The Outcome of BNT162b2, ChAdOx1-Sand mRNA-1273 Vaccines and Two Boosters: A Prospective Longitudinal Real-World Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Study Participants, and Follow-up
2.2. Inclusion, Exclusion Criteria, and Control Group
- o
- Inflammatory cardiac illness within the past three months; myocarditis or pericarditis; acute rheumatic fever or acute rheumatic heart disease (i.e., with active myocardial inflammation); or acute decompensated heart failure.
- o
- Vaccination was temporarily deferred up to 4 months after a confirmed infection with COVID-19.
- o
- Until recovery from a severe medical condition (such as major surgery or hospital admission for a serious illness).
- o
- Until recovery from a multisystem inflammatory syndrome in adults.
- o
- The serious adverse event caused by a previous dose of a COVID-19 vaccine, with no acceptable alternative vaccine available.
- o
- Treatment with a monoclonal antibody for COVID-19.
- o
- Initially, data were limited about the vaccine’s safety in immunocompromised patients (HIV, patients on immunosuppressant drugs, and immunocompromising diseases). The treating physician and the patient discussed the available safety data before administering the vaccine to evaluate risks and benefits.
- o
- In the early phase of the study, data about the vaccine’s safety in pregnant women were limited. Thus, for pregnant women, particularly those with high-risk pregnancies, vaccination was postponed until delivery.
2.3. Assessment of Vaccine Effectiveness and Measurement of the Study Outcomes
2.4. COVID-19 Vaccines Registration, Documentation, and Management
2.5. Types, Preparation, Storage, and Administration of Vaccines
- -
- ChAdOx1 nCoV-19 COVID-19vaccine: The multi-dose vial is stored in cold chain conditions of 2 °C to 8 °C for six months. Once opened, the vial can be used after 6 h at room temperature or 48 h in the refrigerator (2 °C to 8 °C). Vial content does not need to be mixed with a diluent.
- -
- BNT162b2 COVID-19vaccine (Pfizer-Biontech, Inc., NY, USA) is provided as multi-dose vials. The vaccine is stored frozen and is thawed before dilution. Vials are thawed either in the refrigerator (2 °C and eight °C (35.6 °F and 46 °F)) or at room temperature (up to 25 °C). The BNT162b2 vaccine vial was removed from the refrigerator and kept at room temperature. It should be diluted within 2 h. The BNT162b2 vaccine is administered intramuscularly in the deltoid muscle after cutting the vial. The diluent is 1.8 mL of 0.9% sodium chloride (normal saline, preservative-free). After dilution, the vial contains five 0.3 mL doses of the vaccine that can be used. The interval between the two doses is 21–28 days
- -
- mRNA-1273COVID-19vaccine: The multi-dose vial is stored frozen and must be thawed before use either in the refrigerator (2 °C and 8 °C) or at room temperature (8 °C and 25 °C). The vial does not need to be mixed with a diluent. The Moderna vaccine is administered intramuscularly in the deltoid muscle. The interval between the two doses is 21–28 days.
2.6. Adverse Events (AEs) Recording and Reporting
2.7. Measurement of Anti–SARS-CoV-2 Antibody Levels
2.8. Statistical Analysis
3. Results
3.1. Demographics and Characteristics of Enrolled Subjects
3.2. The Outcome of Vaccination in the Three Groups
3.3. Vaccine Adverse Events
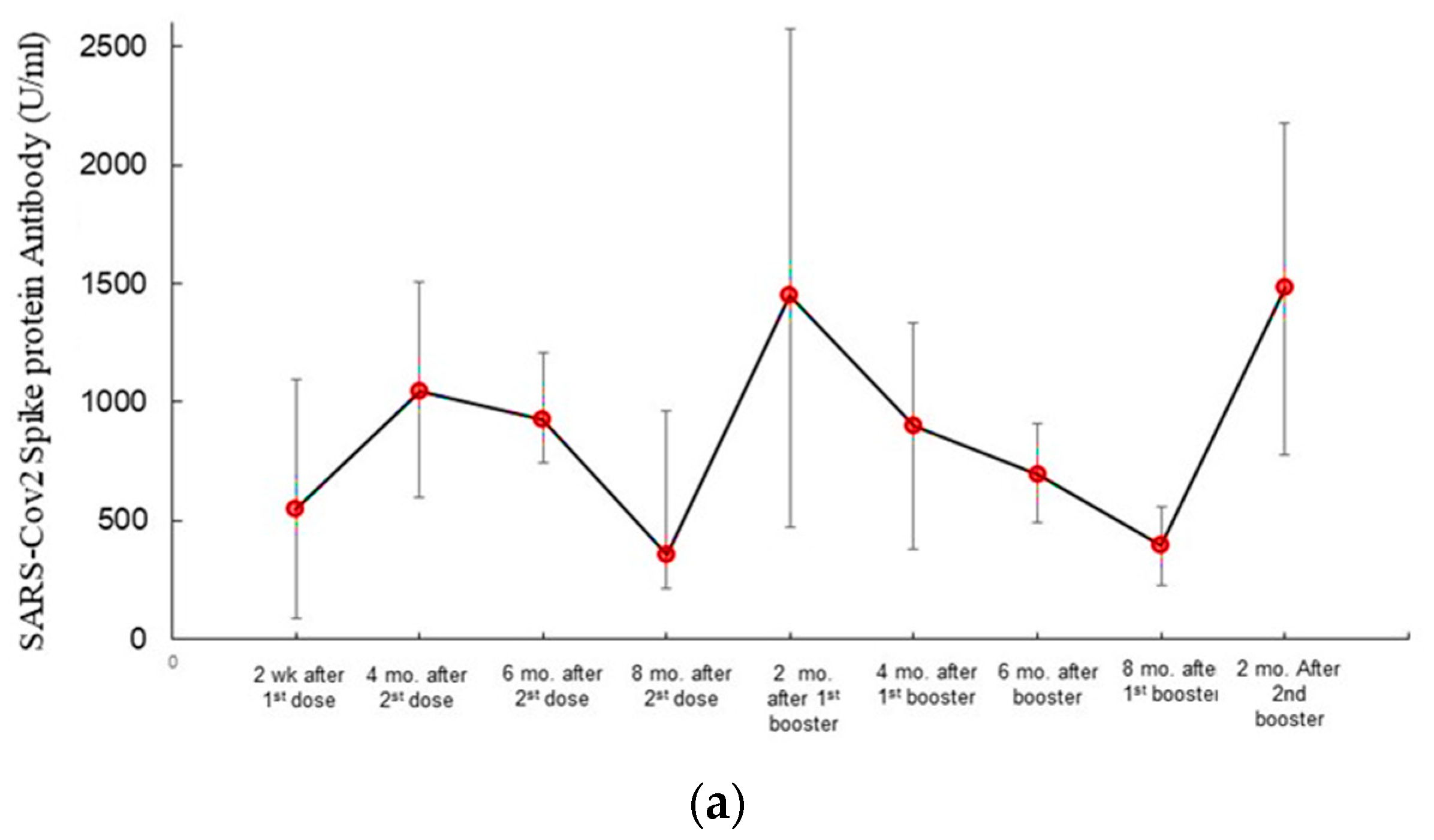
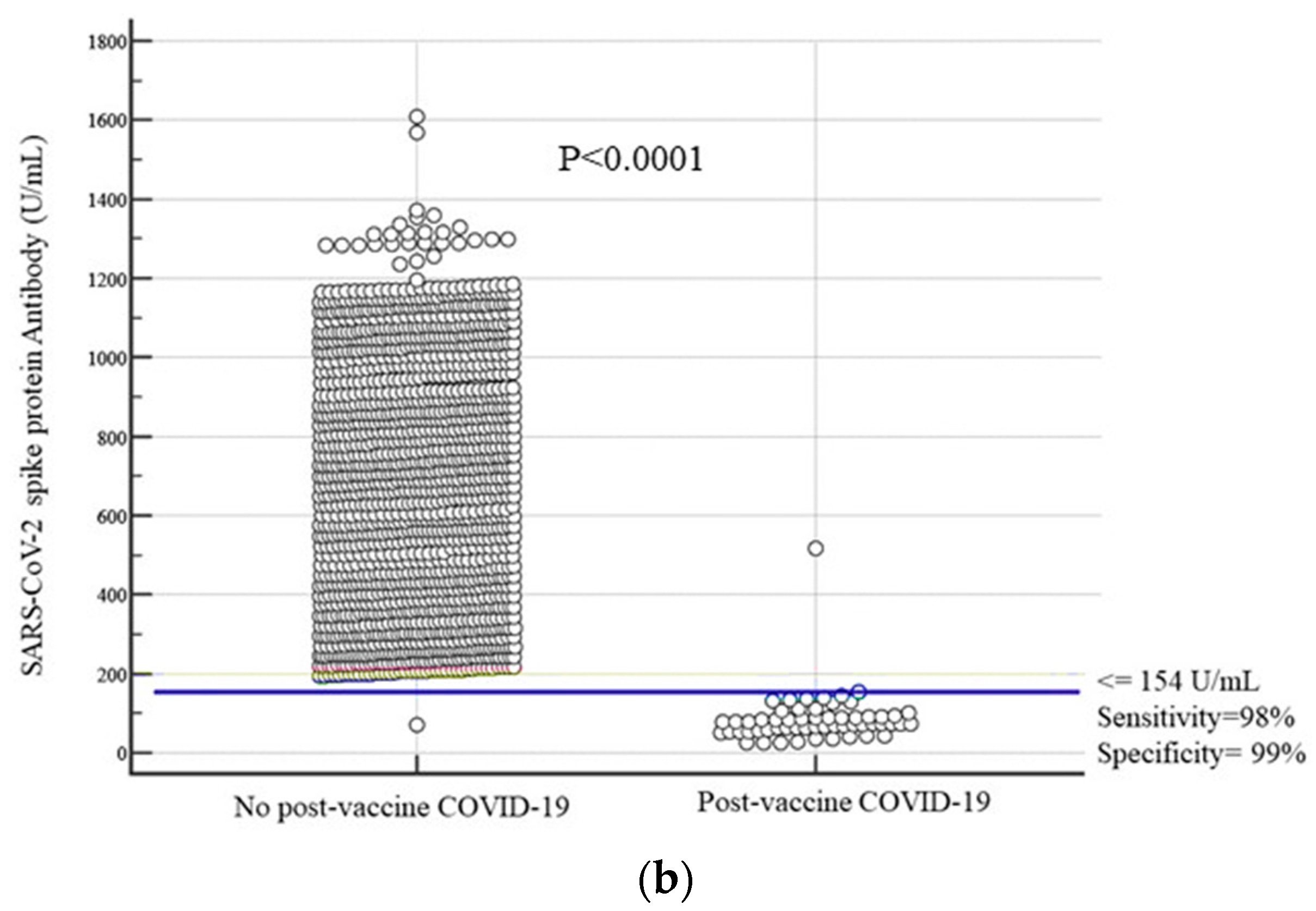
3.4. SARS-CoV-2 Antibody Dynamics
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation (WHO). Coronavirus Disease (COVID-19) (Internet). Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 16 November 2022).
- Johns Hopkins Corona Resource Center (Internet). Available online: https://coronavirus.jhu.edu/map.html (accessed on 20 November 2022).
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Feng, Z.; Xiang, N.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Munster, V.J.; Tamin, A.; Lloyd-Smith, J.O.; de Wit, T.; et al. Aerosol and Surface Stability of SARS-CoV-2 Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Bak, A.; Mugglestone, M.A.; Ratnaraja, N.V.; Wilson, J.A.; Loveday, H.P.; Rivett, L.; Wilson, A.; Islam, J.; Loveday, H.P.; Price, J.; et al. SARS-CoV-2 routes of transmission and recommendations for preventing acquisition: Joint British Infection Association (BIA), Healthcare Infection Society (HIS), Infection Prevention Society (IPS) and Royal College of Pathologists (RCPath) guidance. J. Hosp. Infect. 2021, 114, 79–103. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.C.; Biele, G.; Mühlemann, B.; Veith, T.; Schneider, J.; Beheim-Schwarzbach, J.; Drosten, C.; Corman, V.M.; Edelmann, A.; Stein, A.; et al. Estimating infectiousness throughout SARS-CoV-2 infection course. Science 2021, 373, eabi5273. [Google Scholar] [CrossRef]
- Walensky, R.P.; Walke, H.T.; Fauci, A.S. SARS-CoV-2 Variants of Concern in the United States-Challenges and Opportunities. JAMA 2021, 325, 1037–1038. [Google Scholar] [CrossRef]
- Gu, H.; Krishnan, P.; Ng, D.Y.M.; Chang, L.D.J.; Liu, G.Y.Z.; Cheng, S.S.M.; Hui, M.M.Y.; Fan, M.C.Y.; Wan, J.H.L.; Lau, L.H.K.; et al. Probable Transmission of SARS-CoV-2 Omicron Variant in Quarantine Hotel, Hong Kong, China, November 2021. Emerg. Infect. Dis. 2022, 28, 460–462. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Davis, B.D.; Chen, S.S.; Sincuir Martinez, J.M.; Plummer, J.T.; Vail, E. Emergence of a Novel SARS-CoV-2 Variant in Southern California. JAMA 2021, 325, 1324–1326. [Google Scholar] [CrossRef] [PubMed]
- Boehm, E.; Kronig, I.; Neher, R.A.; Eckerle, I.; Vetter, P.; Kaiser, L. Geneva Centre for Emerging Viral Diseases. Novel SARS-CoV-2 variants: The pandemics within the pandemic. Clin. Microbiol. Infect. 2021, 27, 1109–1117. [Google Scholar] [CrossRef]
- V’kovski, P.; Kratzel, A.; Steiner, S.; Stalder, H.; Thiel, V. Coronavirus biology and replication: Implications for SARS-CoV-2. Nat. Rev. Microbiol 2021, 19, 155–170. [Google Scholar] [CrossRef]
- Hillen, H.S.; Kokic, G.; Farnung, L.; Dienemann, C.; Tegunov, D.; Cramer, P. Structure of replicating SARS-CoV-2 polymerase. Nature 2020, 584, 154–156. [Google Scholar] [CrossRef]
- Troyano-Hernáez, P.; Reinosa, R.; Holguín, Á. Evolution of SARS-CoV-2 Envelope, Membrane, Nucleocapsid, and Spike Structural Proteins from the Beginning of the Pandemic to September 2020: A Global and Regional Approach by Epidemiological Week. Viruses 2021, 13, 243. [Google Scholar] [CrossRef] [PubMed]
- Ke, Z.; Oton, J.; Qu, K.; Cortese, M.; Zila, V.; McKeane, L.; Briggs, A. Structures and distributions of SARS-CoV-2 spike proteins on intact virions. Nature 2020, 588, 498–502. [Google Scholar] [CrossRef] [PubMed]
- Merad, M.; Blish, C.A.; Sallusto, F.; Iwasaki, A. The immunology and immunopathology of COVID-19. Science 2022, 375, 1122–1127. [Google Scholar] [CrossRef]
- Kasuga, Y.; Zhu, B.; Jang, K.J.; Yoo, J.S. Innate immune sensing of coronavirus and viral evasion strategies. Exp. Mol. Med. 2021, 53, 723–736. [Google Scholar] [CrossRef] [PubMed]
- Rydyznski Moderbacher, C.; Ramirez, S.I.; Dan, J.M.; Grifoni, A.; Hastie, K.M.; Weiskopf, D.S.; Crotty, S. Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity. Cell 2020, 183, 996–1012.e19. [Google Scholar] [CrossRef]
- Choi, A.; Koch, M.; Wu, K.; Dixon, G.; Oestreicher, J.; Legault, H.; Stewart-Jones, G.B.E.; Colpitts, T.; Pajon, R.; Bennett, H.; et al. Serum Neutralizing Activity of mRNA-1273 against SARS-CoV-2 Variants. J. Virol. 2021, 95, e0131321. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.X.; Liu, B.Z.; Deng, H.J.; Wu, G.C.; Deng, K.; Chen, Y.K. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 2020, 26, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.H.; Au, I.C.H.; Lau, K.T.K.; Lau, E.H.Y.; Cowling, B.J.; Leung, G.M. Real-world effectiveness of molnupiravir and nirmatrelvir plus ritonavir against mortality, hospitalization, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: An observational study. Lancet 2022, 400, 1213–1222. [Google Scholar]
- Gottlieb, R.L.; Nirula, A.; Chen, P.; Boscia, J.; Heller, B.; Morris, J. Effect of Bamlanivimab as Monotherapy or in Combination With Etesevimab on Viral Load in Patients With Mild to Moderate COVID-19: A Randomized Clinical Trial. JAMA 2021, 325, 632–644. [Google Scholar] [CrossRef]
- World Health Organisation (WHO). COVID-19 Vaccines (Internet). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 20 October 2022).
- Creech, C.B.; Walker, S.C.; Samuels, R.J. SARS-CoV-2 Vaccines. JAMA 2021, 325, 1318–1320. [Google Scholar] [CrossRef] [PubMed]
- Grumbach, K.; Carson, M.; Harris, O.O. Achieving Racial and Ethnic Equity in COVID-19 Vaccination: From Individual Readiness to Health System Readiness. JAMA Health Forum. 2021, 2, e211724. [Google Scholar] [CrossRef]
- Saudi Ministry of Health (Internet). Available online: https://covid19.moh.gov.sa/ (accessed on 20 November 2022).
- Falsey, A.R.; Sobieszczyk, M.E.; Hirsch, I.; Sproule, S.; Robb, M.L.; Corey, L.; Neuzil, K.M.; Hahn, W.; Hunt, J.; Mulligan, M.J.; et al. Phase 3 Safety and Efficacy of AZD1222 (ChAdOx1 nCoV-19) Covid-19 Vaccine. N. Engl. J. Med. 2021, 385, 2348–2360. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Baz, I.; Trobajo-Sanmartín, C.; Miqueleiz, A.; Guevara, M.; Fernández-Huerta, M.; Burgui, C.; Casado, I.; Portillo, M.E.; Navascués, A.; Ezpeleta, C.; et al. Product-specific COVID-19 vaccine effectiveness against secondary infection in close contacts, Navara, August 2021. Eurosurveillance 2021, 26, 2100894. [Google Scholar] [CrossRef] [PubMed]
- El Sahly, H.M.; Baden, L.R.; Essink, B.; Doblecki-Lewis, S.; Martin, J.M.; Anderson, E.J. Efficacy of the mRNA-1273 SARS-CoV-2 vaccine at completion of blinded phase. N. Engl. J. Med. 2021, 385, 1774–1785. [Google Scholar] [CrossRef] [PubMed]
- Skowronski, D.M.; De Serres, G. Safety and Efficacy of the BNT16. mRNA Covid-19 Vaccine. N. Engl. J. Med. 2021, 384, 1576–1578. [Google Scholar]
- Pasquale, S.; Gregorio, G.L.; Caterina, A.; Francesco, A.; Beatrice, P.M.; Vincenzo, P.; Caterina, P.M. COVID-19 in Low- and Middle-Income Countries (LMICs): A Narrative Review from Prevention to Vaccination Strategy. Vaccines 2021, 9, 1477. [Google Scholar] [CrossRef]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P. Oxford COVID Vaccine Trial Group. Safety and Efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A.; Hernán, M.A.; Lipsitch, M.; Reis, B.; Balicer, R.D. BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting. N. Engl. J. Med. Mass. Med. Soc. 2021, 384, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. Mass. Med. Soc. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Bergwerk, M.; Gonen, T.; Lustig, Y.; Amit, S.; Lipsitch, M.; Cohen, C.; Mandelboim, M.; Levin, E.G.; Rubin, C.; Indenbaum, V.; et al. COVID-19 Breakthrough Infections in Vaccinated Health Care Workers. N. Engl. J. Med. 2021, 385, 1474–1484. [Google Scholar] [CrossRef]
- Lipsitch, M.; Krammer, F.; Regev-Yochay, G.; Lustig, Y.; Balicer, R.D. SARS-CoV-2 breakthrough infections in vaccinated individuals: Measurement, causes and impact. Nat. Rev. Immunol. 2022, 22, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; McInnes, I.B.; McMurray, J.J.V. Obesity a risk factor for severe COVID-19 infection: Multiple potential mechanisms. Circulation 2020, 142, 4–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- El Bcheraoui, C.; Afshin, A.; Charara, R.; Khalil, I.; Moradi-Lakeh, M.; Kassebaum, N.J.; Collison, M.; Daoud, F. GBD 2015 Eastern Mediterranean Region Obesity Collaborators. The burden of obesity in the Eastern Mediterranean Region: Findings from the Global Burden of Disease 2015 study. Int. J. Public Health 2018, 63, 165–176. [Google Scholar]
- Singh, A.S.; Gupta, R.; Ghosh, A.; Misra, A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab. Syndr. 2020, 14, 303–310. [Google Scholar] [CrossRef]
- Al Dawish, M.A.; Robert, A.A.; Braham, R.; Al Hayek, A.A.; Al Saeed, A.; Ahmed, R.A.; Al Sabaan, F.S. Diabetes Mellitus in Saudi Arabia. Curr. Diabetes Rev. 2016, 12, 359–368. [Google Scholar] [CrossRef]
- Shang, J.; Wang, Q.; Zhang, H.; Wang, X.; Wan, J.; Yan, Y.; Gao, Y.; Cheng, J.; Li, Z.; Lin, J. The Relationship Between Diabetes Mellitus and COVID-19 Prognosis: A Retrospective Cohort Study in Wuhan, China. Am. J. Med. 2021, 134, e6–e14. [Google Scholar] [CrossRef]
- Robert, A.A.; Al Saeed, A.; Al Dawish, M.A. COVID-19 among people with diabetes mellitus in Saudi Arabia: Current situation and new perspectives. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 102231. [Google Scholar] [CrossRef]
- Alguwaihes, A.M.; Al-Sofiani, M.E.; Megdad, M.; Albader, S.S.; Alsari, M.H.; Alelayan, A.; Saad, H. Diabetes and COVID-19 among hospitalized patients in Saudi Arabia: A single-center retrospective study. Cardiovasc. Diabetol. 2020, 19, 20. [Google Scholar] [CrossRef]
- Saha, A.; Ahsan, M.M.; Quader, T.-U.; Naher, S.; Akter, F.; Mehedi, H.H.; Chowdhury, A.A.U.; Karim, H.; Rahman, T.; Parvin, A. Clinical characteristics and outcomes of COVID-19 infected diabetic patients admitted in ICUs of the southern region of Bangladesh. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 229–235. [Google Scholar] [CrossRef]
- Aihong, W.; Weibo, Z.; Zhangrong, X.; Jianwen, G. Timely blood glucose management for the outbreak of 2019 novel coronavirus disease (COVID-19) is urgently needed. Diabetes Res. Clin. Pract. 2020, 162, 108118. [Google Scholar]
- Moutschen, M.P.; Scheen, A.J.; Lefebvre, P.J. Impaired immune responses in diabetes mellitus: Analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabete Metab. 1992, 18, 187–201. [Google Scholar]
- Lee, K.A.; Ma, W.; Sikavi, D.R.; Drew, D.A.; Nguyen, L.H.; Bowyer, R.C.E.; Cardoso, M.J.; Fall, T.; Freidin, M.B.; Gomez, M.; et al. Cancer and Risk of COVID-19 Through a General Community Survey. Oncologist 2021, 26, e182–e185. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, M.; Puopolo, M.; Filia, A.; Sacco, C.; Mateo-Urdiales, A.; Alegiani, S.; Pezzotti, P. Effectiveness of an mRNA vaccine booster dose against SARS-CoV-2 infection and severe COVID-19 in persons aged ≥60 years and other high-risk groups during predominant circulation of the delta variant in Italy, July 19 to December 12 2021. Expert Rev. Vaccines 2022, 21, 1–8. [Google Scholar] [CrossRef]
- de Oliveira, P.M.N.; Mendes-De-Almeida, D.P.; Porto, V.B.G.; Cordeiro, C.C.; Teixeira, G.V.; Pedro, R.S.; Takey, P.R.G.; Lignani, L.K.; Xavier, J.R.; da Gama, V.C.D.; et al. Vaccine-induced immune thrombotic thrombocytopenia after COVID-19 Vaccination: Description of a series of 39 cases in Brazil. Vaccine 2022, 40, 4788–4795. [Google Scholar] [CrossRef] [PubMed]
- Greinacher, A.; Thiele, T.; Warkentin, T.E. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N. Engl. J. Med. 2021, 9, 33835769. [Google Scholar] [CrossRef]
- Alkindi, S.; Elsadek, R.; Al-Madhani, A.; Al-Musalhi, M.; Al-Khadouri, G.; Al Rawahi, B.; Al-Ruqeishi, S.; Al-Yazeedi, J.; Wali, Y.; Al Shamakhi, S.; et al. Impact of COVID-19 on vasooclusive crisis in patients with sickle cell anaemia. Int. J. Infect. Dis. 2021, 106, 128–133. [Google Scholar] [CrossRef]
- Alkindi, S.; Elsadek, R.A.; Pathare, A.V. Safety Warning for ChAdOx1 nCov-19 Vaccine in Patients with Sickle Cell Disease. Mediterr. J. Hematol. Infect. Dis. 2021, 13, e2021059. [Google Scholar] [CrossRef]
- Elnahry, A.G.; Al-Nawaflh, M.Y.; Gamal Eldin, A.A.; Solyman, O.; Sallam, A.B.; Phillips, P.H.; Elhusseiny, A.M. COVID-19 Vaccine-Associated Optic Neuropathy: A Systematic Review of 45 Patients. Vaccines 2022, 10, 1758. [Google Scholar] [CrossRef]
- Diaz, G.A.; Parsons, G.T.; Gering, S.K.; Meier, A.R.; Hutchinson, I.V.; Robicsek, A. Myocarditis and Pericarditis After Vaccination for COVID-19. JAMA 2021, 326, 1210–1212. [Google Scholar] [CrossRef]
- Montgomery, J.; Ryan, M.; Engler, R.; Hoffman, D.; McClenathan, B.; Collins, L.; Loran, D.; Hrncir, D.; Herring, K.; Platzer, M.; et al. Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021, 6, 1202. [Google Scholar] [CrossRef]
- Kim, H.W.; Jenista, E.R.; Wendell, D.C.; Azevedo, C.F.; Campbell, M.J.; Darty, S.N.; Parker, M.A.; Kim, R.J. Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol. 2021, 6, 1196. [Google Scholar] [CrossRef]
- Allen, C.M.; Ramsamy, S.; Tarr, A.W.; Tighe, P.J.; Irving, W.L.; Tanasescu, R.; Evans, J.R. Guillain-Barré Syndrome Variant Occurring after SARS-CoV-2 Vaccination. Ann. Neurol. 2021, 90, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Finsterer, J. Exacerbating Guillain-Barré Syndrome Eight Days after Vector-Based COVID-19 Vaccination. Case Rep. Infect. Dis. 2021, 2021, 3619131. [Google Scholar] [CrossRef] [PubMed]
- Maramattom, B.V.; Krishnan, P.; Paul, R.; Padmanabhan, S.; Nampoothiri, D.S.C.V.; Syed, A.A.; Mangat, H.S. Guillain-Barré Syndrome following ChAdOx1-S / nCoV -19 Vaccine. Ann. Neurol. 2021, 90, 312–314. [Google Scholar] [CrossRef] [PubMed]
- Hatzakis, A.; Karabinis, A.; Roussos, S.; Pantazis, N.; Degiannis, D.; Chaidaroglou, A.; Petsios, K.; Pavlopoulou, I.; Tsiodras, S.; Paraskevis, D.; et al. Modelling SARS-CoV-2 Binding Antibody Waning 8 Months after BNT162b2 vaccination. Vaccines 2022, 10, 285. [Google Scholar] [CrossRef]
- Levin, E.G.; Lustig, Y.; Cohen, C.; Fluss, R.; Indenbaum, V.; Amit, S.; Doolman, R.; Asraf, K.; Mendelson, E.; Ziv, A.; et al. Waning Immune Humoral Response to BNT162b2 Covid-19 Vaccine over 6 Months. N. Engl. J. Med. 2021, 385, e84. [Google Scholar] [CrossRef]
- Israel, A.; Shenhar, Y.; Green, I.; Merzon, E.; Golan-Cohen, A.; Schäffer, A.A.; Ruppin, E.; Vinker, S.; Magen, E. Large-Scale Study of Antibody Titer Decay following BNT162b2 mRNA Vaccine or SARS-CoV-2 Infection. Vaccines 2021, 10, 64. [Google Scholar] [CrossRef]
- Doria-Rose, N.; Suthar, M.S.; Makowski, M.; O’Connell, S.; McDermott, A.B.; Flach, B.; Ledgerwood, J.E.; Mascola, J.R.; Graham, B.S.; Lin, B.C.; et al. Antibody Persistence through 6 Months after the Second Dose of mRNA-1273 Vaccine for Covid-19. N. Engl. J. Med. 2021, 384, 2259–2261. [Google Scholar] [CrossRef]


| Parameters | Group A (n = 503) ChAdOx1 nCoV-19 Vaccine | Group B (n = 521) BNT162b2 Vaccine | Group C (N = 476) mRNA-1273 Vaccine | p Value between the Three Vaccinated Groups | Control Group (n = 1500) | p Value between Vaccinated and Non-Vaccinated |
|---|---|---|---|---|---|---|
| Age (years) Mean ± SD | 46.31 ± 14.99 | 44.63 ± 15.63 | 43.79 ± 15.62 | 0.08 | 45.09 ± 16.19 | 0.06 |
| Males; n (%) | 295 (58.65) | 301 (57.77) | 258 (54.2) | 0.36 | 846 (56.4) | 0.45 |
| Nationality | ||||||
| Saudi; n (%) | 256 (50.89) | 267(51.25) | 244 (51.26) | 0.89 | 743 (49.53) | 0.38(1.976% to 5.170%) |
| Non-Saudi; n (%) | 247 (49.15) | 254 (48.75) | 232 (48.75) | 757 (50.47) | ||
| Patients with Comorbidities: Total 386 (25.73%) | p value between the three vaccinated groups; p (95% CI) | p value between vaccinated and non-vaccinated; p (95% CI) | ||||
| Diabetes mellitus; n (%) | 67 (13.32) | 65 (12.48) | 58 (12.18) | 0.54 (−2.344% to 4.878% | 149 (9.30) | 0.41 (−1.363% to 3.364% |
| Hypertension; n (%) | 51 (10.14) | 46 (8.83) | 40 (8.40) | 0.33 (−1.479% to 4.887% | 96 (6.4) | 0.08; (−0.209% to 4.114%) |
| Dyslipidemia; n (%) | 50 (9.94) | 49 (9.4) | 43 (9.03) | 0.64 (−2.292% to 4.097%0 | 83 (5.53) | 0.06; (−0.063% to 4.328%) |
| Overweight/Obesity; n (%) | 49 (9.74) | 58 (11.13) | 55 (11.55) | 0.35 (−1.934% to 4.607%) | 265 (17.7) | p < 0.0001 (17.303% to 22.946%) |
| Cardiac disease; n (%) | 21 (4.17) | 18 (3.45) | 19 (3.99) | 0.62 (−1.447% to 2.865%) | 46 (3.07) | 0.002 **; (0.9527% to 4.1357%) |
| Chronic liver disease; n (%) | 12 (2.34) | 9 (1.73) | 13 (2.73) | 0.89 (−1.391% to 1.992%) | 34 (2.30) | <0.0001 **; (1.747% to 4.149%) |
| Chronic renal disease; n (%) | 9 (1.79) | 8 (1.54) | 6 (1.26) | 0.562 (−0.873% to 2.064% | 59 (3.90) | <0.0001 **; 2.4695% to 5.0889% |
| Hemoglobinopathies; n (%) | 17 (3.38) | 20 (3.84) | 18 (3.78) | 0.72 (−1.841% to 2.229% | 65 (4.33) | 0.241; (−0.569% to 2.243%) |
| Neurologic disorders; n (%) | 8 (1.59) | 10 (1.92) | 7 (1.47) | 0.88 (−1.534% to 1.386% | 57 (3.80) | <0.0001 **; (2.152% to 4.779%) |
| Autoimmune disorders; n (%) | 16 (3.18) | 21 (4.03) | 19 (3.99) | 0.42 (−1.362% to 2.686%) | 68 (4.53) | 0.473; (−0.929% to 1.997%) |
| Malignancy (patients with breast cancer, lymphoma, and prostate cancer); n (%) | 6 (1.19) | 11 (2.11) | 8 (1.68) | 0.32 (−0.841% to 1.93% | 103 (6.87) | <0.0001 **; (3.789% to 6.692%) |
| COVID-19 Cases and Hospitalizations after Vaccines and Booster Doses | Group A (n = 503) ChAdOx1 nCoV-19Vaccine | Group B (n = 521) BNT162b2 Vaccine | Group C (N = 476) mRNA-1273 | p Value and 95% CI between the Three Vaccines | COVID-19 Cases and Hospitalizations in the Control Group throughout the Study (n = 1500) | p Value between Vaccinated and Non-Vaccinated Control Subjects |
|---|---|---|---|---|---|---|
| Participants with confirmed RT-PCR COVID-19 (Cases) after the first vaccine dose; (n,%) | 113 (22.46%) | 66 (12.67%) | 67(14.08%) | <0.0001 ** | 564 (38%) | <0.0001 ** |
| Participants with confirmed RT-PCR COVID-19 (cases) after the second vaccine dose (n,%) | 23 (4.6) | 16 (3.07) | 18 (3. 80) | 0.37 (−1.118% to 3.5%) | ||
| Relative risk (RR); (95% CI) | 0.124 (0.083 to 0.186) | 0.083 (0.051 to 0.135) | 0.10 (0.065 to 0.162) | |||
| Vaccine effectiveness (VE); Relative risk reduction (RRR) | 89% 0.89 | 92% 0.92 | 90% 0.90 | ChAdOx1 nCoV-19 vs. BNT162b2: 0.025 ChAdOx1 nCoV-19 vs. mRNA-1273 : 0.298 BNT162b2 vs. mRNA-1273: 0.244 | ||
| Absolute risk reduction % (ARR) | 37.36%; | 38.75%; | 38.15%; | 0.68 (−4.14% to 6.22%) | ||
| Number needed to vaccinate (NNV) (benefit) | 3.09 | 2.95 | 3.02 | |||
| 95% CI | 2.724 (Benefit) to 3.570 (Benefit) | 2.625 (Benefit) to 3.375 (Benefit) | 2.660 (Benefit) to 3.483 (Benefit) | |||
| COVID-19 (cases after the first booster dose; (n,%) | 4 (0.79) | 3 (0.58) | 3 (0.63) | 0.67 (−0.664% to 1.461%) | ||
| Relative risk after the first booster (95% CI) | 0.024 (0.009 to 0.057) | 0.014; (0.0044 to 0.0425) | 0.015; (0.0049 to 0.047) | 0.19; (−0.444% to 2.784%) | ||
| Relative risk reduction (RRR) | 0.98 | 0.99 | 0.99 | 0.51; −(0.844% to 2.158%) | ||
| Absolute risk reduction (ARR) | 41.10% | 41.40% | 41.30% | 0.93; −(5.046% to 5.474%) | ||
| Participants with confirmed RT-PCR COVID-19 (Cases) after the second booster dose; (n,%) | 0 | 0 | 0 | |||
| Hospitalizations after the vaccine’s first dose | 12 (2.38) | 5 (0.95) | 7 (1.47) | 0.09 (−0.255% to 3.206%) | 103/554 (18.6%) | <0.0001 |
| Hospitalizations after the vaccine’s second dose | 2 (3.9) | 1 (0.19) | 0 | 0.05 * | ||
| Hospitalizations after vaccine boosters 1 or 2 | 0 | 0 | 0 |
| Vaccinated Participants with Comorbidities: (n = 386; 25.73% of the Study Cohort) | COVID-19 Cases after Vaccine Second Dose in Vaccinated Participants with Comorbidities; n (%) | COVID-19 cases after Booster 1 | COVID-19-Related Hospitalizations after Vaccines Second Dose or Booster 1 | Relative Risk (RR.) (95% CI) | Vaccines Effectiveness in Participants with Comorbidities | COVID-19 Cases in Unvaccinated Controls | p Value between COVID-19 Cases in Vaccinated and Unvaccinated Participants with Comorbidities |
|---|---|---|---|---|---|---|---|
| Diabetes mellitus; n = 190 | 11/190 (5.8%) | 2 (1.05) | 1 (0.5%) | 0.137 (0.075 to 0.25) | 86.3% | 63/149 (35.2%) | 0.0001 |
| Hypertension; n = 137 | 2 (1.5%) | 0 | 0 | 0.04 (0.009 0.163) | 96% | 35/96 (21.7%) | 0.0001 |
| Dyslipidemia; n = 142 | 1 (0.7%) | 0 | 0 | 0.019 (0.0054 to 0.251 | 98% | 31/83 (17.9%) | <0.0001 |
| Overweight/Obesity; n = 162 BMI 30–40 BMI > 40 | 3 (1.85) 17 (10.49) | 0 2 (1.23%) | 0 0 | 0.285 (0.186 to 0.439) | 82% | 166/265 (27.1%) | <0.0001 |
| Cardiac disease; n = 58 | 0 | 0 | 0 | 0.017 (0.003 to 0.649) | 98.3% | 23/46 (24%) | 0.004** |
| Chronic liver disease; N = 34 | 0 | 0 | 0 | 0.04 (0.0052 to 1.218) | 98% | 12/34 (18.75%) | 0.02* |
| Chronic renal disease; n = 23 | 1 (4.3%) | 1 (4.3%) | 0 | 0.066 (0.009 to 0.451) | 93.4% | 39/59 (48.1%) | 0.005** |
| Hemoglobinopathies; n = 55 | 2 (3.6%) | 0 | 0 | 0.074 (0.019 to 0.294) | 92.6% | 32/65 (32.3%) | 0.002** |
| Neurologic/psychiatric disorders; n = 25 | 0 | 0 | 0 | 0.057 (0.004 to 0.912) | 94.3% | 19/57 (24. 5%) | 0.04* |
| Autoimmune disorders; n = 56 | 10 (17.9%) | 3 (5.4%) | 1 (1.79%) | 0.229 (0.129 to 0.408) | 80% | 53/68 (78%) | <0.0001** |
| Malignancy; n = 25 | 4 (16%) | 2 (8%) | 1 (4%) | 0.204 (0.082 to 0.502) | 80% | 81/103 (71.8%) | 0.0006** |
| Parameters | Group A (n = 503) ChAdOx1 nCoV-19 Vaccine | Group B (n = 521) BNT162b2 Vaccine | Group C (n = 476) mRNA-1273 Vaccine | p Value; (95% CI) |
|---|---|---|---|---|
| Pain at the injection site | 526 (89.31) | 375 (89.07) | 308 (90.59) | 0.880; (−3.413% to 4.525%) |
| Fever > 38.5 °C | 137 (23.26) | 46 (10.93) | 57 (16.76) | <0.0001 **; (5.0826% to 13.5058%) |
| Fatigue > 2 days | 294 (49.92) | 113 (26.84) | 127 (37.35) | p < 0.0001 **; (12.2457% to 22.6466%) |
| Headache > 2 days | 174 (29.54) | 72 (17.10) | 69 (20.29) | p < 0.0001 **; (6.8979% to 16.1204%) |
| Chills | 35 (5.94) | 19 (4.51) | 24 (7.06) | 0.975; (−2.474% to 2.690%) |
| Muscle pain | 78 (13.24) | 43 (10.21) | 31 (9.12) | 0.084; (−0.406% to 6.534) |
| Skin reaction at the injection site; n (%) | 45 (7.64) | 18 (4.28) | 21 (6.1) | 0.11; (−0.493% to 4.959%) |
| Vomiting or diarrhea | 13 (2.21) | 7 (1.66) | 8 (2.35) | 0.895 (−1.407% to 1.762%) |
| Abdominal pain | 31 (5.26) | 10 (2.31) | 13 (3.82) | 0.003 **; (0.969% to 5.280%) |
| Thrombosis | 11 | 1 | 1 | |
| Numbness | 17 (2.89) | 4 (0.95) | 3 (0.88) | 0.005 **; (0.595% to 3.723%) |
| Joint pains | 29 (4.92) | 9 (2.14) | 7 (2.06) | <0.0001 **; (2.339% to 6.181%) |
| Sleep disorders | 18 (3.06) | 3 (0.71) | 2 (0.59) | 0.457; (−1.091% to 2.591%) |
| Anxiety/restlessness | 5 (0.85) | 1 (0.24) | 1 (0.29) | 0.1020; (−0.194% to 1.765%) |
| Palpitations; n (%) | 17 (2.89) | 6 (1.43) | 4 (1.18) | 0.026 *; (0.1823% to 3.4698%) |
| Thrombosis | 3 (1.8) | 0 | 0 | 0.013 *; (0.32% to 3.19%) |
| Myocarditis | 1 | 1 | 0 | 1.0000 (−1.4% to 1.4%) |
| Visual disturbances | 1 (0.34) | 0 | 0 (0.00) | 1.0000; (−1.1129% to 0.855%) |
| Anaphylaxis | 0 | 1 | 1 | 1.0000 (−1.4% to 1.5%) |
| Guillain–Barré syndrome | 0 | 1 | 0 | 1.0000 (−1.4% to 1.4%) |
| Seizures | 0 | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamal, S.M.; Naghib, M.M.; Daadour, M.; Alsuliman, M.N.; Alanazi, Z.G.; Basalem, A.A.; Alaskar, A.M.; Saed, K. The Outcome of BNT162b2, ChAdOx1-Sand mRNA-1273 Vaccines and Two Boosters: A Prospective Longitudinal Real-World Study. Viruses 2023, 15, 326. https://doi.org/10.3390/v15020326
Kamal SM, Naghib MM, Daadour M, Alsuliman MN, Alanazi ZG, Basalem AA, Alaskar AM, Saed K. The Outcome of BNT162b2, ChAdOx1-Sand mRNA-1273 Vaccines and Two Boosters: A Prospective Longitudinal Real-World Study. Viruses. 2023; 15(2):326. https://doi.org/10.3390/v15020326
Chicago/Turabian StyleKamal, Sanaa M., Moheyeldeen Mohamed Naghib, Moataz Daadour, Mansour N. Alsuliman, Ziad G. Alanazi, Abdulaziz Abdullah Basalem, Abdulaziz M. Alaskar, and Khaled Saed. 2023. "The Outcome of BNT162b2, ChAdOx1-Sand mRNA-1273 Vaccines and Two Boosters: A Prospective Longitudinal Real-World Study" Viruses 15, no. 2: 326. https://doi.org/10.3390/v15020326




