Intrapartum Quality of Care among Healthy Women: A Population-Based Cohort Study in an Italian Region
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Source
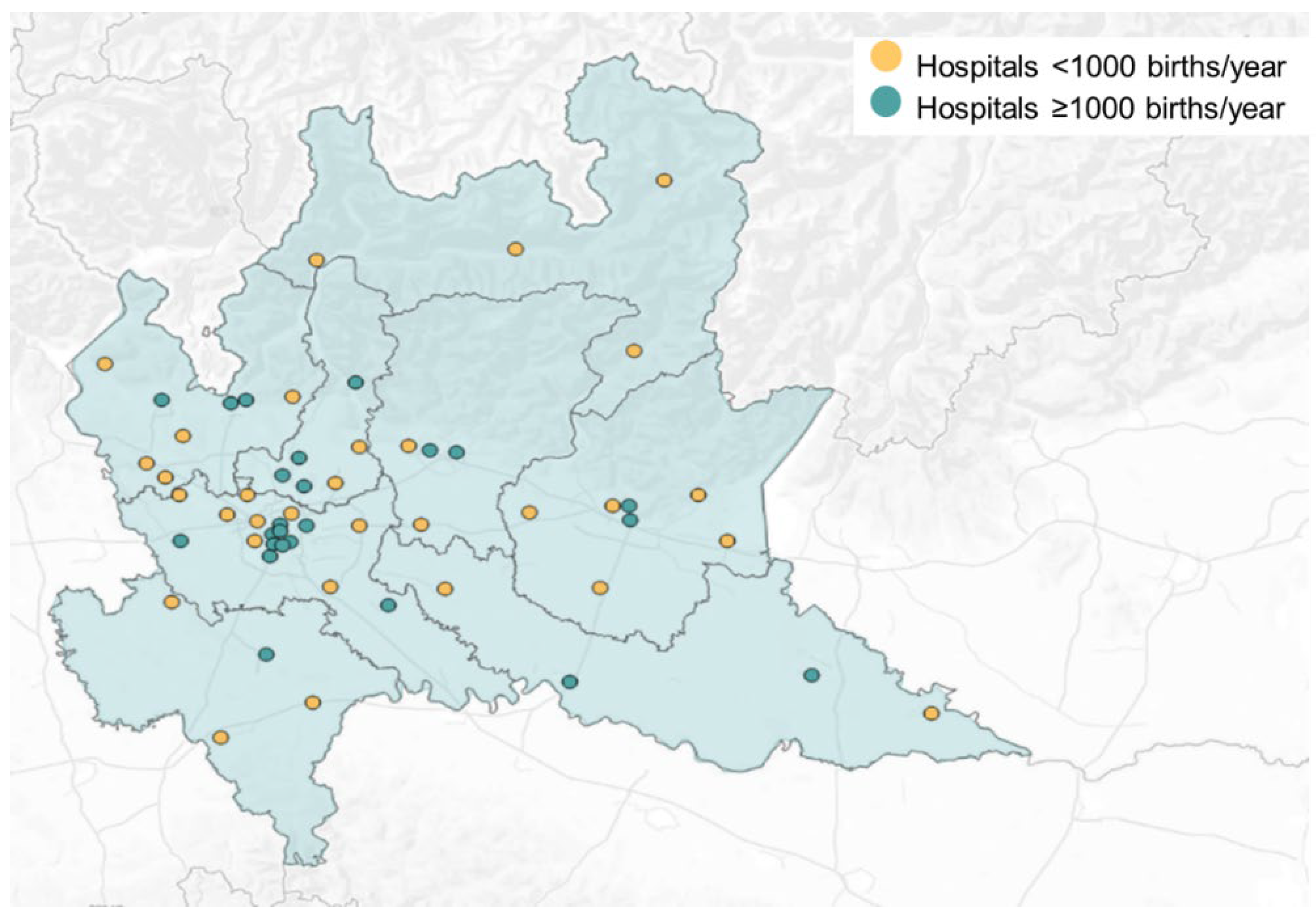
2.2. Setting
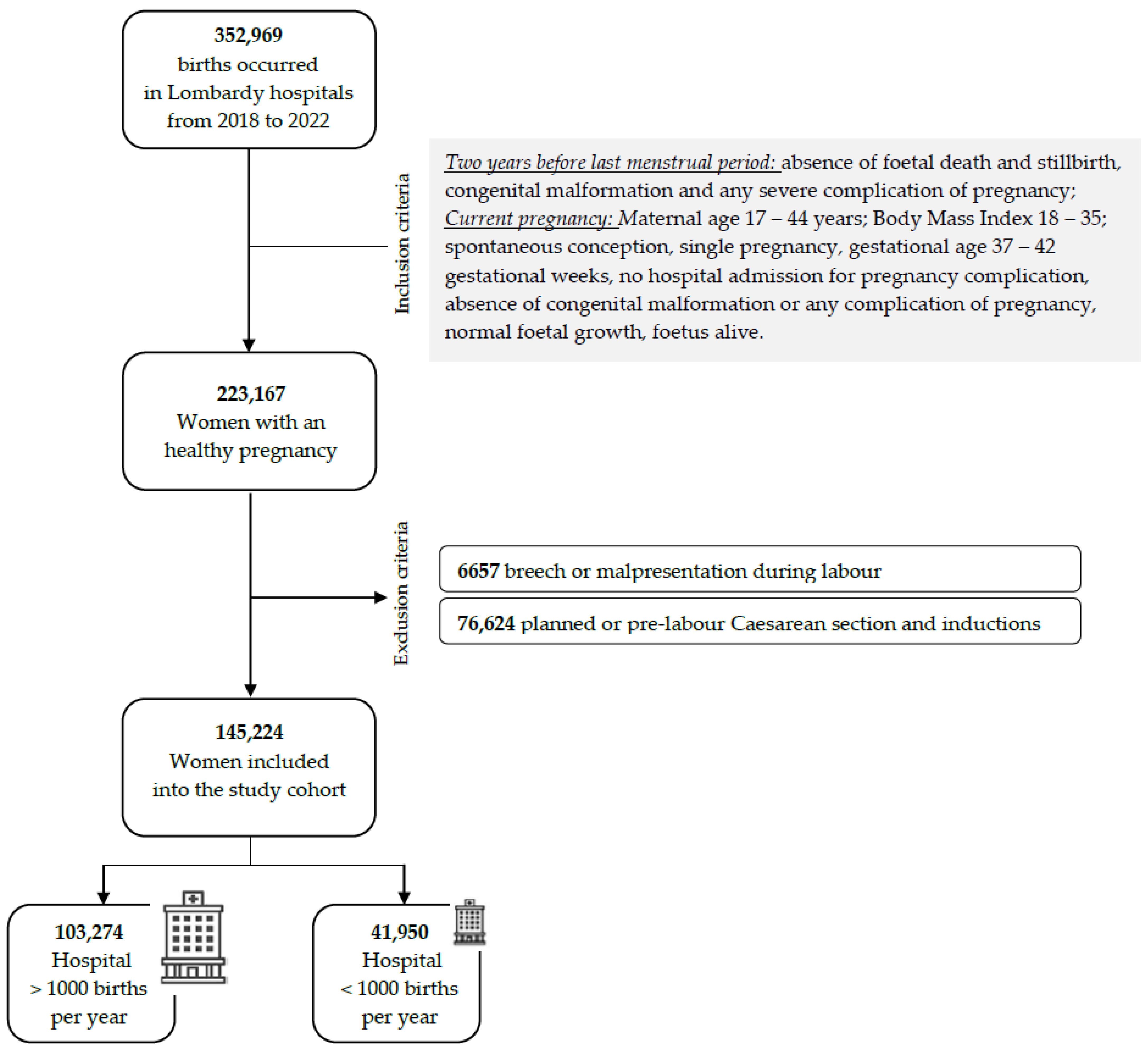
2.3. Participants
2.4. Variables
2.5. Statistical Methods
3. Results
3.1. Sample’s Characteristics
3.2. Impact of Hospital’s Birth Volume Categories on Intrapartum Midwifery Care
3.3. Impact of Hospital’s Birth Volume Categories on Maternal and Neonatal Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015. [Google Scholar]
- World Health Organization. WHO Recommendations. Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. WHO Recommendations on Maternal and Newborn Care for a Positive Postnatal Experience; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- World Health Organisation. Standard for Improving Quality of Maternal and Newborn Care in Health Facilities; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Miller, S.; Abalos, E.; Chamillard, M.; Ciapponi, A.; Colaci, D.; Comande, D.; Diaz, V.; Geller, S.; Hanson, C.; Langer, A.; et al. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016, 388, 2176–2192. [Google Scholar] [CrossRef] [PubMed]
- Burns, E.; Feeley, C.; Hall, P.J.; Vanderlaan, J. Systematic review and meta-analysis to examine intrapartum interventions, and maternal and neonatal outcomes following immersion in water during labour and waterbirth. BMJ Open. 2022, 12, e056517. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.R.; Bergman, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2016, 2016, CD003519. [Google Scholar] [CrossRef] [PubMed]
- Anim-Somuah, M.; Smyth, R.M.; Cyna, A.M.; Cuthbert, A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst. Rev. 2018, 2018, CD000331. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017, 2017, CD000081. [Google Scholar] [CrossRef] [PubMed]
- Lundsberg, L.S.; Main, E.K.; Lee, H.C.; Lin, H.; Illuzzi, J.L.; Xu, X. Low-Interventional Approaches to Intrapartum Care: Hospital Variation in Practice and Associated Factors. J. Midwifery Women’s Health 2019, 65, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Souter, V.; Nethery, E.; Kopas, M.L.; Wurz, H.; Sitcov, K.; Caughey, A.B. Comparison of Midwifery and Obstetric Care in Low-Risk Hospital Births. Obstet. Gynecol. 2019, 134, 1056–1065. [Google Scholar] [CrossRef] [PubMed]
- Bolten, N.; de Jonge, A.; Zwagerman, E.; Zwagerman, P.; Klomp, T.; Zwart, J.J.; Geerts, C.C. Effect of planned place of birth on obstetric interventions and maternal outcomes among low-risk women: A cohort study in the Netherlands. BMC Pregnancy Childbirth 2016, 16, 329. [Google Scholar] [CrossRef] [PubMed]
- Brocklehurst, P.; Hardy, P.; Hollowell, J.; Linsell, L.; Macfarlane, A.; McCourt, C.; Marlow, N.; Miller, A.; Newburn, M.; Petrou, S.; et al. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: The Birthplace in England national prospective cohort study. BMJ Online 2012, 343, d7400. [Google Scholar] [CrossRef]
- Hollowell, J.; Li, Y.; Bunch, K.; Brocklehurst, P. A comparison of intrapartum interventions and adverse outcomes by parity in planned freestanding midwifery unit and alongside midwifery unit births: Secondary analysis of “low risk” births in the birthplace in England cohort. BMC Pregnancy Childbirth 2017, 17, 95. [Google Scholar] [CrossRef]
- Jolles, D.R.; Niemczyk, N.; Velasco, L.H.; Wallace, J.; Wright, J.; Stapleton, S.; Flynn, C.; Pelletier-Butler, P.; Versace, A.; Marcelle, E.; et al. The birth center model of care: Staffing, business characteristics, and core clinical outcomes. Birth 2023, 50, 1045–1056. [Google Scholar] [CrossRef] [PubMed]
- Pfniss, I.; Gold, D.; Holter, M.; Schöll, W.; Berger, G.; Greimel, P.; Lang, U.; Reif, P. Birth during off-hours: Impact of time of birth, staff’s seniority, and unit volume on maternal adverse outcomes—A population-based cross-sectional study of 87,065 deliveries. Birth 2023, 50, 449–460. [Google Scholar] [CrossRef]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef] [PubMed]
- Dissanayake, M.; Bovbjerg, M.L.; Tilden, E.L.; Snowden, J.M. The Association between Hospital Frequency of Labor after Cesarean and Outcomes in California. Women’s Health Issues 2020, 30, 453–461. [Google Scholar] [CrossRef]
- Ferreira, I.M.; Gonçalves, A.S.; Pestana-Santos, M.; Filipe, M.M.L.; Teixeira, L.d.C.; Coutinho, E.d.C. Intrapartum care policies in high-income countries with a universal health system: A scoping review. Sex. Reprod. Health 2023, 36, 100841. [Google Scholar] [CrossRef] [PubMed]
- EuroPERISTAT. European Perinatal Health. 2015. Available online: www.europeristat.com (accessed on 15 December 2023).
- Sandall, J.; Soltani, H.; Gates, S.; Shennan, A.; Devane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016, 2016, CD004667. [Google Scholar] [CrossRef]
- Thao, V.; Hung, P.; Tilden, E.; Caughey, A.B.; Snowden, J.M.; Kozhimannil, K.B. Association between Hospital Birth Volume and Maternal Morbidity among Low-Risk Pregnancies in Rural, Urban, and Teaching Hospitals in the United States. Am. J. Perinatol. 2016, 33, 590–599. [Google Scholar] [CrossRef]
- Aubrey-Bassler, F.K.; Cullen, R.M.; Simms, A.; Asghari, S.; Crane, J.; Wang, P.P.; Godwin, M. Population-based cohort study of hospital delivery volume, geographic accessibility, and obstetric outcomes. Int. J. Gynecol. Obstet. 2019, 146, 95–102. [Google Scholar] [CrossRef]
- Handley, S.C.; Passarella, M.; Herrick, H.M.; Interrante, J.D.; Lorch, S.A.; Kozhimannil, K.B.; Phibbs, C.S.; Foglia, E.E. Birth Volume and Geographic Distribution of US Hospitals with Obstetric Services From 2010 to 2018. JAMA Netw. Open 2021, 4, e2125373. [Google Scholar] [CrossRef]
- Clark, R.R.S.; Lake, E.T. Spontaneous vaginal birth varies significantly across US hospitals. Birth 2021, 48, 44–51. [Google Scholar] [CrossRef]
- Kyser, K.L.; Lu, X.; Santillan, D.A.; Santillan, M.K.; Hunter, S.K.; Cahill, A.G.; Cram, P. The association between hospital obstetrical volume and maternal postpartum complications. Am. J. Obstet. Gynecol. 2012, 207, e1–e42. [Google Scholar] [CrossRef] [PubMed]
- Scarf, V.L.; Rossiter, C.; Vedam, S.; Dahlen, H.G.; Ellwood, D.; Forster, D.; Foureur, M.J.; McLachlan, H.; Oats, J.; Sibbritt, D.; et al. Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: A systematic review and meta-analysis. Midwifery 2018, 62, 240–255. [Google Scholar] [CrossRef] [PubMed]
- Snowden, J.M.; Cheng, Y.W.; Emeis, C.L.; Caughey, A.B. The impact of hospital obstetric volume on maternal outcomes in term, non–low-birthweight pregnancies. Am. J. Obstet. Gynecol. 2015, 212, e1–e380. [Google Scholar] [CrossRef] [PubMed]
- Walther, F.; Kuester, D.B.; Bieber, A.; Ruediger, M.; Malzahn, J.; Schmitt, J.; Deckert, S. Impact of regionalisation and case-volume on neonatal and perinatal mortality: An umbrella review. BMJ Open 2020, 10, e037135. [Google Scholar] [CrossRef] [PubMed]
- Watson, S.I.; Arulampalam, W.; Petrou, S.; Marlow, N.; Morgan, A.S.; Draper, E.S.; Santhakumaran, S.; Modi, N.; NESCOP Group. The effects of designation and volume of neonatal care on mortality and morbidity outcomes of very preterm infants in England: Retrospective population-based cohort study. BMJ Open. 2014, 4, e004856. [Google Scholar] [CrossRef] [PubMed]
- Walther, F.; Kuester, D.; Bieber, A.; Malzahn, J.; Rüdiger, M.; Schmitt, J. Are birth outcomes in low risk birth cohorts related to hospital birth volumes? A systematic review. BMC Pregnancy Childbirth 2021, 21, 531. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute. Certificato Di Assistenza al Parto (CeDAP). Analisi Dell’evento Nascita. Anno 2022. 2023. Available online: www.salute.gov.it/statistiche (accessed on 15 December 2023).
- Fumagalli, S.; Colciago, E.; Antolini, L.; Riva, A.; Nespoli, A.; Locatelli, A. Variables related to maternal satisfaction with intrapartum care in Northern Italy. Women Birth 2021, 34, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, S.; Fumagalli, S.; Colciago, E.; Downey, J.; Spiby, H.; Nespoli, A. How should a video-call service for early labour be provided? A qualitative study of midwives’ perspectives in the United Kingdom and Italy. Women Birth 2023, 36, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Svanera, C.; Nelli, E.; Colciago, E.; Fumagalli, S. Midwifery-led care for normal childbirth pathway in Lombardy Region. Minerva Ginecol. 2017, 69, 115–117. [Google Scholar] [CrossRef]
- Ministero della Salute. Accordo Stato-Regioni 16 dicembre 2010. Published online 2010. Available online: https://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2011-05-17&atto.codiceRedazionale=11A06076&elenco30giorni=false (accessed on 15 December 2023).
- Regione Lombardia. Linee di Indirizzo Operativo per la Definizione ed Organizzazione della Presa in Carico da Parte Dell’Ostetrica/o nel Percorso Nascita Fisiologico Intraospedaliero Ai Sensi della DGR 268/28.06.2018. Allegato 2 (Gestione Autonoma Nel Percorso Nascita Fisiologico, Aree Funzionali nel Percorso Nascita Fisiologico); Ostetriche Brescia: Brescia, Italy, 2018.
- Coxon, K.; Sandall, J.; Fulop, N.J. To what extent are women free to choose where to give birth? How discourses of risk, blame and responsibility influence birth place decisions. Health Risk Soc. 2014, 16, 51–67. [Google Scholar] [CrossRef]
- Miani, C.; Wandschneider, L.; Batram-Zantvoort, S.; Covi, B.; Elden, H.; Nedberg, I.H.; Drglin, Z.; Pumpure, E.; Costa, R.; Rozée, V.; et al. Individual and country-level variables associated with the medicalization of birth: Multilevel analyses of IMAgiNE EURO data from 15 countries in the WHO European region. Int. J. Gynecol. Obstet. 2022, 159, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Dehbarez, N.T.; Lou, S.; Uldbjerg, N.; Moller, A.; Gyrd-Hansen, D.; Sogaard, R. Pregnant women’s choice of birthing hospital: A qualitative study on individuals’ preferences. Women Birth 2018, 31, E389–E394. [Google Scholar] [CrossRef] [PubMed]
- Descieux, K.; Kavasseri, K.; Scott, K.; Beth Parlier, A. Why Women Choose Home Birth: A Narrative Review. MAHEC Online J. Res. 2017, 3, 1–10. [Google Scholar]
- Coxon, K.; Chisholm, A.; Malouf, R.; Rowe, R.; Hollowell, J. What influences birth place preferences, choices and decision-making amongst healthy women with straightforward pregnancies in the UK? A qualitative evidence synthesis using a ‘best fit’ framework approach. BMC Pregnancy Childbirth 2017, 17, 103. [Google Scholar] [CrossRef] [PubMed]
- Zinsser, L.A.; Stoll, K.; Gross, M.M. Midwives’ attitudes towards supporting normal labour and birth—A cross-sectional study in South Germany. Midwifery 2016, 39, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Obstetricians and Gynaecologists. Assisted Vaginal Birth: Green-top Guideline No. 26. BJOG 2020, 127, e70–e112. [Google Scholar] [CrossRef] [PubMed]
- Newnham, E.C.; Moran, P.S.; Begley, C.M.; Carroll, M.; Daly, D. Comparison of labour and birth outcomes between nulliparous women who used epidural analgesia in labour and those who did not: A prospective cohort study. Women Birth 2020, 34, e435–e441. [Google Scholar] [CrossRef] [PubMed]
- Chawanpaiboon, S.; Titapant, V.; Pooliam, J. Maternal complications and risk factors associated with assisted vaginal delivery. BMC Pregnancy Childbirth. 2023, 23, 756. [Google Scholar] [CrossRef] [PubMed]
- Bohren, M.A.; Hofmeyr, G.J.; Sakala, C.; Fukuzawa, R.K.; Cuthbert, A. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2017, 2017, CD003766. [Google Scholar] [CrossRef]
- Lucovnik, M.; Blajic, I.; Verdenik, I.; Mirkovic, T.; Pintaric, T.S. Impact of epidural analgesia on cesarean and operative vaginal delivery rates classified by the Ten Groups Classification System. Int. J. Obstet. Anesthesia 2018, 34, 37–41. [Google Scholar] [CrossRef]
- Alenchery, A.J.; Thoppil, J.; Britto, C.D.; de Onis, J.V.; Fernandez, L.; Suman Rao, P.N. Barriers and enablers to skin-to-skin contact at birth in healthy neonates—A qualitative study. BMC Pediatr. 2018, 18, 48. [Google Scholar] [CrossRef] [PubMed]
- Abdulghani, N.; Edvardsson, K.; Amir, L.H. Worldwide prevalence of mother-infant skin-to-skin contact after vaginal birth: A systematic review. PLoS ONE 2018, 13, e0205696. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Ricchi, A.; Rossi, F.; Borgognoni, P.; Bassi, M.C.; Artioli, G.; Foa, C.; Neri, I. The midwifery-led care model: A continuity of care model in the birth path. Acta Biomed. 2019, 90, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Poggianella, S.; Ambrosi, E.; Mortari, L. Women’s experience of continuity of midwifery care in North-Eastern Italy: A qualitative study. Eur. J. Midwifery 2023, 7, 4. [Google Scholar] [CrossRef]
- Colaceci, S.; Lumaca, A.; Galletti, C.; Del Grande, A.; Robu, A.I.; Terenzi, I.; Giuliani, V.; Lupi, C.; Ricciuto, V.; Marchetti, F. Italian midwives in Europe: A qualitative study on the experiences of professional migration. Ann. Ig. Med. Prev. Comunita 2023, 35, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Fumagalli, S.; Borrelli, S.E.; Galeoto, G.; Panuccio, F.; Pignataro, C.; Gottardi, M.; Nespoli, A. Assessment of the psychometric properties of the Italian version of the perceptions of empowerment in midwifery practice scale-revised (PEMS-R-IT) in midwives. Eur. J. Midwifery 2022, 6, 30. [Google Scholar] [CrossRef]
- Canova, C.; Cantarutti, A. Population-Based Birth Cohort Studies in Epidemiology. Int. J. Environ. Res. Public Health 2020, 17, 5276. [Google Scholar] [CrossRef]
- Fumagalli, S.; Panzeri, M.; Borrelli, S.; Ornaghi, S.; Antolini, L.; Sacco, G.G.A.; Formenti, M.; Sala, S.; Nespoli, A. Midwives’ stress and burnout during the Omicron wave in Italy: An observational survey. J. Adv. Nurs. 2024. ahead of pub. [Google Scholar] [CrossRef]
- Nespoli, A.; Ornaghi, S.; Borrelli, S.; Vergani, P.; Fumagalli, S. Lived experiences of the partners of COVID-19 positive childbearing women: A qualitative study. Women Birth 2022, 35, 289–297. [Google Scholar] [CrossRef]
- Ornaghi, S.; Fumagalli, S.; Montalvo, C.K.G.; Beretta, G.; Invernizzi, F.; Nespoli, A.; Vergani, P. Indirect impact of SARS-CoV-2 pandemic on pregnancy and childbirth outcomes: A nine-month long experience from a university center in Lombardy. Int. J. Gynecol. Obstet. 2022, 156, 466–474. [Google Scholar] [CrossRef]
- Fumagalli, S.; Borrelli, S.; Ornaghi, S.; Vergani, P.; Nespoli, A. Midwives’ experiences of providing maternity care to women and families during the COVID-19 pandemic in Northern Italy. Women Birth 2023, 36, e57–e64. [Google Scholar] [CrossRef] [PubMed]
| Overall | LV Hospitals | HV Hospitals | p-Value | ||||
|---|---|---|---|---|---|---|---|
| n | n | % | n | % | |||
| Number of healthy pregnancies | 145,224 | 41,950 | 28.89 | 103,274 | 71.11 | ||
| mean | SD | mean | SD | mean | SD | ||
| Age | 32.14 | 5.09 | 31.34 | 5.29 | 32.44 | 4.97 | |
| n | % | n | % | n | % | ||
| 16–25 | 15,732 | 10.83 | 6131 | 14.62 | 9601 | 9.30 | <0.0001 |
| 26–35 | 90,613 | 62.40 | 26,140 | 62.31 | 64,473 | 62.43 | |
| 36–45 | 38,371 | 26.42 | 9421 | 22.46 | 28950 | 28.03 | |
| Birth place | n | % | n | % | n | % | |
| Italian born | 97,239 | 66.96 | 25,189 | 60.05 | 72,050 | 69.77 | <0.0001 |
| Foreign born | 47,985 | 33.04 | 16,761 | 39.95 | 31,224 | 30.23 | |
| Education | n | % | n | % | n | % | |
| Primary education | 28,919 | 19.91 | 11,908 | 28.39 | 17,011 | 16.47 | <0.0001 |
| High school | 60,618 | 41.74 | 19,200 | 45.77 | 41,418 | 40.10 | 0.250 |
| Bachelor | 7589 | 5.23 | 2064 | 4.92 | 5525 | 5.35 | 0.004 |
| Master | 48,034 | 33.08 | 8763 | 20.89 | 39,271 | 38.03 | <0.0001 |
| Missing | 64 | 0.04 | 15 | 0.04 | 49 | 0.05 | 0.147 |
| Occupation | n | % | n | % | n | % | |
| Employed | 96,861 | 66.70 | 23,427 | 55.85 | 73,434 | 71.11 | <0.0001 |
| Housewife | 33,010 | 22.73 | 14,127 | 33.68 | 18,883 | 18.28 | <0.0001 |
| Student | 1208 | 0.83 | 341 | 0.81 | 867 | 0.84 | <0.0001 |
| Looking for first employment | 147 | 0.10 | 51 | 0.12 | 96 | 0.09 | 0.102 |
| Unemployed | 13,748 | 9.47 | 3929 | 9.37 | 9819 | 9.51 | 0.653 |
| Others | 155 | 0.11 | 63 | 0.15 | 92 | 0.09 | 0.001 |
| Missing | 95 | 0.07 | 12 | 0.03 | 83 | 0.08 | <0.0001 |
| Parity | |||||||
| Primiparous | 55,114 | 37.95 | 14,271 | 34.02 | 40,843 | 39.55 | <0.0001 |
| Best Practices | Overall (n = 145,224) | LV Hospitals | HV Hospitals | aOR + | 95% CI ++ | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Nonpharmacological coping strategies | 109,601 | 75.47 | 33,955 | 80.94 | 75,646 | 73.25 | 0.802 | [0.775; 0.83] | <0.0001 |
| Presence of birth companion | 122,618 | 84.43 | 33,326 | 79.44 | 89,292 | 86.46 | 1.530 | [1.481; 1.581] | <0.0001 |
| Skin to skin * | 102,728 | 70.74 | 26,971 | 64.29 | 75,757 | 73.36 | 1.393 | [1.357; 1.429] | <0.0001 |
| First breastfeeding within 1 h | 113,224 | 77.97 | 31,537 | 75.18 | 81,687 | 79.10 | 1.218 | [1.183; 1.254] | <0.0001 |
| Intrapartum interventions | |||||||||
| Augmentation with amniotomy | 4100 | 2.82 | 939 | 2.24 | 3161 | 3.06 | 0.995 | [0.705; 1.406] | 0.963 |
| Epidural analgesia | 37,016 | 25.49 | 5917 | 14.10 | 31,099 | 30.11 | 2.263 | [2.197; 2.330] | <0.0001 |
| Nonepidural analgesia | 7257 | 5.00 | 3229 | 7.70 | 4298 | 4.16 | 0.573 | [0.544; 0.605] | <0.0001 |
| Episiotomy * | 23,411 | 16.12 | 6406 | 15.27 | 17,005 | 16.47 | 1.077 | [1.044; 1.110] | <0.0001 |
| Healthcare providers present at birth | |||||||||
| Midwife | 143,485 | 98.80 | 41,393 | 98.67 | 102,092 | 98.86 | 0.956 | [0.861; 1061] | 0.397 |
| Gynecologist ** | 104,174 | 71.73 | 36,130 | 86.13 | 68,044 | 65.89 | 0.34 | [0.33; 0.349] | <0.0001 |
| Pediatrician ** | 63,231 | 43.54 | 23,939 | 57.07 | 39,292 | 38.05 | 0.446 | [0.435; 0.457] | <0.0001 |
| Maternal and Neonatal Outcomes | Overall (n = 145,224) | LV Hospitals | HV Hospitals | aOR + | 95% IC ++ | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|
| Spontaneous vaginal birth | 126,747 | 87.30 | 36,357 | 86.67 | 90,390 | 87.52 | 0.771 | [0.572; 1.039] | 0.081 |
| Vacuum-assisted birth | 7268 | 5.10 | 1885 | 4.49 | 5383 | 5.21 | 0.724 | [0.535; 0.981] | 0.042 |
| Caesarean section | 11,025 | 7.60 | 3680 | 8.77 | 7345 | 7.11 | 0.754 | [0.558; 1.019] | 0.068 |
| Perineal integrity * | 62,214 | 42.84 | 18,914 | 45.09 | 43,300 | 41.93 | 0.89 | [0.869; 0.912] | <0.0001 |
| Blood loss <1000 mL | 140,188 | 96.53 | 40,582 | 96.74 | 99,606 | 96.45 | 0.911 | [0.856; 0.97] | 0.003 |
| Low Apgar score at 5 min (<7) | 597 | 0.41 | 189 | 0.45 | 408 | 0.40 | 0.872 | [0.736; 1.033] | 0.113 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fumagalli, S.; Nespoli, A.; Panzeri, M.; Pellegrini, E.; Ercolanoni, M.; Vrabie, P.S.; Leoni, O.; Locatelli, A. Intrapartum Quality of Care among Healthy Women: A Population-Based Cohort Study in an Italian Region. Int. J. Environ. Res. Public Health 2024, 21, 629. https://doi.org/10.3390/ijerph21050629
Fumagalli S, Nespoli A, Panzeri M, Pellegrini E, Ercolanoni M, Vrabie PS, Leoni O, Locatelli A. Intrapartum Quality of Care among Healthy Women: A Population-Based Cohort Study in an Italian Region. International Journal of Environmental Research and Public Health. 2024; 21(5):629. https://doi.org/10.3390/ijerph21050629
Chicago/Turabian StyleFumagalli, Simona, Antonella Nespoli, Maria Panzeri, Edda Pellegrini, Michele Ercolanoni, Paul Stefan Vrabie, Olivia Leoni, and Anna Locatelli. 2024. "Intrapartum Quality of Care among Healthy Women: A Population-Based Cohort Study in an Italian Region" International Journal of Environmental Research and Public Health 21, no. 5: 629. https://doi.org/10.3390/ijerph21050629
APA StyleFumagalli, S., Nespoli, A., Panzeri, M., Pellegrini, E., Ercolanoni, M., Vrabie, P. S., Leoni, O., & Locatelli, A. (2024). Intrapartum Quality of Care among Healthy Women: A Population-Based Cohort Study in an Italian Region. International Journal of Environmental Research and Public Health, 21(5), 629. https://doi.org/10.3390/ijerph21050629






