A Miniaturized Electrostatic Precipitator Respirator Effectively Removes Ambient SARS-CoV-2 Bioaerosols
Abstract
:1. Introduction
2. Materials and methods
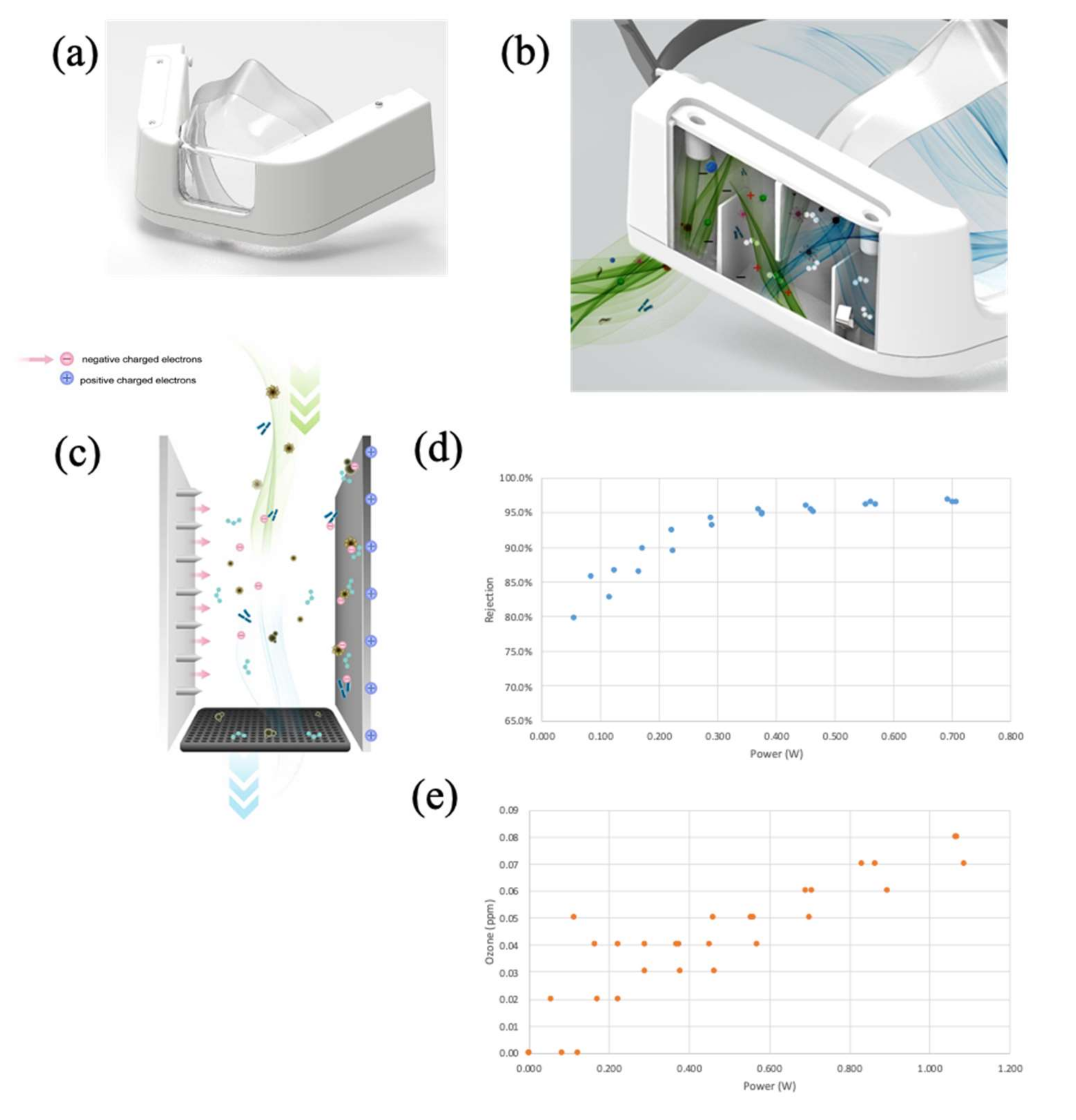
2.1. Design and Operational Principles of the mEP Respirator
2.2. Benchmark Testing of the mEP for Particle Removal
2.3. Experimental Airborne Viral Removal Efficiency
2.3.1. Experimental Configuration
2.3.2. Experimental Procedure
2.3.3. Measurement with Aerodynamic Particle Sizer
2.3.4. Virus and Cells
2.3.5. Quantification of Viral RNA in Aerosol Samples
2.3.6. Quantification of Culturable Virus
2.3.7. Statistics
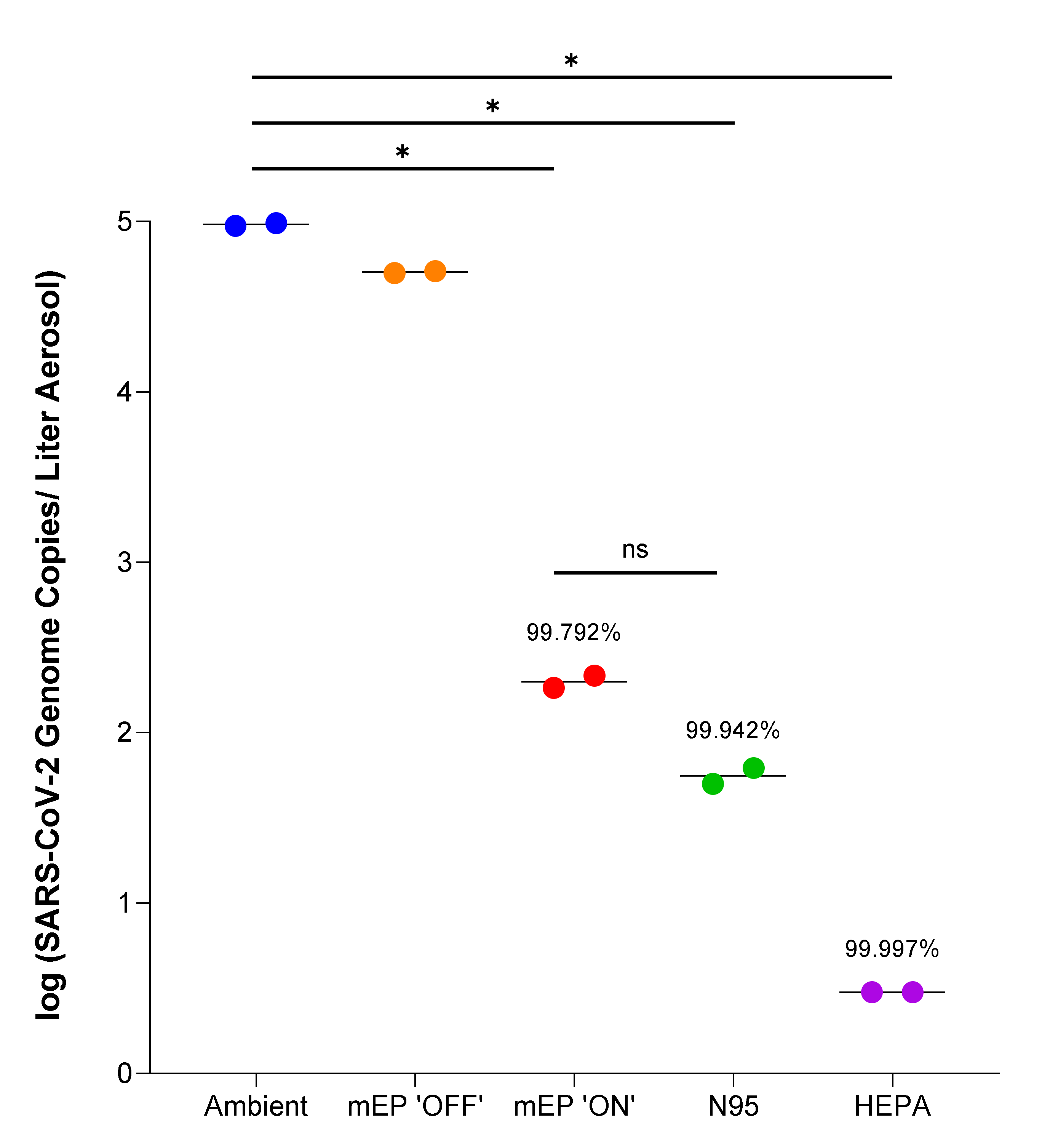
3. Results
4. Discussion
4.1. Significance
4.2. Limitations
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Khan, S.; Siddique, R.; Shereen, M.A.; Ali, A.; Liu, J.; Bai, Q.; Bashir, N.; Xue, M. The emergence of a novel coronavirus (SARS-CoV-2), their biology and therapeutic options. J. Clin. Microbiol. 2020, 58, e00187-20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banik, R.K.; Ulrich, A.K. Evidence of short-range aerosol transmission of SARS-CoV-2 and call for universal airborne precautions for anesthesiologists during the COVID-19 pandemic. Anesth. Analg. 2020, 131, e102–e104. [Google Scholar] [CrossRef] [PubMed]
- Deng, C.X. The global battle against SARS-CoV-2 and COVID-19. Int. J. Biol. Sci. 2020, 16, 1676–1677. [Google Scholar] [CrossRef] [PubMed]
- Fink, J.B.; Ehrmann, S.; Li, J.; Dailey, P.; McKiernan, P.; Darquenne, C.; Martin, A.R.; Rothen-Rutishauser, B.; Kuehl, P.J.; Häussermann, S.; et al. Reducing Aerosol-Related Risk of Transmission in the Era of COVID-19: An Interim Guidance Endorsed by the International Society of Aerosols in Medicine. J. Aerosol Med. Pulm. Drug Deliv. 2020, 33, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Bartoszko, J.J.; Farooqi, M.A.M.; Alhazzani, W.; Loeb, M. Medical Masks vs N95 Respirators for Preventing COVID-19 in Health Care Workers a Systematic Review and Meta-Analysis of Randomized Trials. Influ. Other Respir Viruses 2020, 14, 365–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zangmeister, C.D.; Radney, J.G.; Vicenzi, E.P.; Weaver, J.L. Filtration Efficiencies of Nanoscale Aerosol by Cloth Mask Materials Used to Slow the Spread of SARS-CoV-2. ACS Nano 2020, 14, 9188–9200. [Google Scholar] [CrossRef]
- Clase, C.M.; Fu, E.L.; Joseph, M.; Beale, R.C.; Dolovich, M.B.; Jardine, M.; Mann, J.F.; Pecoits-Filho, R.; Winkelmayer, W.C.; Carrero, J.J. Cloth Masks May Prevent Transmission of COVID-19: An Evidence-Based, Risk-Based Approach. Ann. Intern. Med. 2020, 173, 489–491. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: Are cloth masks still effective? And other questions answered. BMJ 2021, 372, n432. [Google Scholar] [CrossRef]
- Anderson, M.G. Cloth Masks May Prevent Transmission of COVID-19. Ann. Intern. Med. 2021, 174, 579–580. [Google Scholar] [CrossRef]
- Milton, D.K.; Fabian, M.P.; Cowling, B.; Grantham, M.L.; McDevitt, J.J. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013, 9, e1003205. [Google Scholar] [CrossRef] [Green Version]
- Qaseem, A.; Etxeandia-Ikobaltzeta, I.; Yost, J.; Humphrey, L.L. Update Alert: Use of N95, Surgical, or Cloth Masks to Prevent COVID-19 in Health Care and Community Settings: Living Practice Points From the American College of Physicians (Version 1). Ann. Intern. Med. 2020, 173, 170. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Golshahi, L.; Chen, D.-R. Advanced testing method to evaluate the performance of respirator filter media. J. Occup. Environ. Hyg. 2016, 13, 750–758. [Google Scholar] [CrossRef]
- Eshbaugh, J.P.; Gardner, P.D.; Richardson, A.W.; Hofacre, K.C. N95 and P100 respirator filter efficiency under high constant and cyclic flow. J. Occup. Environ. Hyg. 2008, 6, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.; Hu, J.; Gan, C.; Morris, J.; Meacham, K.; Ballard, D. Safety concerns for facial topography customized 3D-printed N95 filtering face-piece respirator produced for the COVID-19 pandemic: Initial step is respiratory fit testing. Int. J. Oral Maxillofac. Surg. 2020, 49, 1660–1661. [Google Scholar] [CrossRef] [PubMed]
- Or, P.; Chung, J.; Wong, T. A novel approach to fit testing the N95 respirator in real time in a clinical setting. Int. J. Nurs. Pract. 2014, 22, 22–30. [Google Scholar] [CrossRef]
- Houwink, E.H.; Rolvink, W. The quantitative assay of bacterial aerosols by electrostatic precipitation. Epidemiol. Infect. 1957, 55, 544–563. [Google Scholar] [CrossRef] [Green Version]
- Park, M.; Son, A.; Chua, B. Microorganism-ionizing respirator with reduced breathing resistance suitable for removing airborne bacteria. Sens. Actuators B Chem. 2018, 276, 437–446. [Google Scholar] [CrossRef]
- Ivanenko, A.A.; Ivanenko, N.B.; Kuzmenkov, M.A.; Jakovleva, E.M.; Skudra, A.; Slyadnev, M.N.; Ganeev, A.A. Direct and rapid analysis of ambient air and exhaled air via electrostatic precipitation of aerosols in an atomizer furnace and Zeeman spectrometry. Anal. Bioanal. Chem. 2005, 381, 713–720. [Google Scholar] [CrossRef]
- Martin, S.B., Jr.; Moyer, E.S. Electrostatic respirator filter media: Filter efficiency and most penetrating particle size effects. Appl. Occup. Environ. Hyg. 2000, 15, 609–617. [Google Scholar] [CrossRef]
- Makowski, K. Deposition and Resuspension of Selected Aerosols Particles on Electrically Charged Filter Materials for Respiratory Protective Devices. Int. J. Occup. Saf. Ergon. 2005, 11, 363–376. [Google Scholar] [CrossRef] [Green Version]
- Fears, A.C.; Klimstra, W.B.; Duprex, P.; Hartman, A.; Weaver, S.C.; Plante, K.S.; Mirchandani, D.; Plante, J.A.; Aguilar, P.V.; Fernández, D.; et al. Persistence of Severe Acute Respiratory Syndrome Coronavirus 2 in Aerosol Suspensions. Emerg. Infect. Dis. 2020, 26, 2168–2171. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Occupational Safety and Health (NIOSH). Respiratory Protective Devices; Final Rules and Notice. Fed. Regist. 1995, 60, 30336. [Google Scholar]
- Chen, B.T.; Cheng, Y.S.; Yeh, H.C. Performance of a TSI Aerodynmaic Particle Sizer. Aerosol Sci. Technol. 1985, 4, 89–97. [Google Scholar] [CrossRef]
- Beddingfield, B.J.; Maness, N.J.; Fears, A.C.; Rappaport, J.; Aye, P.P.; Russell-Lodrigue, K.; Doyle-Meyers, L.A.; Blair, R.V.; Carias, A.M.; Madden, P.J.; et al. Effective Prophylaxis of COVID-19 in Rhesus Macaques Using a Combination of Two Parenterally-Administered SARS-CoV-2 Neutralizing Antibodies. Front Cell. Infect. Microbiol. 2021, 11, 753444. [Google Scholar] [CrossRef] [PubMed]
- Kulmala, I.; Heinonen, K.; Salo, S. Improving filtration efficacy of medical face masks. Aerosol Air Qual. Res. 2021, 21, 210043. [Google Scholar] [CrossRef]
- Ghatak, S.; Khona, D.K.; Sen, A.; Huang, K.; Jagdale, G.; Singh, K.; Gopalakrishnan, V.; Cornetta, K.G.; Roy, S.; Khanna, S.; et al. Electroceutical fabric lowers zeta potential and eradicates coronavirus infectivity upon contact. Sci. Rep. 2021, 11, 21723. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Redmann, R.K.; Beddingfield, B.J.; Spencer, S.; Chirichella, N.R.; Henley, J.L.; Hager, W.; Roy, C.J. A Miniaturized Electrostatic Precipitator Respirator Effectively Removes Ambient SARS-CoV-2 Bioaerosols. Viruses 2022, 14, 765. https://doi.org/10.3390/v14040765
Redmann RK, Beddingfield BJ, Spencer S, Chirichella NR, Henley JL, Hager W, Roy CJ. A Miniaturized Electrostatic Precipitator Respirator Effectively Removes Ambient SARS-CoV-2 Bioaerosols. Viruses. 2022; 14(4):765. https://doi.org/10.3390/v14040765
Chicago/Turabian StyleRedmann, Rachel K., Brandon J. Beddingfield, Skye Spencer, Nicole R. Chirichella, Julian L. Henley, Wes Hager, and Chad J. Roy. 2022. "A Miniaturized Electrostatic Precipitator Respirator Effectively Removes Ambient SARS-CoV-2 Bioaerosols" Viruses 14, no. 4: 765. https://doi.org/10.3390/v14040765






