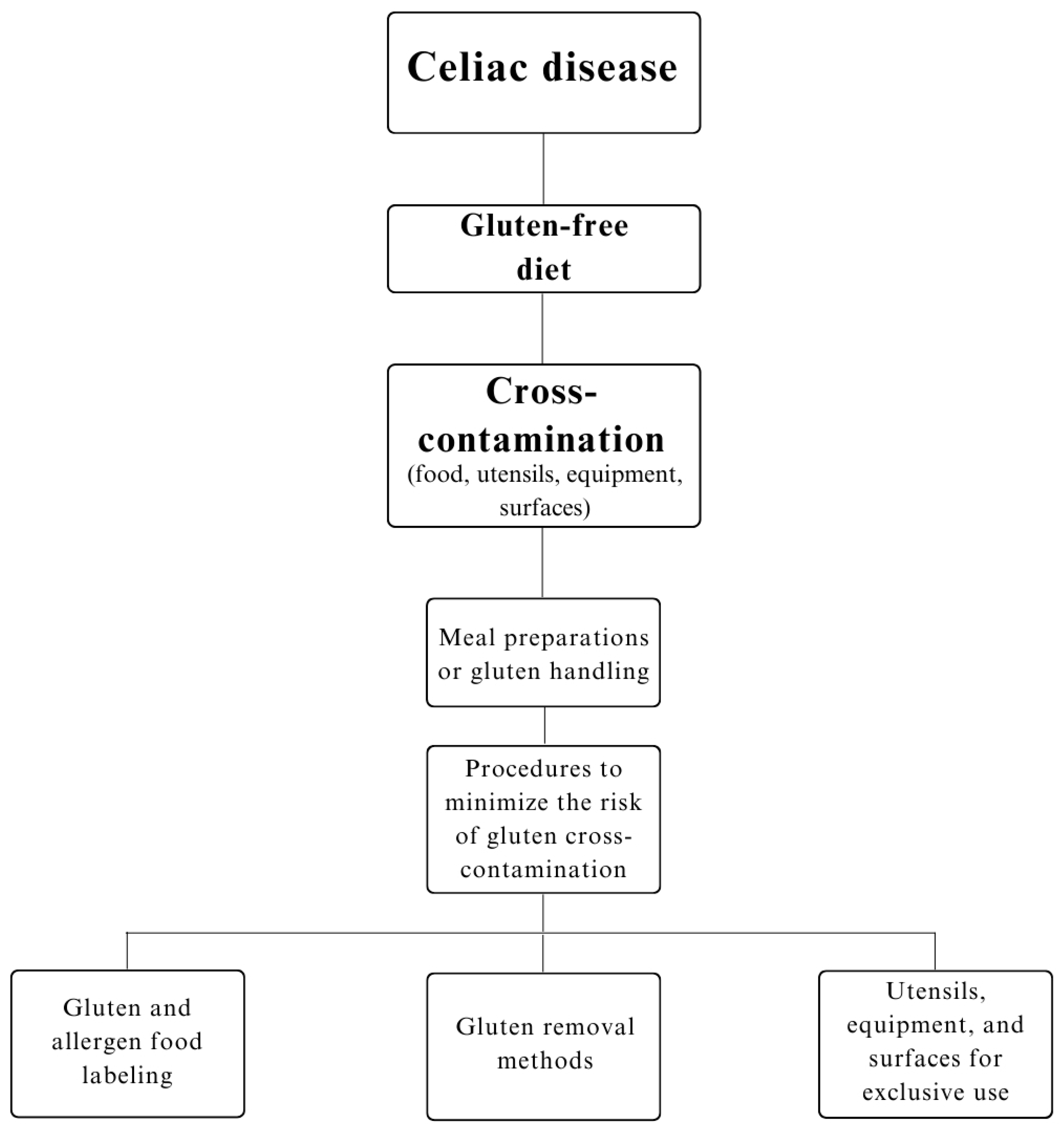
Celiac Disease: Risks of Cross-Contamination and Strategies for Gluten Removal in Food Environments
Abstract
1. Introduction
2. Methods
3. Results and Discussion
3.1. Cross-Contamination in Gluten-Free Products
3.2. Gluten Removal Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mosca, A.C.; Pellegrini, N. Toward an innovative gluten-free diet. In Biotechnological Strategies for the Treatment of Gluten Intolerance; Academic Press: Cambridge, MA, USA, 2021; pp. 131–153. [Google Scholar] [CrossRef]
- Fasano, A. All disease begins in the (leaky) gut: Role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Research 2020, 9, 69. [Google Scholar] [CrossRef] [PubMed]
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef] [PubMed]
- Valitutti, F.; Fasano, A. Breaking down barriers: How understanding celiac disease pathogenesis informed the development of novel treatments. Dig. Dis. Sci. 2019, 64, 1748–1758. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Bhatia, S.; Chunduri, V.; Kaur, S.; Sharma, S.; Kapoor, P.; Kumari, A.; Garg, M. Pathogenesis of celiac disease and other gluten related disorders in wheat and strategies for mitigating them. Front. Nutr. 2020, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Sanders, D.S.; Green, P.H. Coeliac disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Schiepatti, A.; Maimaris, S.; Nicolardi, M.L.; Alimenti, E.; Vernero, M.; Costetti, M.; Costa, S.; Biagi, F. Determinants and trends of adherence to a gluten-free diet in adult celiac patients on a long-term follow-up (2000–2020). Clin. Gastroenterol. Hepatol. 2022, 20, e741–e749. [Google Scholar] [CrossRef] [PubMed]
- Shewry, P. What is gluten—Why is it special? Front. Nutr. 2019, 6, 101. [Google Scholar] [CrossRef]
- Xiong, D.; Xu, Q.; Tian, L.; Bai, J.; Yang, L.; Jia, J.; Liu, X.; Yang, X.; Duan, X. Mechanism of improving solubility and emulsifying properties of wheat gluten protein by pH cycling treatment and its application in powder oils. Food Hydrocoll. 2023, 135, 108132. [Google Scholar] [CrossRef]
- Balakireva, A.V.; Zamyatnin, A.A., Jr. Properties of gluten intolerance: Gluten structure, evolution, pathogenicity and detoxification capabilities. Nutrients 2016, 8, 644. [Google Scholar] [CrossRef]
- Urade, R.; Sato, N.; Sugiyama, M. Gliadins from wheat grain: An overview, from primary structure to nanostructures of aggregates. Biophys. Rev. 2018, 10, 435–443. [Google Scholar] [CrossRef]
- Studerus, D.; Hampe, E.I.; Fahrer, D.; Wilhelmi, M.; Vavricka, S.R. Cross-contamination with gluten by using kitchen utensils: Fact or fiction? J. Food Prot. 2018, 81, 1679–1684. [Google Scholar] [CrossRef] [PubMed]
- Itzlinger, A.; Branchi, F.; Elli, L.; Schumann, M. Gluten-free diet in celiac disease—Forever and for all? Nutrients 2018, 10, 1796. [Google Scholar] [CrossRef] [PubMed]
- Silvester, J.A.; Comino, I.; Kelly, C.P.; Sousa, C.; Duerksen, D.R.; Bernstein, C.N.; Cebolla, A.; Dominguez, M.R.; Graff, L.A.; Green, K.H.; et al. Most patients with celiac disease on gluten-free diets consume measurable amounts of gluten. Gastroenterology 2020, 158, 1497–1499. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shi, R.; Qin, C.; Zhang, Y.; Liu, L.; Wu, Z. Gluten-free and prebiotic oat bread: Optimization formulation by transglutaminase improvement dough structure. J. Food Process. Preserv. 2021, 45, e15684. [Google Scholar] [CrossRef]
- Galan-Malo, P.; Ortiz, J.C.; Carrascon, V.; Razquin, P.; Mata, L. A study to reduce the allergen contamination in food-contact surfaces at canteen kitchens. Int. J. Gastron. Food Sci. 2019, 17, 100165. [Google Scholar] [CrossRef]
- Brazil. Collegiate Board of the National Health Surveillance Agency (ANVISA). Resolution—RDC No. 727, of July 1, 2022. Available online: http://www.anvisa.gov.br/ (accessed on 18 November 2022).
- McDonald, B.D.; Kupfer, S.S. Can We Cross Off Common Kitchen Practices as Causes of Gluten Cross-Contact? Gastroenterology 2020, 158, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Wieser, H.; Segura, V.; Ruiz-Carnicer, Á.; Sousa, C.; Comino, I. Food safety and cross-contamination of gluten-free products: A narrative review. Nutrients 2021, 13, 2244. [Google Scholar] [CrossRef]
- Fuciños, C.; Estévez, N.; Míguez, M.; Fajardo, P.; Chapela, M.J.; Gondar, D.; Rúa, M.L. Effectiveness of proteolytic enzymes to remove gluten residues and feasibility of incorporating them into cleaning products for industrial purposes. Food Res. Int. 2019, 120, 167–177. [Google Scholar] [CrossRef]
- Collin, P.; Thorell, L.; Kaukinen, K.; Mäki, M. The safe threshold for gluten contamination in gluten-free products. Can trace amounts be accepted in the treatment of coeliac disease? Aliment. Pharmacol. Ther. 2004, 19, 1277–1283. [Google Scholar] [CrossRef]
- Bustamante, M.Á.; Fernández-Gil, M.P.; Churruca, I.; Miranda, J.; Lasa, A.; Navarro, V.; Simón, E. Evolution of gluten content in cereal-based gluten-free products: An overview from 1998 to 2016. Nutrients 2017, 9, 21. [Google Scholar] [CrossRef]
- Hassan, H.; Elaridi, J.; Bassil, M. Evaluation of gluten in gluten-free-labeled foods and assessment of exposure level to gluten among celiac patients in Lebanon. Int. J. Food Sci. Nutr. 2017, 68, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Atasoy, G.; Kurt Gokhisar, O.; Turhan, M. Gluten contamination in manufactured gluten-free foods in Turkey. Food Addit. Contam. Part A 2020, 37, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Raju, N.; Joshi AK, R.; Vahini, R.; Deepika, T.; Bhaskarachari, K.; Devindra, S. Gluten contamination in labelled and naturally gluten-free grain products in southern India. Food Addit. Contam. Part A 2020, 37, 531–538. [Google Scholar] [CrossRef] [PubMed]
- Calderón de la Barca, A.M.; Luna-Alcocer, V.; Valenzuela-Miranda, J.R.; Mejía-León, M.E. Gluten-free labeling is misused frequently in foods marketed in Northwestern Mexico. Front. Nutr. 2021, 8, 687843. [Google Scholar] [CrossRef] [PubMed]
- Falcomer, A.L.; Santos Araújo, L.; Farage, P.; Santos Monteiro, J.; Yoshio Nakano, E.; Puppin Zandonadi, R. Gluten contamination in food services and industry: A systematic review. Crit. Rev. Food Sci. Nutr. 2020, 60, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Siminiuc, R.; Ţurcanu, D. Evaluation of gluten contamination of gluten-free products in the Republic of Moldova. J. Eng. Sci. 2022, 29, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Mehtab, W.; Sachdev, V.; Singh, A.; Agarwal, S.; Singh, N.; Malik, R.; Malhotra, A.; Ahuja, V.; Makharia, G. Gluten content in labeled and unlabeled gluten-free food products used by patients with celiac disease. Eur. J. Clin. Nutr. 2021, 75, 1245–1253. [Google Scholar] [CrossRef]
- Verma, A.K.; Gatti, S.; Galeazzi, T.; Monachesi, C.; Padella, L.; Baldo, G.D.; Annibali, R.; Lionetti, E.; Catassi, C. Gluten contamination in naturally or labeled gluten-free products marketed in Italy. Nutrients 2017, 9, 115. [Google Scholar] [CrossRef]
- Thompson, T.; Lee, A.R.; Grace, T. Gluten contamination of grains, seeds, and flours in the United States: A pilot study. J. Am. Diet. Assoc. 2010, 110, 937–940. [Google Scholar] [CrossRef]
- Morais, C.M.Q.D.J.; Godoi, B.K.B.; Luiz, R.A.; Santos, J.M.D. Evaluation of the information regarding to the presence or absence of gluten in some processed foods. Rev. Inst. Adolfo Lutz 2014, 73, 259–263. [Google Scholar] [CrossRef][Green Version]
- López, L.B.; Dyner, L.M.; Vidueiros, S.M.; Pallaro, A.; Valencia, M.E. Gliadins determination in food elaborated with amaranth, quínoa and/or chía. Rev. Chil. Nutr. 2010, 37, 80–86. [Google Scholar] [CrossRef]
- Guennouni, M.; Elmoumou, L.; Admou, B.; Hazime, R.; Elkhoudri, N.; Hakmaoui, A.; Bourrahouat, A.; Hilali, A. Detection of gluten content in both naturally and labelled gluten-free products available in Morocco. J. Consum. Prot. Food Saf. 2022, 17, 137–144. [Google Scholar] [CrossRef]
- Gélinas, P.; McKinnon, C.M.; Mena, M.C.; Méndez, E. Gluten contamination of cereal foods in Canada. Int. J. Food Sci. Technol. 2008, 43, 1245–1252. [Google Scholar] [CrossRef]
- Farage, P.; Zandonadi, R.P.; Gandolfi, L.; Pratesi, R.; Falcomer, A.L.; Araújo, L.S.; Nakano, E.Y.; Ginani, V.C. Accidental gluten contamination in traditional lunch meals from food services in Brasilia, Brazil. Nutrients 2019, 11, 1924. [Google Scholar] [CrossRef] [PubMed]
- Petruzzelli, A.; Foglini, M.; Paolini, F.; Framboas, M.; Serena Altissimi, M.; Naceur Haouet, M.; Mangili, P.; Osimani, A.; Clementi, F.; Cenci, T.; et al. Evaluation of the quality of foods for special diets produced in a school catering facility within a HACCP-based approach: A case study. Int. J. Environ. Health Res. 2014, 24, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, J.C.; Galan-Malo, P.; Garcia-Galvez, M.; Mateos, A.; Ortiz-Ramos, M.; Razquin, P.; Mata, L. Survey on the occurrence of allergens on food-contact surfaces from school canteen kitchens. Food Control 2018, 84, 449–454. [Google Scholar] [CrossRef]
- Miller, K.; McGough, N.; Urwin, H. Catering gluten-free when simultaneously using wheat flour. J. Food Prot. 2016, 79, 282–287. [Google Scholar] [CrossRef]
- Vincentini, O.; Izzo, M.; Maialetti, F.; Gonnelli, E.; Neuhold, S.; Silano, M. Risk of cross-contact for gluten-free pizzas in shared-production restaurants in relation to oven cooking procedures. J. Food Prot. 2016, 79, 1642–1646. [Google Scholar] [CrossRef]
- Hashimoto, H.; Yoshimitsu, M.; Kiyota, K. Analysis of scattering dynamics of wheat allergens after wheat flour sieving operation. Allergy 2017, 66, 209–221. [Google Scholar] [CrossRef]
- Wang, P.; Jin, Z.; Xu, X. Physicochemical alterations of wheat gluten proteins upon dough formation and frozen storage—A review from gluten, glutenin and gliadin perspectives. Trends Food Sci. Technol. 2015, 46, 189–198. [Google Scholar] [CrossRef]
- Vukman, D.; Viličnik, P.; Vahčić, N.; Lasić, D.; Niseteo, T.; Krbavčić, I.P.; Marković, K.; Bituh, M. Design and evaluation of an HACCP gluten-free protocol in a children’s hospital. Food Control 2021, 120, 107527. [Google Scholar] [CrossRef]
- Parsons, K.; Brown, L.; Clark, H.; Allen, E.; McCammon, E.; Clark, G.; Oblad, R.; Kenealey, J. Gluten cross-contact from common food practices and preparations. Clin. Nutr. 2021, 40, 3279–3287. [Google Scholar] [CrossRef] [PubMed]
- Thompson, T.; Lyons, T.B.; Keller, A.; Jaffe, N.; Emerson-Mason, L. Gluten-free foods cooked in shared fryers with wheat: A pilot study assessing gluten cross contact. Front. Nutr. 2021, 76, 652039. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Yoshimitsu, M.; Kiyota, K. Secondary Contamination by Wheat Allergens across Cooking Bowls through the Use of Sponge Scourers. Shokuhin Eiseigaku zasshi. J. Food Hyg. Soc. Jpn. 2022, 63, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Rostami-Nejad, M.; Asri, N.; Olfatifar, M.; Khorsand, B.; Houri, H.; Rostami, K. Systematic review and dose-response meta-analysis on the Relationship between different gluten doses and risk of coeliac disease relapse. Nutrients 2023, 15, 1390. [Google Scholar] [CrossRef] [PubMed]
- Farage, P.; Puppin Zandonadi, R.; Cortez Ginani, V.; Gandolfi, L.; Pratesi, R.; de Medeiros Nóbrega, Y.K. Content validation and semantic evaluation of a check-list elaborated for the prevention of gluten cross-contamination in food services. Nutrients 2017, 9, 36. [Google Scholar] [CrossRef] [PubMed]
- Weisbrod, V.M.; Silvester, J.A.; Raber, C.; Suslovic, W.; Coburn, S.S.; Raber, B.; McMahon, J.; Damast, A.; Kramer, Z.; Kerzner, B. A quantitative assessment of gluten cross-contact in the school environment for children with celiac disease. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 289. [Google Scholar] [CrossRef]
- Oliveira OM, V.; Zandonadi, R.P.; Gandolfi, L.; de Almeida, R.C.; Almeida, L.M.; Pratesi, R. Evaluation of the presence of gluten in beans served at self-service restaurants: A problem for celiac disease carriers. J. Culin. Sci. Technol. 2014, 12, 22–33. [Google Scholar] [CrossRef]
- Aleksić, M.; Popov-Raljić, J.; Đorđević, V.; Rašeta, M.; Lukić, M.; Spirić, D.; Janković, V. Control of nutritive allergens in a hospitality kitchen. Sci. J. Meat Technol. 2020, 61, 75–81. [Google Scholar] [CrossRef]
- McIntosh, J.; Flanagan, A.; Madden, N.; Mulcahy, M.; Dargan, L.; Walker, M.; Burns, D.T. Awareness of coeliac disease and the gluten status of ‘gluten-free’food obtained on request in catering outlets in Ireland. Int. J. Food Sci. Technol. 2011, 46, 1569–1574. [Google Scholar] [CrossRef]
- Magalhães, J.P.; da Silva Oliveira, M.; Monteiro, M.A.M.; Schaefer, M.A.; Garcia, M.A.V.T. Contamination risk for gluten in a restaurant university with preparations for individuals celiacs: A case study. Nutr. Clínica Dietética Hosp. 2017, 37, 165–170. [Google Scholar] [CrossRef]
- Bioletti, L.; Capuano, M.T.; Vietti, F.; Cesari, L.; Emma, L.; Leggio, K.; Fransos, L.; Marzullo, A.; Ropolo, S.; Strumia, C. Celiac disease and school food service in Piedmont Region: Evaluation of gluten-free meal. Ann Ig 2016, 28, 145–157. [Google Scholar] [CrossRef] [PubMed]
- Merz, M.; Appel, D.; Berends, P.; Rabe, S.; Blank, I.; Stressler, T.; Fischer, L. Batch-to-batch variation and storage stability of the commercial peptidase preparation Flavourzyme in respect of key enzyme activities and its influence on process reproducibility. Eur. Food Res. Technol. 2016, 242, 1005–1012. [Google Scholar] [CrossRef]
- Dos Santos Aguilar, J.G.; Sato, H.H. Microbial proteases: Production and application in obtaining protein hydrolysates. Food Res. Int. 2018, 103, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Vojcic, L.; Pitzler, C.; Körfer, G.; Jakob, F.; Martinez, R.; Maurer, K.H.; Schwaneberg, U. Advances in protease engineering for laundry detergents. New Biotechnol. 2015, 32, 629–634. [Google Scholar] [CrossRef]
- Bach, E.; Sant’Anna, V.; Daroit, D.J.; Corrêa, A.P.F.; Segalin, J.; Brandelli, A. Production, one-step purification, and characterization of a keratinolytic protease from Serratia marcescens P3. Process Biochem. 2012, 47, 2455–2462. [Google Scholar] [CrossRef][Green Version]
- Yu, J.M.; Lee, J.H.; Park, J.D.; Choi, Y.S.; Sung, J.M.; Jang, H.W. Analyzing gluten content in various food products using different types of ELISA test kits. Foods 2021, 10, 108. [Google Scholar] [CrossRef]

| Author/Year/Country | Utensil/Surface | Gluten Removal Method Used | Analytical Method Used | Effectiveness |
|---|---|---|---|---|
| Studerus et al. [12] Switzerland | Colander and knife (material: stainless steel) | Washing with cold water, warm water, cleaning with a clean cloth and towel and cleaning with a cloth and towel contaminated with gluten. | ELISA (sandwich) and PCR | <5 ppm gluten |
| Ladle | Cleaning with the following: (1) Clean cloth and towel; (2) Cloth and towel contaminated with gluten. | <10 ppm gluten (weak signal) | ||
| Galan-Malo et al. [16] Spain | Stainless steel, Teflon and plastic utensils | Cleaning with common detergent | ELISA (sandwich) and LFIA | Small reduction |
| Cleaning with protease detergent | Significant reduction | |||
| No extra common washing | Small reduction | |||
| With extra common washing | Significant reduction | |||
| Hand washing | Significant reduction | |||
| Washing in dishwasher | Small reduction | |||
| Fuciños et al. [20] Spain | Conveyor belt (plastic) | Enzymatic cleaning for 15 min | ELISA (sandwich and competitive) | <0.125 ppm gluten |
| Conveyor belt (stainless steel) | Enzymatic cleaning for 5 min | <0.125 ppm gluten |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vargas, F.M.d.; Cardoso, L.T.; Didoné, A.; Lima, J.P.M.; Venzke, J.G.; de Oliveira, V.R. Celiac Disease: Risks of Cross-Contamination and Strategies for Gluten Removal in Food Environments. Int. J. Environ. Res. Public Health 2024, 21, 124. https://doi.org/10.3390/ijerph21020124
Vargas FMd, Cardoso LT, Didoné A, Lima JPM, Venzke JG, de Oliveira VR. Celiac Disease: Risks of Cross-Contamination and Strategies for Gluten Removal in Food Environments. International Journal of Environmental Research and Public Health. 2024; 21(2):124. https://doi.org/10.3390/ijerph21020124
Chicago/Turabian StyleVargas, Fabiana Magnabosco de, Louise Thomé Cardoso, Amanda Didoné, João P. M. Lima, Janaína Guimarães Venzke, and Viviani Ruffo de Oliveira. 2024. "Celiac Disease: Risks of Cross-Contamination and Strategies for Gluten Removal in Food Environments" International Journal of Environmental Research and Public Health 21, no. 2: 124. https://doi.org/10.3390/ijerph21020124
APA StyleVargas, F. M. d., Cardoso, L. T., Didoné, A., Lima, J. P. M., Venzke, J. G., & de Oliveira, V. R. (2024). Celiac Disease: Risks of Cross-Contamination and Strategies for Gluten Removal in Food Environments. International Journal of Environmental Research and Public Health, 21(2), 124. https://doi.org/10.3390/ijerph21020124









