OR ems:ti,ab OR ‘emergency medical technicians’:ti,ab OR ‘emergency medical dispatch’:ti,ab OR ‘rescue personnel’/exp OR ‘fire fighter’/exp OR ‘call center’/exp OR ‘emergency medical dispatch’/exp OR ‘ambulance’/exp) NOT ([animals]/lim NOT [humans]/lim) |
| CINAHL | ((TI exertion OR AB exertion) OR (TI “no rest” OR AB “no rest”) OR (TI exhaustion OR AB exhaustion) OR (TI strain OR AB strain) OR (TI “muscle fatigue” OR AB “muscle fatigue”) OR (TI “Sleep deprivation” OR AB “Sleep deprivation”) OR (TI rest OR AB rest) OR (TI wakefulness OR AB wakefulness) OR (TI fatigue* OR AB fatigue*) OR (MH “muscle fatigue”+) OR (MH “Sleep Deprivation”+) OR (MH Rest+) OR (MH Wakefulness+) OR (MH fatigue+)) AND ((TI Fire* OR AB Fire*) OR (TI paramed* OR AB paramed*) OR (TI “call centers” OR AB “call centers”) OR (TI Ambulance OR AB Ambulance) OR (TI “first responder” OR AB “first responder”) OR (TI EMS OR AB EMS) OR (TI “emergency medical technicians” OR AB “emergency medical technicians”) OR (TI “emergency medical dispatch” OR AB “emergency medical dispatch”) OR (MH “Emergency Medical Technicians”+) OR (MH Firefighters+) OR (MH “Emergency Medical service communications”+) OR (MH Ambulances+)) |
| SPORTDiscus | ((TI “exertion” OR AB “exertion”) OR (TI “no rest” OR AB “no rest”) OR (TI “exhaustion” OR AB “exhaustion”) OR (TI “strain” OR AB “strain”) OR (TI “muscle fatigue” OR AB “muscle fatigue”) OR (TI “Sleep deprivation” OR AB “Sleep deprivation”) OR (TI “rest” OR AB “rest”) OR (TI “wakefulness” OR AB “wakefulness”) OR (TI “fatigue*” OR AB “fatigue*”) OR DE “Sleep Deprivation” OR DE “Rest” OR DE “fatigue”) AND ((TI “Fire*” OR AB “Fire*”) OR (TI “paramed*” OR AB “paramed*”) OR (TI “call centers” OR AB “call centers”) OR (TI “Ambulance” OR AB “Ambulance”) OR (TI “first responder” OR AB “first responder”) OR (TI “EMS” OR AB “EMS”) OR (TI “emergency medical technicians” OR AB “emergency medical technicians”) OR (TI “emergency medical dispatch” OR AB “emergency medical dispatch”) OR DE “Emergency Medical Technicians” OR DE “Call Centers” OR DE “Emergency Medical Dispatch” OR DE “Ambulances”) |
| Author/Year | Participants | Study Design |
|---|---|---|
| Courtney et al., 2013 [41] | Paramedics; n = 148, m = 117, f = 31 | Cross-sectional |
| Courtney et al., 2020 [42] | Firefighters; n = 39, m = 34, f = 4, unknown sex = 1, 38.75 ± 10.60 yr, 190.65 ± 28.51 lb, 27.53 ± 3.38 kg/m2 | Cohort |
| Cvirn et al., 2017 [43] | Volunteer firefighters; n = 61, m = 52, f = 9 Control; n = 25, m = 22, f = 3, 36 ± 15.9 yr, 27 ± 4.8 kg/m2 Awake; n = 25, m = 20, f = 5, 38.5 ± 13.2 yr, 29.2 ± 4.9 kg/m2 Awake/hot; n = 11, m = 10, f = 1, 37.5 ± 15.6 yr, 26.7 ± 4.6 kg/m2 | Cohort |
| Dawson et a., 2015 [44] | Volunteer firefighters; n = 30, unknown sex = 30, 21–65 yr | Qualitative |
| de Carvalho Dutra 2017 [45] | Military firefighters; n = 20, m = 16, f = 4, 26–45 yr, 28.2 kg/m2 | Cross-sectional |
| Dennison et al., 2012 [46] | Firefighters; n = 49, m = 49, Trained; 31.8 ± 6.9 yr, 87.6 ± 14.3 kg, 27.7 ± 3.3 kg/m2 Untrained; 31 ± 9 yr, 102 ± 19.5 kg, 31.3 ± 5.2 kg/m2 | Cohort |
| Donnelly et al., 2019 [47] | Paramedics; n = 717, m = 474, f = 243 | Cross-sectional |
| Donnelly et al., 2020 [48] | Paramedics; n = 717, m = 474, f = 243, 38 ± 10.1 yr | Cross-sectional |
| Ferguson et al., 2016 [49] | Firefighters/volunteers; n = 88, m = 77, f = 11, 38.4 ± 14.4 yr, 27.8 ± 4.53 kg/m2 | Cohort |
| Fullagar et al., 2021 [50] | Firefighters; n = 473, m = 417, f = 51, unknown sex = 5, 46 ± 11 yr | Cross-sectional |
| Games et al., 2020 [51] | Firefighters; n = 41, m = 41, 37 ± 8.1 yr, 98.8 ± 14.3 kg | Cohort |
| Gerstner et al., 2022 [52] | Firefighters; n = 35, m= 32, f = 3, 34 ± 9 yr, 97 ± 21 kg, 30 ± 5.5 kg/m2 | Cohort |
| Ghasemi et al., 2021 [53] | Petrochemical firefighters; n = 261, m = 261, 36.68 ± 6.80 yr | Cross-sectional |
| Giuliani et al., 2020 [54] | Firefighters; n = 32, m = 29, f = 3, 33.7 ± 9.2, 94.5 ± 20.8 kg, 30 ± 5.5 kg/m2 | Cohort |
| Huang et al., 2022 [93] | Firefighters; n = 801, m = 801, 32 ± 7.2 yr, 25 ± 3.7 kg/m2 | Cross-sectional |
| Jeklin et al., 2020 [56] | Firefighters; n = 30, m = 20, f = 10, 24.6 ± 4.8 yr, 25.9 ± 3.2 kg/m2 | Cohort |
| Jeklin, Davies, et al., 2021 [83] | Wildland firefighters; n = 39, m = 26, f = 13, 30.4 ± 11.6 yr | Cohort |
| Jeklin, Perrotta, et al., 2021 [57] | Wildfire services; n = 9, m = 6, f = 3, 48.5 ± 6.4 yr, 84.1 ± 19.0 kg, 28.9 ± 5.3 kg/m2 | Cohort |
| Jeong et al., 2019 [58] | Firefighters; n = 294, m = 269, f = 25, <40 yr =153, 40–49 yr = 94, >50 yr = 47, BMI < 25 = 196 and >25 = 98 | Cross-sectional |
| Kaikkonen et al., 2017 [59] | Firefighters; n = 21, unknown sex = 21, 38 ± 7 yr, 79 ± 10 kg, 25 ± 2 kg/m2 | Cohort |
| Khan et al., 2020 [60] | Paramedics; n = 134, m = 72, f = 62, 39.1 ± 12.1 yr, 26.7 ± 4.9 kg/m2 | Cross-sectional |
| Khan et al., 2021 [61] | Paramedics; n = 12, m = 5, f = 7, 39.5 ± 10.7 yr, 24.5 ± 3.4 kg/m2 | Cohort |
| Kujawski et al., 2018 [62] | Firefighters; n = 55, m = 55, 32.6 ± 6.8, 24.6 ± 2.6 kg/m2 | Cohort |
| Kwak et al., 2020 [63] | Firefighters; n = 352, m = 328, f = 24, 40.1 ± 8.7 yr | Cohort |
| Lin et al., 2020 [64] | EMT; n = 347, m = 334, f = 13, 20–29 yr, BMI 18.5–24 = 135, BMI > 24 = 212 | Cross-sectional |
| Marcel-Millet et al., 2020 [65] | Firefighters; n = 13, m = 13, 36.3 ± 6.2 yr, 73.7 ± 9.4 kg, 23.9 ± 1.7 kg/m2 | Cohort |
| McGillis et al., 2017 [66] | Wildland firefighters; n = 21, m = 21, 29.9 ± 8.4 yr | Cohort |
| Nowak and Łukomska, 2021 [67] | Paramedics; n = 18, m = 12, f = 6, 31.83 ± 4.73 yr Firefighters; n = 15, m = 15, 33 ± 5.61 yr | Cohort |
| Paterson et al., 2016 [68] | Firefighters; n = 46, m = 46, Salaried; 38 ± 10 yr Retained; 33 ± 8 yr | Qualitative |
| Paterson et al., 2014 [69] | Paramedics; n = 49, m = 37, f = 12, 38 ± 9.7 yr | Cross-sectional |
| Patterson et al., 2016 [70] | Paramedics; n = 1, m = 1, 26 yr, 29.5 kg/m2 | Case-report |
| Patterson et al., 2012 [71] | EMT; n = 511, m = 378, f = 133, 37 ±10.6 yr, BMI 18.5–24.9 = 112, BMI 25–30+ = 396 | Cross-sectional |
| Pau et al., 2014 [72] | Firefighters; n = 26, m = 26 Career; 46.2 ± 4.7 yr, 26.3 ± 2.7 kg/m2 Retained; 29.1 ± 6.1 yr, 26.6 ± 3.4 kg/m2 | Cohort |
| Pyper and Paterson, 2016 [73] | Paramedics; n = 134, m = 103, f = 31, 21–60+ yr | Cross-sectional |
| Rodríguez-Marroyo et al., 2012 [74] | Firefighters; n = 160, unknown sex = 160, 25.2 ± 0.4 yr, 75.8 ± 0.8 kg, 24.3 ± 0.2 kg/m2 | Cohort |
| Smith et al., 2016 [75] | Rural firefighters; n= 91, m = 79, f = 12, 38.4 ± 14.4 yr, 27.8 ± 4.53 kg/m2 | Cohort |
| Sofianopoulos et al., 2011 [76] | Paramedics; n = 60, m = 46, f = 14, 21–45+ yr | Cross-sectional |
| Toyokuni et al., 2022 [77] | Paramedics; n = 254, m = 254, 18–50+ yr | Cross-sectional |
| Vincent et al., 2016 [78] | Wildland firefighters; n = 33, m = 25, f = 8 | Cohort |
| Vincent et al., 2016 [79] | Wildfire firefighters; n = 40, m = 31, f = 9, 11.1 ± 11, 26.8 ± 4.7 kg/m2 | Cohort |
| Vincent et al., 2017 [80] | Wildland firefighters; n = 30, m = 27, f = 3, Sleep restricted; n = 17, 93.8 ± 20.2 kg, 29.6 ± 5.5 kg/m2 Hot and sleep restricted; n = 13, 83.8 ± 14.3 kg, 27.0 ± 4.3 kg/m2 | Cohort |
| Vincent et al., 2018 [81] | Firefighters/volunteers; n = 31, m = 26, f = 5 Hot condition; n = 18, 36 ± 13 yr, 88.0 ± 18.0 kg, 27.5 ± 3.5 kg/m2 Hot + sleep restricted; n = 13, 41 ± 17 yr, 83.8 ± 14.3 kg, 27.0 ± 4.3 kg/m2 | Cohort |
| Vincent et al., 2015 [82] | Firefighters; n = 35, m = 30, f = 5 Control; 39 ± 16 yr, 85.1 ± 7.7 kg, 26.7 ± 4.8 kg/m2 Sleep restricted; 39 ± 15 yr, 93.8 ± 20.2 kg, 29.6 ± 5.5 kg/m2 | Cohort |
| Authors | Questions | Overall Score | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||||||||||
| Courtney et al., 2020 [42] | N/A | + | + | + | - | - | + | + | + | + | + | 80% | ||||||||
| Cvirn et al., 2017 [43] | + | + | + | + | - | + | + | + | + | - | + | 82% | ||||||||
| Dennison et al., 2012 [46] | + | + | + | + | - | + | + | + | + | N/A | + | 90% | ||||||||
| Ferguson et al., 2016 [49] | + | + | + | - | - | + | + | + | + | - | + | 73% | ||||||||
| Games et al., 2020 [51] | N/A | + | + | + | - | + | + | + | + | + | + | 90% | ||||||||
| Gerstner et al., 2022 [52] | N/A | + | + | + | - | + | + | + | + | + | + | 90% | ||||||||
| Giuliani et al., 2020 [54] | N/A | + | + | + | + | - | + | + | + | + | + | 90% | ||||||||
| Jeklin et al., 2020 [56] | N/A | + | + | + | - | + | + | + | + | + | + | 90% | ||||||||
| Jeklin, Davies, et al., 2021 [83] | N/A | + | + | - | - | + | + | + | + | + | + | 80% | ||||||||
| Jeklin, Perrotta, et al., 2021 [57] | N/A | + | + | + | - | - | + | + | + | - | + | 70% | ||||||||
| Kaikkonen et al., 2017 [59] | N/A | + | + | + | - | - | + | + | + | - | + | 70% | ||||||||
| Khan et al., 2021 [61] | N/A | + | + | - | - | + | + | + | + | + | + | 80% | ||||||||
| Kwak et al., 2020 [63] | + | + | + | + | + | + | + | + | + | + | + | 100% | ||||||||
| Kujawski et al., 2018 [62] | N/A | + | + | - | - | + | + | + | + | - | + | 70% | ||||||||
| Marcel-Millet et al., 2020 [65] | N/A | + | + | + | - | + | + | + | - | - | + | 70% | ||||||||
| McGillis et al., 2017 [66] | N/A | + | + | + | - | + | + | + | + | - | + | 80% | ||||||||
| Nowak and Łukomska, 2021 [67] | + | + | + | + | - | - | + | + | + | + | + | 82% | ||||||||
| Pau et al., 2014 [72] | + | + | + | + | + | + | + | + | + | + | + | 100% | ||||||||
| Rodríguez-Marroyo et al., 2012 [74] | N/A | + | + | - | - | + | + | + | - | - | + | 60% | ||||||||
| Smith et al., 2016 [81] | + | + | + | + | - | + | + | + | - | - | + | 73% | ||||||||
| Vincent et al., 2015 [82] | + | + | + | + | + | + | + | + | + | + | + | 100% | ||||||||
| Vincent et al., 2016 [78] | N/A | + | + | + | - | - | + | + | + | - | + | 70% | ||||||||
| Vincent et al., 2016 [79] | N/A | + | + | - | - | + | + | - | + | + | + | 70% | ||||||||
| Vincent et al., 2017 [80] | + | + | + | + | + | + | + | + | + | - | + | 90% | ||||||||
| Vincent et al., 2018 [57] | + | + | + | + | - | + | + | + | - | - | + | 73% | ||||||||
| Cross-sectional studies | ||||||||||||||||||||
| Author | Questions | Overall score | ||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||||||||||
| Courtney et al., 2013 [41] | + | - | + | + | - | - | + | + | 63% | |||||||||||
| de Carvalho Dutra, 2017 [45] | + | + | + | + | - | - | + | + | 75% | |||||||||||
| Donnelly et al., 2019 [47] | + | - | + | + | + | + | + | - | 75% | |||||||||||
| Donnelly et al., 2020 [48] | - | + | + | + | + | + | + | + | 88% | |||||||||||
| Fullagar et al., 2021 [50] | + | + | - | + | + | - | - | + | 63% | |||||||||||
| Ghasemi et al., 2021 [53] | - | + | + | - | + | + | + | + | 75% | |||||||||||
| Huang et al., 2022 [55] | + | + | + | + | + | + | + | + | 100% | |||||||||||
| Jeong et al., 2019 [78] | + | + | + | + | + | - | + | + | 88% | |||||||||||
| Khan et al., 2020 [43] | + | + | + | + | + | + | + | + | 100% | |||||||||||
| Lin et al., 2020 [64] | + | + | + | + | + | + | + | + | 100% | |||||||||||
| Paterson et al., 2014 [69] | - | + | + | - | + | - | + | + | 62% | |||||||||||
| Patterson et al., 2012 [71] | - | + | + | + | + | + | + | + | 88% | |||||||||||
| Pyper and Paterson, 2016 [73] | - | + | + | - | - | - | + | - | 37% | |||||||||||
| Sofianopoulos et al., 2011 [76] | + | + | + | + | - | - | + | + | 75% | |||||||||||
| Toyokuni et al., 2022 [77] | + | + | - | - | + | - | - | + | 50% | |||||||||||
| Qualitative studies | ||||||||||||||||||||
| Author | Questions | Overall score | ||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||||||||||
| Dawson et al., 2015 [44] | + | + | + | + | + | - | - | + | + | + | 90% | |||||||||
| Paterson et al., 2016 [68] | + | + | + | + | + | - | + | + | + | + | 90% | |||||||||
| Case-report study | ||||||||||||||||||||
| Author | Questions | Overall score | ||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |||||||||||||
| Patterson et al., 2016 [70] | + | + | + | + | + | + | - | + | 88% | |||||||||||
| Author | Fatiguing Variable | Acute Fatigue, Chronic Fatigue or Combined | Outcome Measures | Results | Summary |
|---|---|---|---|---|---|
| Cvirn et al., 2017 [43] | 3-day 4-night experiment conditions:
| Acute fatigue | Activity monitor Polysomnography (PSG): total sleep time (TST), sleep onset latency (SOL), wake after sleep onset (WASO), light sleep (1 and 2), deep sleep (3), REM sleep | Activity monitor
PSG
| Sleep restriction alone is more adverse than sleeping in heat. |
| Dennison et al., 2012 [46] | 1-day simulated fire ground test (SFGT): In non-fatigued state or fatigued state after exercises session | Acute fatigue | Blood lactate Heart rate Rating of perceived exertion Total SFGT time | Blood lactate
| Long-term benefits of exercise may outweigh the negatives and those that possess higher fitness levels tend to perform more efficiently. |
| Ferguson et al., 2016 [49] | 3-day 12-h shift simulation with normal sleep with or without hot room or sleep restricted with or – hot room with physical tasks: Weighted tire drag, raking debris, walking with weighted hose while avoiding obstacles, holding a weighted hose rake in static position, and a 25 m fire hose rolling up to operational standard | Acute fatigue | Go/No-Go, Stroop Colour Word Test, and the Occupational Safety Performance Assessment Test Psychomotor Vigilance Task (PVT) Samn–Perelli Fatigue Scale (SPFS) Visual analogue scale (VAS) alertness pre-performance of task motivation | PVT
| The PVT was most sensitive objective measure with the SPFS being stronger than self-rated measures of fatigue. |
| Games et al., 2020 [51] | 1-event of the Functional Agility Short-Term Fatigue Protocol | Acute fatigue | Static and dynamic balance: double leg velocity sway single leg sway anterior Y-balance test | Post activity
| Short bouts of physical exertion negatively affected balance. |
| Gerstner et al., 2022 [52] | 3–24-h shift cycles | Acute fatigue | Actigraphy Reactive isometric force (milliseconds): 50 ms 100 ms 150 ms 200 ms Psychomotor Vigilance Task (PVT) | Actigraphy
| Rapid early force production in 50 ms was decreased on the day off following the common 3–24-h on-off shift cycle. |
| Giuliani et al., 2020 [54] | Shift cycle: 3-days on/4 days off | Acute fatigue | Body mass index (BMI) Isometric knee extension Occupational Fatigue Exhaustion Recovery Scale (OFERS) | OFERS
| Increasing age was associated with poorer recovery between shifts and with increased acute and chronic fatigue. |
| Kaikkonen et al., 2017 [59] | 2–24-h, 6-h ambulance, and 6-h fire and rescue shifts | Acute fatigue | Energy expenditure Heart rate Mean and peak Heart rate variability Oxygen uptake (VO2 max) Mean and peak Stress and recovery index | Energy expenditure
| High physiological and psychological stress loads were seen in 24-h shifts compared to shorter shifts. |
| Khan et al., 2021 [61] | 2-day shift, 2-night shift, 4-days off: Times measured were pre-shift, standard day shift, nightshift, day off one and two | Acute fatigue | Actiwatch-2: total sleep time (TST), wake after sleep onset (WASO), time in bed (TIB), number of awakenings (NOA), sleep efficiency (SE), sleep latency (SL) Galvanic skin response Karolinska Sleepiness Scale (KSS) Pittsburgh Sleep Diary (Not reported statistically) Positive and Negative Affect Score (PANAS) Samn–Perelli Fatigue Scale (SPFS) | Galvanic response
| Levels of fatigue, sleepiness, and stress were all related to the sleep restriction that came with night duty. |
| Kujawski et al., 2018 [62] | 2-day sleep deprivation in laboratory | Acute fatigue | Sprawności Operacyjnej Test: choice reaction delayed matching simple reaction visual attention test | Choice reaction
| After 12 h wake cognitive reaction tests had fewer correct responses and increased errors in simple reaction time and peaked at hour 27. |
| Marcel-Millet et al., 2020 [65] | 3-night, 3 experimental conditions: (1) At home (not on shift) (2) At station (no simulation) (3) At station (with simulation: moving two hoses 100 m; (2) obstacle course of 50 m; (3) climbing a 4-storey tower; (4) carry a 60 kg mannequin up/down one floor; (5) going down the 4-storey tower and returning to the starting point | Acute fatigue | Heart rate Heart rate variability Hexoskin sleep measures: total sleep time sleep onset latency sleep efficiency Spiegel Sleep Quality Perception Questionnaire | HR and HRV
| Being on-call affected autonomic sleep measures regardless of work simulation. |
| McGillis et al., 2017 [66] | 1–7+ day wildfire deployment types: Base work (BW) Initial attack (IA) Project fire (PF) | Acute fatigue | Actigraphy: Total sleep time (TST), wake after sleep on set (WASO), sleep efficiency (SE) Fatigue questionnaire Psychomotor Vigilance Task (PVT) | Fatigue questionnaire
| Sleep quality and quantity measures were outside of the recommended thresholds in all deployment types. |
| Nowak and Łukomska, 2021 [67] | Multiple days live job assessment: 24-h shift firefighters; 12-h shift paramedics; 8-h shift controls (office workers) | Acute fatigue | Colour Trails Test (CTT) Perceived workload: Physical and psychological D2 test Epworth Sleep Scale (ESS) Health Behaviour Inventory (HBI) Karolinska Sleepiness Scale (KSS) Pittsburgh Sleep Quality Index (PSQI) | CTT Workload
| Paramedics were most affected by shift work in sleep quality, duration, and decreases in general health scores. |
| Pau et al., 2014 [72] | 1-event of firefighter specific simulated tasks | Acute fatigue | Centre of pressure in postural balance in career vs. retained firefighters |
| Retained firefighters have more risk of balance-related injuries than career firefighters. |
| Smith et al., 2016 [75] | 3-day 12-h shift simulation with normal sleep, normal sleep + hot, sleep restricted, or sleep restricted + hot: Weighted tire drag, raking debris, walking with weighted hose while avoiding obstacles, holding a weighted hose rake in static position, and a 25 m fire hose rolling up to operational standard | Acute fatigue | Psychomotor Vigilance Task (PVT) Visual analogue scale (VAS): self-perceived performance | PVT vs. VAS
| The ability to predict fatigue lessened with each day becoming less reliable. |
| Vincent et al., 2015 [82] | 4-day simulation of six firefighter specific tasks—sleep restricted (SR) vs. control: Charged hose advance, blackout hose work, hose rolling, lateral repositioning, rake, and static hold | Acute fatigue | Core temperature Heart rate Polysomnography (PSG) Rating of perceived exertion (RPE) | Core temperature and heart rate
between SR and control group | Sleep restricted firefighters’ physical performance was largely unaffected by 4-h of sleep. |
| Vincent et al., 2016 [79] | 2–9-day wildfire deployment | Acute fatigue | Actigraphy: total sleep time (TST), sleep efficiency (SE), sleep latency (SL), sleep quality SQ), time woken (TW) Samn–Perelli Fatigue Scale (SPFS) Sleep diary/work diary Sleep location | TST (hours)
| Sleep location, shift length and shift start times have the potential to be areas to focus on to improve sleep quality and should be identified in future fatigue risk management strategies. |
| Vincent et al., 2017 [80] | 3-day 10-h shift simulation with sleep restriction or hot + sleep restriction: Charged hose advance, blackout hose work, hose rolling, lateral repositioning, rake, and static hose hold. | Acute fatigue | Core temperature Heart rate Polysomnography (PSG) Rating of Perceived Exertion (RPE) Task performance | Heart rate and core temperature
| Sleep restriction with heat did not differ in physiological responses, motivation or RPE. |
| Vincent et al., 2018 [81] | 3-day 10-h shift simulation with hot normal sleep or hot sleep restriction: Charged hose advance, blackout hose work, hose rolling, lateral repositioning, rake, and static hose hold. | Acute fatigue | Heart rate Polysomnography (PSG) Rating of Perceived Exertion (RPE) Work performance | PSG
| Physical performance was not impacted by sleep restriction. |
| Courtney et al., 2013 [41] | Survey | Chronic fatigue | Depression Anxiety Stress Scale-21 (DASS21) International Physical Activity Questionnaire-Short Form (IPAQ) Pittsburgh Sleep Quality Index (PSQI) Standard Shiftwork Index- Chronic Fatigue Scale (SSI-CFS) | DASS21 and PSQI
| The largest predictor of chronic fatigue was lack of sleep. |
| Courtney et al., 2020 [42] | Survey | Chronic fatigue | Ecological Momentary Assessment (EMA) Visual Analogue Scale: stress tiredness | EMA-acute stress
| Sleep disruptions contributed to increased levels of both stress and tiredness. |
| Dawson et al., 2015 [44] | Interview | Chronic fatigue | Open-ended questions based on perceptions, attitudes and experience of safety, opinions, and fatigue management systems with the organisation | Qualitative synthesis:
| Fatigue was a clear aspect in all volunteer firefighters and led to safety issues. |
| de Carvalho Dutra, 2017 [45] | Survey | Chronic fatigue | Habitual Physical Activity Questionnaire (AFH) Bipolar Fatigue Evaluation Questionnaire (BFEQ) Pittsburgh Sleep Quality Index Scale of Stress at Work | AFH
| Fatigue was reported by all respondents with physical or mental tiredness. |
| Donnelly et al., 2019 [47] | Survey | Chronic fatigue | Chalder Fatigue Questionnaire Emergency Medical Services Safety Inventory (EMS-SI) injury, adverse events, safety-compromising behaviours | Adverse events
| Those working greater than 40 h a week display were increased fatigue and had a decrease in safety outcomes. |
| Donnelly et al., 2020 [48] | Survey | Chronic fatigue | Chalder Fatigue Questionnaire (CFQ) Emergency Medical Services Chronic Stress Questionnaire Operational stress, organisational stress, critical incident stress Emergency Medical Services Safety Inventory (EMS-SI): injury, adverse events, safety-compromising behaviours PTSD Checklist- Military | Injuries
| Fatigue was significantly related to all stress factors and associated with safety compromising behaviours, and injuries/exposures. |
| Fullagar et al., 2021 [50] | Survey | Chronic fatigue | Visual analogue scale of mental and physical fatigue: | VAS
| The most mentally demanding tasks reported were rescue, structural firefighting, and bushfire-fighting. |
| Ghasemi et al., 2021 [53] | Survey | Chronic fatigue | Multidimension Fatigue Inventory (MFI) Perceived safety climate questions Safety behaviour items from the NFPA 1500 | Fatigue
| Fatigue negatively affects safety behaviour. |
| Huang et al., 2022 [55] | Survey | Chronic fatigue | Pittsburgh Sleep Quality Index (PSQI) | PSQI
| Those with working longer shift cycles had worse sleep quality. |
| Jeklin et al., 2020 [56] | 17-day fire line deployment (14-day work with 3-day rest) | Chronic fatigue | Actigraphy: total sleep time (TST), wake after sleep on set (WASO), sleep latency (SL), sleep efficiency (SE) Psychomotor Vigilance Task (PVT) Sleep diary (Used to enhance actigraphy) Visual analogue scale (VAS 0–10 cm): fatigue alertness sleepiness | PVT
| As deployment length increased so did objective and subjective fatigue measures. |
| Jeklin, Davies, et al., 2021 [83] | 17-day wildfire deployment (14-day work with 3-day rest) | Chronic fatigue | Circadian Alertness Simulator |
| All reported some levels of fatigue but none were high risk of accidents. |
| Jeklin, Perrotta, et al., 2021 [57] | 14-day wildfire deployment | Chronic fatigue | Actigraphy: total sleep time (TST) Heart rate variability (HRV) Reaction time: simple, choice, and discrimination reaction time Visual Analogue Scale (VAS 0–10 cm): fatigue, alertness, and sleepiness | HRV vs.
VAS of alertness
| HRV was significantly associated to increased age, subjective ratings of fatigue, and alertness as deployment time increased. |
| Khan et al., 2020 [60] | Survey | Chronic fatigue | Beck Depression Inventory-Short Form Berlin Questionnaire for OSA Bruxism Assessment Questionnaire Epworth Sleepiness Scale Fatigue Severity Scale General Health Questionnaire (SF-36) Insomnia Severity Index Perceived Stress Scale Pittsburgh Sleep Quality Index Pittsburgh Sleep Quality Index-Addendum for PTSD Shift-work Disorder Screening Questionnaire State-Trait Anxiety Inventory-Short Form Ullanlinna Narcolepsy Scale | Depression and Anxiety
| Paramedics have a high prevalence of sleep quality, insomnia, and mental health issues. |
| Lin et al., 2020 [64] | Survey | Chronic fatigue | Emergency Medical Services Safety Inventory (EMS-SI) Epworth Sleepiness Scale (ESS) Workload questions | ESS vs. EMS-SI
| Sleepiness is a key risk factor in EMS for safety and injury issues. |
| Paterson et al., 2014 [69] | Survey (open answer) | Chronic fatigue | “What do you believe your fatigue is a result of?” | Qualitative synthesis:
| Major contributors to fatigue were reported as nightshift, inadequate rest/breaks, insufficient sleep, sleep difficulties, and high/excessive workload. |
| Paterson et al., 2016 [68] | Interview | Chronic fatigue | Factors increasing health and safety risk | Qualitative synthesis:
| Fatigue is a significant issue for firefighters with retained firefighters reporting higher levels of fatigue. |
| Patterson et al., 2016 [70] | Survey | Chronic fatigue | Chalder Fatigue Questionnaire Epworth Sleepiness Scale Occupation Fatigue Exhaustion Recovery Scale (OFERS) Pittsburgh Sleep Quality Index Sleep Fatigue and Alertness Behaviour | All measures
| Changing from 24-h shift to 8-h shift substantially improved overall fatigue levels. |
| Patterson et al., 2012 [71] | Survey | Chronic fatigue | Chalder Fatigue Questionnaire (CFQ) EMS Safety Inventory (EMS-SI) Pittsburgh Sleep Quality Index (PSQI) | CFS
| Fatigue and poor sleep can increase injury and decrease safety outcomes in provider and patient. |
| Pyper and Paterson, 2016 [73] | Survey | Chronic fatigue | Chalder Fatigue Questionnaire (CFQ) Depression Anxiety Stress Scale (DASS-21) Impact Event Scale | Descriptive analytics was used
| Ambulance personnel have increased experiences of stress, fatigue, and emotional trauma. |
| Rodríguez-Marroyo et al., 2012 [74] | 4 consecutive wildfire seasons (Average 15 fire/subject) | Chronic fatigue | Core body temperature Cumulative Heat Strain Index (CHSI) Exercise workload (TRIMP) Heart rate Physiological Strain Index (PSI) | Core body temperature and heart rate
| Heart rate and core temperature were not reflective of thermal or cardiovascular strain during wildfire deployment. |
| Sofianopoulos et al., 2011 [76] | Survey | Chronic fatigue | Beck depression inventory Berlin Questionnaire Epworth Sleepiness Scale (Scores were not compared statistically) Pittsburgh Sleep Quality Index | PSQI vs. fatigue
No correlation was found for fatigue and the other variables | Paramedics report poor sleep quality, fatigue, and performing at suboptimal levels. |
| Toyokuni et al., 2022 [77] | Survey | Chronic fatigue | “During the past month, how has your fatigue level been after working?” 5-point Likert scale “During emergency rescues in the past month, have you experienced near-miss incidents?” | near-misses (OR 3.19, 95% (CI): 1.68–6.05) | Fatigue combined with an unhealthy lifestyle was associated to greater near-miss incidents. |
| Vincent et al., 2016 [78] | 4-weeks of planned burns | Chronic fatigue | Actigraphy: time in bed (TIB), total sleep time (TST), sleep efficiency (SE), sleep latency (SL) Samn–Perelli Fatigue Scale (SPFS) Sleep diaries Sleep location | Sleep quality
| Sleep quality and quantity are not affected unless shifts are >12 h. |
| Jeong et al., 2019 [58] | Shift cycle vs. day only + 1 rest day: 3- day 6-day 9-day 21-day | Combined | Actigraphy: total sleep time (TST), time in bed (TIB), sleep latency (SL), sleep efficiency (SE), wake after sleep onset (WASO) | Actigraphy
| Sleep quality on night shift and on rest day were lower than controls. |
| Kwak et al., 2020 [63] | Shift cycle: 3-day 6-day 9-day 21-day | Combined | Central Nervous System Vital Signs (CNSVS) Insomnia Severity Index (ISI) The Patient Health Questionnaire-9 (PHQ-9) | CNSVS day vs. night work
| Regardless of shift cycle neurocognitive function showed significant decrease after night shift. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marvin, G.; Schram, B.; Orr, R.; Canetti, E.F.D. Occupation-Induced Fatigue and Impacts on Emergency First Responders: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 7055. https://doi.org/10.3390/ijerph20227055
Marvin G, Schram B, Orr R, Canetti EFD. Occupation-Induced Fatigue and Impacts on Emergency First Responders: A Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(22):7055. https://doi.org/10.3390/ijerph20227055
Chicago/Turabian StyleMarvin, Graham, Ben Schram, Robin Orr, and Elisa F. D. Canetti. 2023. "Occupation-Induced Fatigue and Impacts on Emergency First Responders: A Systematic Review" International Journal of Environmental Research and Public Health 20, no. 22: 7055. https://doi.org/10.3390/ijerph20227055






