The Therapeutic Effect and In Vivo Assessment of Palmitoyl- GDPH on the Wound Healing Process
Abstract
:1. Introduction
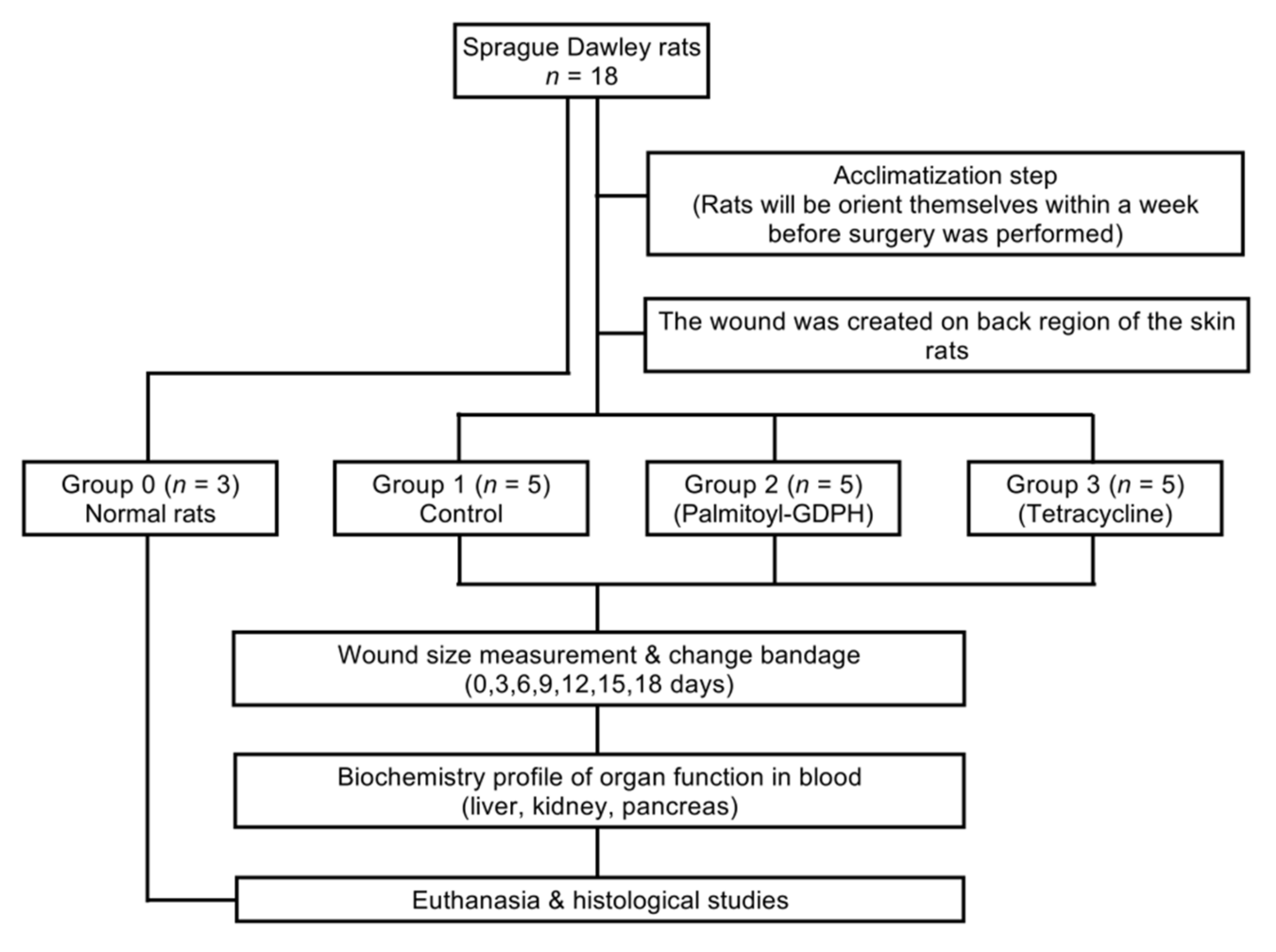
2. Materials and Methods
2.1. Synthesis and Characterization of Peptide
2.2. Ethical Requirement
2.3. Animals and Management
2.4. Excisional Wound
2.5. Topical Application of Therapeutic Agent
2.6. Determination of Body Weight Changes
2.7. Examination of Wound Contraction
2.8. Histological Analysis
2.8.1. Tissue Preparation
2.8.2. Hematoxylin and Eosin (H & E) Staining
2.8.3. Masson’s Trichome Staining
2.9. Collagen Density Evaluation
2.10. Quantitative Histomorphometry
2.11. Assessment of Skin Generation
2.12. Determination of Hematological and Biochemical Endpoints
2.13. Statistical Analysis
3. Results and Discussion
3.1. Properties of Palmitoyl-GDPH
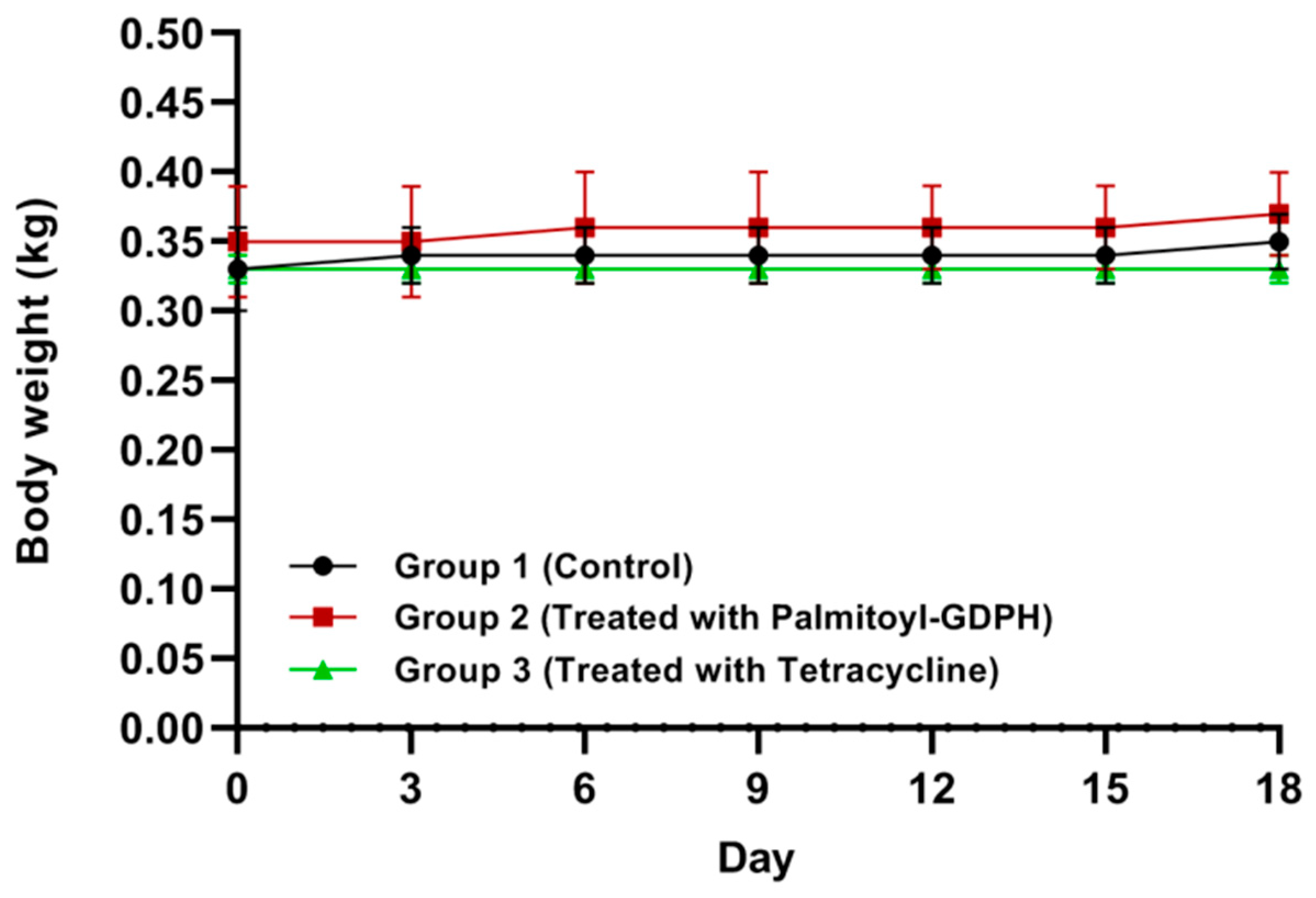
3.2. Effects of Palmitoyl-GDPH on Body Weight
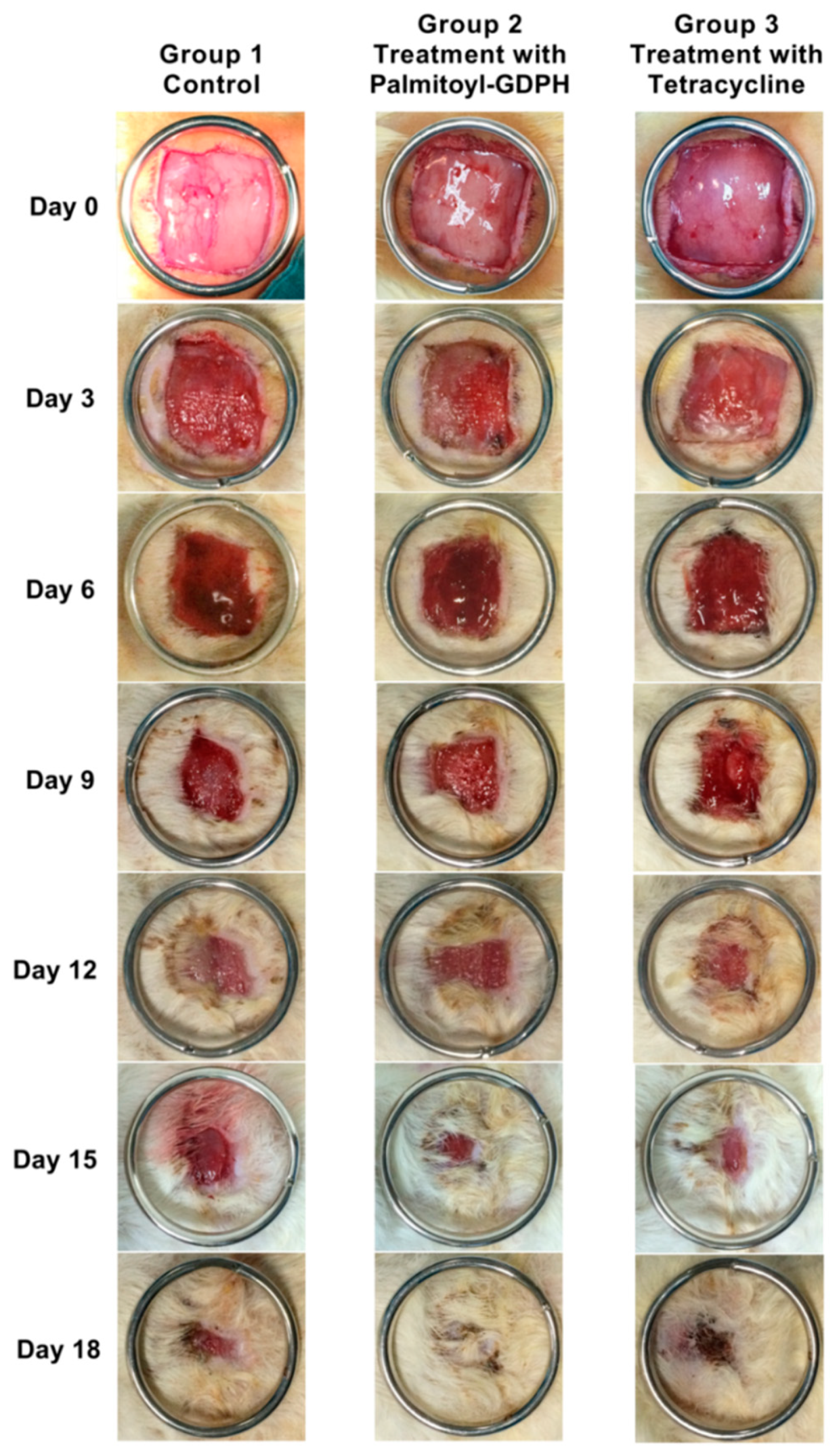
3.3. Wound Contraction Measurement
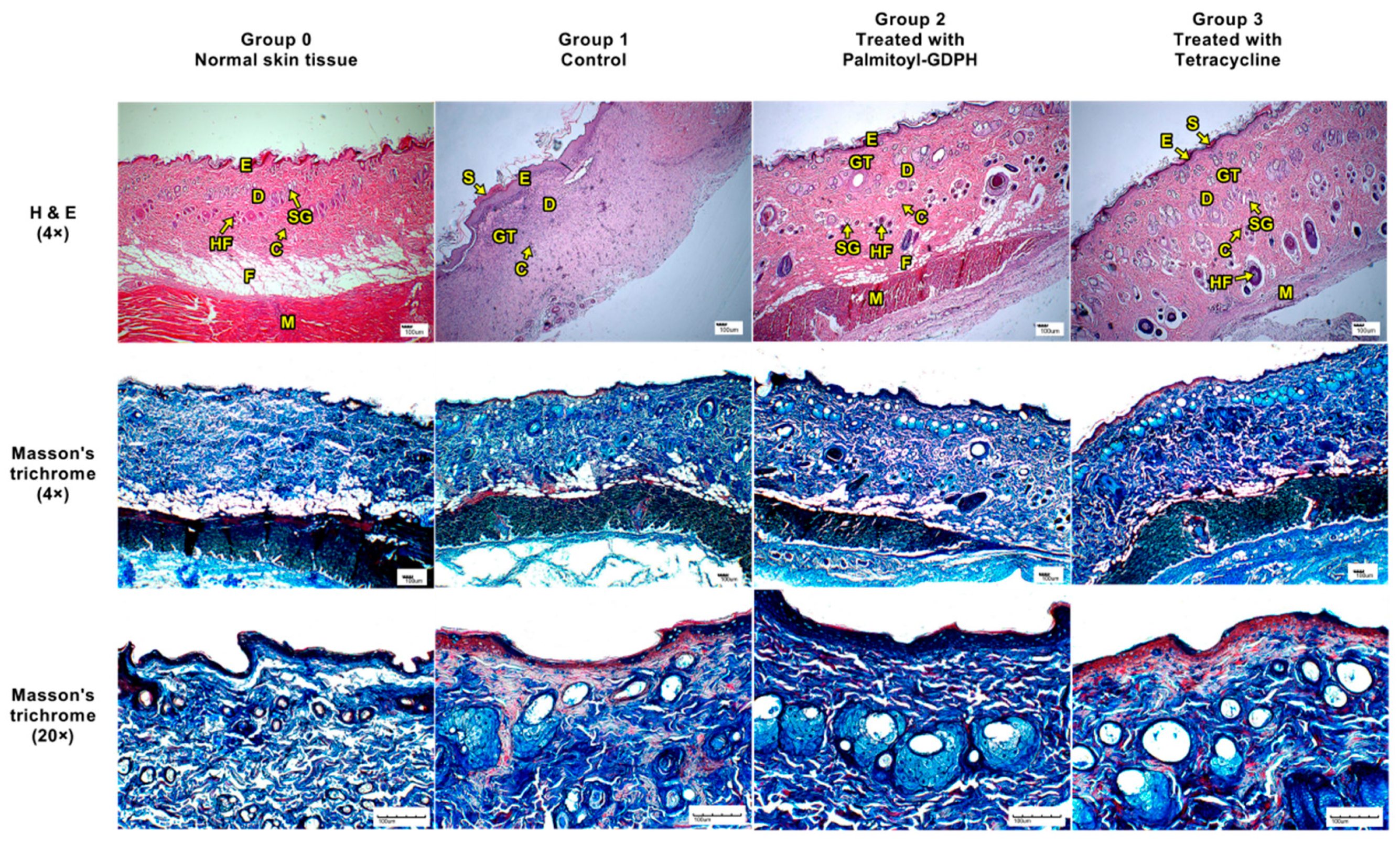
3.4. Histological Assessment
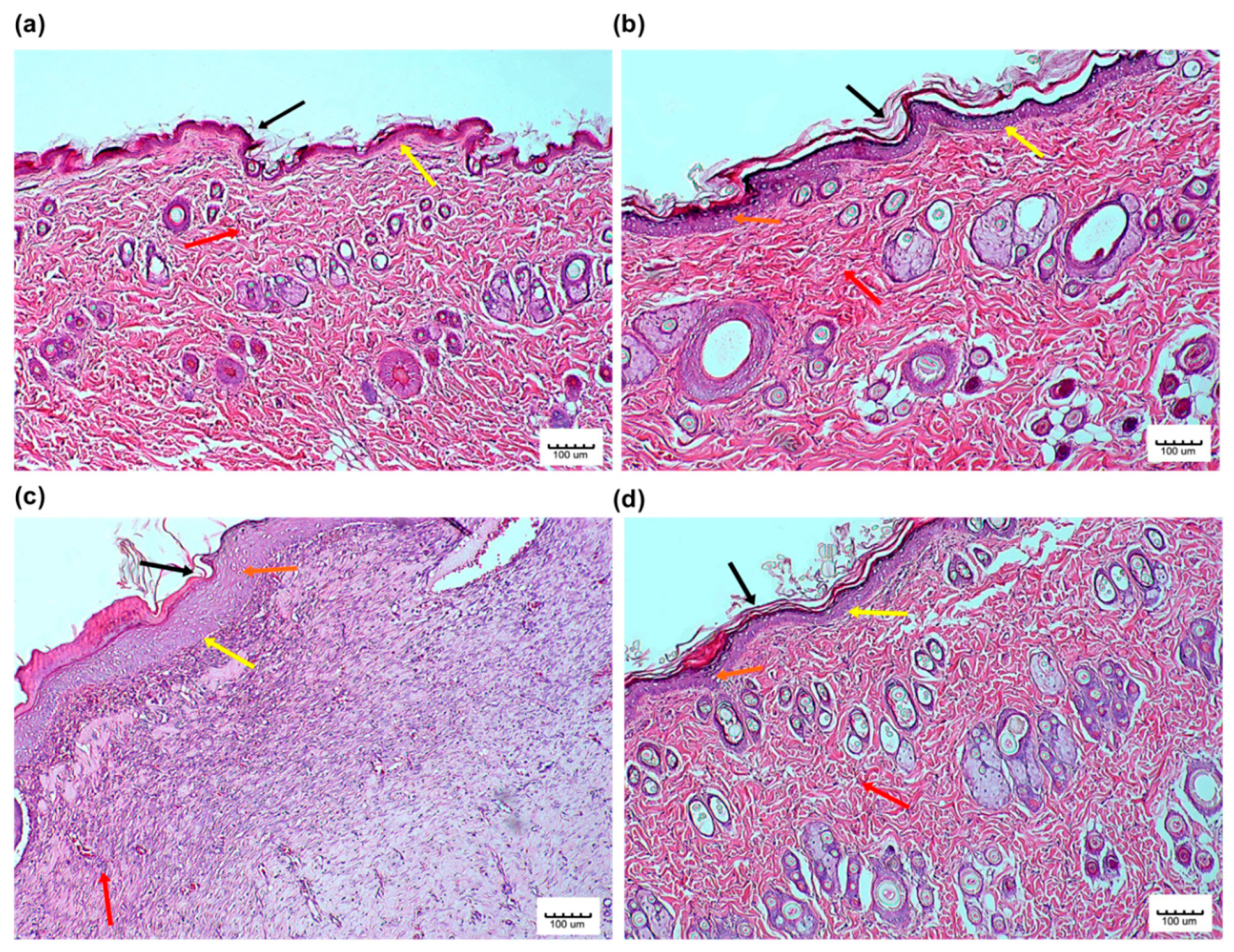
3.4.1. Hematoxylin and Eosin (H & E) and Masson’s Trichrome Staining
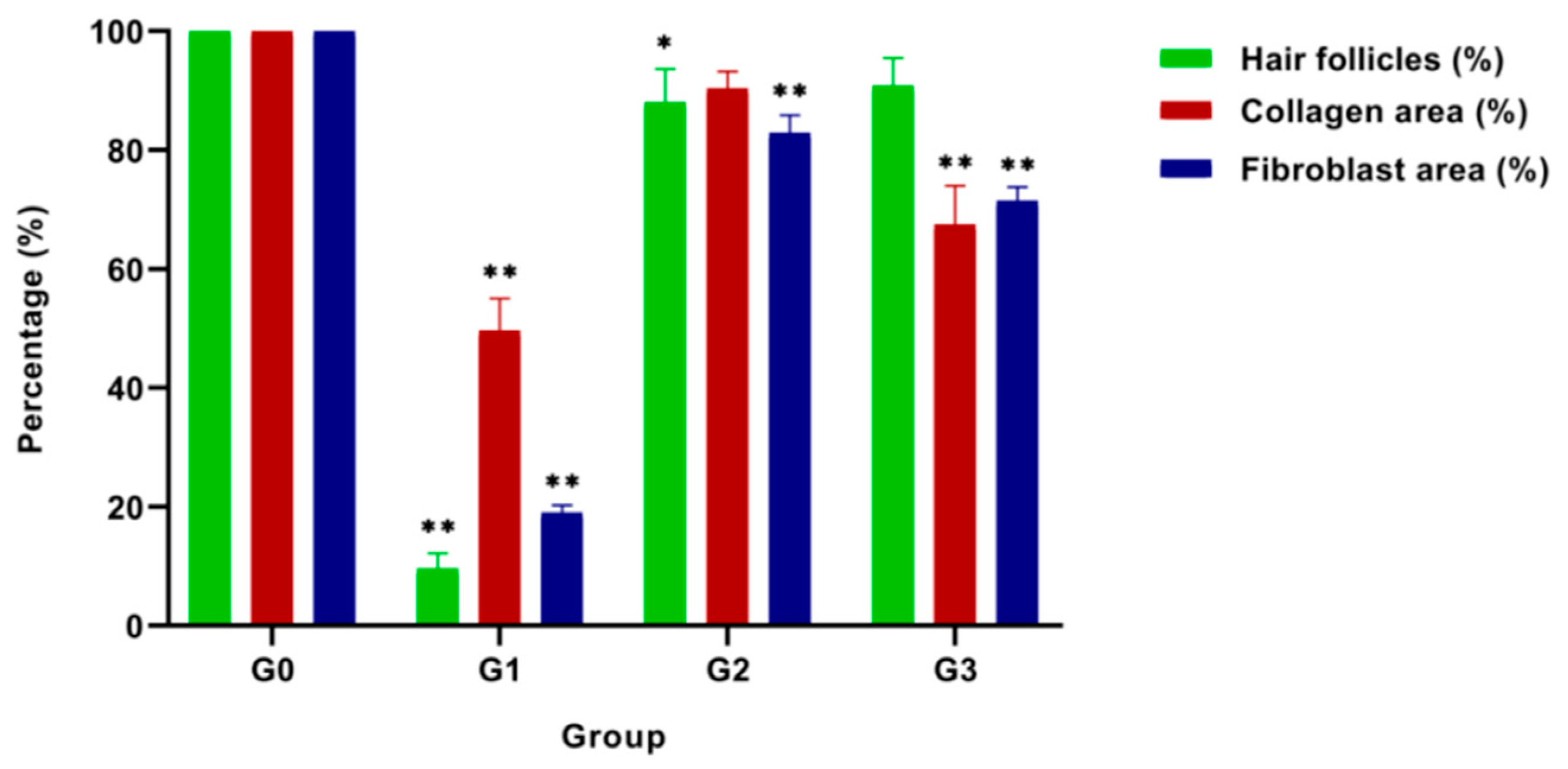
3.4.2. Wound Maturity
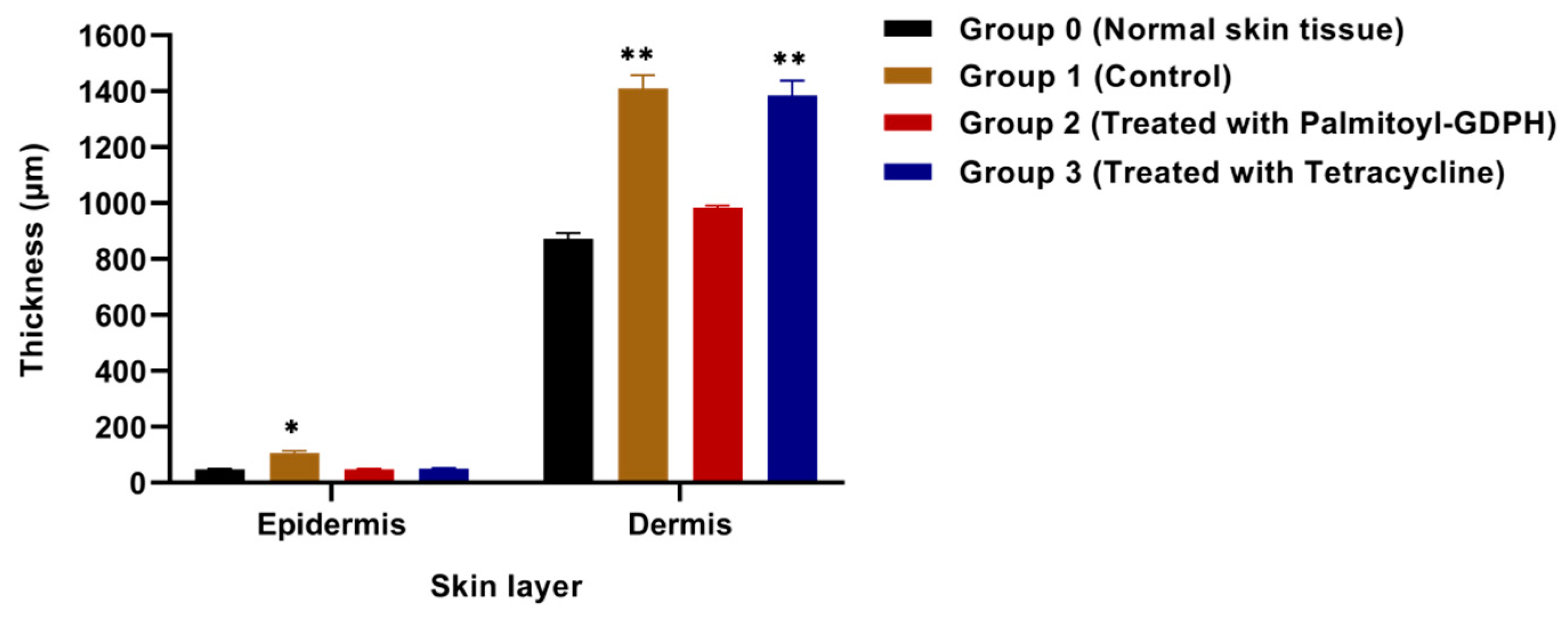
3.4.3. Epidermal and Dermal Thickness
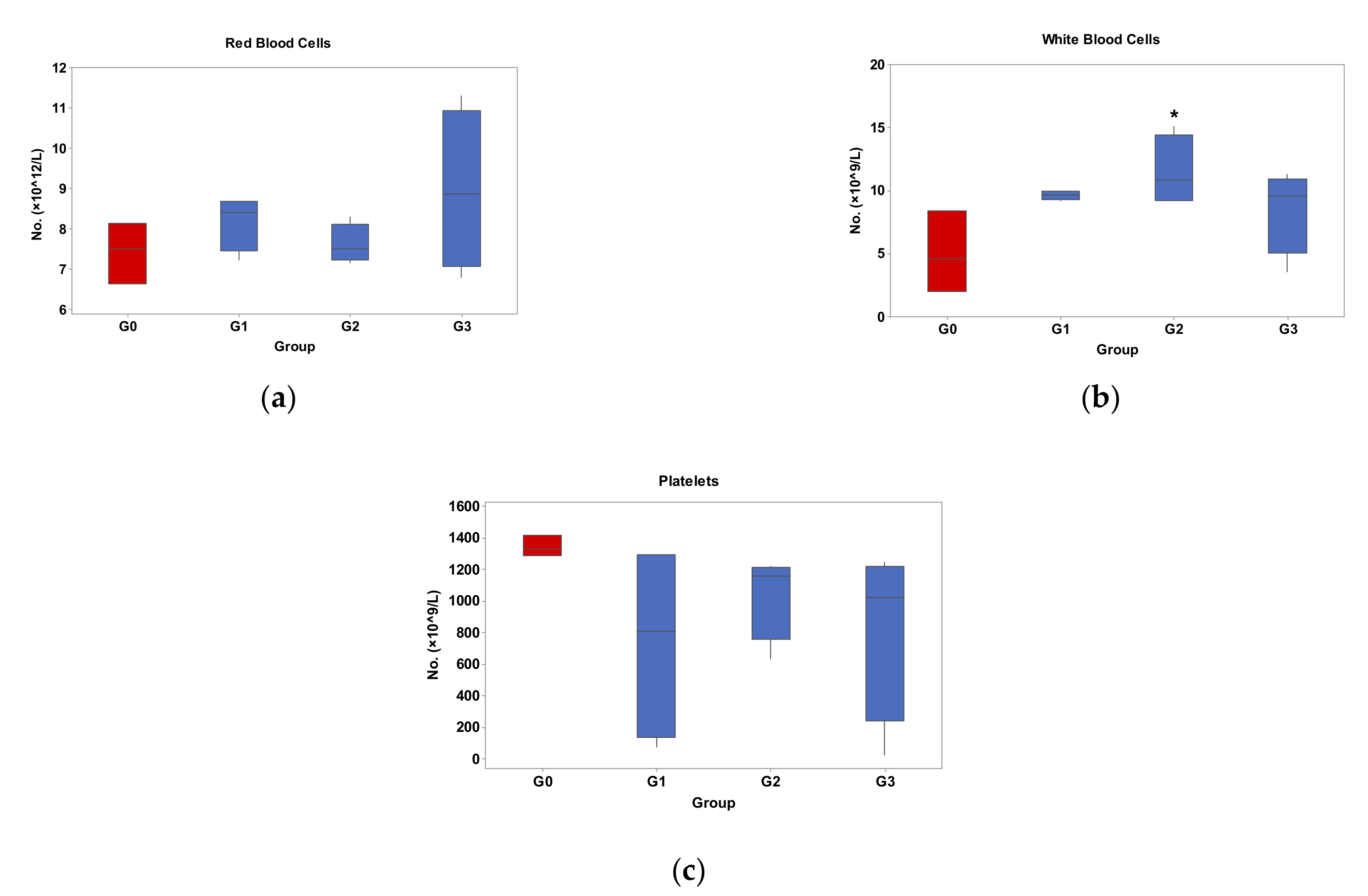
3.5. Effects of Palmitoyl-GDPH on Hematological Indices
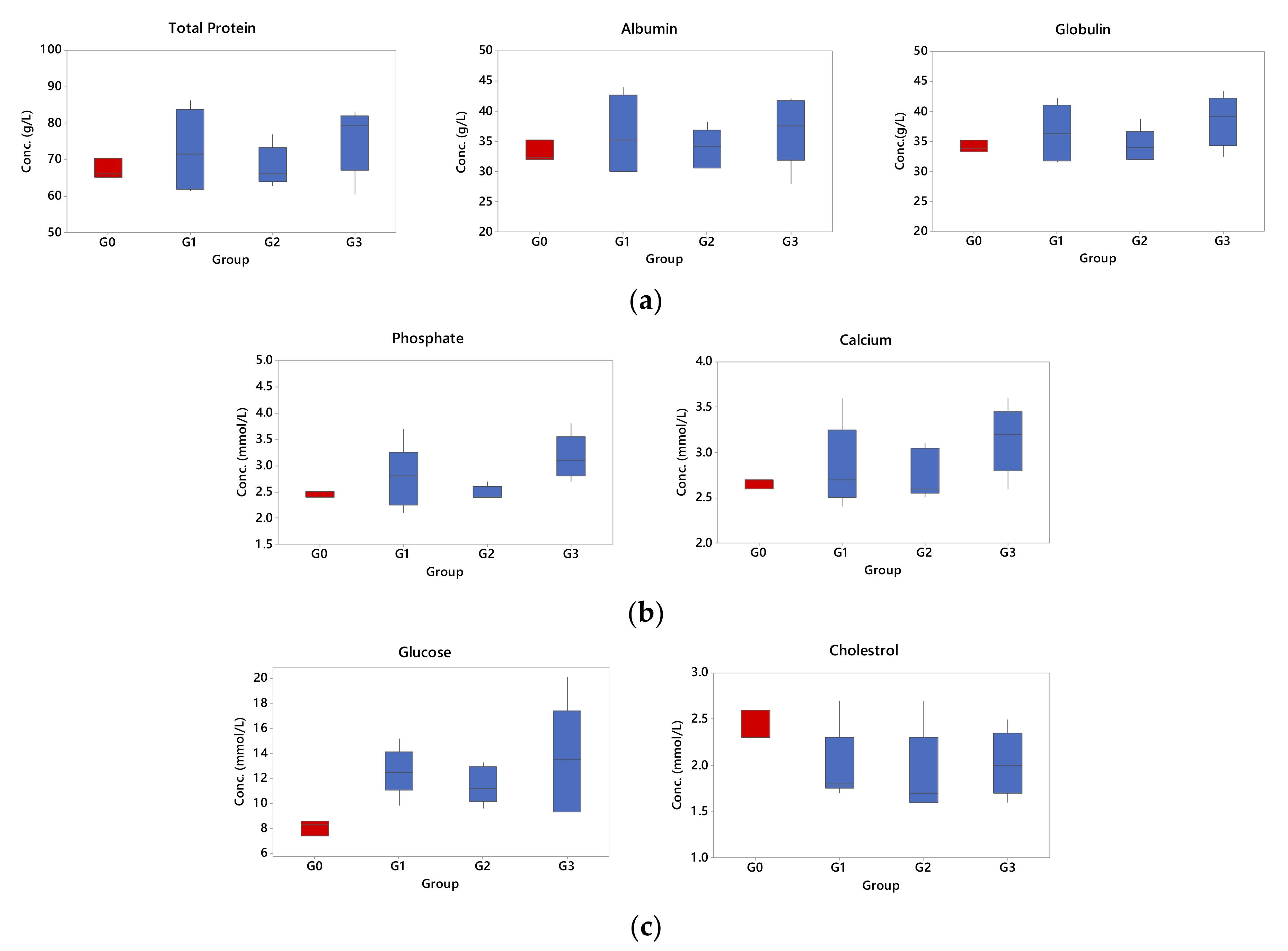
3.6. Effects of Palmitoyl-GDPH on Selected Organ Biomarkers
4. Conclusions
5. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, Y.; Wu, C.; Zhang, X.; Bian, W.; Liu, N.; Yin, S.; Yang, M.; Luo, M.; Tang, J.; Yang, X. A short peptide potentially promotes the healing of skin wound. Biosci. Rep. 2019, 39, 1–20. [Google Scholar] [CrossRef]
- Goh, M.; Hwang, Y.; Tae, G. Epidermal growth factor loaded heparin-based hydrogel sheet for skin wound healing. Carbohydr. Polym. 2016, 147, 251–260. [Google Scholar] [CrossRef]
- El-Ferjani, R.M.; Ahmad, M.; Dhiyaaldeen, S.M.; Harun, F.W.; Ibrahim, M.Y.; Adam, H.; Yamin, B.M.; Al-Obaidi, M.M.J.; Al Batran, R. In vivo Assessment of Antioxidant and Wound Healing Improvement of a New Schiff Base Derived Co (II) Complex in Rats. Sci. Rep. 2016, 6, 38748. [Google Scholar] [CrossRef]
- Ain, N.J.; Diyana, A.S.; Hazirah, N.R.; Fathiah, N.A.; Fairus, A.; Teoh, S.L.; Anum, Y.M. The effect of piper betle on wound healing in male sprague dawley rats. Med. Health Kuala Lumpur 2018, 13, 165–174. [Google Scholar]
- Chin, C.-Y.; Jalil, J.; Ng, P.Y.; Ng, S.-F. Development and formulation of Moringa oleifera standardised leaf extract film dressing for wound healing application. J. Ethnopharmacol. 2018, 212, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Fan, R.; Tong, A.; Yang, M.; Deng, J.; Zhou, L.; Zhang, X.; Guo, G. In situ gel-forming AP-57 peptide delivery system for cutaneous wound healing. Int. J. Pharm. 2015, 495, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.S.; Evans, G.R.D. Advances in Wound Healing: A Review of Current Wound Healing Products. Plast. Surg. Int. 2012, 2012, 1–8. [Google Scholar] [CrossRef]
- Del Gaudio, P.; De Cicco, F.; Aquino, R.P.; Picerno, P.; Russo, P.; Piaz, F.D.; Bizzarro, V.; Belvedere, R.; Parente, L.; Petrella, A. Evaluation of in situ injectable hydrogels as controlled release device for ANXA1 derived peptide in wound healing. Carbohydr. Polym. 2015, 115, 629–635. [Google Scholar] [CrossRef]
- Braff, M.H.; Bardan, A.; Nizet, V.; Gallo, R. Cutaneous Defense Mechanisms by Antimicrobial Peptides. J. Investig. Dermatol. 2005, 125, 9–13. [Google Scholar] [CrossRef] [Green Version]
- Lee, P.H.; Rudisill, J.A.; Lin, K.H.; Zhang, L.; Harris, S.M.; Falla, T.J.; Gallo, R.L. HB-107, a nonbacteriostatic fragment of the antimicrobial peptide cecropin B, accelerates murine wound repair. Wound. Repair. Regen. 2004, 12, 351–358. [Google Scholar] [CrossRef]
- Kim, D.J.; Lee, Y.W.; Park, M.K.; Shin, J.R.; Lim, K.J.; Cho, J.H.; Kim, S.C. Efficacy of the designer antimicrobial peptide SHAP1 in wound healing and wound infection. Amino Acids 2014, 46, 2333–2343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mangoni, M.L.; McDermott, A.M.; Zasloff, M. Antimicrobial peptides and wound healing: Biological and therapeutic considerations. Exp Dermatol. 2016, 25, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Joseph, M.; Trinh, H.M.; Mitra, A.K. Peptide and protein-based therapeutic agents. In Emerging Nanotechnologies for Diagnostics, Drug Delivery and Medical Devices; Elsevier: Amsterdam, The Netherlands, 2017; pp. 145–167. [Google Scholar]
- Tang, J.; Liu, H.; Gao, C.; Mu, L.; Yang, S.; Rong, M.; Zhang, Z.; Liu, J.; Ding, Q.; Lai, R. A Small Peptide with Potential Ability to Promote Wound Healing. PLoS ONE 2014, 9, e92082. [Google Scholar] [CrossRef]
- Kim, D.J.; Chang, S.S.; Lee, J. Anti-aging potential of substance P-based hydrogel for human skin longevity. Int. J. Mol. Sci. 2019, 20, 4453. [Google Scholar] [CrossRef] [Green Version]
- Lau, J.L.; Dunn, M.K. Therapeutic peptides: Historical perspectives, current development trends, and future directions. Bioorganic Med. Chem. 2018, 26, 2700–2707. [Google Scholar] [CrossRef]
- Kanikkannan, N.; Kandimalla, K.; Lamba, S.S.; Singh, M. Structure-activity relationship of chemical penetration enhancers in transdermal drug delivery. Curr. Med. Chem. 2000, 7, 593–608. [Google Scholar] [CrossRef]
- Robinson, L.R.; Fitzgerald, N.C.; Doughty, D.G.; Dawes, N.C.; Berge, C.A.; Bissett, D.L. Topical palmitoyl pentapeptide provides improvement in photoaged human facial skin1. Int. J. Cosmet. Sci. 2005, 27, 155–160. [Google Scholar] [CrossRef]
- Li, Y.; Wang, Y.; Wei, Q.; Zheng, X.; Tang, L.; Kong, D.; Gong, M. Variant fatty acid-like molecules Conjugation, novel approaches for extending the stability of therapeutic peptides. Sci. Rep. 2015, 5, 18039. [Google Scholar] [CrossRef]
- Schagen, S.K. Topical Peptide Treatments with Effective Anti-Aging Results. Cosmetics 2017, 4, 16. [Google Scholar] [CrossRef] [Green Version]
- Lu, C.; Kim, B.M.; Lee, D.; Lee, M.H.; Kim, J.H.; Pyo, H.-B.; Chai, K.Y. Synthesis of lipoic acid–peptide conjugates and their effect on collagen and melanogenesis. Eur. J. Med. Chem. 2013, 69, 449–454. [Google Scholar] [CrossRef]
- Calder, P.C. Omega-3 Fatty Acids and Inflammatory Processes. Nutrient 2010, 2, 355–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCusker, M.M.; Grant-Kels, J.M. Healing fats of the skin: The structural and immunologic roles of the ω-6 and ω-3 fatty acids. Clin. Dermatol. 2010, 28, 440–451. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.W.; Supp, D.M. Role of Arginine and Omega-3 Fatty Acids in Wound Healing and Infection. Adv. Wound Care 2014, 3, 682–690. [Google Scholar] [CrossRef]
- Rodrigues, H.G.; Vinolo, M.A.R.; Sato, F.T.; Magdalon, J.; Kuhl, C.M.C.; Yamagata, A.S.; Pessoa, A.F.M.; Malheiros, G.; Dos Santos, M.F.; Lima, C.; et al. Oral Administration of Linoleic Acid Induces New Vessel Formation and Improves Skin Wound Healing in Diabetic Rats. PLoS ONE 2016, 11, e0165115. [Google Scholar] [CrossRef]
- Silva, J.R.; Burger, B.; Kühl, C.M.C.; Candreva, T.; Dos Anjos, M.B.P.; Rodrigues, H.G. Wound Healing and Omega-6 Fatty Acids: From Inflammation to Repair. Mediat. Inflamm. 2018, 2018, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Fadilah, N.I.M.; Ahmad, H.; Rahman, M.B.A.; Chia, S.L.; Ng, S.-F.; Leong, S.W. Synthesis and in vitro biological evaluations of novel tetrapeptide as therapeutic agent for wound treatment. J. Saudi Chem. Soc. 2020, 24, 606–619. [Google Scholar] [CrossRef]
- Parsa, P.; Paydayesh, A.; Davachi, S.M. Investigating the effect of tetracycline addition on nanocomposite hydrogels based on polyvinyl alcohol and chitosan nanoparticles for specific medical applications. Int. J. Biol. Macromol. 2019, 121, 1061–1069. [Google Scholar] [CrossRef]
- Lovětinská-Šlamborová, I.; Holý, P.; Exnar, P.; Veverková, I. Silica Nanofibers with Immobilized Tetracycline for Wound Dressing. J. Nanomater. 2016, 2016, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Halim, S.Z.; Abdullah, N.R.; Afzan, A.; Rashid, B.A.; Jantan, I.; Ismail, Z. Acute toxicity study of Carica papaya leaf extract in sprague dawley rats. J. Med. Plant. Res. 2011, 5, 1867–1872. [Google Scholar]
- Wen, X.; Zheng, Y.; Wu, J.; Yue, L.; Wang, C.; Luan, J.; Wu, Z.; Wang, K. In vitro and in vivo investigation of bacterial cellulose dressing containing uniform silver sulfadiazine nanoparticles for burn wound healing. Prog. Nat. Sci. Mater. Int. 2015, 25, 197–203. [Google Scholar] [CrossRef] [Green Version]
- Stutler, S.A.; Johnson, E.W.; Still, K.R.; Schaeffer, D.J.; A Hess, R.; Arfsten, D.P. Effect of method of euthanasia on sperm motility of mature Sprague-Dawley rats. J. Am. Assoc. Lab. Anim. Sci. 2007, 46, 13–20. [Google Scholar] [PubMed]
- Ekperikpe, U.S.; Owolabi, O.; Bolanle, I.O. Effects of Parkia biglobosa aqueous seed extract on some biochemical, haematological and histopathological parameters in streptozotocin induced diabetic rats. J. Ethnopharmacol. 2019, 228, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Nayak, B.S.; Pereira, L.M.P. Catharanthus roseus flower extract has wound-healing activity in Sprague Dawley rats. BMC Complement. Altern. Med. 2006, 6, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suvik, A.; Effendy, A.W.M. The use of modified Masson’s trichrome staining in collagen evaluation in wound healing study. Mal. J. Veter. Res. 2012, 3, 39–47. [Google Scholar]
- Gupta, A.; Kumar, P. Assessment of the histological state of the healing wound. Plast. Aesthetic Res. 2015, 2, 239. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Y.; Liang, Y.; Zhang, D.; Sun, X.; Liang, L.; Li, J.; Liu, Y.-N. Gelatin-Based Hydrogels Blended with Gellan as an Injectable Wound Dressing. ACS Omega 2018, 3, 4766–4775. [Google Scholar] [CrossRef] [Green Version]
- He, Q.; Su, G.; Liu, K.; Zhang, F.; Jiang, Y.; Gao, J.; Liu, L.; Jiang, Z.; Jin, M.; Xie, H. Sex-specific reference intervals of hematologic and biochemical analytes in Sprague-Dawley rats using the nonparametric rank percentile method. PLoS ONE 2017, 12, e0189837. [Google Scholar] [CrossRef] [Green Version]
- Azis, H.; Taher, M.; Ahmed, A.; Sulaiman, W.; Susanti, D.; Chowdhury, S.R.; Zakaria, Z. In vitro and in vivo wound healing studies of methanolic fraction of Centella asiatica extract. South Afr. J. Bot. 2017, 108, 163–174. [Google Scholar] [CrossRef]
- Svensjo, T.; Pomahac, B.; Yao, F.; Slama, J.; Eriksson, E. Accelerated healing of full-thickness skin wounds in a wet environment. Plast. Reconstr. Surg. 2000, 106, 602–612. [Google Scholar] [CrossRef]
- Kayır, S.; Demirci, Y.; Ertürk, E.; Ayaz, E.; Doğan, A.; Şahin, F. The in vivo effects of Verbascum speciosum on wound healing. South Afr. J. Bot. 2018, 119, 226–229. [Google Scholar] [CrossRef]
- Speranza, L.; Franceschelli, S.; Pesce, M.; Reale, M.; Menghini, L.; Vinciguerra, I.; De Lutiis, M.A.; Felaco, M.; Grilli, A. Antiinflammatory effects in THP-1 cells treated with verbascoside. Phytother. Res. 2010, 24, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.A.; Korber, A.; Grabbe, S.; Dissemond, P.D.J. Influence of pH on wound-healing: A new perspective for wound-therapy? Arch. Dermatol. Res. 2007, 298, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Kurabayashi, H.; Tamura, K.; Machida, I.; Kubota, K. Inhibiting Bacteria and Skin pH in Hemiplegia: EVects of wash-ing hands with acidic mineral water. Am. J. Phys. Med. Rehabil. 2002, 81, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Morsy, M.A.; Abdel-Latif, R.G.; Nair, A.; Venugopala, K.N.; Ahmed, A.F.; Elsewedy, H.S.; Shehata, T.M. Preparation and Evaluation of Atorvastatin-Loaded Nanoemulgel on Wound-Healing Efficacy. Pharmaceutics 2019, 11, 609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suzuki-Banhesse, V.F.; Azevedo, F.F.; De Araujo, E.P.; Amaral, M.E.C.D.; Caricilli, A.M.; Saad, M.J.A.; Lima, M. Effect of Atorvastatin on Wound Healing in Rats. Biol. Res. Nurs. 2014, 17, 159–168. [Google Scholar] [CrossRef]
- Aly, U.F. Preparation and evaluation of novel topical gel preparations for wound healing in diabetics. Int. J. Pharm. Sci. 2012, 4, 76–82. [Google Scholar]
- Schiefelbein, D.; Goren, I.; Fisslthaler, B.; Schmidt, H.; Geisslinger, G.; Pfeilschifter, J.; Frank, S. Biphasic Regulation of HMG-CoA Reductase Expression and Activity during Wound Healing and Its Functional Role in the Control of Keratinocyte Angiogenic and Proliferative Responses. J. Biol. Chem. 2008, 283, 15479–15490. [Google Scholar] [CrossRef] [Green Version]
- Latif, M.A.; Zaki, M.Z.M.; Leng, T.M.; Rahman, N.H.A.; Arshad, S.A.; Hamid, A. Alocasia denudata Engler treatment enhance open wound healing activities in Wistar rat’s skin. J. Ethnopharmacol. 2015, 176, 258–267. [Google Scholar] [CrossRef]
- Silva, J.P.; Dhall, S.; Garcia, M.; Chan, A.; Costa, C.; Gama, M.; Martins-Green, M. Improved burn wound healing by the antimicrobial peptide LLKKK18 released from conjugates with dextrin embedded in a carbopol gel. Acta Biomater. 2015, 26, 249–262. [Google Scholar] [CrossRef] [Green Version]
- Ram, M.; Singh, V.; Kumawat, S.; Kant, V.; Tandan, S.K.; Kumar, D. Bilirubin modulated cytokines, growth factors and angiogenesis to improve cutaneous wound healing process in diabetic rats. Int. Immunopharmacol. 2016, 30, 137–149. [Google Scholar] [CrossRef]
- Bhan, S.; Mitra, R.; Arya, A.K.; Pandey, H.P.; Tripathi, K. A Study on Evaluation of Apoptosis and Expression of Bcl-2-Related Marker in Wound Healing of Streptozotocin-Induced Diabetic Rats. ISRN Dermatol. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardwicke, J.T.; Hart, J.; Bell, A.; Duncan, R.; Thomas, D.W.; Moseley, R. The effect of dextrin–rhEGF on the healing of full-thickness, excisional wounds in the (db/db) diabetic mouse. J. Control. Release 2011, 152, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Rousselle, P.; Braye, F.; Dayan, G. Re-epithelialization of adult skin wounds: Cellular mechanisms and therapeutic strategies. Adv. Drug Deliv. Rev. 2019, 146, 344–365. [Google Scholar] [CrossRef] [PubMed]
- Ben Djemaa, F.G.; Bellassoued, K.; Zouari, S.; El Feki, A.; Ammar, E. Antioxidant and wound healing activity of Lavandula aspic L. ointment. J. Tissue Viability 2016, 25, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Wirth, M.D.; Sevoyan, M.; Hofseth, L.; Shivappa, N.; Hurley, T.; Hébert, J.R. The Dietary Inflammatory Index is associated with elevated white blood cell counts in the National Health and Nutrition Examination Survey. Brain Behav. Immun. 2018, 69, 296–303. [Google Scholar] [CrossRef]
- Szewczuk, M.; Czerniawska-Piątkowska, E.; Palewski, S. The effect of colostral supplement on the serum protein fractions, health status and growth of calves. Arch. Anim. Breed. 2011, 54, 115–126. [Google Scholar] [CrossRef]
- Kong, D.Y.; Park, J.H.; Lee, K.W.; Park, H.; Cho, J.A. Comparative Analysis of 3 Experimental Mouse Model for Blood Hematology and Chemistry. Biomed. Sci. Lett. 2016, 22, 75–82. [Google Scholar] [CrossRef] [Green Version]
- Kuo, T.; McQueen, A.; Chen, T.C.; Wang, J.C. Regulation of glucose homeostasis by glucocorticoids. In Glucocorticoid Signaling; Springer: New York, NY, USA, 2015; pp. 99–126. [Google Scholar]
- Kim, I.S.; Kim, H.T.; Kim, E.J.; Lee, E.J. A comparative study of the concentration of salivary and blood glucose in normal and diabetic subjects. J. Exp. Biomed. Sci. 2013, 19, 105–111. [Google Scholar]
- Horner, S.; Robinson, S.; Lees, D.; Callander, R.; Roberts, R. Target organ profiles in toxicity studies supporting human dosing: An assessment of recovery and chronic dosing. Regul. Toxicol. Pharmacol. 2014, 70, 270–285. [Google Scholar] [CrossRef]
- Roberts, R.A.; Callander, R.; Duffy, P.; Jacobsen, M.; Knight, R.; Boobis, A. Target organ profiles in toxicity studies supporting human dosing: Does severity progress with longer duration of exposure? Regul. Toxicol. Pharmacol. 2015, 73, 737–746. [Google Scholar] [CrossRef]
- Ekam, V.S.; E Ebong, P. Serum protein and enzyme levels in rats following administration of antioxidant vitamins during caffeinated and non-caffeinated paracetamol induced hepatotoxicity. Niger. J. Physiol. Sci. 2008, 22, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramaiah, S.K. A toxicologist guide to the diagnostic interpretation of hepatic biochemical parameters. Food Chem. Toxicol. 2007, 45, 1551–1557. [Google Scholar] [CrossRef] [PubMed]
- Agnelli, S.; Arriarán, S.; Oliva, L.; Remesar, X.; Fernández-López, J.A.; Alemany, M. Modulation of rat liver urea cycle and related ammonium metabolism by sex and cafeteria diet. RSC Adv. 2016, 6, 11278–11288. [Google Scholar] [CrossRef] [Green Version]




| Microscopic Parameter | Score | ||
|---|---|---|---|
| 0 | 1 | 2 | |
| Epidermal integration | Destroyed | Partial | Normal |
| Epidermal-dermal junction | Destroyed | Partial | Normal |
| Fibroblast and collagen presence | Plenty | Moderate | A few |
| Apoptotic keratinocytes | High | Moderate | Normal |
| Composition | Percentage Secondary Structure Types (%) | ||
|---|---|---|---|
| pH 4 | pH 7 | pH 10 | |
| α-helix | 34.40 | 17.70 | 0.00 |
| β-sheet | 2.60 | 23.20 | 34.50 |
| Turn | 30.00 | 20.80 | 21.10 |
| Random | 43.70 | 38.30 | 44.40 |
| Group | Rats Taken | Day/Body Weight (kg) | ||||||
|---|---|---|---|---|---|---|---|---|
| 0th | 3rd | 6th | 9th | 12th | 15th | 18th | ||
| Control (Group 1) | 0.28 ± 0.02 | 0.33 ± 0.03 | 0.34 ± 0.02 | 0.34 ± 0.02 | 0.34 ± 0.02 | 0.34 ± 0.02 | 0.34 ± 0.02 | 0.35 ± 0.02 |
| Palmitoyl-GDPH (Group 2) | 0.28 ± 0.02 | 0.35 ± 0.04 | 0.35 ± 0.04 | 0.36 ± 0.04 | 0.36 ± 0.04 | 0.36 ± 0.03 | 0.36 ± 0.03 | 0.37 ± 0.03 |
| Tetracycline (Group 3) | 0.28 ± 0.03 | 0.33 ± 0.01 | 0.33 ± 0.01 | 0.33 ± 0.01 | 0.33 ± 0.01 | 0.33 ± 0.01 | 0.33 ± 0.01 | 0.33 ± 0.01 |
| Parameters (Unit) | Group 0 | Group 1 | Group 2 | Group 3 |
|---|---|---|---|---|
| Normal | Control | Palmitoyl-GDPH | Tetracycline | |
| Red blood cells (×1012/L) | 7.43 ± 0.75 | 8.51 ± 0.31 | 7.39 ± 0.20 | 8.18 ± 1.56 |
| Haemoglobin (g/L) | 150 ± 10.39 | 154 ± 1.00 | 157 ± 0.71 | 153 ± 11.31 |
| Mean red blood cell volume (fL) | 52 ± 1.00 | 52 ± 2.52 | 54 ± 1.53 | 49 ± 0.58 |
| Mean corpuscular Hb conc. (g/L) | 373 ± 5.66 | 371 ± 2.00 | 383 ± 4.93 | 387 ± 2.52 |
| White blood cells (×109/L) | 5.0 ± 3.22 | 9.8 ± 0.26 | 10.3 ± 1.73* | 10.2 ± 0.99 |
| Neutrophils (×109/L) | 0.99 ± 0.90 | 2.41 ± 0.61 | 2.33 ± 0.36 | 3.93 ± 2.16 |
| Lymphocytes (×109/L) | 3.65 ± 2.08 | 6.21 ± 0.55 | 6.26 ± 0.60 | 7.86 ± 2.06 |
| Monocytes (×109/L) | 0.23 ± 0.17 | 0.51 ± 0.06 | 0.72 ± 0.12 | 0.5 ± 0.33 |
| Eosinophils (×109/L) | 0.08 ± 0,08 | 0.14 ± 0.06 | 0.24 ± 0.05 | 0.91 ± 0.95 |
| Platelets (×109/L) | 1354 ± 66.34 | 1295 ± 0.00 | 1162 ± 1.09 | 1201 ± 0.78 |
| Parameters (Unit) | Group 0 | Group 1 | Group 2 | Group 3 |
|---|---|---|---|---|
| Normal | Control | Palmitoyl-GDPH | Tetracycline | |
| Total protein (g/L) | 67.2 ± 2.78 | 61.9 ± 0.49 | 65.9 ± 0.71 | 76.5 ± 3.89 |
| Albumin(g/L) | 33.2 ± 1.77 | 31.8 ± 2.97 | 32.8 ± 2.55 | 38.3 ± 2.86 |
| Globulin (g/L) | 34.1 ± 1.03 | 36.1 ± 3.90 | 33.5 ± 1.35 | 38.8 ± 2.52 |
| Phosphate (mmol/L) | 2.5 ± 0.06 | 2.7 ± 0.23 | 2.4 ± 0.06 | 2.9 ± 0.20 |
| Calcium (mmol/L) | 2.6 ± 0.06 | 2.6 ± 0.15 | 2.6 ± 0.06 | 3.4 ± 0.21 |
| Glucose (mmol/L) | 8.1 ± 0.62 | 12.6 ± 0.36 | 11.5 ± 0.98 | 12.5 ± 2.84 |
| Cholestrol (mmol/L) | 2.4 ± 0.17 | 1.8 ± 0.06 | 1.6± 0.06 | 1.8 ± 0.2 |
| Parameters (Unit) | Group 0 | Group 1 | Group 2 | Group 3 |
|---|---|---|---|---|
| Normal | Control | Palmitoyl-GDPH | Tetracycline | |
| Total bilirubin (µmol/L) | 0.7 ± 0.35 | 3.9 ± 0.15 | 4.2 ± 0.82 | 4.2 ± 0.32 |
| ALT (U/L) | 34 ± 3.21 | 73 ± 7.07 | 61 ± 2.65 | 63 ± 6.43 |
| ALP (U/L) | 173 ± 9.54 | 193 ± 5.03 | 222 ± 2.12 | 317 ± 3.54 |
| Amylase (U/L) | 2134 ± 0.71 | 2360 ± 7.68 | 2553 ± 5.77 | 2475 ± 5.90 |
| Urea (mmol/L) | 4.5 ± 0.35 | 10.6 ± 1.04 * | 8.7 ± 0.47 * | 9.5 ± 0.26 * |
| Creatinine (µmol/L) | 38 ± 1.53 | 42 ± 1.73 | 42 ± 1.53 | 50 ± 5.69 |
| Lipase (U/L) | 35 ± 3.61 | 37 ± 3.51 | 37 ± 2.00 | 36 ± 6.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadilah, N.I.M.; Rahman, M.B.A.; Yusof, L.M.; Mustapha, N.M.; Ahmad, H. The Therapeutic Effect and In Vivo Assessment of Palmitoyl- GDPH on the Wound Healing Process. Pharmaceutics 2021, 13, 193. https://doi.org/10.3390/pharmaceutics13020193
Fadilah NIM, Rahman MBA, Yusof LM, Mustapha NM, Ahmad H. The Therapeutic Effect and In Vivo Assessment of Palmitoyl- GDPH on the Wound Healing Process. Pharmaceutics. 2021; 13(2):193. https://doi.org/10.3390/pharmaceutics13020193
Chicago/Turabian StyleFadilah, Nur Izzah Md, Mohd Basyaruddin Abdul Rahman, Loqman Mohamad Yusof, Noordin Mohamed Mustapha, and Haslina Ahmad. 2021. "The Therapeutic Effect and In Vivo Assessment of Palmitoyl- GDPH on the Wound Healing Process" Pharmaceutics 13, no. 2: 193. https://doi.org/10.3390/pharmaceutics13020193






