Challenges and Complications of Poly(lactic-co-glycolic acid)-Based Long-Acting Drug Product Development
Abstract
:1. Introduction
2. Complexity in Developing Generic PLGA-Based LAI Drug Products
3. Lack of a Standard Compendial Method for In Vitro Release Studies
4. Constraints Related to the Physicochemical Properties of PLGA
5. Complex Drug Release Mechanism
6. Differences in the Manufacturing Process
7. Strategies to Improve Encapsulation Efficiency and Drug Release
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Makadia, H.K.; Siegel, S.J. Poly Lactic-co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Qu, W.; Choi, S.H. FDA’s Regulatory Science Program for Generic PLA/PLGA-Based Drug Products|American Pharmaceutical Review—The Review of American Pharmaceutical Business & Technology. Available online: https://www.americanpharmaceuticalreview.com/Featured-Articles/188841-FDA-s-Regulatory-Science-Program-for-Generic-PLA-PLGA-Based-Drug-Products/ (accessed on 22 October 2020).
- Burgess, D.J.; Hussain, A.S.; Ingallinera, T.S.; Chen, M.-L. Assuring Quality and Performance of Sustained and Controlled Release Parenterals: Workshop Report. AAPS PharmSci 2002, 4, 13–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez, M.N.; Rathbone, M.J.; Burgess, D.; Huynh, M. Breakout Session Summary from AAPS/CRS Joint Workshop on Critical Variables in the In Vitro and In Vivo Performance of Parenteral Sustained Release Products. J. Control Release 2009, 142, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Otte, A.; Sharifi, F.; Park, K. Interfacial Tension Effects on the Properties of PLGA Microparticles. Colloids Surf. B Biointerfaces 2020, 196, 111300. [Google Scholar] [CrossRef]
- O’Brien, M.N.; Jiang, W.; Wang, Y.; Loffredo, D.M. Challenges and Opportunities in the Development of Complex Generic Long-Acting Injectable Drug Products. J. Control Release 2021, 336, 144–158. [Google Scholar] [CrossRef]
- Zhou, J.; Hirota, K.; Ackermann, R.; Walker, J.; Wang, Y.; Choi, S.; Schwendeman, A.; Schwendeman, S.P. Reverse Engineering the 1-Month Lupron Depot®. AAPS J. 2018, 20, 105. [Google Scholar] [CrossRef]
- Beig, A.; Feng, L.; Walker, J.; Ackermann, R.; Hong, J.K.Y.; Li, T.; Wang, Y.; Qin, B.; Schwendeman, S.P. Physical-Chemical Characterization of Octreotide Encapsulated in Commercial Glucose-Star PLGA Microspheres. Mol. Pharm. 2020, 17, 4141–4151. [Google Scholar] [CrossRef]
- Schoubben, A.; Ricci, M.; Giovagnoli, S. Meeting the Unmet: From Traditional to Cutting-Edge Techniques for Poly Lactide and Poly Lactide-co-Glycolide Microparticle Manufacturing. J. Pharm. Investig. 2019, 49, 381–404. [Google Scholar] [CrossRef] [Green Version]
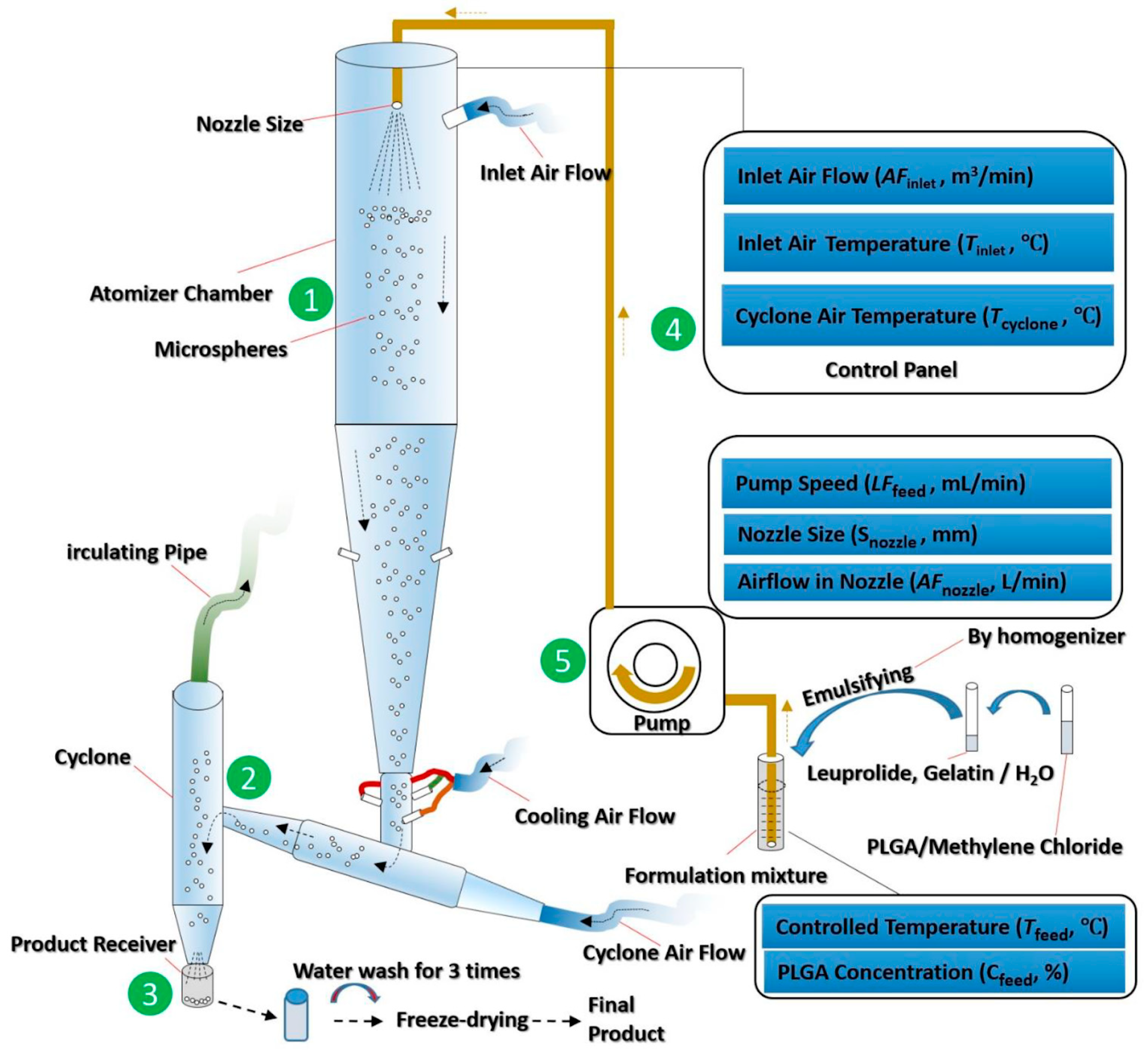
- Zhang, C.; Yang, L.; Wan, F.; Bera, H.; Cun, D.; Rantanen, J.; Yang, M. Quality by Design Thinking in the Development of Long-Acting Injectable PLGA/PLA-Based Microspheres for Peptide and Protein Drug Delivery. Int. J. Pharm. 2020, 585, 119441. [Google Scholar] [CrossRef]
- Simões, M.F.; Pinto, R.M.A.; Simões, S. Hot-Melt Extrusion in the Pharmaceutical Industry: Toward Filing a New Drug Application. Drug Discov. Today 2019, 24, 1749–1768. [Google Scholar] [CrossRef]
- Park, K.; Skidmore, S.; Hadar, J.; Garner, J.; Park, H.; Otte, A.; Soh, B.K.; Yoon, G.; Yu, D.; Yun, Y.; et al. Injectable, Long-Acting PLGA Formulations: Analyzing PLGA and Understanding Microparticle Formation. J. Control Release 2019, 304, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Wan, F.; Yang, M. Design of PLGA-Based Depot Delivery Systems for Biopharmaceuticals Prepared by Spray Drying. Int. J. Pharm. 2016, 498, 82–95. [Google Scholar] [CrossRef] [PubMed]
- Intersect ENT Sinuva (Mometasone Furoate) Sinus Implant. Highlights of Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209310lbl.pdf (accessed on 6 June 2021).
- Tolmar Pharmaceuticals Fensolvi (Leuprolide Acetate) for Injectable Suspension. Highlights of Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213150s000lbl.pdf (accessed on 7 June 2021).
- Garner, J.; Skidmore, S.; Park, H.; Park, K.; Choi, S.; Wang, Y. Beyond Q1/Q2: The Impact of Manufacturing Conditions and Test Methods on Drug Release From PLGA-Based Microparticle Depot Formulations. J. Pharm. Sci. 2018, 107, 353–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Medicines Agency Questions and Answers on the Review of Novosis Goserelin, Goserelin Cell Pharm, Novimp and Associated Names (Goserelin, 3.6 Mg Implant). Available online: https://www.ema.europa.eu/en/documents/referral/questions-answers-review-novosis-goserelin-goserelin-cell-pharm-novimp-associated-names-goserelin-36_en.pdf (accessed on 4 May 2021).
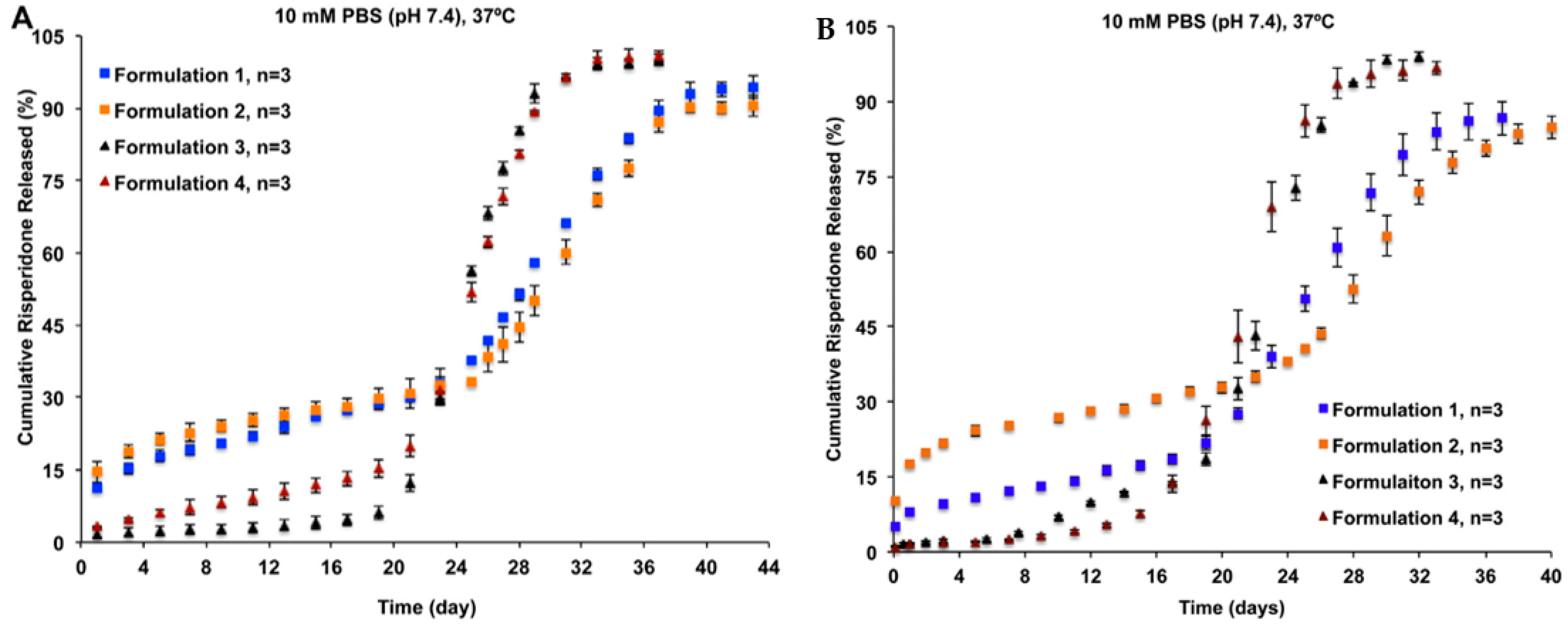
- Shen, J.; Choi, S.; Qu, W.; Wang, Y.; Burgess, D.J. In Vitro-In Vivo Correlation of Parenteral Risperidone Polymeric Microspheres. J. Control Release 2015, 218, 2–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
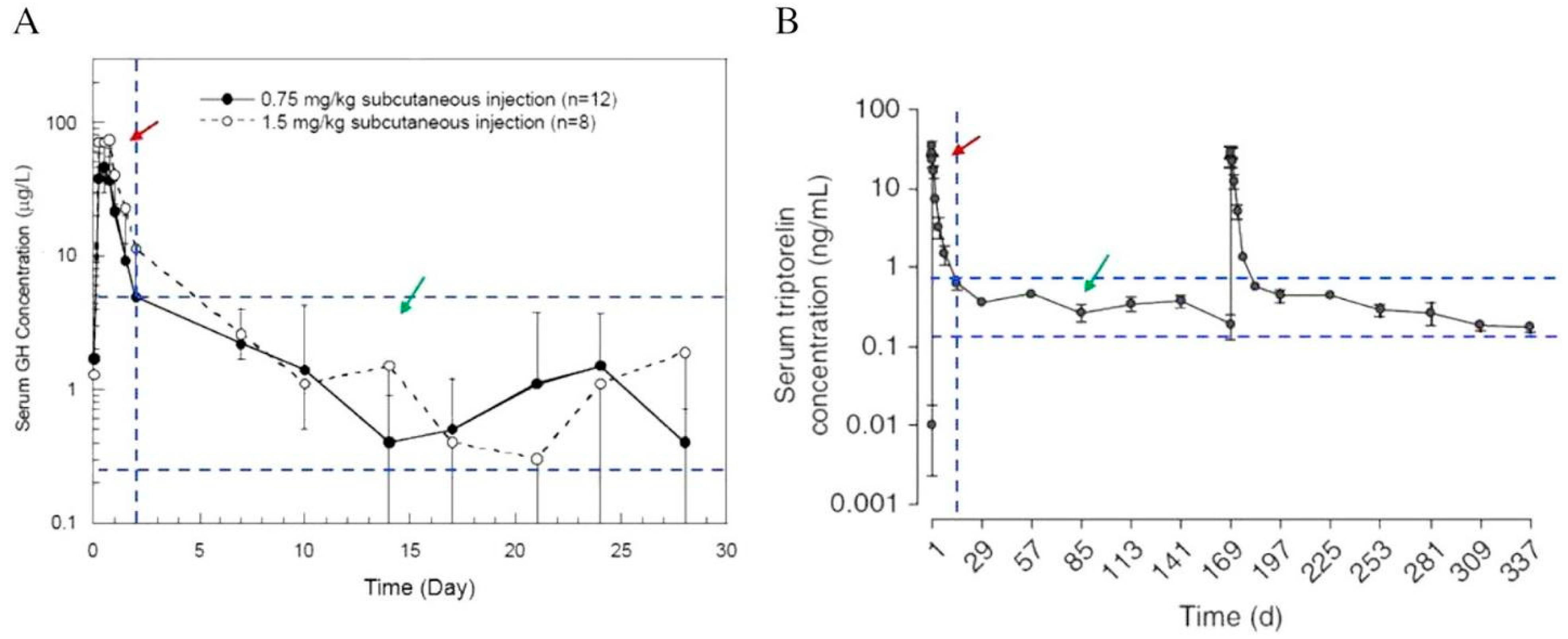
- Høybye, C.; Cohen, P.; Hoffman, A.R.; Ross, R.; Biller, B.M.K.; Christiansen, J.S. Status of Long-Acting-Growth Hormone Preparations—2015. Growth Horm. IGF Res. 2015, 25, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Andhariya, J.V.; Shen, J.; Choi, S.; Wang, Y.; Zou, Y.; Burgess, D.J. Development of In Vitro-In Vivo Correlation of Parenteral Naltrexone Loaded Polymeric Microspheres. J. Control Release 2017, 255, 27–35. [Google Scholar] [CrossRef]
- Gottlieb, S. Statement from FDA Commissioner Scott Gottlieb, M.D., on New Agency Actions to Further Deter ‘Gaming’ of the Generic Drug Approval Process by the Use of Citizen Petitions. Available online: https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-new-agency-actions-further-deter-gaming-generic-drug (accessed on 10 August 2021).
- Wang, Y.; Qin, B.; Xia, G.; Choi, S.H. FDA’s Poly (Lactic-co-Glycolic Acid) Research Program and Regulatory Outcomes. AAPS J. 2021, 23, 92. [Google Scholar] [CrossRef]
- United States Food and Drug Administration FY2018 Regulatory Science Report: Long Acting Injectables and Implants. Available online: https://www.fda.gov/media/129010/download (accessed on 6 July 2021).
- Soares, S.; Sousa, J.; Pais, A.; Vitorino, C. Nanomedicine: Principles, Properties, and Regulatory Issues. Front. Chem. 2018, 6, 360. [Google Scholar] [CrossRef]
- Leblanc, D. PLGA Microspheres: The Art of the Science. Available online: https://www.pharmamanufacturing.com/articles/2018/the-art-of-the-science/ (accessed on 10 August 2021).
- Dadhaniya, T.M.; Sharma, O.P.; Gohel, M.C.; Mehta, P.J. Current Approaches for In Vitro Drug Release Study of Long Acting Parenteral Formulations. Curr. Drug Deliv. 2015, 12, 256–270. [Google Scholar] [CrossRef]
- Busatto, C.; Pesoa, J.; Helbling, I.; Luna, J.; Estenoz, D. Effect of Particle Size, Polydispersity and Polymer Degradation on Progesterone Release from PLGA Microparticles: Experimental and Mathematical Modeling. Int. J. Pharm. 2018, 536, 360–369. [Google Scholar] [CrossRef]
- Shen, J.; Lee, K.; Choi, S.; Qu, W.; Wang, Y.; Burgess, D.J. A Reproducible Accelerated In Vitro Release Testing Method for PLGA Microspheres. Int. J. Pharm. 2016, 498, 274–282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andhariya, J.V.; Choi, S.; Wang, Y.; Zou, Y.; Burgess, D.J.; Shen, J. Accelerated In Vitro Release Testing Method for Naltrexone Loaded PLGA Microspheres. Int. J. Pharm. 2017, 520, 79–85. [Google Scholar] [CrossRef] [PubMed]
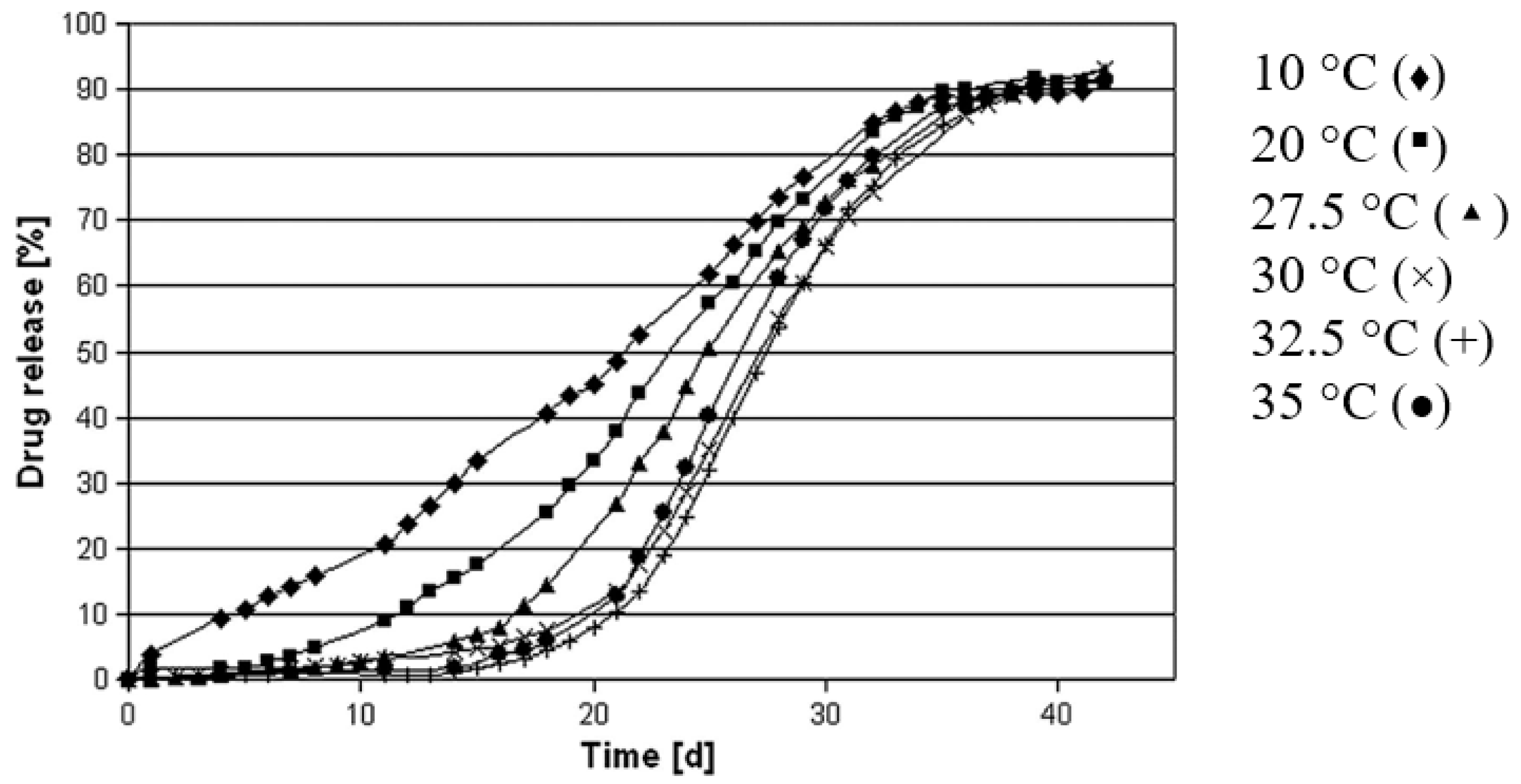
- Zolnik, B.S.; Leary, P.E.; Burgess, D.J. Elevated Temperature Accelerated Release Testing of PLGA Microspheres. J. Control Release 2006, 112, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Burgess, D.J. Accelerated In Vitro Release Testing of Implantable PLGA Microsphere/PVA Hydrogel Composite Coatings. Int. J. Pharm. 2012, 422, 341–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
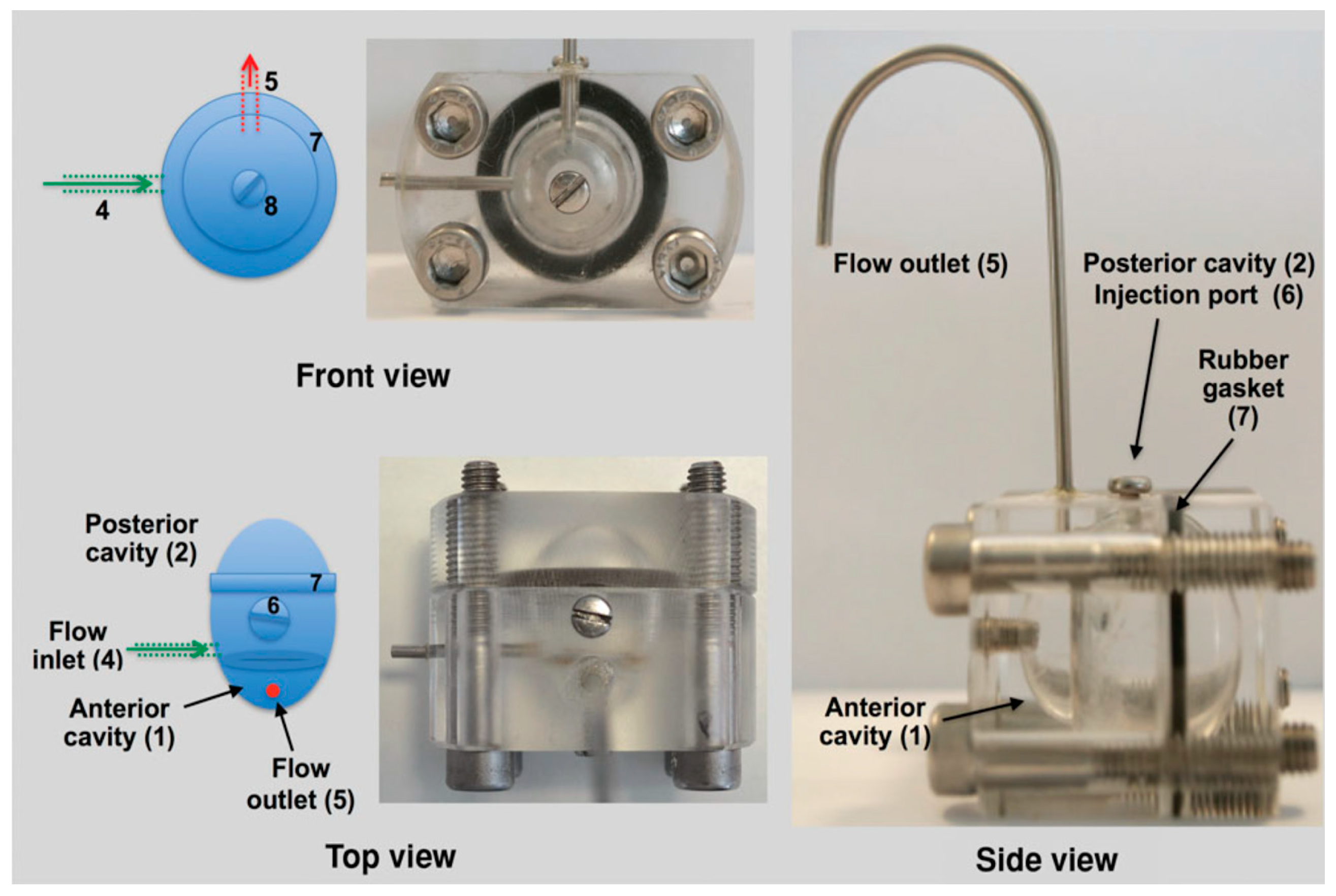
- Tipnis, N.P.; Shen, J.; Jackson, D.; Leblanc, D.; Burgess, D.J. Flow-through Cell-Based In Vitro Release Method for Triamcinolone Acetonide Poly (Lactic-co-Glycolic) Acid Microspheres. Int. J. Pharm. 2020, 579, 119130. [Google Scholar] [CrossRef] [PubMed]
- Center for Drug Evaluation and Research Extended Release Oral Dosage Forms: Development, Evaluation, and Application of In Vitro/In Vivo Correlations. FDA. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/extended-release-oral-dosage-forms-development-evaluation-and-application-vitroin-vivo-correlations (accessed on 10 August 2021).
- Andhariya, J.V.; Jog, R.; Shen, J.; Choi, S.; Wang, Y.; Zou, Y.; Burgess, D.J. Development of Level A In Vitro-In Vivo Correlations for Peptide Loaded PLGA Microspheres. J. Control Release 2019, 308, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Andhariya, J.V.; Jog, R.; Shen, J.; Choi, S.; Wang, Y.; Zou, Y.; Burgess, D.J. In Vitro-In Vivo Correlation of Parenteral PLGA Microspheres: Effect of Variable Burst Release. J. Control Release 2019, 314, 25–37. [Google Scholar] [CrossRef]
- Doty, A.C.; Weinstein, D.G.; Hirota, K.; Olsen, K.F.; Ackermann, R.; Wang, Y.; Choi, S.; Schwendeman, S.P. Mechanisms of in Vivo Release of Triamcinolone Acetonide from PLGA Microspheres. J. Control Release 2017, 256, 19–25. [Google Scholar] [CrossRef]
- Parent, M.; Nouvel, C.; Koerber, M.; Sapin, A.; Maincent, P.; Boudier, A. PLGA in Situ Implants Formed by Phase Inversion: Critical Physicochemical Parameters to Modulate Drug Release. J. Control Release 2013, 172, 292–304. [Google Scholar] [CrossRef]
- Mohammad, A.K.; Reineke, J.J. Quantitative Detection of PLGA Nanoparticle Degradation in Tissues following Intravenous Administration. Mol. Pharm. 2013, 10, 2183–2189. [Google Scholar] [CrossRef]
- Park, T.G. Degradation of Poly(Lactic-co-Glycolic Acid) Microspheres: Effect of Copolymer Composition. Biomaterials 1995, 16, 1123–1130. [Google Scholar] [CrossRef]
- Lin, X.; Yang, H.; Su, L.; Yang, Z.; Tang, X. Effect of Size on the In Vitro/In Vivo Drug Release and Degradation of Exenatide-Loaded PLGA Microspheres. J. Drug Deliv. Sci. Technol. 2018, 45, 346–356. [Google Scholar] [CrossRef]
- Dunne, M.; Corrigan, O.I.; Ramtoola, Z. Influence of Particle Size and Dissolution Conditions on the Degradation Properties of Polylactide-co-Glycolide Particles. Biomaterials 2000, 21, 1659–1668. [Google Scholar] [CrossRef]
- Vay, K.; Frieß, W.; Scheler, S. A Detailed View of Microparticle Formation by In-Process Monitoring of the Glass Transition Temperature. Eur. J. Pharm. Biopharm. 2012, 81, 399–408. [Google Scholar] [CrossRef] [PubMed]
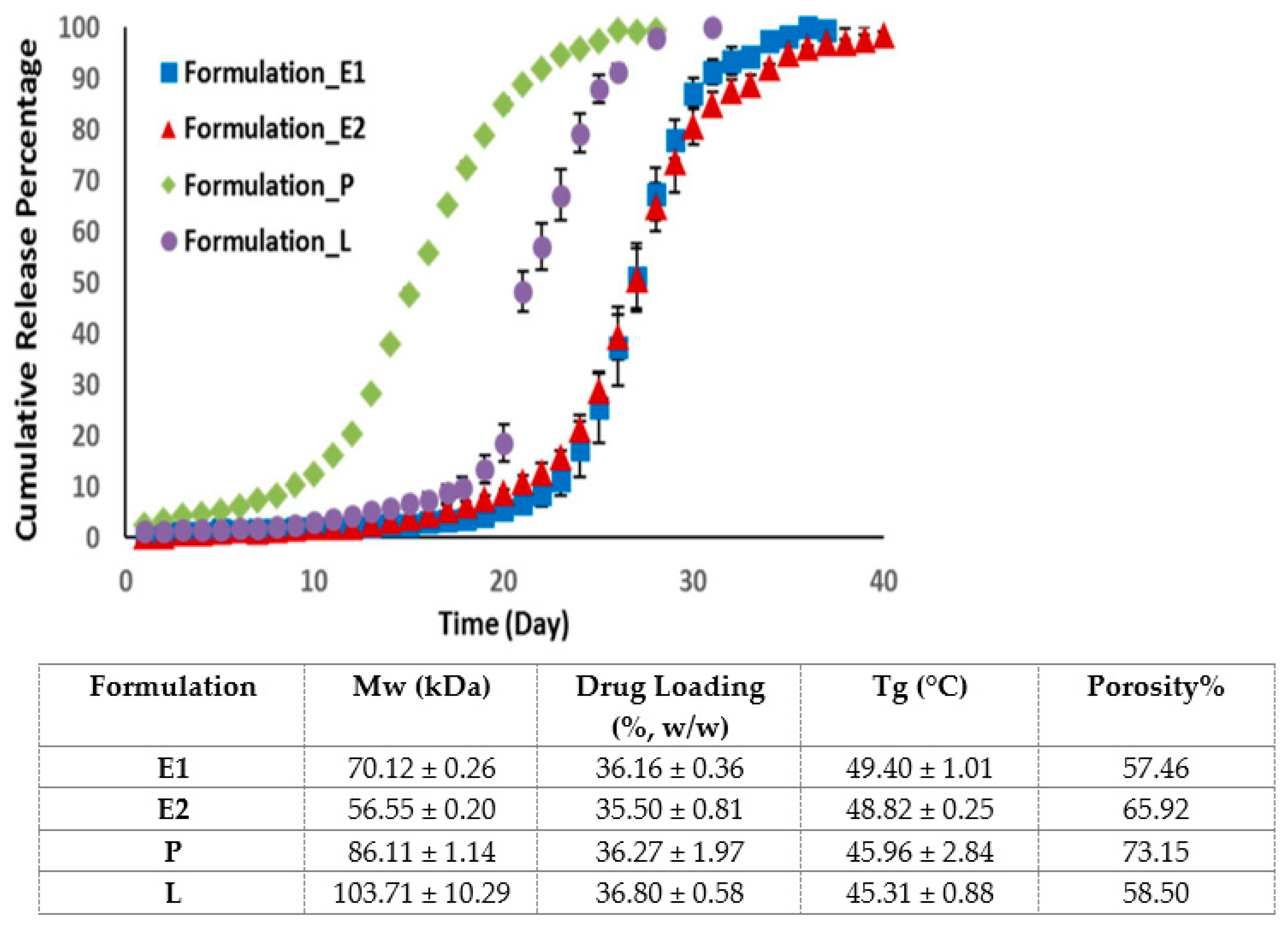
- Kohno, M.; Andhariya, J.V.; Wan, B.; Bao, Q.; Rothstein, S.; Hezel, M.; Wang, Y.; Burgess, D.J. The Effect of PLGA Molecular Weight Differences on Risperidone Release from Microspheres. Int. J. Pharm. 2020, 582, 119339. [Google Scholar] [CrossRef] [PubMed]
- Hadar, J.; Skidmore, S.; Garner, J.; Park, H.; Park, K.; Wang, Y.; Qin, B.; Jiang, X. Characterization of Branched Poly(Lactide-co-Glycolide) Polymers Used in Injectable, Long-Acting Formulations. J. Control Release 2019, 304, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Tracy, M.A.; Ward, K.L.; Firouzabadian, L.; Wang, Y.; Dong, N.; Qian, R.; Zhang, Y. Factors Affecting the Degradation Rate of Poly(Lactide-co-Glycolide) Microspheres In Vivo and In Vitro. Biomaterials 1999, 20, 1057–1062. [Google Scholar] [CrossRef]
- Patel, R.B.; Carlson, A.N.; Solorio, L.; Exner, A.A. Characterization of Formulation Parameters Affecting Low Molecular Weight Drug Release from in Situ Forming Drug Delivery Systems. J. Biomed. Mater. Res. Part A 2010, 94, 476–484. [Google Scholar] [CrossRef] [Green Version]
- Dawes, G.J.S.; Fratila-Apachitei, L.E.; Mulia, K.; Apachitei, I.; Witkamp, G.J.; Duszczyk, J. Size Effect of PLGA Spheres on Drug Loading Efficiency and Release Profiles. J. Mater. Sci. Mater. Med. 2009, 20, 1089–1094. [Google Scholar] [CrossRef] [Green Version]
- Siepmann, J.; Faisant, N.; Akiki, J.; Richard, J.; Benoit, J.P. Effect of the Size of Biodegradable Microparticles on Drug Release: Experiment and Theory. J. Control Release 2004, 96, 123–134. [Google Scholar] [CrossRef]
- Wang, T.; Xue, P.; Wang, A.; Yin, M.; Han, J.; Tang, S.; Liang, R. Pore Change during Degradation of Octreotide Acetate-Loaded PLGA Microspheres: The Effect of Polymer Blends. Eur. J. Pharm. Sci. 2019, 138, 104990. [Google Scholar] [CrossRef] [PubMed]
- Doty, A.C.; Zhang, Y.; Weinstein, D.G.; Wang, Y.; Choi, S.; Qu, W.; Mittal, S.; Schwendeman, S.P. Mechanistic Analysis of Triamcinolone Acetonide Release from PLGA Microspheres as a Function of Varying In Vitro Release Conditions. Eur. J. Pharm. Biopharm. 2017, 113, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Zolnik, B.S.; Burgess, D.J. Effect of Acidic PH on PLGA Microsphere Degradation and Release. J. Control Release 2007, 122, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Houchin, M.L.; Neuenswander, S.A.; Topp, E.M. Effect of Excipients on PLGA Film Degradation and the Stability of an Incorporated Peptide. J. Control Release 2007, 117, 413–420. [Google Scholar] [CrossRef] [Green Version]
- Ghalanbor, Z.; Körber, M.; Bodmeier, R. Interdependency of Protein-Release Completeness and Polymer Degradation in PLGA-Based Implants. Eur. J. Pharm. Biopharm. 2013, 85, 624–630. [Google Scholar] [CrossRef]
- Ford Versypt, A.N.; Pack, D.W.; Braatz, R.D. Mathematical Modeling of Drug Delivery from Autocatalytically Degradable PLGA Microspheres—A Review. J. Control Release 2013, 165, 29–37. [Google Scholar] [CrossRef]
- Huang, C.L.; Steele, T.W.; Widjaja, E.; Boey, F.Y.; Venkatraman, S.S.; Loo, J.S. The Influence of Additives in Modulating Drug Delivery and Degradation of PLGA Thin Films. NPG Asia Mater. 2013, 5, e54. [Google Scholar] [CrossRef] [Green Version]
- Gu, B.; Sun, X.; Papadimitrakopoulos, F.; Burgess, D.J. Seeing Is Believing, PLGA Microsphere Degradation Revealed in PLGA Microsphere/PVA Hydrogel Composites. J. Control Release 2016, 228, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Xiong, Y.; Yu, Z.; Lang, Y.; Hu, J.; Li, H.; Yan, Y.; Tu, C.; Yang, T.; Song, Y.; Duan, H.; et al. In Vitro Stress Effect on Degradation and Drug Release Behaviors of Basic Fibroblast Growth Factor-Poly(Lactic-co-Glycolic-Acid) Microsphere. Drug Des. Dev. Ther. 2016, 10, 431–440. [Google Scholar] [CrossRef] [Green Version]
- Gasmi, H.; Siepmann, F.; Hamoudi, M.C.; Danede, F.; Verin, J.; Willart, J.F.; Siepmann, J. Towards a Better Understanding of the Different Release Phases from PLGA Microparticles: Dexamethasone-Loaded Systems. Int. J. Pharm. 2016, 514, 189–199. [Google Scholar] [CrossRef]
- Wan, F.; Maltesen, M.J.; Andersen, S.K.; Bjerregaard, S.; Baldursdottir, S.G.; Foged, C.; Rantanen, J.; Yang, M. Modulating Protein Release Profiles by Incorporating Hyaluronic Acid into PLGA Microparticles via a Spray Dryer Equipped with a 3-Fluid Nozzle. Pharm. Res. 2014, 31, 2940–2951. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.H.; Lee, B.K.; Park, K. Controlled Drug Delivery: Historical Perspective for the next Generation. J. Control Release 2015, 219, 2–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
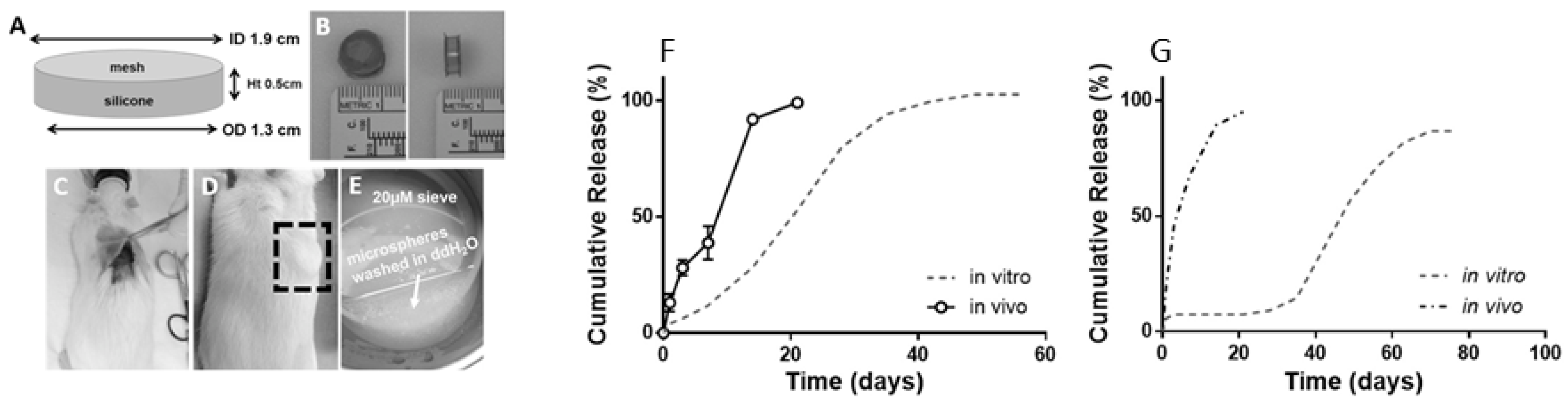
- Doty, A.C.; Hirota, K.; Olsen, K.F.; Sakamoto, N.; Ackermann, R.; Feng, M.R.; Wang, Y.; Choi, S.; Qu, W.; Schwendeman, A.; et al. Validation of a Cage Implant System for Assessing In Vivo Performance of Long-Acting Release Microspheres. Biomaterials 2016, 109, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Ansorena, E.; Silva, J.M.; Coco, R.; Le Breton, A.; Préat, V. PLGA-Based Nanoparticles: An Overview of Biomedical Applications. J. Control Release 2012, 161, 505–522. [Google Scholar] [CrossRef] [PubMed]
- Fredenberg, S.; Wahlgren, M.; Reslow, M.; Axelsson, A. The Mechanisms of Drug Release in Poly(Lactic-co-Glycolic Acid)-Based Drug Delivery Systems—A Review. Int. J. Pharm. 2011, 415, 34–52. [Google Scholar] [CrossRef]
- Awwad, S.; Day, R.M.; Khaw, P.T.; Brocchini, S.; Fadda, H.M. Sustained Release Ophthalmic Dexamethasone: In Vitro In Vivo Correlations Derived from the PK-Eye. Int. J. Pharm. 2017, 522, 119–127. [Google Scholar] [CrossRef] [Green Version]
- Herrero-Vanrell, R.; Molina-Martinez, I.T. PLA and PLGA Microparticles for Intravitreal Drug Delivery: An Overview. J. Drug Deliv. Sci. Technol. 2007, 17, 11–17. [Google Scholar] [CrossRef]
- Li, J.; Zheng, H.; Qin, L.; Xu, E.Y.; Yang, L.; Zhang, L.; Zhang, X.; Fan, L.; Beck-Broichsitter, M.; Muenster, U.; et al. In Vitro–In Vivo Correlation of Inhalable Budesonide-Loaded Large Porous Particles for Sustained Treatment Regimen of Asthma. Acta Biomater. 2019, 96, 505–516. [Google Scholar] [CrossRef]
- Awwad, S.; Lockwood, A.; Brocchini, S.; Khaw, P.T. The PK-Eye: A Novel In Vitro Ocular Flow Model for Use in Preclinical Drug Development. J. Pharm. Sci. 2015, 104, 3330–3342. [Google Scholar] [CrossRef] [Green Version]
- Katare, Y.K.; Panda, A.K. Influences of Excipients on In Vitro Release and In Vivo Performance of Tetanus Toxoid Loaded Polymer Particles. Eur. J. Pharm. Sci. 2006, 28, 179–188. [Google Scholar] [CrossRef]
- Chen, L.-Q.; Ahmed, A.M.Q.; Deng, Y.; Cao, D.; Du, H.-H.; Cui, J.-H.; Lee, B.-J.; Cao, Q.-R. Novel Triptorelin Acetate-Loaded Microspheres Prepared by a Liquid/Oil/Oil Method with High Encapsulation Efficiency and Low Initial Burst Release. J. Drug Deliv. Sci. Technol. 2019, 54, 101390. [Google Scholar] [CrossRef]
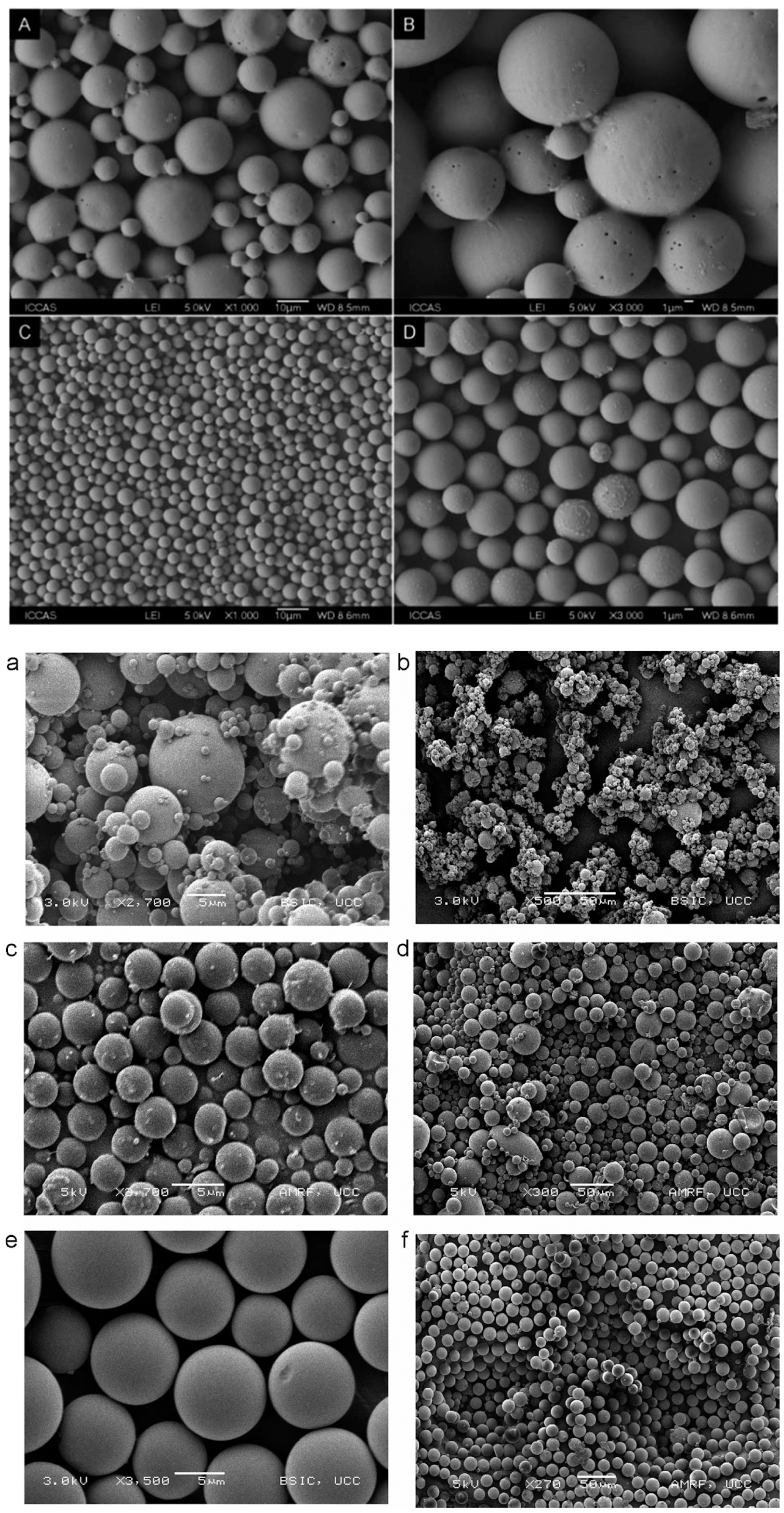
- Liu, Z.; Li, X.; Xiu, B.; Duan, C.; Li, J.; Zhang, X.; Yang, X.; Dai, W.; Johnson, H.; Zhang, H.; et al. A Novel and Simple Preparative Method for Uniform-Sized PLGA Microspheres: Preliminary Application in Antitubercular Drug Delivery. Colloids Surf. B Biointerfaces 2016, 145, 679–687. [Google Scholar] [CrossRef]
- Liu, D.; Cito, S.; Zhang, Y.; Wang, C.F.; Sikanen, T.M.; Santos, H.A. A Versatile and Robust Microfluidic Platform toward High Throughput Synthesis of Homogeneous Nanoparticles with Tunable Properties. Adv. Mater. 2015, 27, 2298–2304. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Chen, Q.; Lin, J.; Cai, Z.; Liao, G.; Wang, K.; Bai, L.; Zhao, P.; Yu, Z. Recent Advance in Polymer Based Microspheric Systems for Controlled Protein and Peptide Delivery. Curr. Med. Chem. 2019, 26, 2285–2296. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Lee, S.M.Y.; Yi, C.; Li, C.W. Controllable Synthesis of Functional Nanoparticles by Microfluidic Platforms for Biomedical Applications-a Review. Lab Chip 2017, 17, 209–226. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.G.; Rickey, M.E.; Ramstack, J.M.; Lyons, S.L.; Hotz, J.M. Method for Preparing Microparticles Having a Selected Polymer Molecular. Weight. Patent No. US-6264987-B1, 24 July 2001. [Google Scholar]
- Whitesides, G.M. The Origins and the Future of Microfluidics. Nature 2006, 442, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.H.; Sheng, F.; Wang, Z.H.; Yang, G.; Li, C.G.; Wang, H.; Song, Z.M. Shear Speed-Regulated Properties of Long-Acting Docetaxel Control Release Poly (Lactic-Co-Glycolic Acid) Microspheres. Front. Pharm. 2020, 11, 1286. [Google Scholar] [CrossRef]
- Zhang, Y.; Shams, T.; Harker, A.H.; Parhizkar, M.; Edirisinghe, M. Effect of Copolymer Composition on Particle Morphology and Release Behavior In Vitro Using Progesterone. Mater. Des. 2018, 159, 57–67. [Google Scholar] [CrossRef]
- Liu, B.; Zhou, X.; Yang, F.; Shen, H.; Wang, S.; Zhang, B.; Zhi, G.; Wu, D. Fabrication of Uniform Sized Polylactone Microcapsules by Premix Membrane Emulsification for Ultrasound Imaging. Polym. Chem. 2014, 5, 1693–1701. [Google Scholar] [CrossRef]
- Rezvantalab, S.; Keshavarz Moraveji, M. Microfluidic Assisted Synthesis of PLGA Drug Delivery Systems. RSC Adv. 2019, 9, 2055–2072. [Google Scholar] [CrossRef] [Green Version]
- Keohane, K.; Brennan, D.; Galvin, P.; Griffin, B.T. Silicon Microfluidic Flow Focusing Devices for the Production of Size-Controlled PLGA Based Drug Loaded Microparticles. Int. J. Pharm. 2014, 467, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Duncanson, W.J.; Lin, T.; Abate, A.R.; Seiffert, S.; Shah, R.K.; Weitz, D.A. Microfluidic Synthesis of Advanced Microparticles for Encapsulation and Controlled Release. Lab Chip 2012, 12, 2135–2145. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.M.; Swami, A.; Gilson, L.M.; Chopra, S.; Choi, S.; Wu, J.; Langer, R.; Karnik, R.; Farokhzad, O.C. Ultra-High Throughput Synthesis of Nanoparticles with Homogeneous Size Distribution Using a Coaxial Turbulent Jet Mixer. ACS Nano 2014, 8, 6056–6065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iqbal, M.; Zafar, N.; Fessi, H.; Elaissari, A. Double Emulsion Solvent Evaporation Techniques Used for Drug Encapsulation. Int. J. Pharm. 2015, 496, 173–190. [Google Scholar] [CrossRef]
- Swider, E.; Koshkina, O.; Tel, J.; Cruz, L.J.; de Vries, I.J.M.; Srinivas, M. Customizing Poly(Lactic-co-Glycolic Acid) Particles for Biomedical Applications. Acta Biomater. 2018, 73, 38–51. [Google Scholar] [CrossRef]
- Bohr, A.; Kristensen, J.; Dyas, M.; Edirisinghe, M.; Stride, E. Release Profile and Characteristics of Electrosprayed Particles for Oral Delivery of a Practically Insoluble Drug. J. R. Soc. Interface 2012, 9, 2437–2449. [Google Scholar] [CrossRef]
- Xie, J.; Jiang, J.; Davoodi, P.; Srinivasan, M.P.; Wang, C.H. Electrohydrodynamic Atomization: A Two-Decade Effort to Produce and Process Micro-/Nanoparticulate Materials. Chem. Eng. Sci. 2015, 125, 32–57. [Google Scholar] [CrossRef] [Green Version]
- Shi, N.-Q.; Zhou, J.; Walker, J.; Li, L.; Hong, J.K.Y.; Olsen, K.F.; Tang, J.; Ackermann, R.; Wang, Y.; Qin, B.; et al. Microencapsulation of Luteinizing Hormone-Releasing Hormone Agonist in Poly (Lactic-co-Glycolic Acid) Microspheres by Spray-Drying. J. Control Release 2020, 321, 756–772. [Google Scholar] [CrossRef]
- Hua, Y.; Wang, Z.; Wang, D.; Lin, X.; Liu, B.; Zhang, H.; Gao, J.; Zheng, A. Key Factor Study for Generic Long-Acting PLGA Microspheres Based on a Reverse Engineering of Vivitrol®. Molecules 2021, 26, 1247. [Google Scholar] [CrossRef]
- Li, T.; Chandrashekar, A.; Beig, A.; Walker, J.; Hong, J.K.Y.; Benet, A.; Kang, J.; Ackermann, R.; Wang, Y.; Qin, B.; et al. Characterization of Attributes and In Vitro Performance of Exenatide-Loaded PLGA Long-Acting Release Microspheres. Eur. J. Pharm. Biopharm. 2021, 158, 401–409. [Google Scholar] [CrossRef]
- Liang, R.; Zhang, R.; Li, X.; Wang, A.; Chen, D.; Sun, K.; Liu, W.; Li, Y. Stability of Exenatide in Poly(d,l-lactide-co-glycolide) Solutions: A Simplified Investigation on the Peptide Degradation by the Polymer. Eur. J. Pharm. Sci. 2013, 50, 502–510. [Google Scholar] [CrossRef]
- Yang, S.; Yuan, W.; Jin, T. Formulating Protein Therapeutics into Particulate Forms. Expert Opin. Drug Deliv. 2009, 6, 1123–1133. [Google Scholar] [CrossRef]
- Ghahremankhani, A.A.; Dorkoosh, F.; Dinarvand, R. PLGA-PEG-PLGA Tri-Block Copolymers as in Situ Gel-Forming Peptide Delivery System: Effect of Formulation Properties on Peptide Release. Pharm. Dev. Technol. 2008, 13, 49–55. [Google Scholar] [CrossRef]
- Haggag, Y.; Abdel-Wahab, Y.; Ojo, O.; Osman, M.; El-Gizawy, S.; El-Tanani, M.; Faheem, A.; McCarron, P. Preparation and In Vivo Evaluation of Insulin-Loaded Biodegradable Nanoparticles Prepared from Diblock Copolymers of PLGA and PEG. Int. J. Pharm. 2016, 499, 236–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haggag, Y.A.; Faheem, A.M.; Tambuwala, M.M.; Osman, M.A.; El-Gizawy, S.A.; O’Hagan, B.; Irwin, N.; McCarron, P.A. Effect of Poly(Ethylene Glycol) Content and Formulation Parameters on Particulate Properties and Intraperitoneal Delivery of Insulin from PLGA Nanoparticles Prepared Using the Double-Emulsion Evaporation Procedure. Pharm. Dev. Technol. 2017, 23, 370–381. [Google Scholar] [CrossRef] [PubMed]
- Ghitman, J.; Biru, E.I.; Stan, R.; Iovu, H. Review of Hybrid PLGA Nanoparticles: Future of Smart Drug Delivery and Theranostics Medicine. Mater. Des. 2020, 193, 108805. [Google Scholar] [CrossRef]
- Zhang, L.; Chan, J.M.; Gu, F.X.; Rhee, J.W.; Wang, A.Z.; Radovic-Moreno, A.F.; Alexis, F.; Langer, R.; Farokhzad, O.C. Self-Assembled Lipid-Polymer Hybrid Nanoparticles: A Robust Drug Delivery Platform. ACS Nano 2008, 2, 1696–1702. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Yu, B.; Wu, Y.; Huang, B.; Yuan, Y.; Liu, C.S. Controlled Preparation and Antitumor Efficacy of Vitamin e TPGS-Functionalized PLGA Nanoparticles for Delivery of Paclitaxel. Int. J. Pharm. 2013, 446, 24–33. [Google Scholar] [CrossRef]
- Gaudana, R.; Khurana, V.; Parenky, A.; Mitra, A.K. Encapsulation of Protein-Polysaccharide HIP Complex in Polymeric Nanoparticles. J. Drug Deliv. 2011, 2011, 458128. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Gaudana, R.; Mitra, A.K. A Novel Approach for Antibody Nanocarriers Development through Hydrophobic Ion-Pairing Complexation. J. Microencapsul. 2014, 31, 542–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, S.; Xu, J.; Cai, C.; Germershaus, O.; Schaper, A.; Kissel, T. Effect of WOW Process Parameters on Morphology and Burst Release of FITC-Dextran Loaded PLGA Microspheres. Int. J. Pharm. 2007, 334, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Cun, D.M.; Jensen, D.K.; Maltesen, M.J.; Bunker, M.; Whiteside, P.; Scurr, D.; Foged, C.; Nielsen, H.M. High loading efficiency and sustained release of siRNA encapsulated in PLGA nanoparticles: Quality by design optimization and characterization. Eur. J. Pharm. Biopharm. 2011, 77, 26–35. [Google Scholar] [CrossRef]
- Kakade, S.M.; Hassan, D.M. Effects of Formulation Parameters on the Characteristics of Biodegradable Microspheres of Goserelin Acetate. Asian J. Pharm. 2018, 12, 691–697. [Google Scholar] [CrossRef]
- Park, H.; Ha, D.; Ha, E.; Kim, J.; Kim, M. Effect of Stabilizers on Encapsulation Efficiency and Release Behavior of Exenatide-Loaded PLGA Microsphere Prepared by the W/O/W Solvent Evaporation Method. Pharmaceutics 2019, 11, 627. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Zhang, S.; Machado, A.; Lecommandoux, S.; Sandre, O.; Gu, F.; Colin, A. Controllable Microfluidic Production of Drug-Loaded PLGA Nanoparticles Using Partially Water-Miscible Mixed Solvent Microdroplets as a Precursor. Sci. Rep. 2017, 7, 4794. [Google Scholar] [CrossRef]
- Allison, S.D. Analysis of Initial Burst in PLGA Microparticles. Expert Opin. Drug Deliv. 2008, 5, 615–628. [Google Scholar] [CrossRef]
- Xu, Y.; Koo, D.; Gerstein, E.A.; Kim, C.S. Multi-Scale Modeling of Polymer-Drug Interactions and Their Impact on the Structural Evolutions in PLGA-Tetracycline Films. Polymer 2016, 84, 121–131. [Google Scholar] [CrossRef]
- Bragagni, M.; Gil-Alegre, M.E.; Mura, P.; Cirri, M.; Ghelardini, C.; Di Cesare Mannelli, L. Improving the Therapeutic Efficacy of Prilocaine by PLGA Microparticles: Preparation, Characterization and In Vivo Evaluation. Int. J. Pharm. 2018, 547, 24–30. [Google Scholar] [CrossRef] [Green Version]
- Gilchrist, S.E.; Rickard, D.L.; Letchford, K.; Needham, D.; Burt, H.M. Phase Separation Behavior of Fusidic Acid and Rifampicin in PLGA Microspheres. Mol. Pharm. 2012, 9, 1489–1501. [Google Scholar] [CrossRef]
- Nagarajan, R.; Barry, M.; Ruckenstein, E. Unusual Selectivity in Solubilization by Block Copolymer Micelles. Langmuir 1986, 2, 210–215. [Google Scholar] [CrossRef]
- Potter, C.B.; Davis, M.T.; Albadarin, A.B.; Walker, G.M. Investigation of the Dependence of the Flory-Huggins Interaction Parameter on Temperature and Composition in a Drug-Polymer System. Mol. Pharm. 2018, 15, 5327–5335. [Google Scholar] [CrossRef] [PubMed]
- Thakral, S.; Thakral, N.K. Prediction of Drug–Polymer Miscibility through the Use of Solubility Parameter Based Flory–Huggins Interaction Parameter and the Experimental Validation: PEG as Model Polymer. J. Pharm. Sci. 2013, 102, 2254–2263. [Google Scholar] [CrossRef] [PubMed]
- Tambasco, M.; Lipson, J.E.G.; Higgins, J.S. Blend Miscibility and the Flory-Huggins Interaction Parameter: A Critical Examination. Macromolecules 2006, 39, 4860–4868. [Google Scholar] [CrossRef]
- Callaway, C.P.; Hendrickson, K.; Bond, N.; Lee, S.M.; Sood, P.; Jang, S.S. Molecular Modeling Approach to Determine the Flory-Huggins Interaction Parameter for Polymer Miscibility Analysis. ChemPhysChem 2018, 19, 1655–1664. [Google Scholar] [CrossRef]
- Chaudhari, M.I.; Pratt, L.R.; Paulaitis, M.E. Concentration Dependence of the Flory-Huggins Interaction Parameter in Aqueous Solutions of Capped PEO Chains. J. Chem. Phys. 2014, 141, 244908. [Google Scholar] [CrossRef] [Green Version]
- Qiao, B.; Zhao, D. A Theory of Polymer Solutions without the Mean-Field Approximation in Flory-Huggins Theory. J. Chem. Phys. 2004, 121, 4968–4973. [Google Scholar] [CrossRef]
- Marquette, S.; Peerboom, C.; Yates, A.; Denis, L.; Langer, I.; Amighi, K.; Goole, J. Stability Study of Full-Length Antibody (Anti-TNF Alpha) Loaded PLGA Microspheres. Int. J. Pharm. 2014, 470, 41–50. [Google Scholar] [CrossRef]
- Koda, S.; Okumura, N.; Kitano, J.; Koizumi, N.; Tabata, Y. Development of Poly Lactic/Glycolic Acid (PLGA) Microspheres for Controlled Release of Rho-Associated Kinase Inhibitor. J. Ophthalmol. 2017, 2017, 1598218. [Google Scholar] [CrossRef] [Green Version]
- Yeo, Y.; Park, K. Control of Encapsulation Efficiency and Initial Burst in Polymeric Microparticle Systems. Arch. Pharmacal. Res. 2004, 27, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Tran, V.T.; Karam, J.P.; Garric, X.; Coudane, J.; Benoît, J.P.; Montero-Menei, C.N.; Venier-Julienne, M.C. Protein-Loaded PLGA-PEG-PLGA Microspheres: A Tool for Cell Therapy. Eur. J. Pharm. Sci. 2012, 45, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Nie, L.; Zou, P.; Suo, J. Effects of Drug and Polymer Molecular Weight on Drug Release from PLGA-MPEG Microspheres. J. Appl. Polym. Sci. 2015, 132, 1–8. [Google Scholar] [CrossRef]
- Hines, D.J.; Kaplan, D.L. Poly (Lactic-co-Glycolic Acid) Controlled Release Systems: Experimental and Modeling Insights. Crit. Rev. Inther. Drug Carr. Syst. 2013, 30, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Qi, P.; Bu, R.; Zhang, H.; Yin, J.; Chen, J.; Zhang, A.; Gou, J.; Yin, T.; Zhang, Y.; He, H.; et al. Goserelin Acetate Loaded Poloxamer Hydrogel in PLGA Microspheres: Core−Shell Di-Depot Intramuscular Sustained Release Delivery System. Mol. Pharm. 2019, 16, 3502–3513. [Google Scholar] [CrossRef] [PubMed]
| No | Brand Name | API | Indication | Type/ROA | Duration | Manufacturing Method | Year Approved | Ref. |
|---|---|---|---|---|---|---|---|---|
| 1 | Lupron Depot® | Leuprolide acetate | Advanced prostate cancer, endometriosis, fibroid | Microsphere; I.M. | 1, 3, 4, 6 months | Water-in-oil emulsification | 1989, 1995, 1997, 2011 | [9,10] |
| 2 | Zoladex® | Goserelin acetate | Advanced breast cancer in pre- and perimenopausal women, endometriosis and prostate cancer | Solid implant; S.C. | 1, 3 months | Hot melt extrusion | 1989, 1996 | [11] |
| 3 | Sandostatin® LAR | Octreotide acetate | Acromegaly | Microsphere; S.C. | 1 month | Emulsion solvent evaporation | 1998 | [9,10] |
| 4 | Atridox™ | Doxycycline hyclate | Chronic adult periodontitis | In situ gel; Periodontal | 1 week | NA | 1998 | [12] |
| 5 | Nutropin Depot® | Somatotropin | Growth hormone deficiency | Microsphere; S.C. | 1 month | Spray drying | 1999 | [13] |
| 6 | Trelstar® | Triptorelin pamoate | Palliative treatment of advanced prostate cancer | Microsphere; I.M. | 1, 3, 6 months | Spray drying or Coacervation | 2000, 2001, 2010 | [10] |
| 7 | Arestin® | Minocycline HCl | Periodontal disease | Microsphere; Periodontal | 2 weeks | NA | 2001 | [12] |
| 8 | Eligard® | Leuprolide acetate | Advanced prostate cancer | In situ gel; S.C. | 1, 3, 4, 6 months | NA | 2002 | [12] |
| 9 | Risperidal® Consta® | Risperidone | Schizophrenia, bipolar I disorder | Microsphere; I.M. | 2 weeks | Emulsion solvent evaporation | 2003, 2007 | [9] |
| 10 | Vivitrol® | Naltrexone | Alcohol dependence, opioid dependence | Microsphere; I.M. | 1 month | Emulsion solvent evaporation | 2006 | [9] |
| 11 | Somatuline® Depot | Lanreotide | Acromegaly, gastroenteropancreatic neuroendocrine tumours, Carcinoid Syndrome | Microsphere; S.C. | 1 month | Spray drying | 2007 | [10] |
| 12 | Ozurdex® | Dexamethasone | Macular edema | Solid implant; Intravitreal injection | 3 months | Spray drying | 2009 | [11] |
| 13 | Propel® | Mometasone furoate | Nasal polyps | Solid implant; Sinus implant | 1 month | NA | 2011 | [12] |
| 14 | Lupron Depot-PED® | Leuprolide acetate | Central precocious puberty | Microsphere; I.M. | 1 month | Water-in-oil emulsification | 2011 | [9] |
| 15 | Bydureon® | Exenatide | Type 2 diabetes mellitus | Microsphere; S.C. | 1 week | Emulsion solvent evaporation or coacervation | 2012 | [9,10] |
| 16 | Lupaneta Pack™ | Leuprolide acetate and norethindrone acetate * | Endometriosis | Microsphere; I.M. | 1, 3 months | NA | 2012 | [12] |
| 17 | Bydureon® Pen | Exenatide | Type 2 diabetes mellitus | Microsphere; S.C. | 1 week | Emulsion solvent evaporation or coacervation | 2014 | [9,10] |
| 18 | Signifor® LAR | Pasireotide | Acromegaly | Microsphere; I.M. | 1 month | Emulsion solvent evaporation | 2014 | [9,10] |
| 19 | Bydureon Bcise® | Exenatide | Type 2 diabetes mellitus | Microsphere; S.C. | 1 week | Emulsion solvent evaporation or coacervation | 2017 | [9,10] |
| 20 | Triptodur™ | Triptorelin pamoate | Central precocious puberty | Microsphere; I.M. | 6 months | Oil-in-water emulsification/phase separation | 2017 | [9] |
| 21 | Zilretta® | Triamcinolone acetonide | Osteoarthritis | Microsphere; Intra-articular | 3 months | NA | 2017 | [12] |
| 22 | Sublocade® | Buprenorphine | Moderate-to-severe opioid addiction | In situ gel; I.M. | 1 month | NA | 2017 | [12] |
| 23 | Sinuva™ | Mometasone furoate | Nasal polyps | Solid Sinus implant | 3 months | NA | 2017 | [14] |
| 24 | Perseris™ | Risperidone | Adult schizophrenia | In situ gel; S.C. | 1 month | NA | 2018 | [12] |
| 25 | Fensolvi® | Leuprolide acetate | Central precocious puberty | In situ gel; S.C. | 6 months | NA | 2020 | [15] |
| Physicochemical Property | Type of Constraints | Ref. |
|---|---|---|
| Lactide:glycolide ratio | Increase hydration rate and drug release rate by increasing proportion of glycolic acid | [39] |
| Glass transition temperature (Tg) | A higher processing temperature than Tg produces PLGA microspheres with a dense matrix and a smooth surface | [42] |
| Molecular weight (MW) | Affect drug release kinetics | [43] |
| Polymer architecture (i.e., star or linear branched chain) | Affect drug release characteristics; difficult to characterise the type of polymer by using conventional gel permeation chromatography and nuclear magnetic resonance spectroscopic methods | [44] |
| Porosity | High porosity results in faster polymer degradation and drug release | [43] |
| Particle size | Affect PLGA degradation and drug release | [38] |
| Drug-polymer interaction | Produce by-products and impurities | [8] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, Y.W.; Tan, W.S.; Ho, K.L.; Mariatulqabtiah, A.R.; Abu Kasim, N.H.; Abd. Rahman, N.; Wong, T.W.; Chee, C.F. Challenges and Complications of Poly(lactic-co-glycolic acid)-Based Long-Acting Drug Product Development. Pharmaceutics 2022, 14, 614. https://doi.org/10.3390/pharmaceutics14030614
Lim YW, Tan WS, Ho KL, Mariatulqabtiah AR, Abu Kasim NH, Abd. Rahman N, Wong TW, Chee CF. Challenges and Complications of Poly(lactic-co-glycolic acid)-Based Long-Acting Drug Product Development. Pharmaceutics. 2022; 14(3):614. https://doi.org/10.3390/pharmaceutics14030614
Chicago/Turabian StyleLim, Yi Wen, Wen Siang Tan, Kok Lian Ho, Abdul Razak Mariatulqabtiah, Noor Hayaty Abu Kasim, Noorsaadah Abd. Rahman, Tin Wui Wong, and Chin Fei Chee. 2022. "Challenges and Complications of Poly(lactic-co-glycolic acid)-Based Long-Acting Drug Product Development" Pharmaceutics 14, no. 3: 614. https://doi.org/10.3390/pharmaceutics14030614






