Spatial Diffusion of Influenza Outbreak-Related Climate Factors in Chiang Mai Province, Thailand
Abstract
:1. Introduction
2. Materials and Methods
2.1. Physical and Climatic Setting of Chiang Mai Province, Thailand
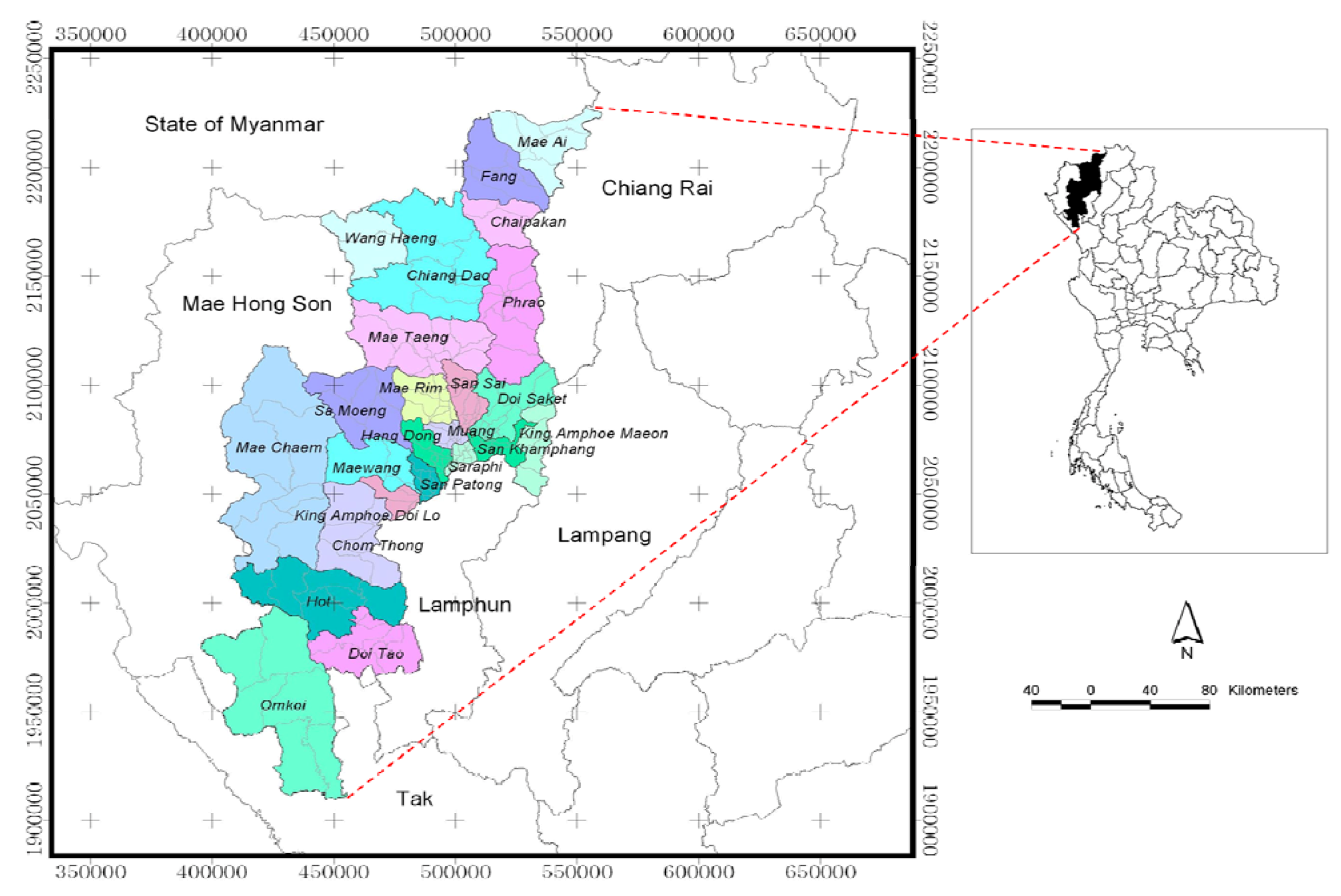
2.1.1. Physical Setting of Chiang Mai
2.1.2. Climate Variability of Chiang Mai
2.2. Data Acquisition
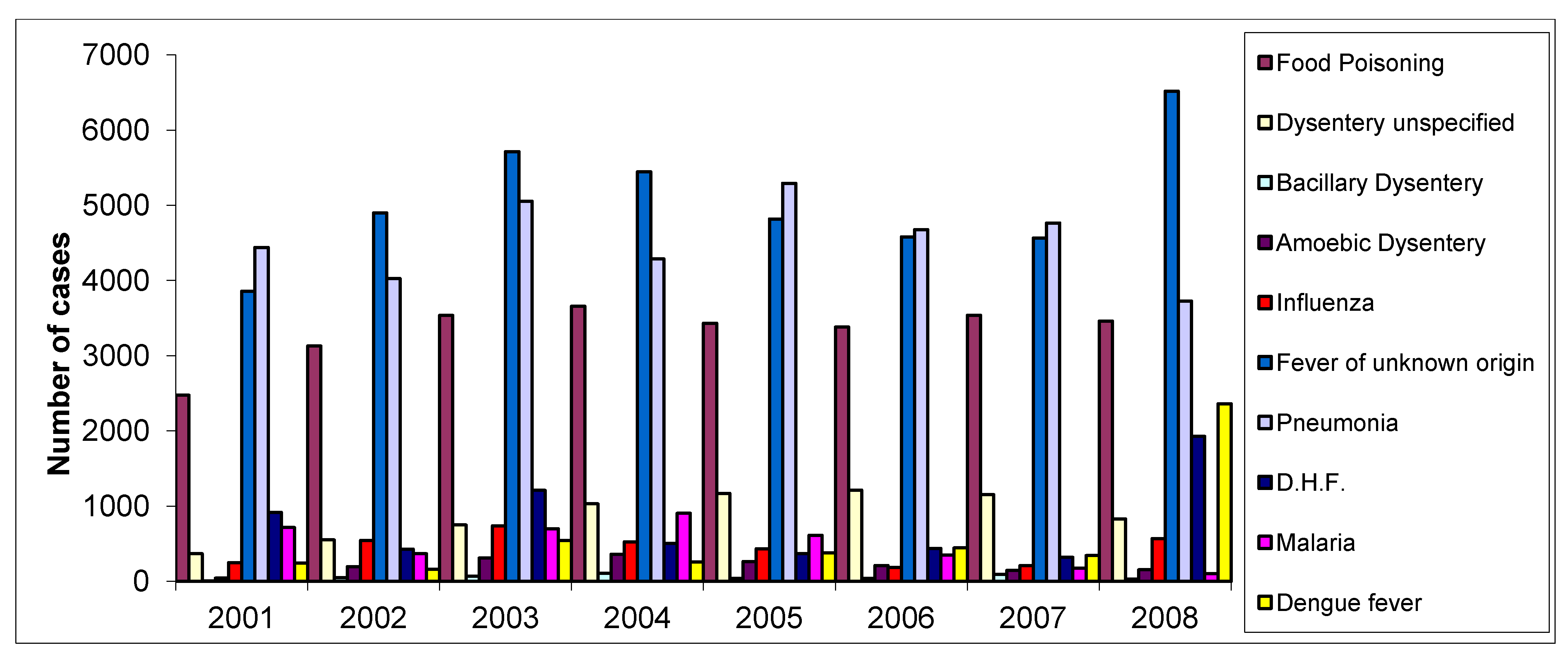
2.2.1. Epidemic Data
2.2.2. Climate Data
2.2.3. Tambon Data
2.3. Spatio-Temporal Analysis

2.4. Multiple Regression Analysis
3. Results
3.1. Spatio-Temporal Analysis of Influenza
3.1.1. General Analysis
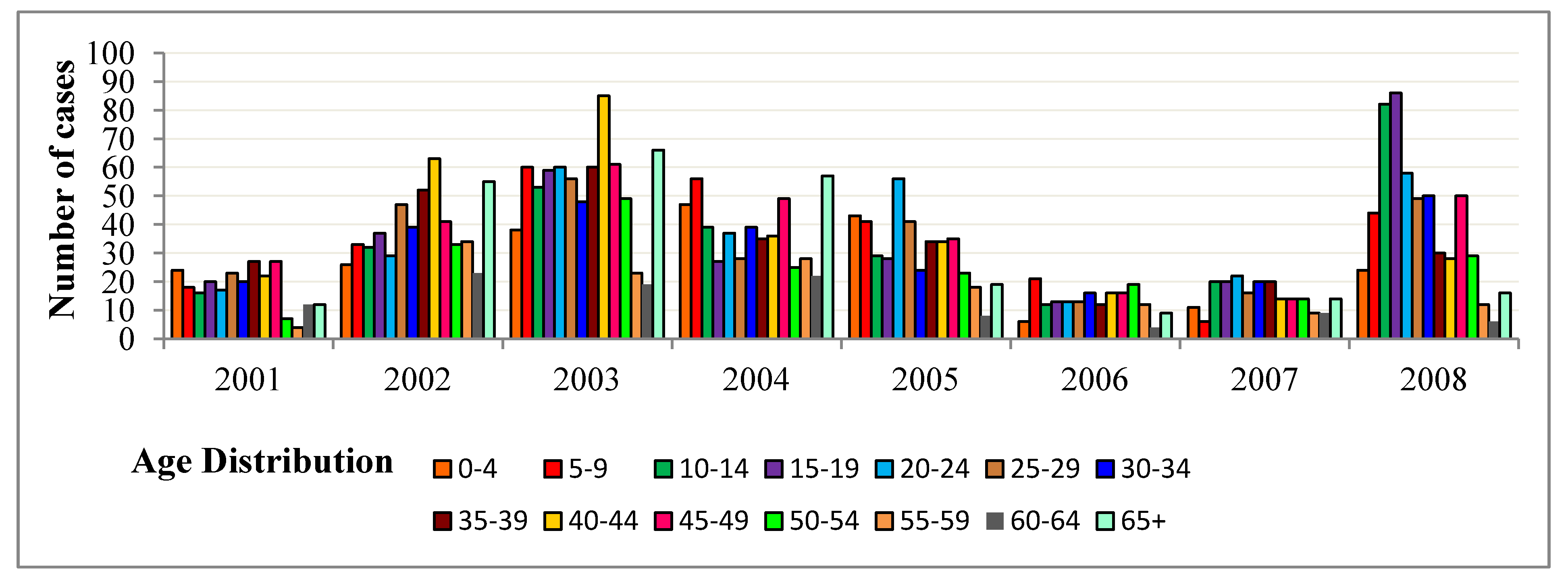
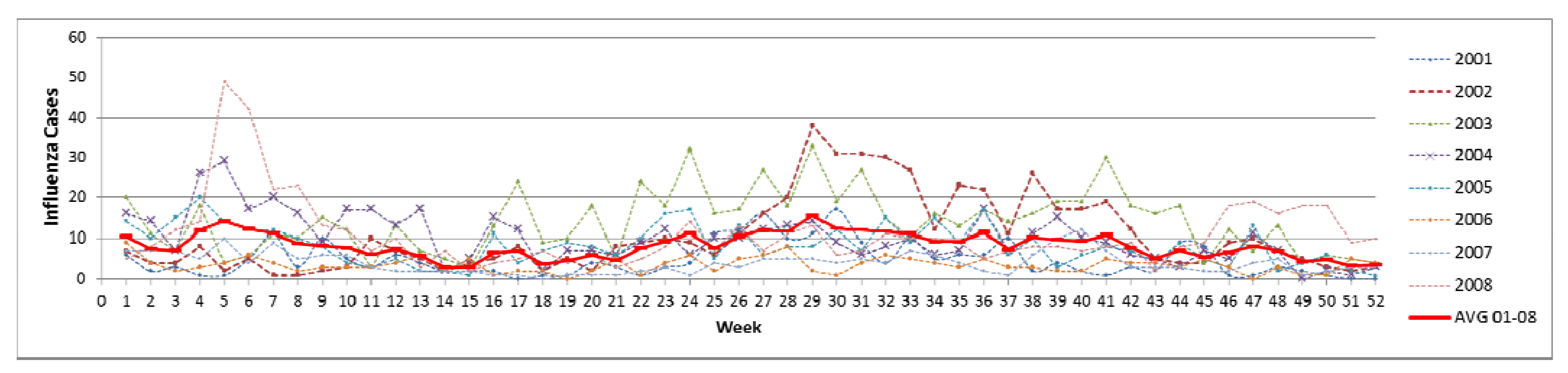
3.1.2. Temporal Analysis
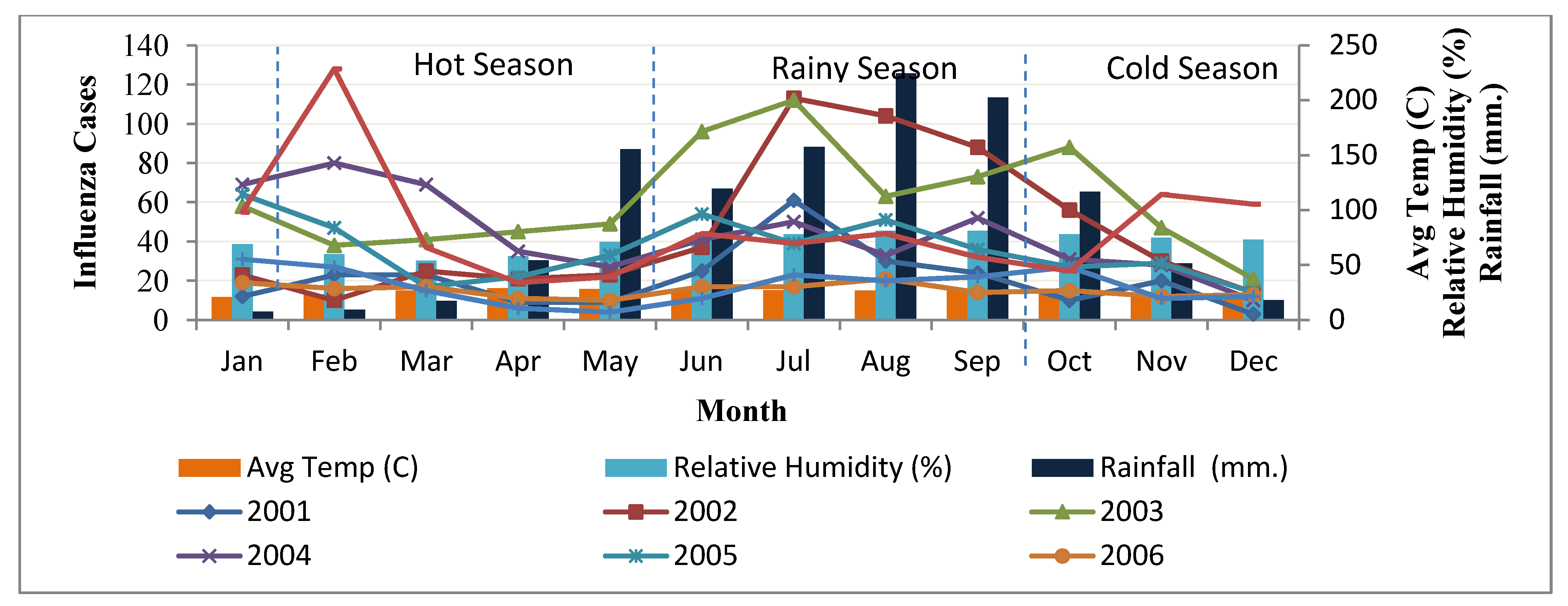
3.2. Multiple Regression Model Development
| Dependent Variable | |||
| Y | Estimated number of influenza cases | ||
| Independent Variable | |||
| Xr | Amount of rainy day | ||
| Xt | Temperature difference | ||
| XRh | Relative humidity | ||
| Climate Factors | Variable | Year | Rainy Season | t-test |
|---|---|---|---|---|
| Influenza cases | Y | 8.27 ± 3.02 | 9.97 ± 2.43 | t1.52 = −0.438 * |
| Rainy days | Xr | 2.21 ± 1.74 | 4.05 ± 0.66 | t1.52 = 1.394 ** |
| Temperature Difference | Xt | 11.05 ± 3.00 | 8.12 ± 0.81 | t1.52 = 0.785 * |
| Relative Humidity | XRh | 74.12 ± 10.26 | 82.44 ± 2.35 | t1.52 = 1.043 * |
| Period | Multiple Regression Model | Linear Regression Model | F Value |
|---|---|---|---|
| Year | Relationship Equation-1(RE-1) | Y = 0.789Xr + 0.420Xt + 0.107XRh − 6.039 | F3.48 = 2.51 * |
| Rainy Season | Relationship Equation-2(RE-2) | Y = −0.783Xr – 2.663Xt – 0.079XRh + 41.299 | F3.17 = 6.97 ** |
3.2.1. Relationship Equation-1 (RE-1)
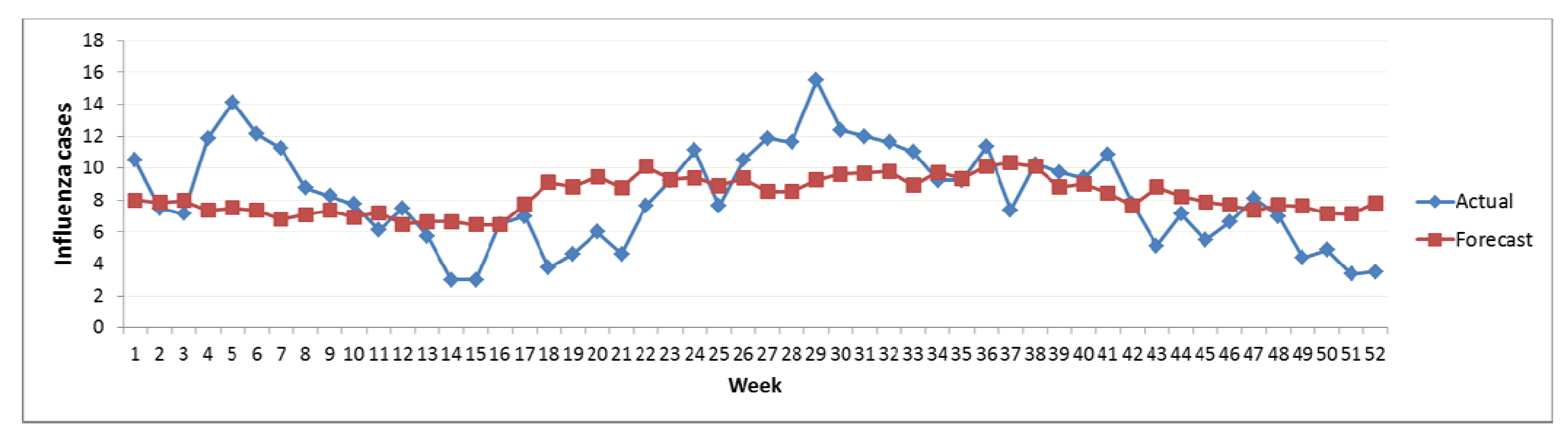
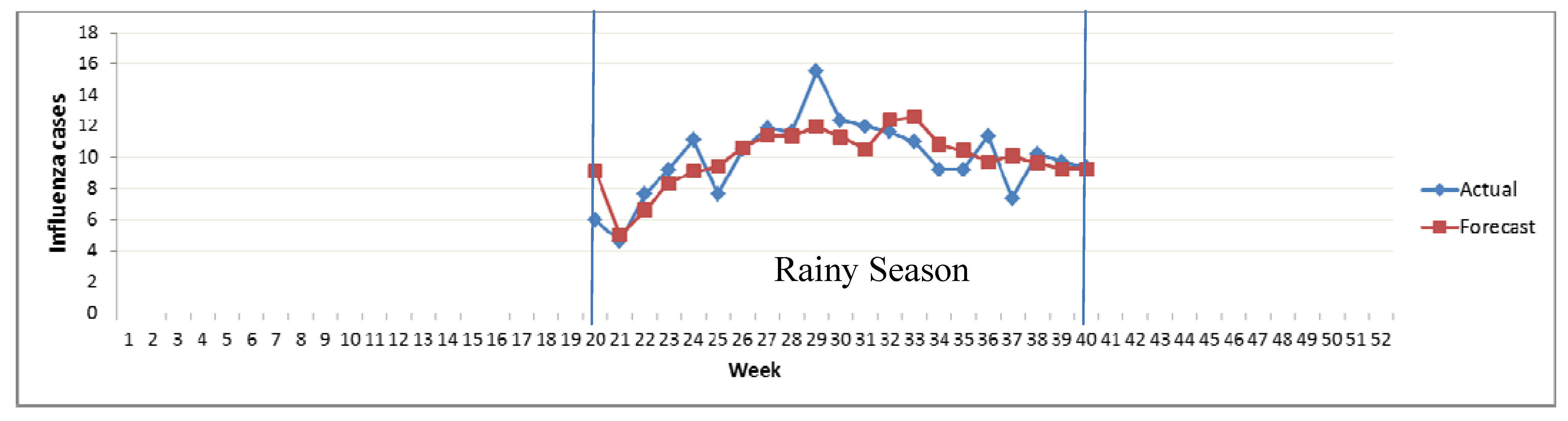
3.2.2. Relationship Equation-2 (RE-2)
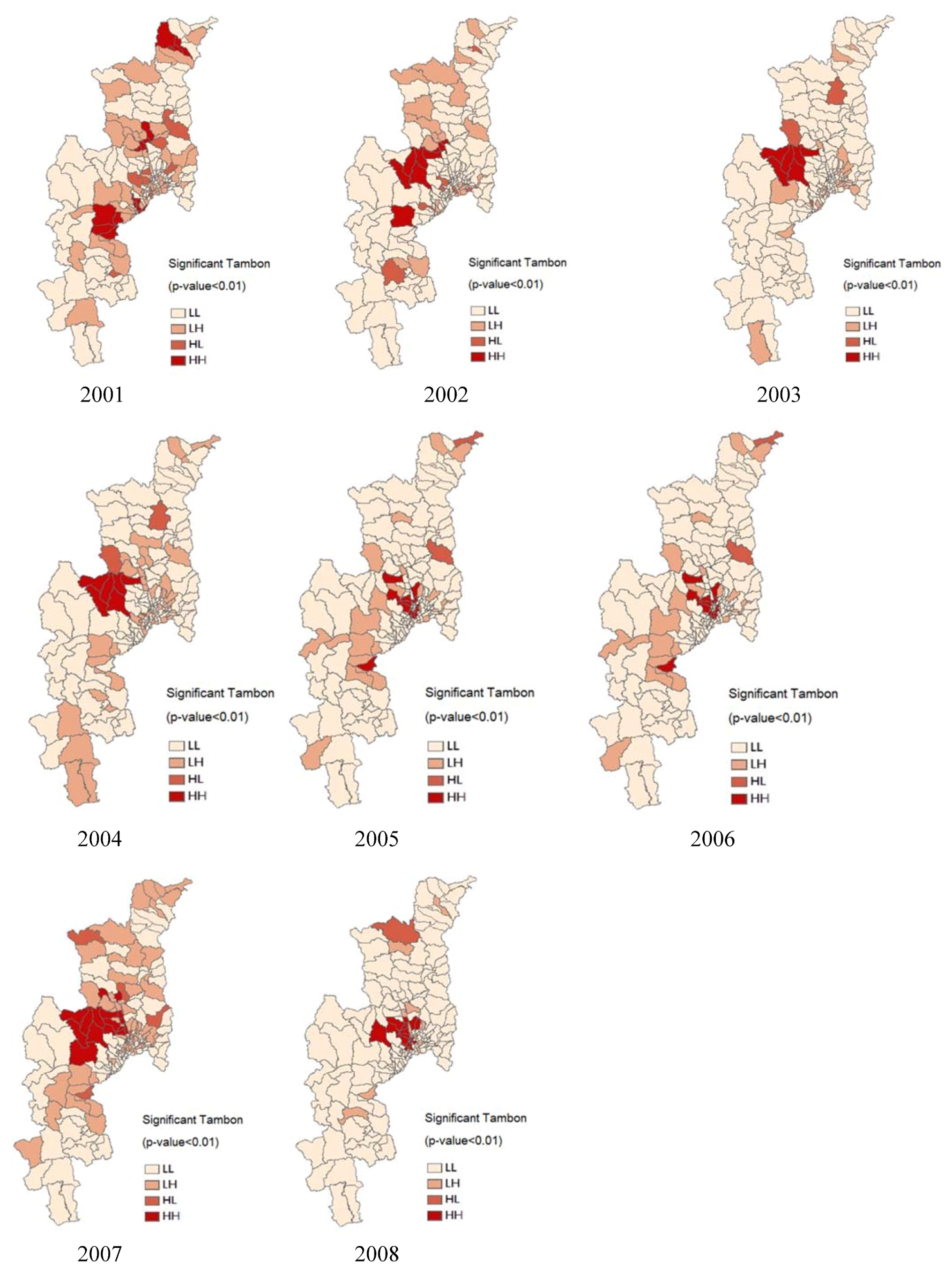
3.2.3. Spatial Analysis

| Year | IMR | Pattern | |
|---|---|---|---|
| Moran’s I | Z (I) | ||
| 2001 | 0.02 | 6.26 | Clustered |
| 2002 | 0.08 | 19.08 | Clustered |
| 2003 | 0.07 | 16.08 | Clustered |
| 2004 | 0.06 | 14.76 | Clustered |
| 2005 | 0.08 | 18.12 | Clustered |
| 2006 | 0.08 | 18.11 | Clustered |
| 2007 | 0.05 | 12.18 | Clustered |
| 2008 | 0.08 | 19.36 | Clustered |
3.3. Influenza Risk Zone Map Detection
4. Discussion
5. Conclusions
Acknowledgments
References
- World Health Organization (WHO), Using Climate to Predict Infectious Disease Outbreak: A Review; WHO: Geneva, Switzerland, 2004.
- Patz, J.A.; McCarty, J.P.; Hussein, S.; Confalonieri, U.; de Wet, N. Climate Change and Infectious Disease; World Health Organization (WHO): Geneva, Switzerland, 2003. [Google Scholar]
- World Health Organization (WHO), Dengue Haemorrhagic Fever: Diagnosis, Treatment, Prevention and Control, 2nd edWHO: Geneva, Switzerland, 2002.
- World Health Organization (WHO), Social Mobilization and Communication for Dengue Fever Prevention and Control: A Guide on Achieving and Sustaining Behavioral Results; WHO: Geneva, Switzerland, 2002.
- World Health Organization (WHO). Influenza (Seasonal), 2009. Available online: http://www.who.int/mediacentre/factsheets/fs211/en/index.html (accessed on 24 January 2009).
- Kovats, R.S. El Niño and Human Health; World Health Organization (WHO): Geneva, Switzerland, 2000; pp. 1127–1135. [Google Scholar]
- Bangs, M.J.; Larasati, R.P.; Corwin, A.L.; Wuryadi, S. Climatic factors associated with epidemic dengue in palembang, indonesia: Implications of short-term meteorological events on virus transmission. Southeast Asian J. Trop. Med. Public Health 2006, 37, 1103–1116. [Google Scholar]
- Tamerius, J.; Nelson, M.I.; Zhou, S.Z.; Viboud, C.; Miller, M.A.; Alonso, W.J. Global influenza seasonality: Reconciling patterns across temperate and tropical regions. Environ. Health Perspect. 2011, 119, 439–445. [Google Scholar]
- Brankston, G.; Gitterman, L.; Hirji, Z.; Lemieux, C.; Gardam, M. Transmission of influenza a in human beings. Lancet Infect. Dis. 2007, 7, 257–265. [Google Scholar]
- Hemmes, J.H.; Winkler, K.C.; Kool, S.M. Virus survival as a seasonal factor in influenza and poliomylitis. Antonievan Leeuwenhoek 1962, 28, 221–233. [Google Scholar] [CrossRef]
- Anderson, R.N. Deaths: Leading causes for 2000. Natl. Vital. Stat. Rep. 2002, 50, 1–85. [Google Scholar]
- Urashima, M. A seasonal model to simulate influenza oscillation in tokyo. Jpn. J. Infect. Dis. 2003, 56, 15–64. [Google Scholar]
- Nicholson, K.J.; Wood, J.M.; Zambon, M. Influenza. Lancet 2003, 362, 1733–1745. [Google Scholar]
- Inouye, S.; Matsudaira, Y.; Sugihara, Y. Marks for influenza patients: Measurement of airflow from the mouth. Jpn. J. Infect. Dis. 2006, 59, 179–181. [Google Scholar]
- Miyamoto, H. Study on the analysis of active dynamic surveillance of influenza and the pandemic prediction; Functional Empowerment Examination Regional Health Inst. Scientific EBM: Okinawa, Japan, 2001; pp. 18–27. [Google Scholar]
- Miyamoto, H. Analysis of active dynamic surveillance of influenza and the pandemic prediction. Jpn. J. Public Health 2003, 50, 18–25. [Google Scholar]
- Epidemiology Surveillance Report; Chiang Mai Provincial Public Health Office: Chiang Mai, Thailand, 2008.
- Chumkiew, S.; Srisang, W.; Jaroensutasinee, M.; Jaroensutasinee, K. Climate factors affecting on influenza cases in nakhon si thammarat. World Academy of Science, Engineering and Technology 2007, 36, 19–22. [Google Scholar]
- Hanshaoworakul, W.; Simmerman, J.M.; Narueponjirakul, U.; Sanasuttipun, W.; Shinde, V.; Kaewchana, S.; Areechokechai, D.; Levy, J.; Ungchusak, K. Severe human influenza infections in Thailand: Oseltamivir treatment and risk factors for fatal outcome. PLoSONE 2009, 4, 1–7. [Google Scholar]
- Davis, R.E.; Rossier, C.E.; Enfield, K.B. The impact of weather on influenza and pneumonia mortality in New York city, 1975–2002: A retrospective study. PLoSONE 2012, 7, e34091. [Google Scholar]
- Mondini, A.; Chiaravalloti-Neto, F. Spatial correlation of incidence of dengue with socioeconomic, demographic and environmental variables in a brazilian city. Sci. Total Environ. 2008, 393, 241–248. [Google Scholar]
- Ruankaew, N. Gis and epidemiology. J. Med. Assoc. Thailand 2005, 88, 1735–1738. [Google Scholar]
- Si, Y.L.; Debba, P.; Skidmore, A.K.; Toxopeus, A.G.; Li, L. Spatial and temporal patterns of global H5N1 outbreaks. Int. Arch. Photogram Rem. Sens. Spatial Inform. Sci. 2008, 1117, 69–74. [Google Scholar]
- Chiangmai Database; Chiang Mai Provincial Office: Chiang Mai, Thailand, 2008.
- Chaikaew, N.; Tripathi, N.K.; Souris, M. Exploring spatial patterns and hotspots of diarrhea in Chiang Mai, Thailand. Int. J. Health Geogr. 2009, 8, 36. [Google Scholar]
- Jeefoo, P.; Tripathi, N.K.; Souris, M. Spatio-temporal diffusion pattern and hotspot detection of dengue in Chachoengsao Province, Thailand. Int. J. Environ. Res. Public Health 2010, 8, 51–74. [Google Scholar]
- Epidemiology Surveillance Report, 2006. Available online: http://61.19.145.137/cmpho_web/epe_web/ (assessed on 24 August 2007). Chiang Mai Provincial Public Health Office.
- Wenger, J.B.; Naumova, E.N. Seasonal synchronization of influenza in the United States older adult population. PLoS ONE 2010, 5, e10187. [Google Scholar]
- Marshall, R. Mapping disease and mortality rates using empirical bayes estimators. J. Appl. Statist. 1991, 40, 283–294. [Google Scholar]
- Fisher, N.I.; Lewis, T.; Embleton, B.J. Statistical Analysis of Spherical Data; Cambridge University Press: Cambridge, UK, 1987. [Google Scholar]
- Legates, D.R.; Willmott, C.J. Mean seasonal and spatial variability in global surface air temperature. Theor. Appl. Climatol. 1990, 41, 11–21. [Google Scholar] [CrossRef]
- Nakhapakorn, K.; Jirakajohnkool, S. Temporal and spatial autocorrelation statistics of dengue fever. Dengue Bull. 2006, 30, 177–183. [Google Scholar]
- Nakhapakorn, K.; Tripathi, N.K. An information value based analysis of physical and climatic factors affecting dengue fever and dengue hemorrhagic fever incidence. Int. J. Health Geogr. 2005, 4, 13. [Google Scholar] [CrossRef] [Green Version]
- Curriero, F.C.; Patz, J.A.; Rose, J.B.; Subhash, L. The association between extreme precipitation and waterborne disease outbreaks in the united states, 1948–1994. Am. J. Public Health 2001, 91, 1194–1199. [Google Scholar] [CrossRef]
- Cliff, A.; Haggett, P.; Ord, J. Spatial Aspects of Influenza Epidemics; Page Bros.: London, UK, 1986. [Google Scholar]
- Pyle, G.F. The Diffusion of Influenza; Rowland & Littlefield: New Jersey, NJ, USA, 1986. [Google Scholar]
- Curmen, M.; Devid, T. Winter mortality, temperature and influenza: Has the relationship changed in recent years? Popul. Trends 1988, 54, 17–20. [Google Scholar]
- Mims, C.; Dockrell, H.; Goering, R.; Roitt, I.; Wakelin, I.; Zuckerman, M. Medical Microbiology, 3rd ed; Mosby: New York, NY, USA, 2004. [Google Scholar]
- McMicheal, A.J.; Campbell-Lendrum, D.H.; Corvalan, C.F.; Ebi, K.L.; Githeko, A.K.; Scheraga, J.D.; Woodward, A. Climate Change and Human Health: Risks and Responses; World Health Organization (WHO): Geneva, Switzerland, 2003. [Google Scholar]
- Anselin, L. Exploring Spatial Data with GeoDaTM: A Workbook; Spatial Analysis Laboratory, Department of Geography, University of Illinois at Urbana-Champaign: Champaign, IL, USA, 2005. [Google Scholar]
- Scott, L.M.; Janikas, M.V. Spatial Statistics in Arcgis; Springer: Berlin, Germany, 2010. [Google Scholar]
- Cooper, D.L.; Smith, G.E.; Regan, M.; Large, S.; Groenewegen, P.P. Tracking the spatial diffusion of influenza and norovirus using telehealth data: A spatiotemporal analysis of syndromic data. BMC Med. 2008, 6, 1–14. [Google Scholar] [CrossRef]
- Goodchild, M.F. Spatial Autocorrelation, Concept and Techniques in Modern Geography; Geo Books: Norwich, UK, 1986. [Google Scholar]
- Lee, J.; Wong, D.W.S. Statistical Analysis with Arcview GIS; John Wiley & Sons Ltd.: New York, NY, USA, 2001. [Google Scholar]
- Pathirana, S.; Kawabata, M.; Goonatilake, R. Study of potential risk of dengue disease outbreak in srilanka using gis and statistical modelling. J. Rural Trop. Public Health 2009, 8, 8–17. [Google Scholar]
- Warren-Gash, C.; Bhaskaran, K.; Hayward, A.; Leung, G.M.; Lo, S.-V.; Wong, C.-M.; Ellis, J.; Pebody, R.; Smeeth, L.; Cowling, B.J. Circulating influenza virus, climatic factors and acute myocardial infarction: A time series study in england & wales and hong kong. JID 2011, 203, 1710–1718. [Google Scholar] [CrossRef]
- Baumgarten, E.A; Dao, C.N.; Nasreen, S.; Bhuiyan, M.U.; Mah-E-Muneer, S.; Mamun, A.A.; Sharker, M.A.Y.; Zaman, R.U.; Cheng, P.-Y.; Klimov, A.I.; et al. Seasonality, timing and climatic drivers of influenza activity worldwide. JID 2012, 206, 838–846. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Nakapan, S.; Tripathi, N.K.; Tipdecho, T.; Souris, M. Spatial Diffusion of Influenza Outbreak-Related Climate Factors in Chiang Mai Province, Thailand. Int. J. Environ. Res. Public Health 2012, 9, 3824-3842. https://doi.org/10.3390/ijerph9113824
Nakapan S, Tripathi NK, Tipdecho T, Souris M. Spatial Diffusion of Influenza Outbreak-Related Climate Factors in Chiang Mai Province, Thailand. International Journal of Environmental Research and Public Health. 2012; 9(11):3824-3842. https://doi.org/10.3390/ijerph9113824
Chicago/Turabian StyleNakapan, Supachai, Nitin Kumar Tripathi, Taravudh Tipdecho, and Marc Souris. 2012. "Spatial Diffusion of Influenza Outbreak-Related Climate Factors in Chiang Mai Province, Thailand" International Journal of Environmental Research and Public Health 9, no. 11: 3824-3842. https://doi.org/10.3390/ijerph9113824




