Evolution and Control of COVID-19 Epidemic in Hong Kong
Abstract
:1. Introduction
2. Global Epidemiology of COVID-19
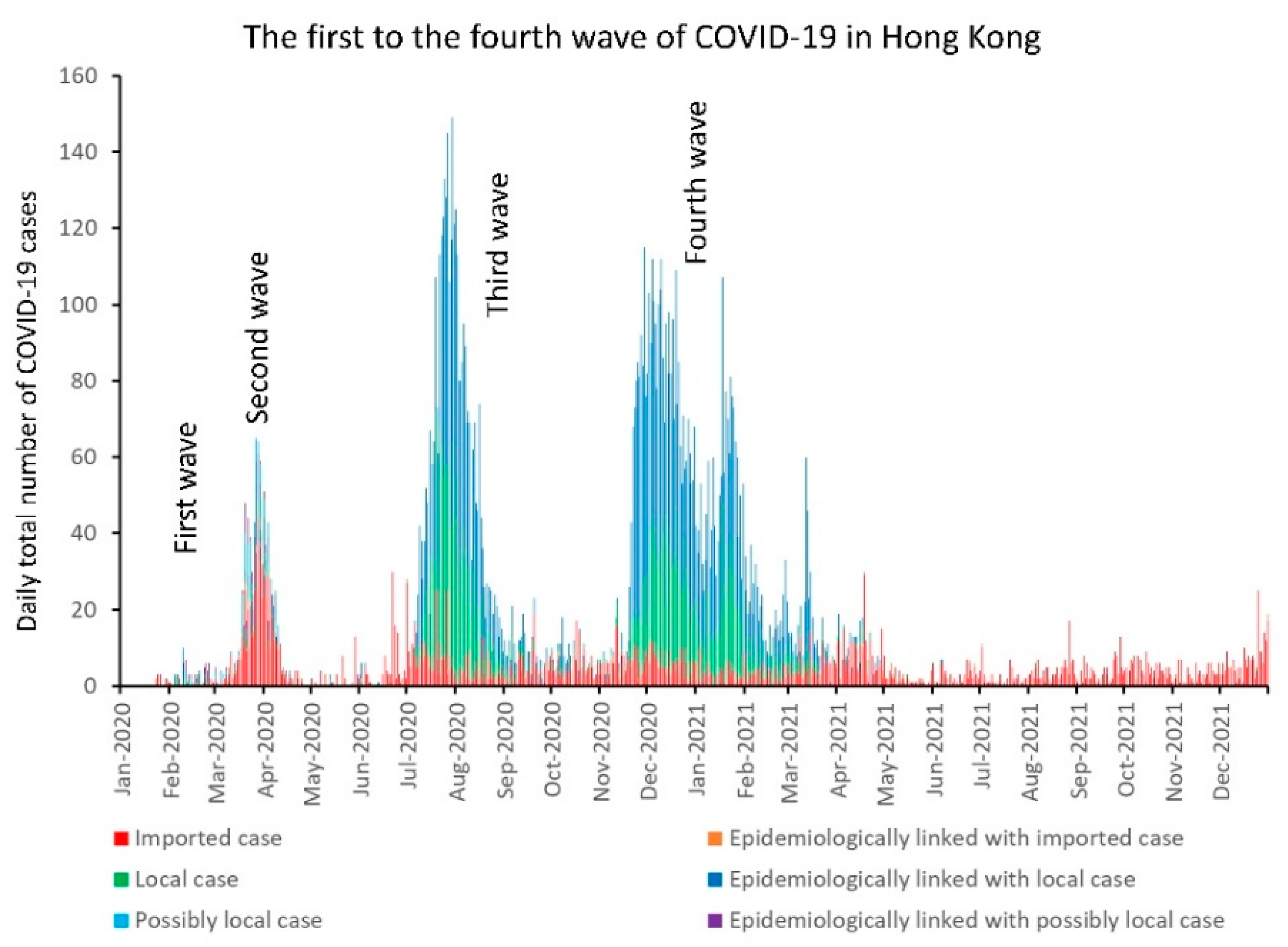
3. Epidemiology of COVID-19 in Hong Kong
4. Evolving SARS-CoV-2 VOCs in Hong Kong
5. Infection Control and Preparedness for COVID-19 in Hong Kong
5.1. Background
5.2. Infection Control for COVID-19 in the Hospitals
5.2.1. Active Surveillance
5.2.2. Training of Healthcare Workers
5.2.3. Environmental Control
5.2.4. Air Sampling for SARS-CoV-2 RNA
5.3. Relieving the Burden of COVID-19 Patients in the Hospitals
5.3.1. Proactive Screening of High-Risk Groups in Quarantine Centers
5.3.2. Setting Up Temporary Test Centers for Suspected COVID-19 Patients
5.3.3. Setting Up Community Isolation and Treatment Facilities for COVID-19 Patients
5.4. COVID-19 Infection among Healthcare Workers
6. Public Health Measures for COVID-19 in Hong Kong
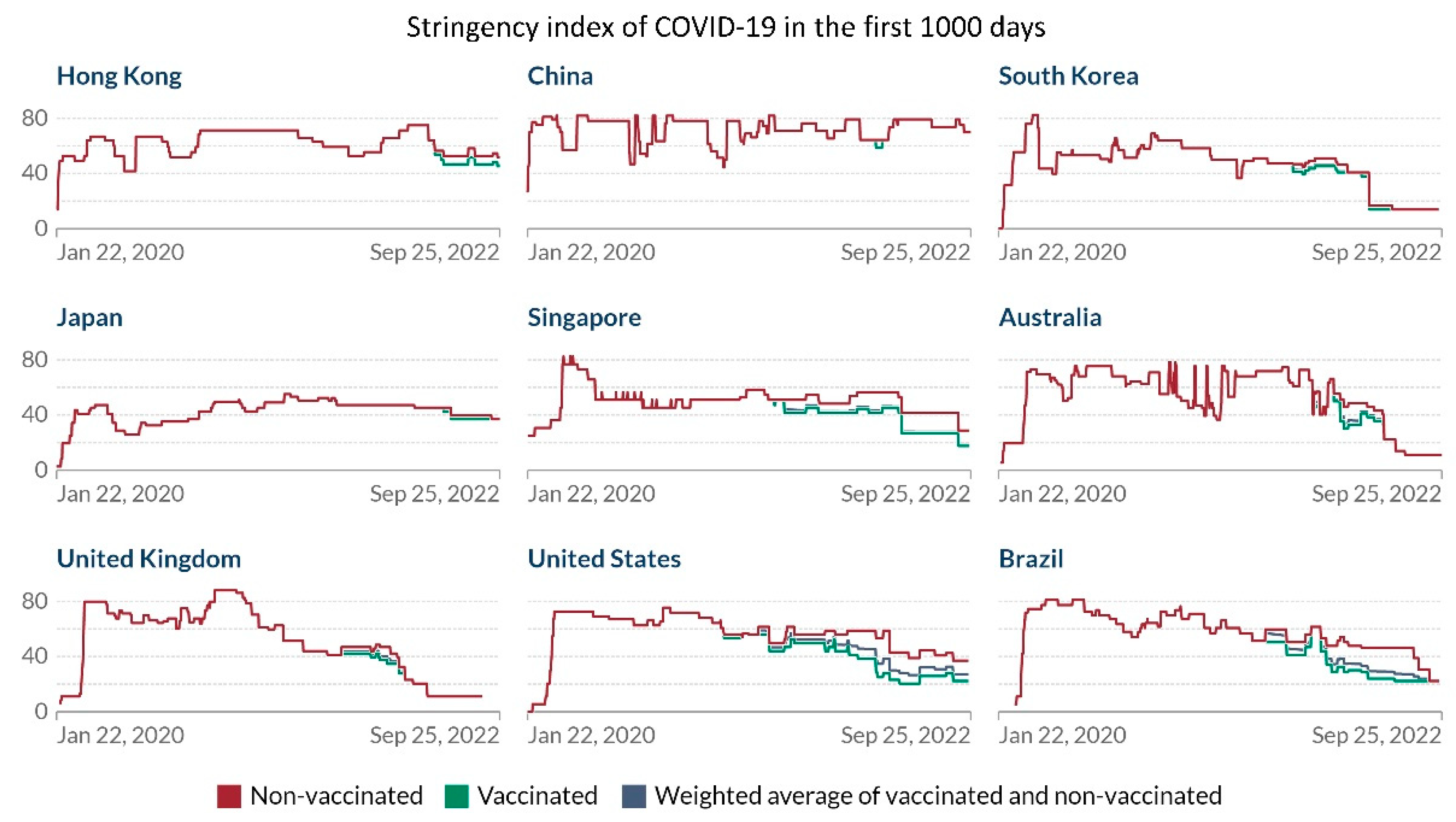
6.1. Background
6.2. Universal Masking and Social Distancing for COVID-19
6.3. Quarantine Measures for Inbound Travelers
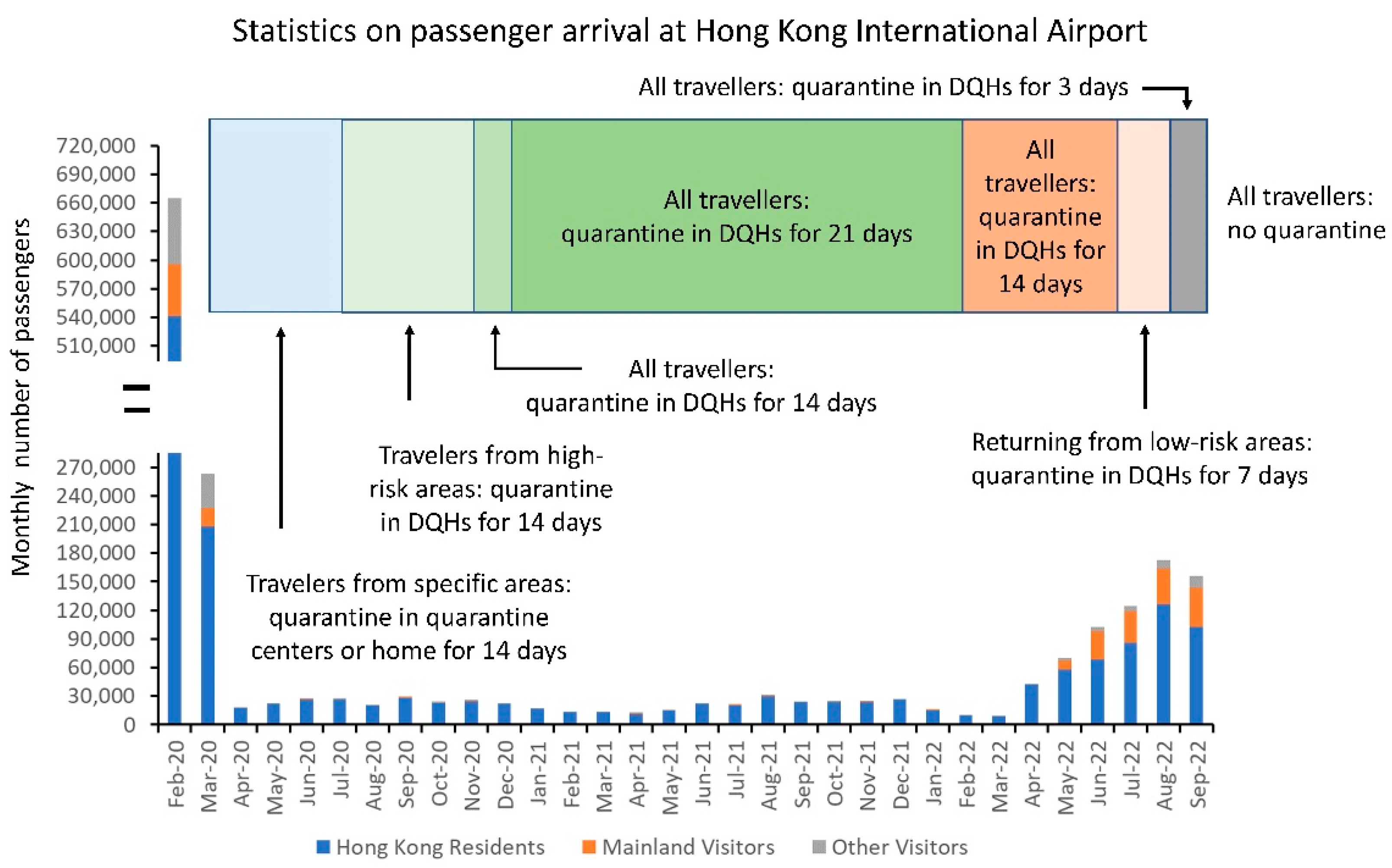
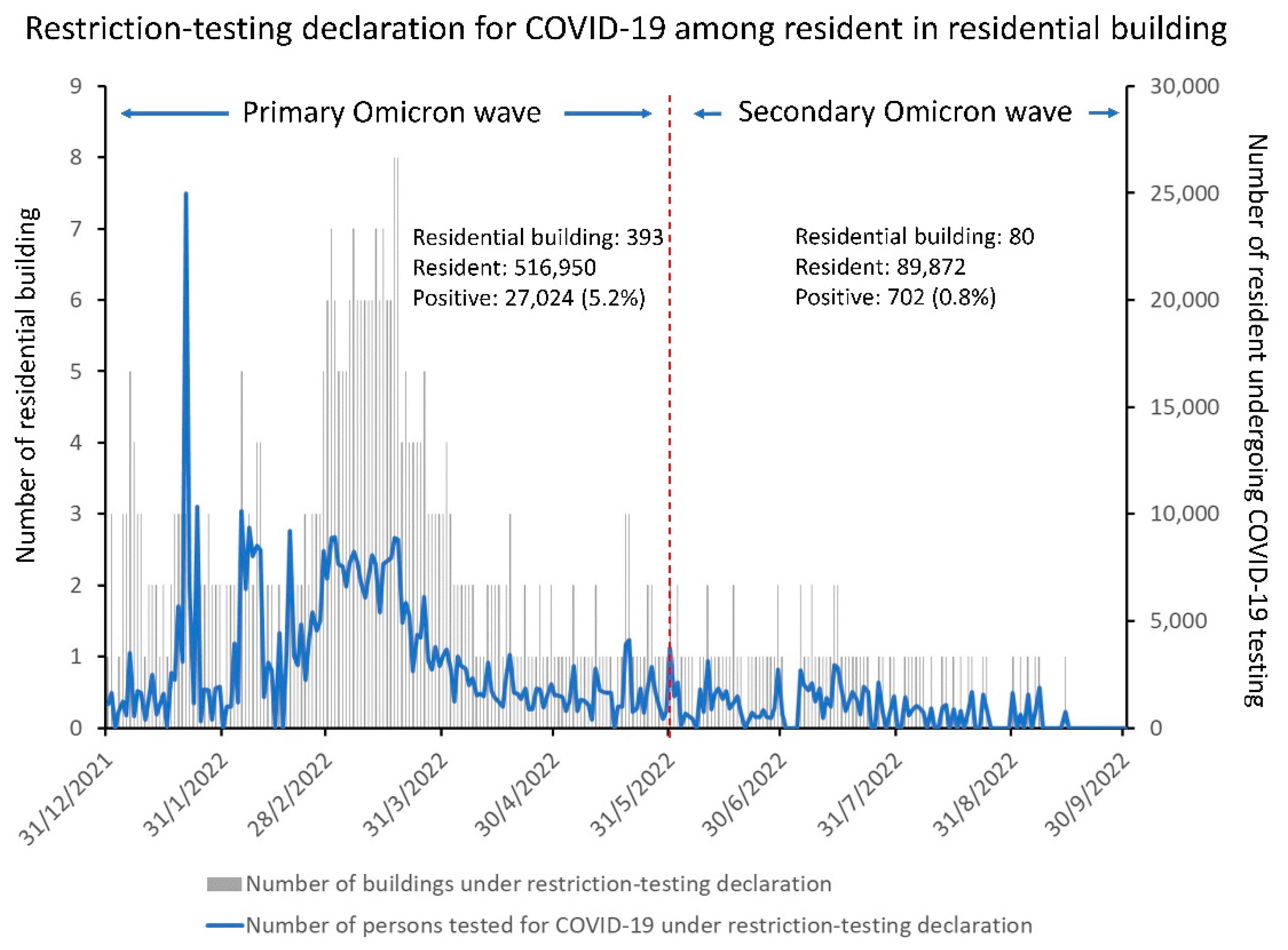
6.4. Extensive COVID-19 Testing in the Community
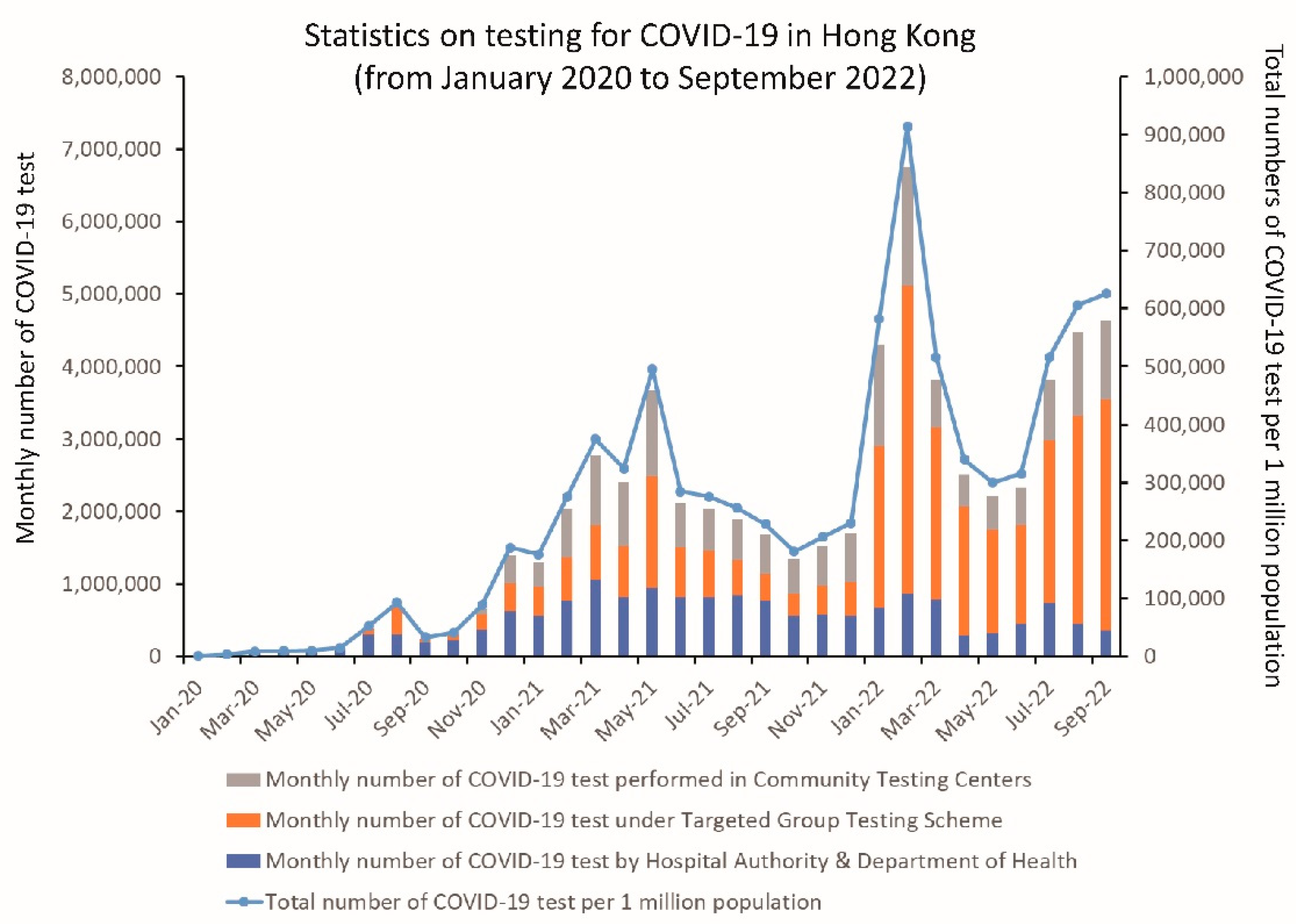
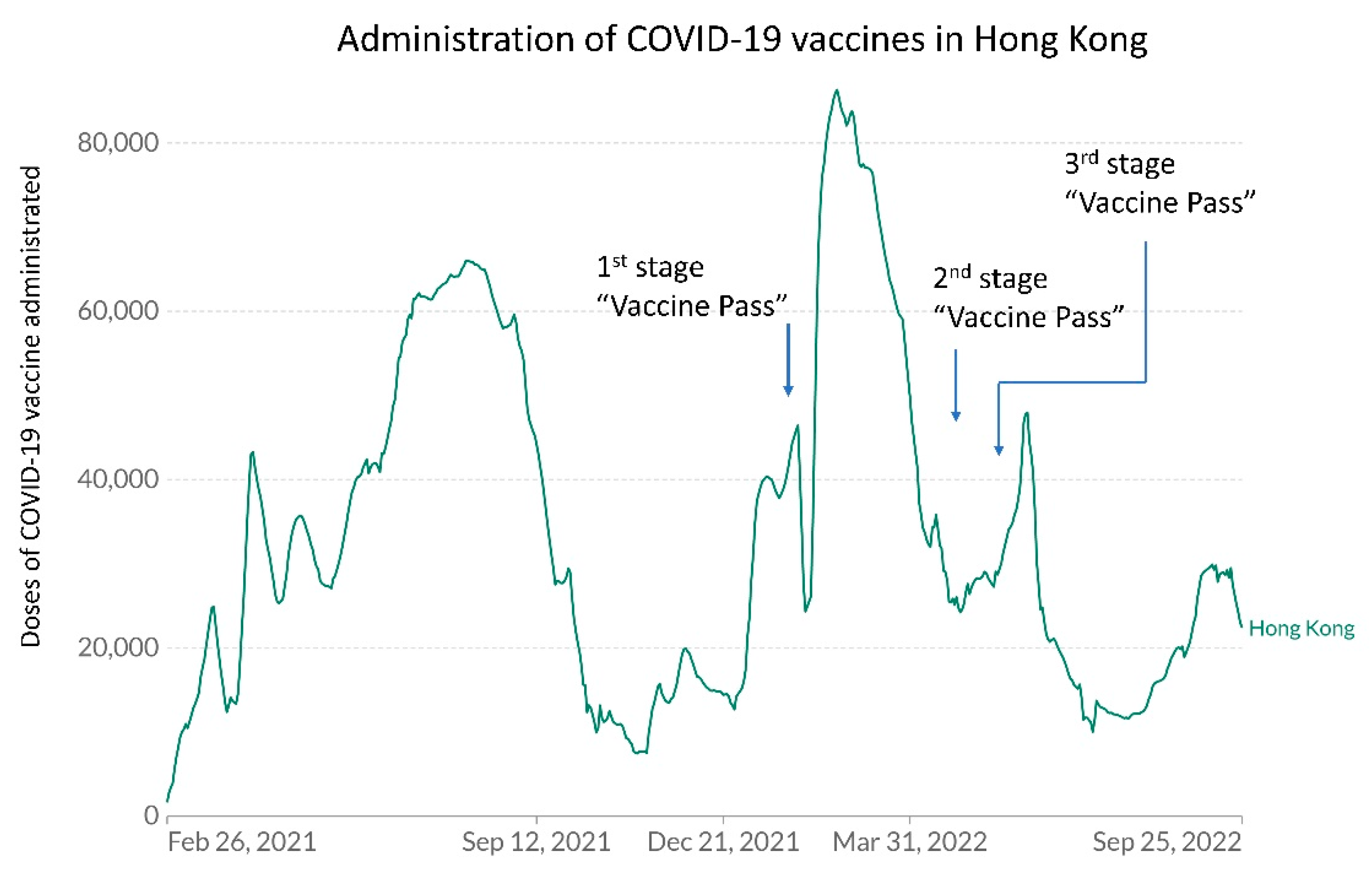
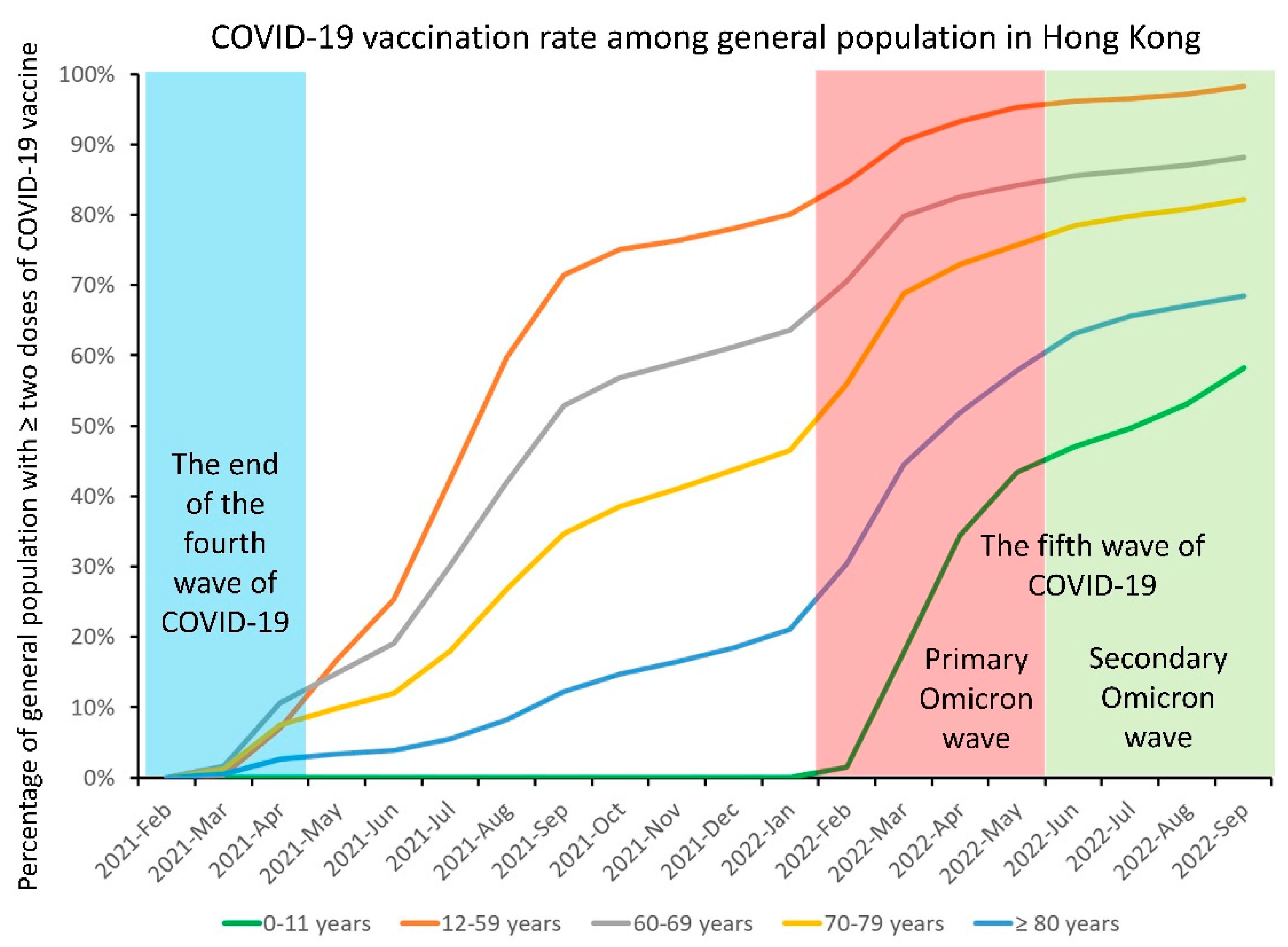
6.5. COVID-19 Vaccination in the Community
6.6. Other Non-Pharmaceutical Intervention in the Community
7. The Way Forward
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morens, D.M.; Fauci, A.S. Emerging Pandemic Diseases: How We Got to COVID-19. Cell 2020, 182, 1077–1092. [Google Scholar] [CrossRef] [PubMed]
- Raoult, D.; Mouffok, N.; Bitam, I.; Piarroux, R.; Drancourt, M. Plague: History and contemporary analysis. J. Infect. 2013, 66, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Butler, T. Plague into the 21st century. Clin. Infect. Dis. 2009, 49, 736–742. [Google Scholar] [CrossRef] [Green Version]
- Taubenberger, J.K.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15–22. [Google Scholar] [CrossRef]
- Bootsma, M.C.; Ferguson, N.M. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc. Natl. Acad. Sci. USA 2007, 104, 7588–7593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Honigsbaum, M. Revisiting the 1957 and 1968 influenza pandemics. Lancet 2020, 395, 1824–1826. [Google Scholar] [CrossRef]
- Jester, B.J.; Uyeki, T.M.; Jernigan, D.B. Fifty Years of Influenza A(H3N2) Following the Pandemic of 1968. Am. J. Public Health 2020, 110, 669–676. [Google Scholar] [CrossRef]
- Cheng, V.C.; To, K.K.; Tse, H.; Hung, I.F.; Yuen, K.-Y. Two years after pandemic influenza A/2009/H1N1: What have we learned? Clin. Microbiol. Rev. 2012, 25, 223–263. [Google Scholar] [CrossRef] [Green Version]
- Dawood, F.S.; Iuliano, A.D.; Reed, C.; Meltzer, M.I.; Shay, D.K.; Cheng, P.Y.; Bandaranayake, D.; Breiman, R.F.; Brooks, W.A.; Buchy, P.; et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: A modelling study. Lancet Infect. Dis. 2012, 12, 687–695. [Google Scholar] [CrossRef] [Green Version]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Rajendran, M.; Nachbagauer, R.; Ermler, M.E.; Bunduc, P.; Amanat, F.; Izikson, R.; Cox, M.; Palese, P.; Eichelberger, M.; Krammer, F. Analysis of Anti-Influenza Virus Neuraminidase Antibodies in Children, Adults, and the Elderly by ELISA and Enzyme Inhibition: Evidence for Original Antigenic Sin. mBio 2017, 8, e02281-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulabbi, E.N.; Tweyongyere, R.; Byarugaba, D.K. The history of the emergence and transmission of human coronaviruses. Onderstepoort. J. Vet. Res. 2021, 88, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- van der Hoek, L.; Pyrc, K.; Jebbink, M.F.; Vermeulen-Oost, W.; Berkhout, R.J.; Wolthers, K.C.; Wertheim-van Dillen, P.M.; Kaandorp, J.; Spaargaren, J.; Berkhout, B. Identification of a new human coronavirus. Nat. Med. 2004, 10, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Woo, P.C.; Lau, S.K.; Chu, C.-M.; Chan, K.-H.; Tsoi, H.-W.; Huang, Y.; Wong, B.H.; Poon, R.W.; Cai, J.J.; Luk, W.-K.; et al. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J. Virol. 2005, 79, 884–895. [Google Scholar] [CrossRef] [Green Version]
- Cheng, V.C.; Lau, S.K.; Woo, P.C.; Yuen, K.-Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin. Microbiol. Rev. 2007, 20, 660–694. [Google Scholar] [CrossRef] [Green Version]
- Chan, J.F.; Lau, S.K.; To, K.K.; Cheng, V.C.; Woo, P.C.; Yuen, K.-Y. Middle East respiratory syndrome coronavirus: Another zoonotic betacoronavirus causing SARS-like disease. Clin. Microbiol. Rev. 2015, 28, 465–522. [Google Scholar] [CrossRef] [Green Version]
- Bloom, D.E.; Cadarette, D. Infectious Disease Threats in the Twenty-First Century: Strengthening the Global Response. Front. Immunol. 2019, 10, 549. [Google Scholar] [CrossRef] [Green Version]
- Honigsbaum, M. Disease X and other unknowns. Lancet 2019, 393, 1496–1497. [Google Scholar] [CrossRef]
- Van Kerkhove, M.D.; Ryan, M.J.; Ghebreyesus, T.A. Preparing for “Disease X”. Science 2021, 374, 377. [Google Scholar] [CrossRef]
- Jiang, S.; Shi, Z.L. The First Disease X is Caused by a Highly Transmissible Acute Respiratory Syndrome Coronavirus. Virol. Sin. 2020, 35, 263–265. [Google Scholar] [CrossRef]
- The Centre for Health Protection Closely Monitors Cluster of Pneumonia Cases on Mainland. Press Release of the Department of Health, Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm (accessed on 1 October 2022).
- Cheng, V.C.-C.; Wong, S.-C.; To, K.K.-W.; Ho, P.-L.; Yuen, K.-Y. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J. Hosp. Infect. 2020, 104, 254–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Delaune, D.; Hul, V.; Karlsson, E.A.; Hassanin, A.; Ou, T.P.; Baidaliuk, A.; Gámbaro, F.; Prot, M.; Tu, V.T.; Chea, S.; et al. A novel SARS-CoV-2 related coronavirus in bats from Cambodia. Nat. Commun. 2021, 12, 6563. [Google Scholar] [CrossRef]
- Lam, T.T.; Jia, N.; Zhang, Y.W.; Shum, M.H.; Jiang, J.F.; Zhu, H.C.; Tong, Y.G.; Shi, Y.X.; Ni, X.B.; Liao, Y.S.; et al. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 2020, 583, 282–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Temmam, S.; Vongphayloth, K.; Baquero, E.; Munier, S.; Bonomi, M.; Regnault, B.; Douangboubpha, B.; Karami, Y.; Chrétien, D.; Sanamxay, D.; et al. Bat coronaviruses related to SARS-CoV-2 and infectious for human cells. Nature 2022, 604, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Lau, S.K.; Woo, P.C.; Li, K.S.; Huang, Y.; Tsoi, H.-W.; Wong, B.H.; Wong, S.S.; Leung, S.-Y.; Chan, K.-H.; Yuen, K.-Y. Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proc. Natl. Acad. Sci. USA 2005, 102, 14040–14045. [Google Scholar] [CrossRef] [Green Version]
- Lau, S.K.; Chan, J.F. Coronaviruses: Emerging and re-emerging pathogens in humans and animals. Virol. J. 2015, 12, 209. [Google Scholar] [CrossRef] [Green Version]
- Coronavirus Disease (COVID-19) Pandemic, World Health Organization. Available online: https://www.who.int/europe/emergencies/situations/covid-19 (accessed on 1 October 2022).
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-51. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 (accessed on 1 October 2022).
- COVID-19 Weekly Epidemiological Update, Edition 111 Published 28 September 2022, World Health Organization. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---28-september-2022 (accessed on 1 October 2022).
- Lockdowns Compared: Tracking Governments’ Coronavirus Responses. Financial Times. Available online: https://ig.ft.com/coronavirus-lockdowns/ (accessed on 1 October 2022).
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104, 368504211019854. [Google Scholar] [CrossRef]
- Countries by Population Density. Available online: https://worldpopulationreview.com/country-rankings/countries-by-density (accessed on 1 October 2022).
- Tracking SARS-CoV-2 Variants, World Health Organization. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 1 October 2022).
- Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update, World Health Organization. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 2 October 2022).
- COVID-19 Situation Update Worldwide. European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 2 October 2022).
- COVID-19 Dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. Available online: https://coronavirus.jhu.edu/map.html (accessed on 2 October 2022).
- COVID-19 Coronavirus Pandemic, Worldmeter. Available online: https://www.worldometers.info/coronavirus/ (accessed on 2 October 2022).
- Coronavirus Pandemic (COVID-19), Our World in Data. Available online: https://ourworldindata.org/coronavirus (accessed on 2 October 2022).
- Coronavirus World Map: Tracking the Global Outbreak, The New York Times. Available online: https://www.nytimes.com/interactive/2021/world/covid-cases.html (accessed on 2 October 2022).
- Covid Map: Coronavirus Cases, Deaths, Vaccinations by Country, BBC News. Available online: https://www.bbc.com/news/world-51235105 (accessed on 2 October 2022).
- COVID-19 (SARS-CoV-2 Coronavirus), American Society for Microbiology. Available online: https://asm.org/Resource-Pages/COVID-19-Resources (accessed on 2 October 2022).
- Davies, N.G.; Abbott, S.; Barnard, R.C.; Jarvis, C.I.; Kucharski, A.J.; Munday, J.D.; Pearson, C.A.B.; Russell, T.W.; Tully, D.C.; Washburne, A.D.; et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science 2021, 372, eabg3055. [Google Scholar] [CrossRef]
- Volz, E.; Mishra, S.; Chand, M.; Barrett, J.C.; Johnson, R.; Geidelberg, L.; Hinsley, W.R.; Laydon, D.J.; Dabrera, G.; O’Toole, Á.; et al. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature 2021, 593, 266–269. [Google Scholar] [CrossRef]
- Earnest, R.; Uddin, R.; Matluk, N.; Renzette, N.; Turbett, S.E.; Siddle, K.J.; Loreth, C.; Adams, G.; Tomkins-Tinch, C.H.; Petrone, M.E.; et al. Comparative transmissibility of SARS-CoV-2 variants Delta and Alpha in New England, USA. Cell. Rep. Med. 2022, 3, 100583. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; Piantham, C.; Nishiura, H. Relative instantaneous reproduction number of Omicron SARS-CoV-2 variant with respect to the Delta variant in Denmark. J. Med. Virol. 2022, 94, 2265–2268. [Google Scholar] [CrossRef] [PubMed]
- Jalali, N.; Brustad, H.K.; Frigessi, A.; MacDonald, E.A.; Meijerink, H.; Feruglio, S.L.; Nygård, K.M.; Rø, G.; Madslien, E.H.; de Blasio, B.F. Increased household transmission and immune escape of the SARS-CoV-2 Omicron compared to Delta variants. Nat. Commun. 2022, 13, 5706. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Thematic Website. Centre for Health Protection. Department of Health, The Government of the Hong Kong Special Administrative Region. Available online: https://www.coronavirus.gov.hk/eng/index.html (accessed on 2 October 2022).
- Cheng, V.C.; Wong, S.-C.; Au, A.K.; Zhang, C.; Chen, J.H.; So, S.Y.; Li, X.; Wang, Q.; Lu, K.K.; Lung, D.C.; et al. Explosive outbreak of SARS-CoV-2 Omicron variant is associated with vertical transmission in high-rise residential buildings in Hong Kong. Build. Environ. 2022, 221, 109323. [Google Scholar] [CrossRef]
- Gu, H.; Chu, D.K.-W.; Chang, L.D.-J.; Cheuk, S.S.-Y.; Gurung, S.; Krishnan, P.; Ng, D.Y.-M.; Liu, G.Y.-Z.; Wan, C.K.-C.; Xie, R.; et al. Genetic Diversity of SARS-CoV-2 among Travelers Arriving in Hong Kong. Emerg. Infect. Dis. 2021, 27, 2666–2668. [Google Scholar] [CrossRef]
- Leung, K.S.; Ng, T.T.; Wu, A.K.; Yau, M.C.; Lao, H.-Y.; Choi, M.-P.; Tam, K.K.; Lee, L.-K.; Wong, B.K.; Ho, A.Y.; et al. Territorywide Study of Early Coronavirus Disease Outbreak, Hong Kong, China. Emerg. Infect. Dis. 2021, 27, 196–204. [Google Scholar] [CrossRef]
- Chan, W.-M.; Ip, J.D.; Chu, A.W.; Tse, H.; Tam, A.R.; Li, X.; Kwan, M.Y.; Yau, Y.-S.; Leung, W.-S.; Chik, T.S.; et al. Phylogenomic analysis of COVID-19 summer and winter outbreaks in Hong Kong: An observational study. Lancet Reg. Health West Pac. 2021, 10, 100130. [Google Scholar] [CrossRef]
- Gu, H.; Cheng, S.S.-M.; Krishnan, P.; Ng, D.Y.-M.; Chang, L.D.-J.; Liu, G.Y.-Z.; Cheuk, S.S.-Y.; Hui, M.M.-Y.; Fan, M.C.-Y.; Wan, J.H.-L.; et al. Monitoring International Travelers Arriving in Hong Kong for Genomic Surveillance of SARS-CoV-2. Emerg. Infect. Dis. 2022, 28, 247–250. [Google Scholar] [CrossRef]
- Cheng, V.C.-C.; Ip, J.D.; Chu, A.W.-H.; Tam, A.R.; Chan, W.-M.; Abdullah, S.M.-U.; Chan, B.P.-C.; Wong, S.-C.; Kwan, M.Y.-W.; Chua, G.T.; et al. Rapid Spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Omicron Subvariant BA.2 in a Single-Source Community Outbreak. Clin. Infect. Dis. 2022, 75, e44–e49. [Google Scholar] [CrossRef]
- Chan, J.F.-W.; Siu, G.K.-H.; Yuan, S.; Ip, J.D.; Cai, J.-P.; Chu, A.W.-H.; Chan, W.-M.; Abdullah, S.M.-U.; Luo, C.; Chan, B.P.-C.; et al. Probable Animal-to-Human Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Delta Variant AY.127 Causing a Pet Shop-Related Coronavirus Disease 2019 (COVID-19) Outbreak in Hong Kong. Clin. Infect. Dis. 2022, 75, e76–e81. [Google Scholar] [CrossRef]
- Kok, K.-H.; Wong, S.-C.; Chan, W.-M.; Wen, L.; Chu, A.W.; Ip, J.D.; Lee, L.-K.; Wong, I.T.; Lo, H.W.; Cheng, V.C.; et al. Co-circulation of two SARS-CoV-2 variant strains within imported pet hamsters in Hong Kong. Emerg. Microbes Infect. 2022, 11, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003 (Based on Data as of the 31 December 2003). World Health Organization. Available online: https://www.who.int/csr/sars/country/table2004_04_21/en/ (accessed on 4 October 2022).
- Report of the Select Committee to Inquire into the Handling of the Severe Acute Respiratory Syndrome Outbreak by the Government and the Hospital Authority July 2004. Available online: https://www.legco.gov.hk/yr03-04/english/sc/sc_sars/reports/sars_rpt.htm (accessed on 4 October 2022).
- SARS Expert Committee. Available online: https://www.sars-expertcom.gov.hk/english/reports/reports.html (accessed on 4 October 2022).
- Benitez, M.A. Expert committee reviews SARS outbreak in Hong Kong. Lancet 2003, 362, 624. [Google Scholar] [CrossRef]
- Message from the Controller, Centre for Health Protection, Department of Health, The Government of the Hong Kong Special Administrative Region. Available online: https://www.chp.gov.hk/en/static/23993.html (accessed on 4 October 2022).
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.-C.; Wong, S.-C.; Chen, J.H.-K.; Yip, C.C.-Y.; Chuang, V.W.-M.; Tsang, O.T.-Y.; Sridhar, S.; Chan, J.F.-W.; Ho, P.-L.; Yuen, K.-Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 2020, 41, 493–498. [Google Scholar] [CrossRef] [Green Version]
- Cheng, V.C.; Wong, S.-C.; Tong, D.W.; Chuang, V.W.; Chen, J.H.; Lee, L.L.; To, K.K.; Hung, I.F.; Ho, P.-L.; Yeung, D.T.; et al. Multipronged infection control strategy to achieve zero nosocomial coronavirus disease 2019 (COVID-19) cases among Hong Kong healthcare workers in the first 300 days of the pandemic. Infect. Control Hosp. Epidemiol. 2022, 43, 334–343. [Google Scholar] [CrossRef]
- To, K.K.; Tsang, O.T.; Yip, C.C.; Chan, K.-H.; Wu, T.-C.; Chan, J.M.; Leung, W.-S.; Chik, T.S.; Choi, C.Y.; Kandamby, D.H.; et al. Consistent Detection of 2019 Novel Coronavirus in Saliva. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- To, K.K.; Tsang, O.T.; Leung, W.-S.; Tam, A.R.; Wu, T.-C.; Lung, D.C.; Yip, C.C.; Cai, J.-P.; Chan, J.M.; Chik, T.S.; et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 2020, 20, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.H.; Yip, C.C.; Poon, R.W.; Chan, K.-H.; Cheng, V.C.; Hung, I.F.; Chan, J.F.; Yuen, K.-Y.; To, K.K. Evaluating the use of posterior oropharyngeal saliva in a point-of-care assay for the detection of SARS-CoV-2. Emerg. Microbes Infect. 2020, 9, 1356–1359. [Google Scholar] [CrossRef]
- Butler-Laporte, G.; Lawandi, A.; Schiller, I.; Yao, M.; Dendukuri, N.; McDonald, E.G.; Lee, T.C. Comparison of Saliva and Nasopharyngeal Swab Nucleic Acid Amplification Testing for Detection of SARS-CoV-2: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2021, 181, 353–360. [Google Scholar] [CrossRef]
- Hung, D.L.; Li, X.; Chiu, K.H.; Yip, C.C.; To, K.K.; Chan, J.F.; Sridhar, S.; Chung, T.W.; Lung, K.-C.; Liu, R.W.; et al. Early-Morning vs Spot Posterior Oropharyngeal Saliva for Diagnosis of SARS-CoV-2 Infection: Implication of Timing of Specimen Collection for Community-Wide Screening. Open Forum Infect. Dis. 2020, 7, ofaa210. [Google Scholar] [CrossRef]
- Lynch, J.B.; Davitkov, P.; Anderson, D.J.; Bhimraj, A.; Cheng, V.C.; Guzman-Cottrill, J.; Dhindsa, J.; Duggal, A.; Jain, M.K.; Lee, G.M.; et al. Infectious Diseases Society of America Guidelines on Infection Prevention for Health Care Personnel Caring for Patients with Suspected or Known COVID-19. Clin. Infect. Dis. 2020, ciaa1063. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.B.; Davitkov, P.; Anderson, D.J.; Bhimraj, A.; Cheng, V.C.; Guzman-Cottrill, J.; Dhindsa, J.; Duggal, A.; Jain, M.K.; Lee, G.M.; et al. Infectious Diseases Society of America Guidelines on Infection Prevention for Healthcare Personnel Caring for Patients with Suspected or Known COVID-19. Clin. Infect. Dis. 2021, ciab953. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-C.; AuYeung, C.H.; Lam, G.K.; Leung, E.Y.; Chan, V.W.; Yuen, K.-Y.; Cheng, V.C. Is it possible to achieve 100 percent hand hygiene compliance during the coronavirus disease 2019 (COVID-19) pandemic? J. Hosp. Infect. 2020, 105, 779–781. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-C.; Lam, G.K.; AuYeung, C.H.; Chan, V.W.; Wong, N.L.; So, S.Y.; Chen, J.H.; Hung, I.F.; Chan, J.F.; Yuen, K.-Y.; et al. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: Implication of universal masking in hospitals. Infect. Control Hosp. Epidemiol. 2021, 42, 218–221. [Google Scholar] [CrossRef]
- Cheng, V.C.; Wong, S.-C.; Chan, V.W.; So, S.Y.; Chen, J.H.; Yip, C.C.; Chan, K.-H.; Chu, H.; Chung, T.W.; Sridhar, S.; et al. Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19). Infect. Control Hosp. Epidemiol. 2020, 41, 1258–1265. [Google Scholar] [CrossRef]
- Wu, S.; Wang, Y.; Jin, X.; Tian, J.; Liu, J.; Mao, Y. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease 2019. Am. J. Infect. Control. 2020, 48, 910–914. [Google Scholar] [CrossRef]
- Ryu, B.H.; Cho, Y.; Cho, O.H.; Hong, S.I.; Kim, S.; Lee, S. Environmental contamination of SARS-CoV-2 during the COVID-19 outbreak in South Korea. Am. J. Infect. Control. 2020, 48, 875–879. [Google Scholar] [CrossRef]
- Dancer, S.J. Reducing the risk of COVID-19 transmission in hospitals: Focus on additional infection control strategies. Surgery 2021, 39, 752–758. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020, 323, 1610–1612. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.H.; Fan, Y.Z.; Jiang, L.; Wang, H.B. Aerosol and environmental surface monitoring for SARS-CoV-2 RNA in a designated hospital for severe COVID-19 patients. Epidemiol. Infect. 2020, 148, e154. [Google Scholar] [CrossRef]
- Kim, U.J.; Lee, S.Y.; Lee, J.Y.; Lee, A.; Kim, S.E.; Choi, O.J.; Lee, J.S.; Kee, S.J.; Jang, H.C. Air and Environmental Contamination Caused by COVID-19 Patients: A Multi-Center Study. J. Korean Med. Sci. 2020, 35, e332. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.D.; Wang, Z.Y.; Zhang, S.F.; Li, X.; Li, L.; Li, C.; Cui, Y.; Fu, R.B.; Dong, Y.Z.; Chi, X.Y.; et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020, 26, 1583–1591. [Google Scholar] [CrossRef] [PubMed]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-C.; Chan, V.W.; AuYeung, C.H.; Chen, J.H.; Yip, C.C.; So, S.Y.; Li, X.; Lung, D.C.; Tsang, A.M.; To, K.K.; et al. Air dispersal of respiratory viruses other than severe acute respiratory coronavirus virus 2 (SARS-CoV-2) and the implication on hospital infection control. Infect. Control Hosp. Epidemiol. 2022, 1–6. [Google Scholar] [CrossRef]
- Wong, S.-C.; Yuen, L.L.; Chan, V.W.; Chen, J.H.; To, K.K.; Yuen, K.-Y.; Cheng, V.C. Airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): What is the implication of hospital infection control? Infect. Control Hosp. Epidemiol. 2022, 43, 1522–1523. [Google Scholar] [CrossRef]
- Wong, S.-C.; Chan, V.W.; Yuen, L.L.; Auyeung, C.H.; Leung, J.O.; Li, C.-K.; Kwok, M.O.; So, S.Y.; Chen, J.H.; Tam, A.R.; et al. Air dispersal of SARS-CoV-2 in general wards: Implication on hospital infection control during the fifth wave of COVID-19 due to Omicron variant in Hong Kong. Infect. Control Hosp. Epidemiol. 2022; accepted; in press. [Google Scholar]
- Wong, S.-C.; Lam, G.K.; Chen, J.H.; Li, X.; Ip, F.T.; Yuen, L.L.; Chan, V.W.; AuYeung, C.H.; So, S.Y.; Ho, P.-L.; et al. Air dispersal of multidrug-resistant Acinetobacter baumannii: Implications for nosocomial transmission during the COVID-19 pandemic. J. Hosp. Infect. 2021, 116, 78–86. [Google Scholar] [CrossRef]
- Wong, S.-C.; Chen, J.H.; Yuen, L.L.; Chan, V.W.; AuYeung, C.H.; Leung, S.S.; So, S.Y.; Chan, B.W.; Li, X.; Leung, J.O.; et al. Air dispersal of meticillin-resistant Staphylococcus aureus in residential care homes for the elderly: Implications for transmission during the COVID-19 pandemic. J. Hosp. Infect. 2022, 123, 52–60. [Google Scholar] [CrossRef]
- Hung, I.F.; Cheng, V.C.; Li, X.; Tam, A.R.; Hung, D.L.; Chiu, K.H.; Yip, C.C.; Cai, J.-P.; Ho, D.T.; Wong, S.-C.; et al. SARS-CoV-2 shedding and seroconversion among passengers quarantined after disembarking a cruise ship: A case series. Lancet Infect. Dis. 2020, 20, 1051–1060. [Google Scholar] [CrossRef]
- To, K.K.; Cheng, V.C.; Cai, J.-P.; Chan, K.-H.; Chen, L.L.; Wong, L.-H.; Choi, C.Y.; Fong, C.H.; Ng, A.C.; Lu, L.; et al. Seroprevalence of SARS-CoV-2 in Hong Kong and in residents evacuated from Hubei province, China: A multicohort study. Lancet Microbe. 2020, 1, e111–e118. [Google Scholar] [CrossRef]
- Temporary Test Centres Speed up Tests for People Upon Arrival, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202003/19/P2020031900664.htm (accessed on 4 October 2022).
- Wong, S.-C.; Leung, M.; Lee, L.L.; Chung, K.-L.; Cheng, V.C. Infection control challenge in setting up a temporary test centre at Hong Kong International Airport for rapid diagnosis of COVID-19 due to SARS-CoV-2. J. Hosp. Infect. 2020, 105, 571–573. [Google Scholar] [CrossRef]
- Wong, S.-C.; Leung, M.; Tong, D.W.; Lee, L.L.; Leung, W.L.; Chan, F.W.; Chen, J.H.; Hung, I.F.; Yuen, K.-Y.; Yeung, D.T.; et al. Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): Implementation of directly observed environmental disinfection. Infect. Control Hosp. Epidemiol. 2021, 42, 1037–1045. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhang, Z.; Yang, J.; Wang, J.; Zhai, X.; Bärnighausen, T.; Wang, C. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet 2020, 395, 1305–1314. [Google Scholar] [CrossRef]
- Fang, D.; Pan, S.; Li, Z.; Yuan, T.; Jiang, B.; Gan, D.; Sheng, B.; Han, J.; Wang, T.; Liu, Z. Large-scale public venues as medical emergency sites in disasters: Lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob. Health 2020, 5, e002815. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus: Singapore Expo to House First Batch of Mild Cases Tomorrow to Free Up Hospitals, Straits Times Website, Published 9 April 2020. Available online: https://www.straitstimes.com/singapore/health/spore-expo-to-house-first-batch-of-mild-cases-tomorrow-to-free-up-hospitals (accessed on 5 October 2022).
- UK Opens 4000-Bed Coronavirus Field Hospital, Deutsche Welle Website, Published 3 April 2020. Available online: https://www.dw.com/en/uk-opens-4000-bed-coronavirus-field-hospital/a-53005844 (accessed on 5 October 2022).
- Coronavirus: Wales’ 19 field Hospitals Cost £166m to Build, BBC News Website, Published 21 May 2020. Available online: https://www.bbc.com/news/uk-wales-52752976 (accessed on 5 October 2022).
- Naganathan, S.; Meehan-Coussee, K.; Pasichow, S.; Rybasack-Smith, H.; Binder, W.; Beaudoin, F.; Musits, A.N.; Sutton, E.; Petrone, G.; Levine, A.C.; et al. From Concerts to COVID: Transforming the RI Convention Center into an Alternate Hospital Site in under a Month. Rhode Isl. Med. J. 2020, 103, 8–13. [Google Scholar]
- Cheng, V.C.; Lung, D.C.; Wong, S.-C.; Au, A.K.; Wang, Q.; Chen, H.; Li, X.; Chu, A.W.; Ip, J.D.; Chan, W.-M.; et al. Outbreak investigation of airborne transmission of Omicron (B.1.1.529)-SARS-CoV-2 variant of concern in a restaurant: Implication for enhancement of indoor air dilution. J. Hazard. Mater. 2022, 430, 128504. [Google Scholar] [CrossRef]
- CE Inspects Handover of Community Isolation Facility in Penny’s Bay, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202204/19/P2022041900544.htm (accessed on 6 October 2022).
- Kai Tak Community Isolation Facility Commences Operation. Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202208/19/P2022081900552.htm?fontSize=1 (accessed on 6 October 2022).
- COVID-19 has Infected Some 570,000 health Workers and Killed 2500 in the Americas, Pan American Health Organization, World Health Organization. Available online: https://www.paho.org/en/news/2-9-2020-covid-19-has-infected-some-570000-health-workers-and-killed-2500-americas-paho (accessed on 5 October 2022).
- Bandyopadhyay, S.; Baticulon, R.E.; Kadhum, M.; Alser, M.; Ojuka, D.K.; Badereddin, Y.; Kamath, A.; Parepalli, S.A.; Brown, G.; Iharchane, S.; et al. Infection and mortality of healthcare workers worldwide from COVID-19: A systematic review. BMJ Glob. Health. 2020, 5, e003097. [Google Scholar] [CrossRef]
- Health and Care Worker Deaths during COVID-19, World Health Organization. Available online: https://www.who.int/news/item/20-10-2021-health-and-care-worker-deaths-during-covid-19 (accessed on 5 October 2022).
- Cheng, V.C.; Wong, S.-C.; Yuen, K.-Y. Estimating Coronavirus Disease 2019 Infection Risk in Health Care Workers. JAMA Netw. Open 2020, 3, e209687. [Google Scholar] [CrossRef]
- Cheng, V.C.-C.; Wong, S.-C.; Chuang, V.W.-M.; So, S.Y.-C.; Chen, J.H.-K.; Sridhar, S.; To, K.K.-W.; Chan, J.F.-W.; Hung, I.F.-N.; Ho, P.-L.; et al. Absence of nosocomial transmission of coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in the prepandemic phase in Hong Kong. Am. J. Infect. Control 2020, 48, 890–896. [Google Scholar] [CrossRef]
- Cheng, V.C.; Fung, K.S.; Siu, G.K.; Wong, S.-C.; Cheng, L.S.; Wong, M.-S.; Lee, L.-K.; Chan, W.-M.; Chau, K.-Y.; Leung, J.S.; et al. Nosocomial Outbreak of Coronavirus Disease 2019 by Possible Airborne Transmission Leading to a Superspreading Event. Clin. Infect. Dis. 2021, 73, e1356–e1364. [Google Scholar] [CrossRef]
- Over 12,500 Staff at Hong Kong’s Overloaded Public Hospitals Contracted COVID During 5th Wave, Hong Kong Free Press. Available online: https://hongkongfp.com/2022/03/11/over-12500-staff-at-hong-kongs-overloaded-pubic-hospitals-contracted-covid-during-5th-wave-ae-chief-in-tears/ (accessed on 5 October 2022).
- Wong, S.-C.; Chan, V.W.; Yuen, L.L.; Auyeung, C.H.; Leung, J.O.; Li, C.-K.; Kwok, M.O.; So, S.Y.; Chen, J.H.; Chiu, K.H.; et al. Infection of healthcare workers despite a high vaccination rate during the fifth wave of COVID-19 due to Omicron variant in Hong Kong. 2022; submitted, under review . [Google Scholar]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Bai, D.-S.; Geng, P.; Wang, Z.-D.; Wang, X.-L.; Xu, G.-R.; Ye, Q.; Guo, N.; Zhao, Y.; Yang, C.; Song, H.; et al. Practice and experience of regional medical center entrance linkage and closed-loop management under the wartime situation of the COVID-19 in China. Ann. Transl. Med. 2022, 10, 112. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- COVID-19 Government Response Tracker. Available online: https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker (accessed on 7 October 2022).
- Variation in Government Responses to COVID-19. Blavatnik School Working Paper. BSG-WP-2020/032, version 14.1. Updated 12 August 2022. Available online: https://www.bsg.ox.ac.uk/research/publications/variation-government-responses-covid-19 (accessed on 7 October 2022).
- Gibney, E. Whose coronavirus strategy worked best? Scientists hunt most effective policies. Nature 2020, 581, 15–16. [Google Scholar] [CrossRef]
- Cheng, V.C.; Wong, S.-C.; Chuang, V.W.; So, S.Y.; Chen, J.H.; Sridhar, S.; To, K.K.; Chan, J.F.; Hung, I.F.; Ho, P.-L.; et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020, 81, 107–114. [Google Scholar] [CrossRef]
- Cap. 599I Prevention and Control of Disease (Wearing of Mask) Regulation. Available online: https://www.elegislation.gov.hk/hk/cap599I (accessed on 7 October 2022).
- Lam, H.Y.; Lam, T.S.; Wong, C.H.; Lam, W.H.; Leung, C.M.E.; Au, K.W.A.; Lam, C.K.Y.; Lau, T.W.W.; Chan, Y.W.D.; Wong, K.H.; et al. The epidemiology of COVID-19 cases and the successful containment strategy in Hong Kong-January to May 2020. Int. J. Infect. Dis. 2020, 98, 51–58. [Google Scholar] [CrossRef]
- Li, K.K.F.; Jarvis, S.A.; Minhas, F. Elementary effects analysis of factors controlling COVID-19 infections in computational simulation reveals the importance of social distancing and mask usage. Comput. Biol. Med. 2021, 134, 104369. [Google Scholar] [CrossRef]
- Government to Impose Mandatory Quarantine on People Entering Hong Kong from Mainland, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202002/05/P2020020500793.htm (accessed on 7 October 2022).
- DH to Strengthen Health Quarantine Arrangements on Inbound Travellers from Italy’s Three Regions and Iran, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202002/28/P2020022800820.htm (accessed on 7 October 2022).
- DH to Further Strengthen Health Quarantine Arrangements on Inbound Travellers from Overseas, Press Releases. The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202003/10/P2020031000663.htm (accessed on 7 October 2022).
- DH to Further Extend and Adjust Health Quarantine Arrangements on Inbound Travellers from overseas, Press releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202003/13/P2020031300832.htm (accessed on 7 October 2022).
- Specifications Under the Prevention and Control of Disease (Regulation of Cross-boundary Conveyances and Travellers) Regulation Gazette, Press releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202007/18/P2020071800038.htm?fontSize=3 (accessed on 7 October 2022).
- COVID-19: All Travellers to Hong Kong Must Quarantine in Hotels, but Some China Arrivals Exempt, Hong Kong Free Press. Available online: https://hongkongfp.com/2020/11/12/covid-19-all-travellers-to-hong-kong-must-quarantine-in-hotels-but-some-china-arrivals-exempt/ (accessed on 7 October 2022).
- Hong Kong, China, Extends Quarantine Period for Most Inbound Travelers Effective Dec. 25. Available online: https://crisis24.garda.com/alerts/2020/12/china-officials-extend-quarantine-period-for-most-inbound-travelers-effective-dec-25-entry-banned-for-travelers-from-south-africa-update-45 (accessed on 7 October 2022).
- Hong Kong to Cut Quarantine for Arrivals to 14 Days from Next Month. Available online: https://www.reuters.com/world/china/hong-kong-shorten-21-day-quarantine-requirement-arrivals-2022-01-27/ (accessed on 7 October 2022).
- Government Adjusts Boarding, Quarantine and Testing Arrangements for Inbound Travellers on Risk-Based Principle, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202203/27/P2022032700005.htm?fontSize=1 (accessed on 7 October 2022).
- Government Announces Adjustments to Quarantine Arrangements for Inbound Persons, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202208/08/P2022080800803.htm (accessed on 7 October 2022).
- Government Announces Lifting of Compulsory Quarantine Requirement on Arrival at Hong Kong, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202209/24/P2022092400048.htm?fontSize=1 (accessed on 7 October 2022).
- Wong, S.-C.; Chen, H.; Lung, D.C.; Ho, P.-L.; Yuen, K.-Y.; Cheng, V.C. To prevent SARS-CoV-2 transmission in designated quarantine hotel for travelers: Is the ventilation system a concern? Indoor Air 2021, 31, 1295–1297. [Google Scholar] [CrossRef]
- Wong, S.-C.; Au, A.K.; Chen, H.; Yuen, L.L.; Li, X.; Lung, D.C.; Chu, A.W.; Ip, J.D.; Chan, W.-M.; Tsoi, H.-W.; et al. Transmission of Omicron (B.1.1.529)-SARS-CoV-2 Variant of Concern in a designated quarantine hotel for travelers: A challenge of elimination strategy of COVID-19. Lancet Reg. Health West Pac. 2022, 18, 100360. [Google Scholar] [CrossRef]
- Cheng, V.C.; Siu, G.K.; Wong, S.-C.; Au, A.K.; Ng, C.S.; Chen, H.; Li, X.; Lee, L.-K.; Leung, J.S.; Lu, K.K.; et al. Complementation of contact tracing by mass testing for successful containment of beta COVID-19 variant (SARS-CoV-2 VOC B.1.351) epidemic in Hong Kong. Lancet Reg. Health West Pac. 2021, 17, 100281. [Google Scholar] [CrossRef] [PubMed]
- Cap. 599J Prevention and Control of Disease (Compulsory Testing for Certain Persons) Regulation. Available online: https://www.elegislation.gov.hk/hk/cap599J (accessed on 7 October 2022).
- Restriction-testing declaration, Centre for Health Protection, Department of Health, The Government of the Hong Kong Special Administrative Region. Available online: https://www.coronavirus.gov.hk/eng/compulsory-testing.html#Restriction-testing-declaration (accessed on 7 October 2022).
- Wong, S.-C.; Yuen, L.L.-H.; Chen, J.H.-K.; Yuen, K.-Y.; Cheng, V.C.-C. Infection control challenges in handling recurrent blockage of sewage pipes in isolation facility designated for patients with COVID-19. J. Hosp. Infect. 2021, 114, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.-C.; Chan, V.W.; Lam, G.K.-M.; Yuen, L.L.; AuYeung, C.H.; Li, X.; Chen, J.H.; Chau, P.-H.; Yuen, K.-Y.; Cheng, V.C. The impact of personal coaching on influenza vaccination among healthcare workers before and during COVID-19 pandemic. Vaccine 2022, 40, 4905–4910. [Google Scholar] [CrossRef] [PubMed]
- Early Vaccination for All. COVID-19 Vaccination Programme, The Government of the Hong Kong Special Administrative Region. Available online: https://www.covidvaccine.gov.hk/en/dashboard (accessed on 8 October 2022).
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/covid-vaccinations?country=OWID_WRL (accessed on 8 October 2022).
- Archive of Statistics on 5th Wave of COVID-19. Centre for Health Protection, Department of Health, The Government of the Hong Kong Special Administrative Region. Available online: https://www.coronavirus.gov.hk/eng/5th-wave-statistics.html (accessed on 8 October 2022).
- Luk, T.T.; Zhao, S.; Wu, Y.; Wong, J.Y.; Wang, M.P.; Lam, T.H. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine 2021, 39, 3602–3607. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.Y.; Lam, J.C.; Lam, S.C.; Li, Y.; Chen, S.; Lam, M.Y.; Yeung, W.F. COVID-19 vaccine hesitancy and resistance in an urban Chinese population of Hong Kong: A cross-sectional study. Hum. Vaccin. Immunother. 2022, 18, 2072144. [Google Scholar] [CrossRef]
- Yasmin, F.; Najeeb, H.; Moeed, A.; Naeem, U.; Asghar, M.S.; Chughtai, N.U.; Yousaf, Z.; Seboka, B.T.; Ullah, I.; Lin, C.Y.; et al. COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Front. Public Health 2021, 9, 770985. [Google Scholar] [CrossRef]
- Cénat, J.M.; Noorishad, P.G.; Moshirian Farahi, S.M.M.; Darius, W.P.; Mesbahi El Aouame, A.; Onesi, O.; Broussard, C.; Furyk, S.E.; Yaya, S.; Caulley, L.; et al. Prevalence and factors related to COVID-19 vaccine hesitancy and unwillingness in Canada: A systematic review and meta-analysis. J. Med. Virol. 2022. [Google Scholar] [CrossRef]
- Ackah, B.B.B.; Woo, M.; Stallwood, L.; Fazal, Z.A.; Okpani, A.; Ukah, U.V.; Adu, P.A. COVID-19 vaccine hesitancy in Africa: A scoping review. Glob. Health Res. Policy 2022, 7, 21. [Google Scholar] [CrossRef]
- Aw, J.; Seah, S.S.Y.; Seng, B.J.J.; Low, L.L. COVID-19-Related Vaccine Hesitancy among Community Hospitals’ Healthcare Workers in Singapore. Vaccines 2022, 10, 537. [Google Scholar] [CrossRef]
- Caiazzo, V.; Witkoski Stimpfel, A. Vaccine hesitancy in American healthcare workers during the COVID-19 vaccine roll out: An integrative review. Public Health 2022, 207, 94–104. [Google Scholar] [CrossRef]
- Venkatesan, K.; Menon, S.; Haroon, N.N. COVID-19 vaccine hesitancy among medical students: A systematic review. J. Educ. Health Promot. 2022, 11, 218. [Google Scholar] [PubMed]
- Pires, C. Global Predictors of COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 1349. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Lee, W.; Lin, F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. Int. J. Environ. Res. Public Health 2022, 19, 8033. [Google Scholar] [CrossRef] [PubMed]
- Chau, C.Y.C. COVID-19 vaccination hesitancy and challenges to mass vaccination. Hong Kong Med. J. 2021, 27, 377–379. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Tang, A.; Tsoi, M.T.F.; Chan, E.Y.Y.; Tang, J.W.T.; Wong, A.; Wei, W.I.; Wong, S.Y.S. Psychobehavioral Responses and Likelihood of Receiving COVID-19 Vaccines during the Pandemic, Hong Kong. Emerg. Infect. Dis. 2021, 27, 1802–1810. [Google Scholar] [CrossRef]
- Silver, A. ‘COVID zero’ regions struggle with vaccine complacency. Nature 2022. [Google Scholar] [CrossRef]
- LeaveHomeSafe Moblie App. Available online: https://www.leavehomesafe.gov.hk/en/ (accessed on 10 November 2022).
- Government announces implementation arrangements for Vaccine Pass. Press releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202202/21/P2022022100781.htm (accessed on 8 October 2022).
- Government adjusts vaccination requirements of Vaccine Pass, Press releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202203/20/P2022032000438.htm (accessed on 8 October 2022).
- McMenamin, M.E.; Nealon, J.; Lin, Y.; Wong, J.Y.; Cheung, J.K.; Lau, E.H.Y.; Wu, P.; Leung, G.M.; Cowling, B.J. Vaccine effectiveness of one, two, and three doses of BNT162b2 and CoronaVac against COVID-19 in Hong Kong: A population-based observational study. Lancet Infect. Dis. 2022, 22, 1435–1443. [Google Scholar] [CrossRef]
- Kang, W.; Shami, J.J.P.; Yan, V.K.C.; Ye, X.; Blais, J.E.; Li, X.; Lee, V.H.F.; Chui, C.S.L.; Lai, F.T.T.; Wan, E.Y.F.; et al. Safety of two-dose COVID-19 vaccination (BNT162b2 and CoronaVac) in adults with cancer: A territory-wide cohort study. J. Hematol. Oncol. 2022, 15, 66. [Google Scholar] [CrossRef]
- Ye, X.; Ma, T.; Blais, J.E.; Yan, V.K.C.; Kang, W.; Chui, C.S.L.; Lai, F.T.T.; Li, X.; Wan, E.Y.F.; Wong, C.K.H.; et al. Association between BNT162b2 or CoronaVac COVID-19 vaccines and major adverse cardiovascular events among individuals with cardiovascular disease. Cardiovasc. Res. 2022, 118, 2329–2338. [Google Scholar] [CrossRef]
- Cheng, F.W.T.; Fan, M.; Wong, C.K.H.; Chui, C.S.L.; Lai, F.T.T.; Li, X.; Wan, E.Y.F.; Tang, S.C.W.; Chan, E.W.Y.; Wong, I.C.K. The effectiveness and safety of mRNA (BNT162b2) and inactivated (CoronaVac) COVID-19 vaccines among individuals with chronic kidney diseases. Kidney Int. 2022, 102, 922–925. [Google Scholar] [CrossRef] [PubMed]
- Wan, E.Y.F.; Wang, Y.; Chui, C.S.L.; Mok, A.H.Y.; Xu, W.; Yan, V.K.C.; Lai, F.T.T.; Li, X.; Wong, C.K.H.; Chan, E.W.Y.; et al. Safety of an inactivated, whole-virion COVID-19 vaccine (CoronaVac) in people aged 60 years or older in Hong Kong: A modified self-controlled case series. Lancet Healthy Longev. 2022, 3, e491–e500. [Google Scholar] [CrossRef]
- Air Change/Installation of Air Purifier in Catering Premises. Food and Environmental Hygiene Department, The Government of Hong Kong Special Administrative Region. Available online: https://www.fehd.gov.hk/english/licensing/guide_general_reference/report_air-changes_purification.html (accessed on 10 November 2022).
- Final Report on Compliance with the Requirement on Air Change or Air Purifiers in Seating Areas of Dine-in Catering Premises under Cap. 599F, Food and Environmental Hygiene Department, The Government of Hong Kong Special Administrative Region. Available online: https://www.fehd.gov.hk/english/licensing/guide_general_reference/air-changes_report2021.pdf (accessed on 10 November 2022).
- Ioannidis, J.P.A. The end of the COVID-19 pandemic. Eur. J. Clin. Investig. 2022, 52, e13782. [Google Scholar] [CrossRef] [PubMed]
- Del Rio, C.; Malani, P.N. COVID-19 in 2022-The Beginning of the End or the End of the Beginning? JAMA 2022, 327, 2389–2390. [Google Scholar] [CrossRef]
- Nyberg, T.; Ferguson, N.M.; Nash, S.G.; Webster, H.H.; Flaxman, S.; Andrews, N.; Hinsley, W.; Bernal, J.L.; Kall, M.; Bhatt, S.; et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: A cohort study. Lancet 2022, 399, 1303–1312. [Google Scholar] [CrossRef]
- Ward, I.L.; Bermingham, C.; Ayoubkhani, D.; Gethings, O.J.; Pouwels, K.B.; Yates, T.; Khunti, K.; Hippisley-Cox, J.; Banerjee, A.; Walker, A.S.; et al. Risk of covid-19 related deaths for SARS-CoV-2 omicron (B.1.1.529) compared with delta (B.1.617.2): Retrospective cohort study. BMJ 2022, 378, e070695. [Google Scholar] [CrossRef]
- Liu, Y.; Yu, Y.; Zhao, Y.; He, D. Reduction in the infection fatality rate of Omicron variant compared with previous variants in South Africa. Int. J. Infect. Dis. 2022, 120, 146–149. [Google Scholar] [CrossRef]
- COVID-19 Forecasting Team. Variation in the COVID-19 infection-fatality ratio by age, time, and geography during the pre-vaccine era: A systematic analysis. Lancet 2022, 399, 1469–1488. [CrossRef]
- Smith, D.J.; Hakim, A.J.; Leung, G.M.; Xu, W.; Schluter, W.W.; Novak, R.T.; Marston, B.; Hersh, B.S. COVID-19 Mortality and Vaccine Coverage-Hong Kong Special Administrative Region, China, January 6, 2022-March 21, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 545–548. [Google Scholar] [CrossRef]
- Chen, L.L.; Abdullah, S.M.U.; Chan, W.-M.; Chan, B.P.; Ip, J.D.; Chu, A.W.; Lu, L.; Zhang, X.; Zhao, Y.; Chuang, V.W.; et al. Contribution of low population immunity to the severe Omicron BA.2 outbreak in Hong Kong. Nat. Commun. 2022, 13, 3618. [Google Scholar] [CrossRef]
- Poon, R.W.; Chan, B.P.; Chan, W.-M.; Fong, C.H.; Zhang, X.; Lu, L.; Chen, L.L.; Lam, J.Y.; Cheng, V.C.; Wong, S.S.-Y.; et al. SARS-CoV-2 IgG seropositivity after the severe Omicron wave of COVID-19 in Hong Kong. Emerg. Microbes Infect. 2022, 11, 2116–2119. [Google Scholar] [CrossRef] [PubMed]
- Hung, I.F.; Lung, K.-C.; Tso, E.Y.; Liu, R.; Chung, T.W.; Chu, M.-Y.; Ng, Y.-Y.; Lo, J.; Chan, J.; Tam, A.R.; et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: An open-label, randomised, phase 2 trial. Lancet 2020, 395, 1695–1704. [Google Scholar] [CrossRef]
- Tam, A.R.; Zhang, R.R.; Lung, K.C.; Liu, R.; Leung, K.Y.; Liu, D.; Fan, Y.; Lu, L.; Lam, A.H.Y.; Chung, T.W.H.; et al. Early treatment of high-risk hospitalized COVID-19 patients with a combination of interferon beta-1b and remdesivir: A phase 2 open-label randomized controlled trial. Clin. Infect. Dis. 2022, ciac523. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.H.; Lau, K.T.K.; Au, I.C.H.; Xiong, X.; Lau, E.H.Y.; Cowling, B.J. Clinical Improvement, Outcomes, Antiviral Activity, and Costs Associated with Early Treatment with Remdesivir for Patients with Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2022, 74, 1450–1458. [Google Scholar] [CrossRef]
- Wong, C.K.H.; Lau, K.T.K.; Au, I.C.H.; Xiong, X.; Chung, M.S.H.; Lau, E.H.Y.; Cowling, B.J. Optimal Timing of Remdesivir Initiation in Hospitalized Patients with Coronavirus Disease 2019 (COVID-19) Administered with Dexamethasone. Clin. Infect. Dis. 2022, 75, e499–e508. [Google Scholar] [CrossRef]
- Wong, C.K.H.; Lau, K.T.K.; Au, I.C.H.; Xiong, X.; Chung, M.S.H.; Leung, B.Y.C.; Lau, E.H.Y.; Cowling, B.J. Initiation of Tocilizumab or Baricitinib Were Associated with Comparable Clinical Outcomes Among Patients Hospitalized With COVID-19 and Treated with Dexamethasone. Front. Pharmacol. 2022, 13, 866441. [Google Scholar] [CrossRef]
- Wong, C.K.H.; Au, I.C.H.; Lau, K.T.K.; Lau, E.H.Y.; Cowling, B.J.; Leung, G.M. Real-world effectiveness of early molnupiravir or nirmatrelvir-ritonavir in hospitalised patients with COVID-19 without supplemental oxygen requirement on admission during Hong Kong’s omicron BA.2 wave: A retrospective cohort study. Lancet Infect. Dis. 2022. [Google Scholar] [CrossRef]
- Bhimraj, A.; Morgan, R.L.; Shumaker, A.H.; Lavergne, V.; Baden, L.; Cheng, V.C.; Edwards, K.M.; Gandhi, R.; Muller, W.J.; O’Horo, J.C.; et al. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Clin. Infect. Dis. 2020, ciaa478. [Google Scholar] [CrossRef]
- Bhimraj, A.; Morgan, R.L.; Shumaker, A.H.; Baden, L.; Cheng, V.C.C.; Edwards, K.M.; Gallagher, J.C.; Gandhi, R.T.; Muller, W.J.; Nakamura, M.M.; et al. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Clin. Infect. Dis. 2022, ciac724. [Google Scholar] [CrossRef]
- Response to Media Enquiries about Quarantine Arrangements, Press Releases, The Government of the Hong Kong Special Administrative Region. Available online: https://www.info.gov.hk/gia/general/202209/01/P2022090100815.htm?fontSize=3 (accessed on 15 October 2022).
- Kim, H.; Webster, R.G.; Webby, R.J. Influenza Virus: Dealing with a Drifting and Shifting Pathogen. Viral Immunol. 2018, 31, 174–183. [Google Scholar] [CrossRef]
- SARS-CoV-2 Variants of Concern Update. Available online: https://www.health.govt.nz/system/files/documents/pages/sars-cov-2-variant-of-concern-update-27sep22.pdf (accessed on 11 October 2022).
- Tan, C.W.; Lim, B.L.; Young, B.E.; Yeoh, A.Y.; Yung, C.F.; Yap, W.C.; Althaus, T.; Chia, W.N.; Zhu, F.; Lye, D.C.; et al. Comparative neutralisation profile of SARS-CoV-2 omicron subvariants BA.2.75 and BA.5. Lancet Microbe 2022. [Google Scholar] [CrossRef]



| Countries | Cumulative Number of Confirmed Cases | Cumulative Number of Deaths among All Confirmed Cases | Incidence per 1000 Population a | Death per 1000 Population a | Case Fatality Rate (%) |
|---|---|---|---|---|---|
| United States of America | 95,795,378 | 1,050,631 | 289.4 | 3.2 | 1.1 |
| India | 44,560,749 | 528,487 | 32.3 | 0.4 | 1.2 |
| France | 35,056,032 | 154,854 | 518.2 | 2.3 | 0.4 |
| Brazil | 34,624,427 | 685,750 | 162.9 | 3.2 | 2.0 |
| Germany | 32,905,086 | 149,368 | 395.7 | 1.8 | 0.5 |
| Korea | 24,620,128 | 28,213 | 480.2 | 0.6 | 0.1 |
| United Kingdom | 23,621,956 | 189,919 | 347.1 | 2.8 | 0.8 |
| Italy | 22,241,369 | 176,775 | 375.5 | 3.0 | 0.8 |
| Japan | 20,992,896 | 44,262 | 166.0 | 0.4 | 0.2 |
| Russia | 20,694,894 | 386,551 | 141.8 | 2.7 | 1.9 |
| Turkey | 16,852,382 | 101,068 | 201.6 | 1.2 | 0.6 |
| Spain | 13,393,196 | 113,845 | 282.6 | 2.4 | 0.9 |
| Vietnam | 11,467,619 | 43,146 | 117.8 | 0.5 | 0.4 |
| Australia | 10,191,312 | 14,853 | 399.7 | 0.6 | 0.2 |
| Nomenclature by the World Health Organization | Earliest Documented Samples (Place and Date) | Duration | Pango Lineage | GISAID Clade | Nextstrain Clade |
|---|---|---|---|---|---|
| Alpha | United Kingdom, September 2020 | 18 December 2020 to 9 March 2022 | B.1.1.7 | GRY | 20I (V1) |
| Beta | South Africa, May 2020 | 18 December 2020 to 9 March 2022 | B.1.351 | GH/501Y.V2 | 20H (V2) |
| Gamma | Brazil, November 2020 | 11 January 2021 to 9 March 2022 | P.1 | GR/501Y.V3 | 20J (V3) |
| Delta | India, October 2020 | 11 May 2021 to 7 June 2022 | B.1.617.2 | G/478K.V1 | 21A, 21I, 21J |
| Omicron | Multiple countries, November 2021 | 26 November 2021 onwards | B.1.1.529 | GR/484A | 21K, 21L, 21M, 22A, 22B, 22C, 22D |
| Wave of COVID-19 | Period (Duration of Each Wave, Day) a | Total Number of Cases b (Death, Case Fatality rate) | Number (%) of Cases in (Episodes of) Community Outbreaks c | Number (%) of Imported Cases (Remark) | Predominant Virus Strain |
|---|---|---|---|---|---|
| 1st | 23 January 2020 (day 24) to 14 March 2020 (day 75) (51 days) | 142 (4, 2.8%) | 53 (37.3%) (4) | 56 (39.4%) (mainly from China) | NA |
| 2nd | 15 March 2020 (day 76) to 30 June 2020 (day 183) (108 days) | 1064 (4, 0.38%) | 130 (12.2%) (3) | 739 (69.4%) | NA |
| 3rd | 1 July 2020 (day 184) to 31 October 2020 (day 306) (123 days) | 4118 (103, 2.5%) | 681 (16.5%) (23) | 678 (16.5%) | B.1.1.63 |
| 4th | 1 November 2020 (day 307) to 30 April 2021 (day 487) (181 days) | 6451 (101, 1.6%) | 1480 (22.9%) (24) | 960 (14.9%) | B.1.36.27 |
| Window phase d | 1 May 2021 (day 488) to 30 December 2021 (day 731) (244 days) | 861 e (1, 0.12%) | No | 854 (99.2%) (without community outbreak | NA |
| 5th (primary Omicron) | 31 December 2021 (day 732) to 31 May 2022 (day 883) (152 days) | 1,200,068 (9318, 0.78%) f | NA g | 2292 (0.19%) | Omicron BA.2 |
| 5th (secondary Omicron) | 1 June 2022 (day 884) to 25 September 2022 (day 1000) (117 days) | 532,801 (585, 0.11%) f | NA g | 20,519 (3.9%) | Omicron BA.5 |
| A | Clinical Criteria (Time of Implementation) a | Remark |
|---|---|---|
| 1. | Presented with fever and acute respiratory illness or pneumonia (from day 1 to day 23) | Prepare for the importation of index patient to Hong Kong |
| 2. | Presented with fever or acute respiratory illness or pneumonia (with effect from day 24) | In response to the importation of index patient to Hong Kong |
| B | Epidemiological criteria (time of implementation) a | |
| 1. | Travel history to Wuhan, Hubei province, People’s Republic of China, within 14 days before onset of symptoms, irrespective of any exposure to wet market or seafood market (from day 1 to day 16) | Prepare for the importation of index patient to Hong Kong |
| 2. | Patient met with one of the following within 14 days prior to the onset of symptoms: (a) had visited Wuhan (regardless of whether the individual had visited wet markets or seafood markets there), (b) had visited a medical hospital in Mainland China, or (c) had had close contact with a confirmed case of the novel coronavirus while that patient was symptomatic (from day 17 to day 20) | In response to the evolving epidemic with increasing number of confirmed cases in Wuhan |
| 3. | Patient met with one of the following within 14 days prior to the onset of symptoms: (a) had visited Hubei Province (regardless of whether the individual had visited wet markets or seafood markets there) or 2(b) or 2(c) listed above (with effect from day 21) | In response to spread of SARS-CoV-2 beyond Wuhan |
| 4. | Universal admission screening for asymptomatic patients (with effect from 9 September 2020 (day 265) onwards) | In response to widespread transmission of SARS-CoV-2 locally |
| Stage | Time Period | Requirement |
|---|---|---|
| First | 24 February 2022 (day 422) to 29 April 2022 (day 851) | Persons ≥ 12 years are required to receive at least one dose of COVID-19 vaccine in order to use the Vaccine Pass to enter specified premises. |
| Second | 30 April 2022 (day 852) to 30 May 2022 (day 882) | For persons ≥ 18 years: Two doses of COVID-19 vaccine. For persons aged 12 to 17 years: 1st dose, if within 6 months of 1st dose, or 2nd dose, if after 6 months from 1st dose. |
| Third | 31 May 2022 (day 883) onwards b | For persons ≥ 18 years: 2nd dose, if within 6 months of 2nd dose, or 3rd dose, if after 6 months from 2nd dose. For persons aged 12 to 17 years: 2nd dose, if within 6 months of 2nd dose, or 3rd dose, if after 6 months from 2nd dose. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, S.-C.; Au, A.K.-W.; Lo, J.Y.-C.; Ho, P.-L.; Hung, I.F.-N.; To, K.K.-W.; Yuen, K.-Y.; Cheng, V.C.-C. Evolution and Control of COVID-19 Epidemic in Hong Kong. Viruses 2022, 14, 2519. https://doi.org/10.3390/v14112519
Wong S-C, Au AK-W, Lo JY-C, Ho P-L, Hung IF-N, To KK-W, Yuen K-Y, Cheng VC-C. Evolution and Control of COVID-19 Epidemic in Hong Kong. Viruses. 2022; 14(11):2519. https://doi.org/10.3390/v14112519
Chicago/Turabian StyleWong, Shuk-Ching, Albert Ka-Wing Au, Janice Yee-Chi Lo, Pak-Leung Ho, Ivan Fan-Ngai Hung, Kelvin Kai-Wang To, Kwok-Yung Yuen, and Vincent Chi-Chung Cheng. 2022. "Evolution and Control of COVID-19 Epidemic in Hong Kong" Viruses 14, no. 11: 2519. https://doi.org/10.3390/v14112519





