Physicochemical and Biological Performance of Aloe Vera-Incorporated Native Collagen Films
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Mixture Preparation
2.3. Film Processing
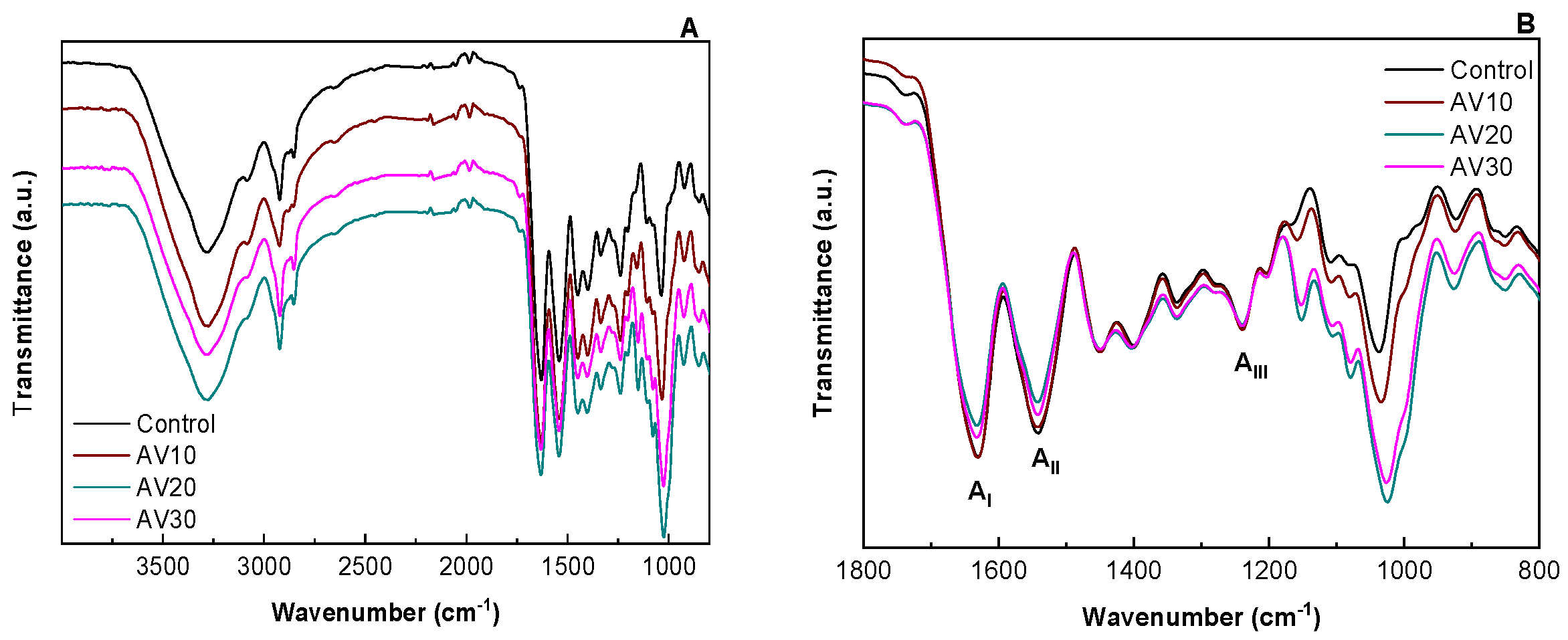
2.4. Fourier Transform Infrared (FTIR) Spectroscopy
2.5. Moisture Content (MC) and Mass Loss (ML)
2.6. Water Uptake (WU)
2.7. Thermo-Gravimetric Analysis (TGA)
2.8. Differential Scanning Calorimetry (DSC)
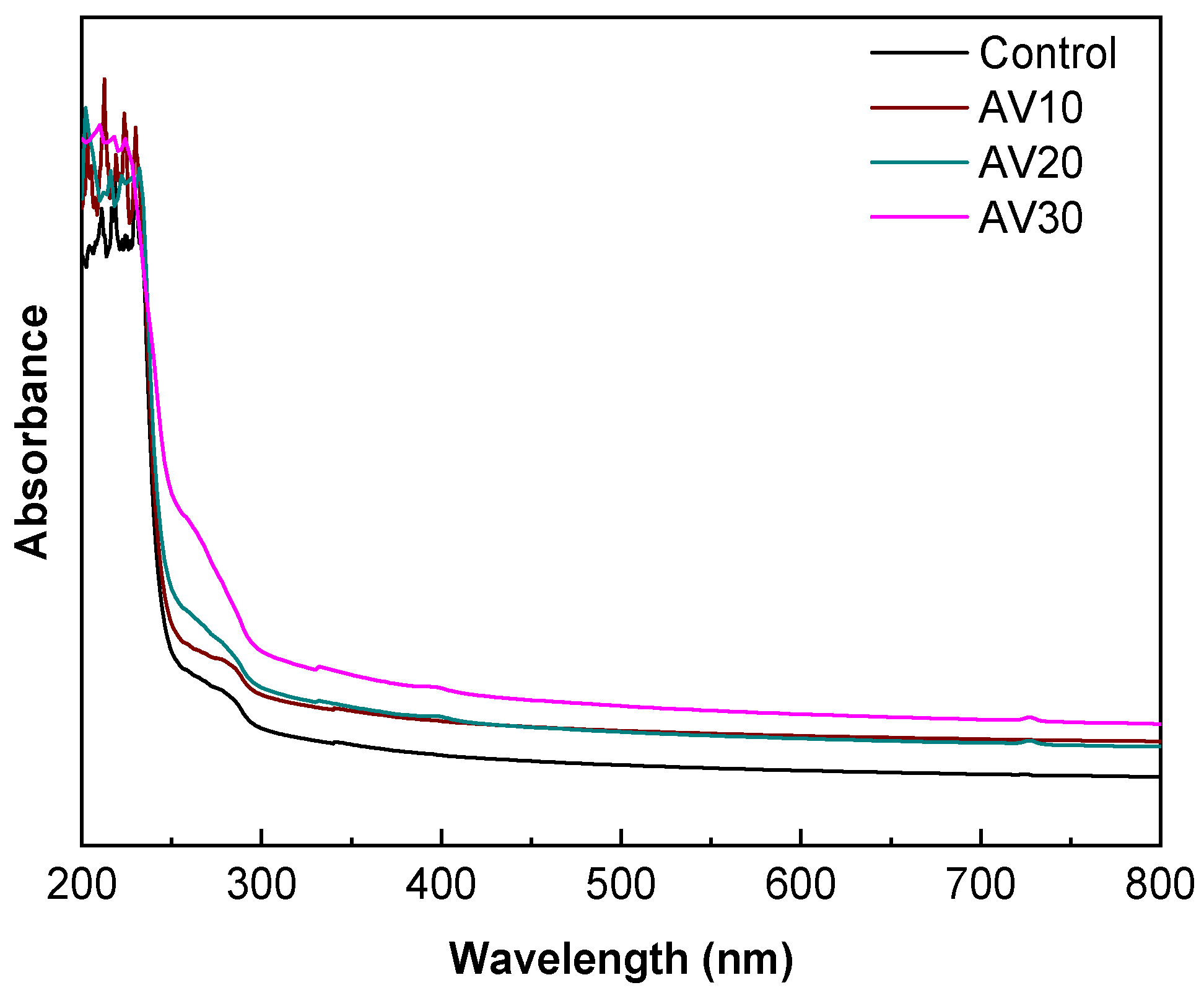
2.9. Ultraviolet–Visible (UV–Vis) Spectroscopy
2.10. Water Contact Angle (WCA)
2.11. Mechanical Properties
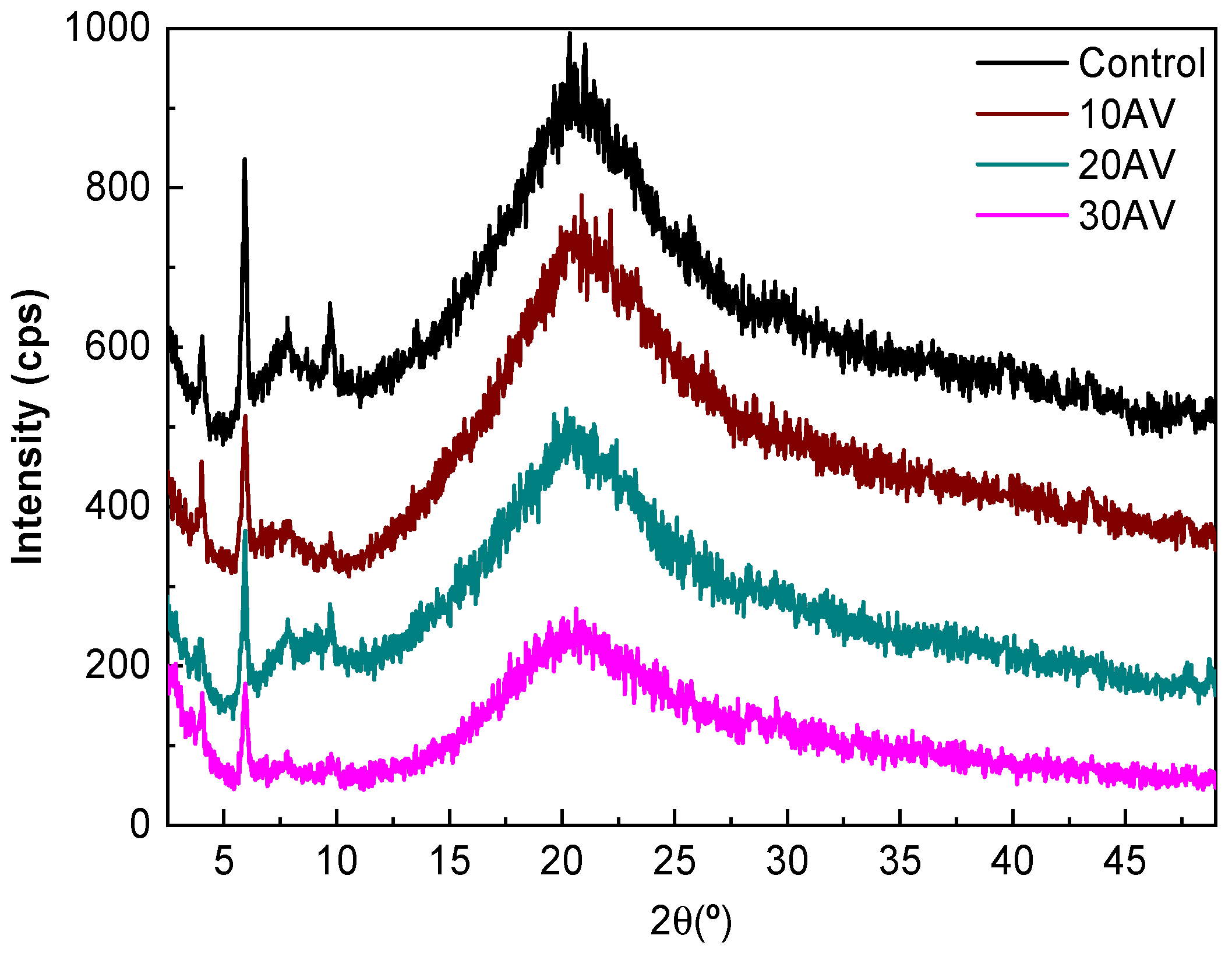
2.12. X-ray Diffraction (XRD)
2.13. Scanning Electron Microscopy (SEM)
2.14. Degradation Studies
2.15. Cell Culture
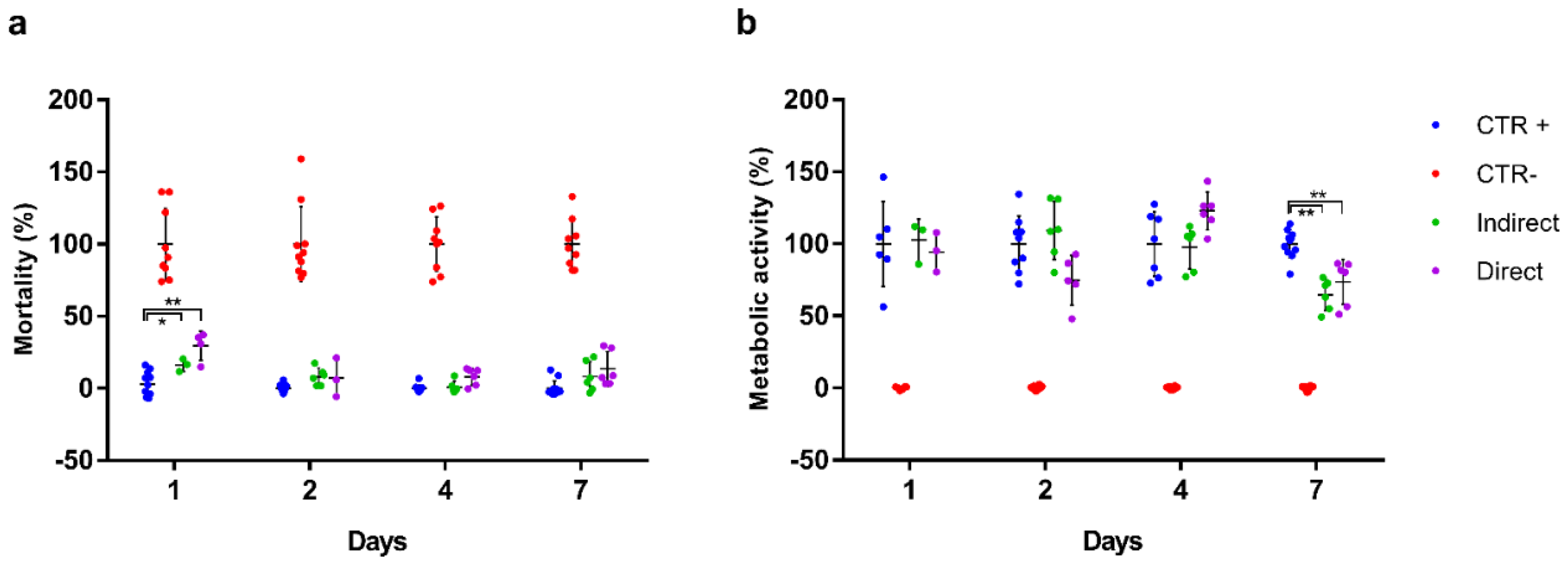
2.16. Biocompatibility Assay
2.17. Statistical Analysis
3. Results and Discussion
3.1. Physicochemical Properties
3.2. Thermal Properties
3.3. Barrier and Mechanical Properties
3.4. Morphological Properties
3.5. Degradation and Biocompatibility Studies
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Singh, H.; Singh, S.; Prakash, C. Current trends in biomaterials and bio-manufacturing. In Biomanufacturing; Prakash, C., Singh, S., Singh, R., Ramakrishna, S., Pabla, B.S., Puri, S., Uddin, M.S., Eds.; Springer: Cham, Switzerland, 2019; pp. 1–34. [Google Scholar]
- Nagarajan, S.; Radhakrishnan, S.; Kalkura, S.N.; Balme, S.; Miele, P.; Bechelany, M. Overview of protein-based biopolymers for biomedical application. Macromol. Chem. Phys. 2019, 220, 14. [Google Scholar] [CrossRef]
- Rajalekshmy, G.P.; Lekshmi, D.L.; Joseph, J.; Rekha, M.R. An overview on the potential biomedical applications of polysaccharides. In Functional Polysaccharides for Biomedical Applications; Maiti, S., Jana, S., Eds.; Woodhead Publishing: Duxford, UK, 2019; pp. 33–94. [Google Scholar]
- Jahangirian, H.; Azizi, S.; Rafiee-Moghaddam, R.; Baratvand, B.; Webster, T.J. Status of plant protein-based green scaffolds for regenerative medicine applications. Biomolecules 2019, 9, 619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigaroodi, F.; Shafaei, H.; Karimipour, M.; Dolatkhah, M.A.; Delazar, A. Aloe Vera/Collagen mixture induced integrin α1β1 and PECAM-1 genes expression in human adiposed-derived stem cells. Adv. Pharm. Bull. 2019, 9, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Meyer, M. Processing of collagen based biomaterials and the resulting materials properties. Biomed. Eng. Online 2019, 18, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Myllyharju, J.; Kivirikko, K. Collagens and collagen-related diseases. Ann. Med. 2001, 33, 7–21. [Google Scholar] [CrossRef]
- Aoki, K.; Saito, N. Biodegradable polymers as drug delivery systems for bone regeneration. Pharmaceutics 2020, 12, 95. [Google Scholar] [CrossRef] [Green Version]
- Naskar, A.; Kim, K.S. Recent advances in nanomaterial-based wound healing therapeutics. Pharmaceutics 2020, 12, 499. [Google Scholar] [CrossRef]
- Parenteau-Bareil, R.; Gauvin, R.; Berthod, F. Collagen-based biomaterials for tissue engineering applications. Materials 2010, 3, 1863–1887. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.H.; Hsieh, D.J.; Periasamy, S.; Chuang, C.T.; Tseng, F.W.; Kuo, J.C.; Tarng, Y.W. Regenerative porcine dermal collagen matrix developed by supercritical carbon dioxide extraction technology: Role in accelerated wound healing. Materialia 2020, 9, 100576. [Google Scholar] [CrossRef]
- Abdollahi, M.; Rezai, M.; Jafarpour, A.; Undeland, I. Sequential extraction of gel-forming proteins, collagen and collagen hydrolysate from gutted silver carp (Hypophthalmichthys molitrix), a biorefinery approach. Food Chem. 2018, 242, 568–578. [Google Scholar] [CrossRef]
- Gallo, N.; Lunetti, P.; Bettini, S.; Barca, A.; Madaghiele, M.; Valli, L.; Capobianco, L.; Sannino, A.; Salvatore, L. Assessment of physico-chemical and biological properties of sericin-collagen substrates for PNS regeneration. Int. J. Polym. Mat. 2020. In Press. [Google Scholar] [CrossRef]
- Ahtzaz, S.; Sher Waris, T.; Shahzadi, L.; Anwar Chaudhry, A.; Ur Rehman, I.; Yar, M. Boron for tissue regeneration-it’s loading into chitosan/collagen hydrogels and testing on chorioallantoic membrane to study the effect on angiogenesis. Int. J. Polym. Mat. 2020, 69, 525–534. [Google Scholar] [CrossRef]
- Nagarajan, U.; Kawakami, K.; Zhang, S.; Chandrasekaran, B.; Nair, B.U. Fabrication of solid collagen nanoparticles using electrospray deposition. Chem. Pharm. Bull. 2014, 62, 422–428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Las Heras, K.; Santos-Vizcaino, E.; Garrido, T.; Borja Gutierrez, F.; Aguirre, J.J.; de la Caba, K.; Guerrero, P.; Igartua, M.; Hernandez, R.M. Soy protein and chitin sponge-like scaffolds: From natural by-products to cell delivery systems for biomedical applications. Green Chem. 2020, 22, 3445–3460. [Google Scholar] [CrossRef]
- David, G. Collagen-based 3D structures-versatile, efficient materials for biomedical applications. In Biopolymer-Based Formulations; Pal, K., Banerjee, I., Sarkar, P., Kim, D., Deng, W.P., Dubey, N.K., Majumder, K., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 881–906. [Google Scholar]
- Ghorbani, M.; Nezhad-Mokhtari, P.; Ramazani, S. Aloe vera-loaded nanofibrous scaffold based on Zein/Polycaprolactone/Collagen for wound healing. Int. J. Biol. Macromol. 2020, 153, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Jithendra, P.; Rajam, A.M.; Kalaivani, T.; Mandal, A.B.; Rose, C. Preparation and characterization of aloe vera blended collagen-chitosan composite scaffold for tissue engineering applications. ACS Appl. Mater. Interfaces 2013, 5, 7291–7298. [Google Scholar] [CrossRef]
- Patel, P.; Harshitha, C.G.; Shoba, M.S. Aloe vera: Functional and processing value in food. Int. J. Chem. Stud. 2019, 7, 714–721. [Google Scholar]
- Femenia, A.; Sánchez, E.S.; Simal, S.; Rosselló, C. Compositional features of polysaccharides from Aloe vera (Aloe barbadensis Miller) plant tissues. Carbohydr. Polym. 1999, 39, 109–117. [Google Scholar] [CrossRef]
- Rethinam, S.; Vihayan, S.; Aruni, A.W.; Basaran, B.; Alagumuthu, T.; Ramamoorthy, R. Enhanced tissue regeneration using an nano-bioactive scaffold—A novel perspective. Mater. Chem. Phys. 2020, 240, 122303. [Google Scholar] [CrossRef]
- Isfandiary, A.; Widiyanti, P.; Hikmawati, D. Composite of chitosan-collagen-aloe vera for scaffolds application on skin tissue. J. Biomimetics Biomater. Biomed. Eng. 2017, 32, 82–89. [Google Scholar] [CrossRef]
- Langmead, L.; Makins, R.J.; Rampton, D.S. Anti-inflammatory effects of Aloe vera gel in human colorectal mucosa in vitro. Aliment. Pharmacol. Ther. 2004, 19, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Tarameshloo, M.; Norouzian, M.; Zarein-Dolab, S.; Dadpay, M.; Mohsenifar, J.; Gazor, R. Aloe vera gel and thyroid hormone cream may improve wound healing in Wistar rats. Anat. Cell Biol. 2012, 45, 170–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syed, T.; Afzal, M.; Ahmad, S.A.; Holt, A.; Ahmad, S.A.; Ahmad, S. Management of genital herpes in men with 0.5% Aloe vera extract in a hydrophilic cream: A placebo-controlled double-blind study. J. Dermatol. Treat. 2009, 8, 99–102. [Google Scholar] [CrossRef]
- Olatunya, O.S.; Olatunya, A.M.; Anyabolu, H.C.; Adejuyigbe, E.A.; Oyelami, O.A. Preliminary trial of Aloe vera gruel on HIV infection. J. Altern. Complement. Med. 2012, 18, 850–853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mansour, G.; Ouda, S.; Shaker, A.; Abdallah, H.M. Clinical efficacy of new Aloe vera and myrrh-based oral mucoadhesive gels in the management of minor recurrent aphthous stomatitis: A randomized, double-blind, vehicle-controlled study. J. Oral Pathol. Med. 2014, 43, 405–409. [Google Scholar] [CrossRef]
- Radha, M.H.; Laxmipriya, N.P. Evaluation of biological properties and clinical effectiveness of Aloe vera: A systematic review. J. Tradit. Complement. Med. 2015, 5, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Devaraj, S.; Jialal, R.; Jialal, I.; Rockwood, J. A pilot randomized placebo controlled trial of 2 Aloe vera supplements in patients with pre-diabetes/metabolic syndrome. Planta Med. 2008, 74, 77. [Google Scholar] [CrossRef]
- Chen, C.P.; Wang, B.; Weng, Y.M. Physiochemical and antimicrobial properties of edible aloe/gelatin composite films. Int. J. Food Sci. Technol. 2010, 45, 1050–1055. [Google Scholar] [CrossRef]
- Pereira, R.; Mendes, A.; Bártolo, P. Alginate/aloe vera hydrogel films for biomedical applications. Proc. CIRP 2013, 5, 210–215. [Google Scholar] [CrossRef]
- Silva, S.S.; Popa, E.G.; Gomes, M.E.; Cerqueira, M.; Marques, A.P.; Caridade, S.G.; Teixeira, P.; Sousa, C.; Mano, J.F.; Reis, R.L. An investigation of the potential application of chitosan/Aloe-based membranes for regenerative medicine. Acta Biomater. 2013, 9, 6790–6797. [Google Scholar] [CrossRef] [Green Version]
- Dadashzadeh, A.; Imani, R.; Moghassemi, S.; Omidfar, K.; Abolfathi, N. Study off hybrid alginate/gelatin hydrogel-incorporated niosomal Aloe vera as potential skin wound dressing. Polym. Bull. 2019, 77, 387–403. [Google Scholar] [CrossRef]
- Valencia, G.A.; Luciano, C.G.; Lourenço, R.V.; Bittante, A.M.Q.B.; Sobral, P.J.A. Morphological and physical properties of nano-biocomposite films base on collagen loaded with laponite®. Food Packag. Shelf Life 2019, 19, 24–30. [Google Scholar] [CrossRef]
- Andonegi, M.; de la Caba, K.; Guerrero, P. Effect of citric acid on collagen sheets processed by compression. Food Hydrocoll. 2020, 100, 105427. [Google Scholar] [CrossRef]
- Bajer, D.; Janczak, K.; Bajer, K. Novel starch/chitosan/aloe vera composites as promising biopackaging materials. J. Polym. Environ. 2020, 28, 1021–1039. [Google Scholar] [CrossRef] [Green Version]
- Kapashi, E.; Kapnisti, M.; Dafnomili, A.; Noli, F. Aloe Vera as an effective biosorbent for the removal of thorium and barium from aqueous solutions. J. Radioanal. Nucl. Chem. 2019, 321, 217–226. [Google Scholar] [CrossRef]
- Kiran, P.; Rao, P.S. Development and characterization of reconstituted hydrogel from Aloe vera (Aloe barbadensis Miler) powder. J. Food Meas. Charact. 2016, 10, 411–424. [Google Scholar] [CrossRef]
- Ahlawat, K.S.; Khatkar, B.S. Processing, food applications and safety of aloe vera product indicating the interactions of collagen with the additives incorporated in the formulations: A review. J. Food Sci. Technol. 2011, 48, 525–533. [Google Scholar] [CrossRef] [Green Version]
- El-Azazy, M.; Dimassi, S.N.; El-Shafie, A.S.; Issa, A.A. Bio-Waste Aloe vera leaves as an efficient adsorbent for titan yellow from wastewater. Appl. Sci. 2019, 9, 4856. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Wang, W.; Wang, Y.; Guo, Y.; Duan, S.; Zhao, K.; Li, S. Metal ions increase mechanical strength and barrier properties of collagen-sodium polyacrylate composite films. Int. J. Biol. Macromol. 2018, 119, 15–22. [Google Scholar] [CrossRef]
- Shadangi, K.P.; Mohanty, K. Kinetic study and thermal analysis of the pyrolysis of non-edible oilseed powders by thermogravimetric and differential scanning calorimetric analysis. Renew. Energy 2014, 63, 337–344. [Google Scholar] [CrossRef]
- Bozec, L.; Odlyha, M. Thermal denaturation studies of collagen by microthermal analysis and atomic force microscopy. Biophys. J. 2011, 101, 228–236. [Google Scholar] [CrossRef] [Green Version]
- Shi, D.; Liu, F.; Yu, Z.; Chang, B.; Goff, H.D.; Zhong, F. Effect of aging treatment on the physicochemical properties of collagen films. Food Hydrocoll. 2019, 87, 436–447. [Google Scholar] [CrossRef]
- Duan, R.; Zhang, J.; Du, X.; Yao, X.; Konno, K. Properties of collagen from skin, scales and bone of carp (Cyprinus carpio). Food Chem. 2009, 112, 702–706. [Google Scholar] [CrossRef]
- Chen, S.; Chen, H.; Xie, Q.; Hong, B.; Chen, J.; Hua, F.; Bai, K.; He, J.; Yi, R.; Wu, H. Rapid isolation of high purity pepsin-soluble type I collagen from scales of red drum fish (Sciaenops ocellatus). Food Hydrocoll. 2016, 52, 468–477. [Google Scholar] [CrossRef]
- Dey, A.; Bera, R.; Chakrabarty, D. Influence of Aloe vera on the properties of N-vinylpyrrolidone-Acrylamide copolymer hydrogel. Mater. Chem. Phys. 2015, 168, 168–179. [Google Scholar] [CrossRef]
- Perumal, R.K.; Perumal, S.P.; Thangam, R.; Gopinath, A.; Ramadass, S.K.; Madhan, B.; Sivasubramanian, S. Collagen-fucoidan blend film with the potential to induce fibroblast proliferation for regenerative applications. Int. J. Biol. Macromol. 2018, 106, 1032–1040. [Google Scholar] [CrossRef]
- Zou, Y.; Wang, L.; Cai, P.; Li, P.; Zhang, M.; Sun, Z.; Sun, C.; Xu, W.; Wang, D. Effect of ultrasound assisted extraction on the physicochemical and functional properties of collagen from soft-shelled turtle calipash. Int. J. Biol. Macromol. 2017, 105, 1602–1610. [Google Scholar] [CrossRef]
- Liao, W.; Guanghua, X.; Li, Y.; Shen, X.R.; Li, C. Comparison of characteristics and fibril-forming ability of skin collagen from barramundi (Lates calcarifer) and tilapia (Oreochromis niloticus). Int. J. Biol. Macromol. 2018, 107, 549–559. [Google Scholar] [CrossRef]
- Shekhter, A.B.; Fayzullin, A.L.; Vukolova, M.N.; Rudenko, T.G.; Osipycheva, V.D.; Litvitsky, P.F. Medical applications of collagen and collagen-based materials. Curr. Med. Chem. 2019, 26, 506–516. [Google Scholar] [CrossRef]
- Hu, K.; Cui, F.; Lv, Q.; Ma, J.; Feng, Q.; Xu, L.; Fan, D. Preparation of fibroin/recombinant human—Like collagen scaffold to promote fibroblasts compatibility. J. Biomed. Mater. Res. A 2008, 84, 483–490. [Google Scholar] [CrossRef]




| Film | MC (%) | ML (%) |
|---|---|---|
| Control | 12.2 ± 0.7 a | 21.9 ± 0.7 a |
| AV10 | 9.8 ± 0.4 b | 31.1 ± 0.8 b |
| AV20 | 7.3 ± 0.4 c | 31.7 ± 0.5 b |
| AV30 | 5.8 ± 0.6 c | 35.6 ± 0.8 c |
| Film | WCA (°) | YM (MPa) | TS (MPa) | EAB (%) |
|---|---|---|---|---|
| Control | 107 ± 5 a | 805 ± 25 a | 13.8 ± 1.1 a | 13.5 ± 1.0 a |
| AV10 | 106 ± 3 a | 840 ± 11 a,b | 11.5 ± 0.8 b | 11.5 ± 1.2 b |
| AV20 | 97 ± 3 b | 867 ± 11 a,b | 11.3 ± 1.3 b | 11.2 ± 0.8 b |
| AV30 | 86 ± 5 c | 879 ± 52 a,b | 10.2 ± 0.7 b | 8.6 ± 0.8 c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andonegi, M.; Irastorza, A.; Izeta, A.; de la Caba, K.; Guerrero, P. Physicochemical and Biological Performance of Aloe Vera-Incorporated Native Collagen Films. Pharmaceutics 2020, 12, 1173. https://doi.org/10.3390/pharmaceutics12121173
Andonegi M, Irastorza A, Izeta A, de la Caba K, Guerrero P. Physicochemical and Biological Performance of Aloe Vera-Incorporated Native Collagen Films. Pharmaceutics. 2020; 12(12):1173. https://doi.org/10.3390/pharmaceutics12121173
Chicago/Turabian StyleAndonegi, Mireia, Ainhoa Irastorza, Ander Izeta, Koro de la Caba, and Pedro Guerrero. 2020. "Physicochemical and Biological Performance of Aloe Vera-Incorporated Native Collagen Films" Pharmaceutics 12, no. 12: 1173. https://doi.org/10.3390/pharmaceutics12121173







