Acute and Sub-Chronic Intraperitoneal Toxicity Studies of the Elsholtzia ciliata Herbal Extract in Balb/c Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Estimation of Acute Intraperitoneal Toxicity
2.3. Estimation of Sub-Chronic Intraperitoneal Toxicity
2.4. Blood Samples and Tissues Collections
2.5. Hematology Analyzes
2.6. Serum Biochemistry Analyses
2.7. Blood Correlation Analysis
2.8. Preparation of Mitochondria and Mitochondrial Respiratory Measurements
2.9. Histological Analysis
2.10. Cytotoxicity Testing
2.11. Statistics
3. Results
3.1. Plant Material and Experimental Design
3.2. Assessment of Acute Toxicity
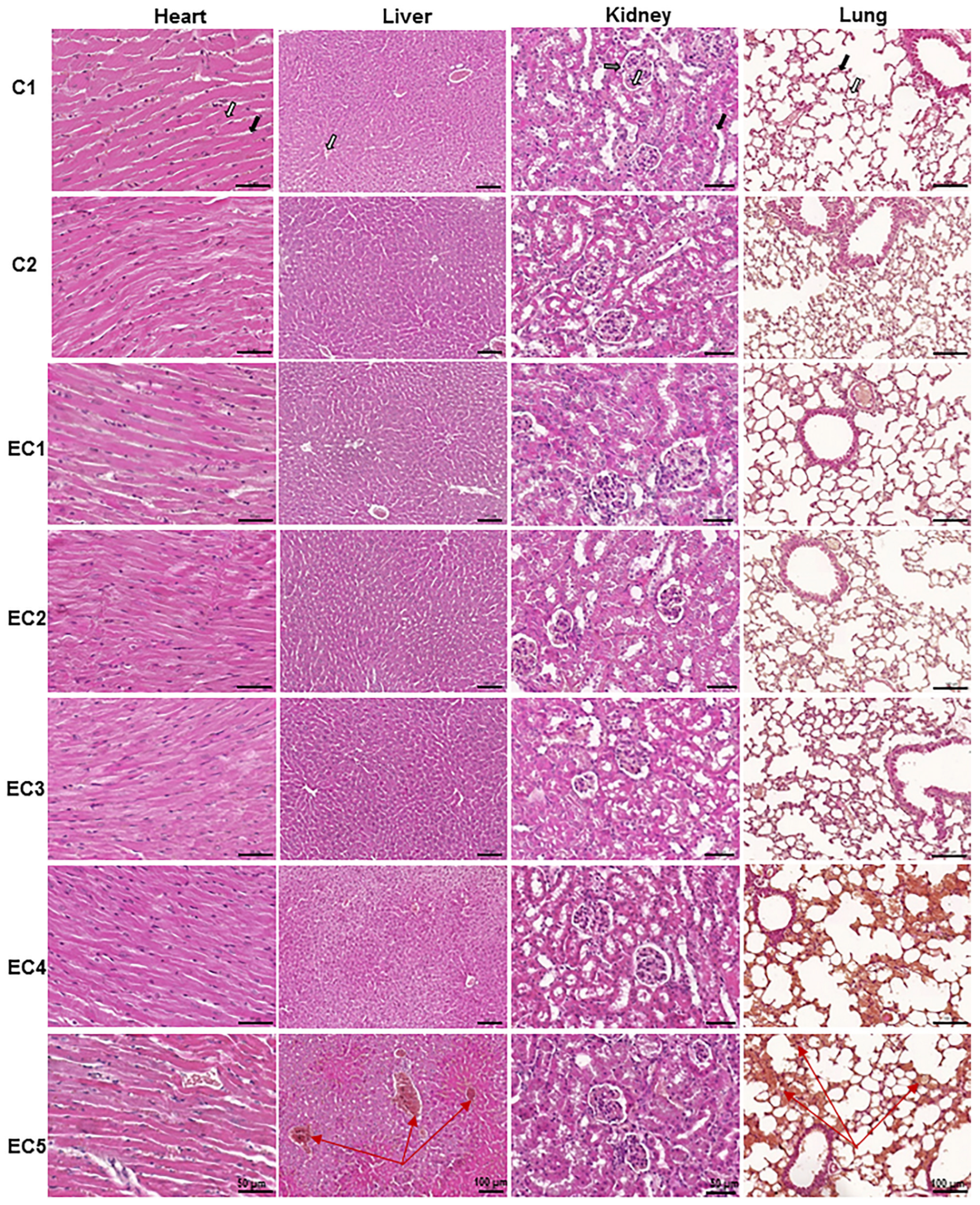
3.2.1. Evaluation of the Acute Toxicity of E. ciliata Extract from Histological Preparations
3.2.2. Detection of the Therapeutic Index and the Protective Index of E. ciliata Extract
3.3. Assessment of Sub-Chronic Toxicity
3.3.1. The Influence of E. ciliata Extract on Organs and Body Weights of Mice under the Sub-Chronic Toxicity Study
3.3.2. Evaluation of Blood Hematological Parameters
3.3.3. Evaluation of Serum Biochemical Parameters
3.3.4. Assessment of the Relationships between Blood Variables
3.3.5. Effects of E. ciliata on Mitochondrial Respiration
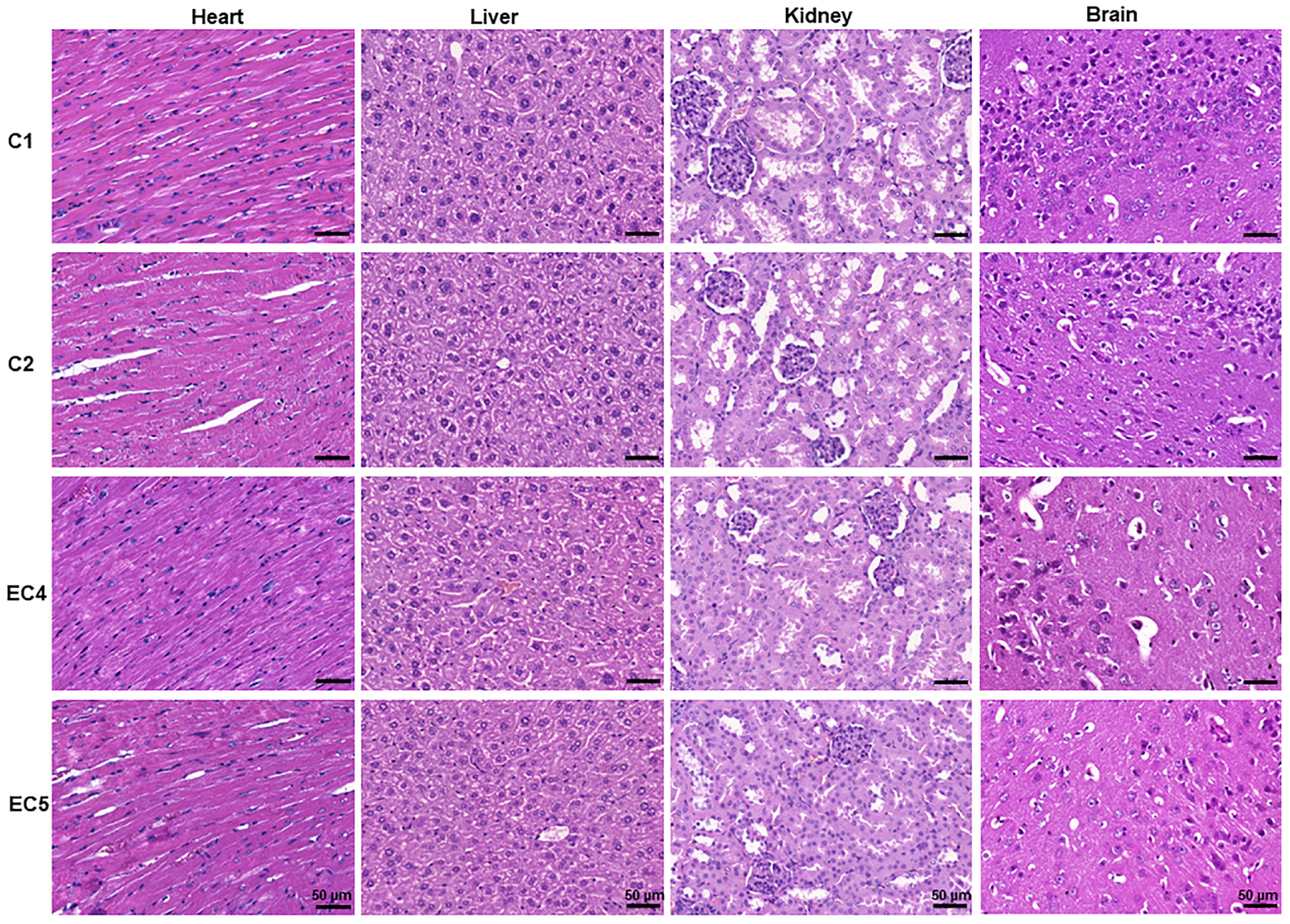
3.3.6. Evaluation of the Sub-Chronic Toxicity of E. ciliata from Histological Preparations
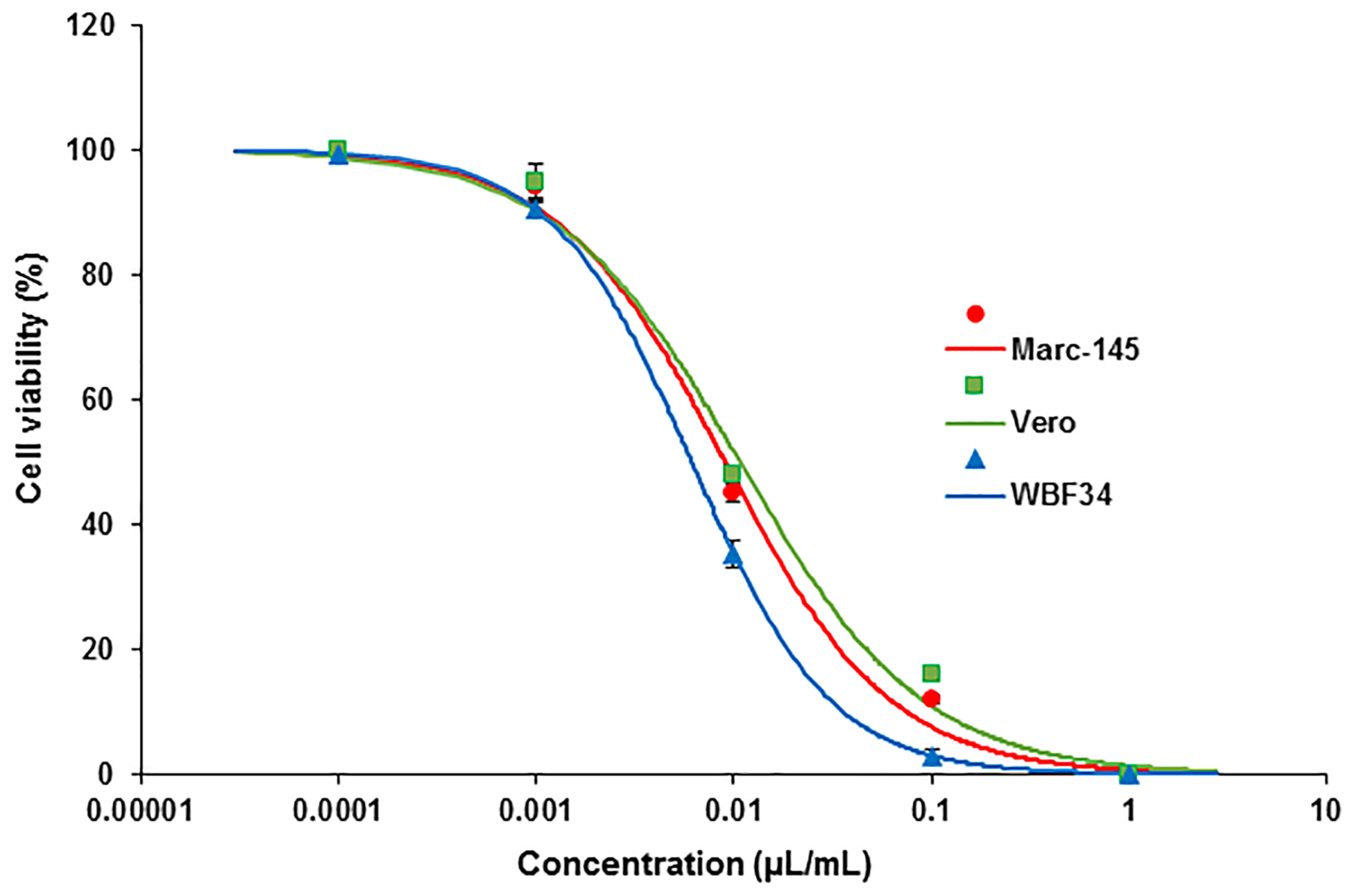
3.3.7. Evaluation of Cytotoxicity Potential in Immortalized Cell Lines
4. Discussion
5. Conclusions
- We determined a lethal dose and therapeutic index (TI) of 90, indicating a broad safety margin and suggesting a favorable safety profile for the extract.
- High-dose mortality is likely linked to drops in blood pressure rather than direct toxicity, highlighting the need for cautious dosing.
- A 60-day sub-chronic study showed no significant adverse effects on various parameters, indicating a high safety margin.
- We observed a mild inhibition of mitochondrial activity caused by the extract, which does not induce uncoupling and could potentially be beneficial in pathological conditions.
- Discrepancies between in vitro and in vivo cytotoxicity results emphasize the importance of whole-organism studies in toxicity assessment.
6. Patents
- Bernatonienė, J.; Pudžiuvelytė, L.; Jurevičius, J.; Mačianskienė, R.; Šimonytė, S. Elsholtzia Ciliata Essential Oil Extract as Antiarrhythmic Drug. WO Patent WO/2019/193400, 10 October 2019.
- Bernatonienė, J.; Pudžiuvelytė, L.; Jurevičius, J.; Mačianskienė, R.; Šimonytė, S. Elsholtzia ciliata essential oil extract as antiarrhythmic drug. 抗不整脈薬としてのエルショルツィア・シリアタ精油抽出物: 特許査定 JP2021516263; 特願 2021-500392; CPC A61K 9/0053, A61K 36/53, A61K 47/26, A61K 9/107, A61K 47/26; 申請日2018年4月6日; 公布号 2021516263A; 発行日2021年7月1日; Date of Drafting 9 December 2022 Osaka & Tokyo: Harakenzo World Patent & Trademark 2022.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chauhan, A.; Venkatesha, K.T.; Padalia, R.C.; Singh, V.R.; Verma, R.S.; Chanotiya, C.S. Essential oil composition of leaves and inflorescences of Elsholtzia densa Benth. from western Himalaya. J. Essent. Oil Res. 2019, 31, 217–222. [Google Scholar] [CrossRef]
- da Silva, L.R.R.; Ferreira, O.O.; Cruz, J.N.; Franco, C.d.J.P.; dos Anjos, T.O.; Cascaes, M.M.; da Costa, W.A.; Andrade, E.H.d.A.; de Oliveira, M.S. Lamiaceae Essential Oils, Phytochemical Profile, Antioxidant, and Biological Activities. Evidence-Based Complement. Altern. Med. 2021, 2021, 6748052. [Google Scholar] [CrossRef]
- Michel, J.; Rani, N.Z.A.; Husain, K. A Review on the Potential Use of Medicinal Plants From Asteraceae and Lamiaceae Plant Family in Cardiovascular Diseases. Front. Pharmacol. 2020, 11, 852. [Google Scholar] [CrossRef] [PubMed]
- Selvi, S.; Polat, R.; Çakilcioğlu, U.; Celep, F.; Dirmenci, T.; Ertuğ, Z.F. An ethnobotanical review on medicinal plants of the Lamiaceae family in Turkey. Turk. J. Bot. 2022, 46, 283–332. [Google Scholar] [CrossRef]
- Peng, C.I. Elsholtzia ciliata. In Flora of Taiwan, 2nd ed.; Department of Botany, National Taiwan University: Taipei, Taiwan, 1998; Volume 4, p. 459. [Google Scholar]
- Wu, Z.Y.; Li, X.W.; Huang, S.R. Flora Reipublicae Popularis Sinicae; Science Press: Beijing, China, 1977; Volume 66, pp. 304–348. [Google Scholar]
- Harley, R.M.; Atkins, S.; Budantsev, A.; Cantino, P.D.; Conn, B.J.; Grayer, R.; Harley, M. Labiatae. In The Families and Genera of Vascular Plants; Kubitzki, K., Kadereit, J.W., Eds.; Springer: Berlin/Heidelberg, Germany, 2004; Volume 7, pp. 167–275. [Google Scholar] [CrossRef]
- Pu, C.; Chen, W.; Zhou, Z. Elsholtzia litangensis sp. nov. (Lamiaceae) endemic to China. Nord. J. Bot. 2012, 30, 174–177. [Google Scholar] [CrossRef]
- Xiang, C.-L.; Liu, E.-D. Elsholtzia lamprophylla (Lamiaceae): A new species from Sichuan, southwest China. J. Syst. Evol. 2012, 50, 578–579. [Google Scholar] [CrossRef]
- Wang, F.; Liu, X.; Chen, Y.; An, Y.; Zhao, W.; Wang, L.; Tian, J.; Kong, D.; Xu, Y.; Ba, Y.; et al. Elsholtzia ciliata (Thunb.) Hyland: A Review of Phytochemistry and Pharmacology. Molecules 2022, 27, 6411. [Google Scholar] [CrossRef]
- Han, S.T. Medicinal Plants in the Republic of Korea, 1st ed.; WHO Regional Office for the Western Pacific: Manila, Philippines, 1998; p. 107. [Google Scholar]
- Pudziuvelyte, L.; Stankevicius, M.; Maruska, A.; Petrikaite, V.; Ragazinskiene, O.; Draksiene, G.; Bernatoniene, J. Chemical composition and anticancer activity of Elsholtzia ciliata essential oils and extracts prepared by different methods. Ind. Crop. Prod. 2017, 107, 90–96. [Google Scholar] [CrossRef]
- Mačianskienė, R.; Pudžiuvelytė, L.; Bernatonienė, J.; Almanaitytė, M.; Navalinskas, A.; Treinys, R.; Andriulė, I.; Jurevičius, J. Antiarrhythmic Properties of Elsholtzia ciliata Essential Oil on Electrical Activity of the Isolated Rabbit Heart and Preferential Inhibition of Sodium Conductance. Biomolecules 2020, 10, 948. [Google Scholar] [CrossRef]
- Zigmantaitė, V.; Jonušaitė, E.; Grigalevičiūtė, R.; Kučinskas, A.; Treinys, R.; Navalinskas, A.; Žvikas, V.; Jakštas, V.; Pudžiuvelytė, L.; Bernatonienė, J.; et al. Evaluation of the Cardiac Electrophysiological and Haemodynamic Effects of Elsholtzia ciliata Essential Oil on Swine. Pharmaceuticals 2022, 15, 982. [Google Scholar] [CrossRef]
- Shi, X.F.; He, F.J.; Yu, Y. Study on chemical constituents of essential oil from Elsholtzia ciliate (Thunb.) Hyland. Gansu Med. 1994, 13, 152–153. [Google Scholar]
- Thappa, R.K.; Agarwal, S.G.; Kapahl, B.K.; Srivastava, T.N. Chemosystematics of the Himalayan Elsholtzia. J. Essent. Oil Res. 1999, 11, 97–103. [Google Scholar] [CrossRef]
- Korolyuk, E.A.; König, W.; Tkachev, A.V. Composition of essential oil of Elsholtzia ciliata (Thunb.) Hyl. from the Novosibirsk region, Russia. Chem. Plant Mater. 2002, 1, 31–36. [Google Scholar]
- Shin, S. Study on activities of the essential oil from Elsholtzia ciliata against some antibiotic-susceptible and resistant strains of pathogenic bacteria. Yakhak Hoeji 2010, 54, 122–125. [Google Scholar]
- Liu, X.P.; Jing, X.M. Study on chemical constituents and biological activities of E. Ciliata essential oil. J. Heilongjiang Bayi Agric. Univ. 2018, 30, 1002–2090. [Google Scholar]
- Zhao, M.P.; Liu, X.C.; Lai, D.; Zhou, L.; Liu, Z.L. Analysis of the Essential Oil of Elsholtzia ciliate Aerial Parts and Its Insecticidal Activities against Liposcelis bostrychophila. Helvetica Chim. Acta 2016, 99, 90–94. [Google Scholar] [CrossRef]
- Liang, J.-Y.; Xu, J.; Yang, Y.-Y.; Shao, Y.-Z.; Zhou, F.; Wang, J.-L. Toxicity and Synergistic Effect of Elsholtzia ciliata Essential Oil and Its Main Components against the Adult and Larval Stages of Tribolium castaneum. Foods 2020, 9, 345. [Google Scholar] [CrossRef]
- Song, B.M.; Choi, J.S.; Park, H.J. Composition and Anti-cholinesterase Activity of the Essential Oil Obtained from Korean Elsholtzia ciliata. Korean J. Pharmacogn. 2016, 47, 226–231. [Google Scholar]
- Nhan, N.T.; Le, V.T.T.; Thao, N.T.; Hanh, T.T.P.; Luong, N.X.; Cuong, T.D.; Hung, D.V.; Lam, D.T. Chemical Composition and Biological Activities of Essential Oil of Elsholtzia ciliata obtained at Central Highlands of Vietnam’s Two Seasons. Asian J. Chem. 2022, 34, 2849–2853. [Google Scholar] [CrossRef]
- Li, F.; Wang, C.; Xu, J.; Wang, X.; Cao, M.; Wang, S.; Zhang, T.; Xu, Y.; Wang, J.; Pan, S.; et al. Evaluation of the antibacterial activity of Elsholtzia ciliate essential oil against halitosis-related Fusobacterium nucleatum and Porphyromonas gingivalis. Front. Microbiol. 2023, 14, 1219004. [Google Scholar] [CrossRef]
- To, D.C.; Ngu, T.N.; Nguyen, V.T.; Hanh, D.T.B.; Phong, T.B.; Nguyen, P.H.; Tran, M.H. Phytochemical Composition and Antioxidant Activity of Flavonoid-Rich Extracts of Elsholtzia ciliata Collected in Dak Lak Province, Vietnam. Curr. Overv. Pharm. Sci. 2023, 6, 16–32. [Google Scholar] [CrossRef]
- Guo, Z.; Liu, Z.; Wang, X.; Liu, W.; Jiang, R.; Cheng, R.; She, G. Elsholtzia: Phytochemistry and biological activities. Chem. Central J. 2012, 6, 147. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Chen, J.; Xu, Y.; Wang, X.; Li, J. Elsholtzia: A genus with antibacterial, antiviral, and anti-inflammatory advantages. J. Ethnopharmacol. 2022, 297, 115549. [Google Scholar] [CrossRef]
- Bernatonienė, J.; Pudžiuvelytė, L.; Jurevičius, J.; Mačianskienė, R.; Šimonytė, S. Elsholtzia ciliata Essential Oil Extract as Antiarrhythmic Drug. WO Patent WO/2019/193400, 10 October 2019. [Google Scholar]
- Bernatonienė, J.; Pudžiuvelytė, L.; Jurevičius, J.; Mačianskienė, R.; Šimonytė, S. Elsholtzia ciliate Essential Oil Extract as Antiarrhythmic Drug. JP Patent JP2021516263, 9 December 2022. [Google Scholar]
- Kim, D.W.; Son, K.H.; Chang, H.W.; Bae, K.; Kang, S.S.; Kim, H.P. Anti-inflammatory activity of Elsholtzia splendens. Arch. Pharmacal Res. 2003, 26, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Zotsenko, L.; Kyslychenko, V.; Kalko, K.; Drogovoz, S. The study of phenolic composition and acute toxicity, anti-inflammatory and analgesic effects of dry extracts of some Elsholtzia genus (Lamiaceae) species. PharmacologyOnLine 2021, 2, 637–649. [Google Scholar]
- Mai, P.T.; Ha, H.T.T.; Suu, B.T.; Thao, L.T.; Quyen, N.T.; Toan, T.D.; Lien, V.T.; Rei, Y. Screening of Five Lamiaceae Essential Oils as Repellents for Sweet Potato Weevil, Cylas Formicarius (F.) (Coleoptera: Brentidae). Asian J. Agric. Rural. Dev. 2021, 11, 327–333. [Google Scholar] [CrossRef]
- Turner, P.V.; Brabb, T.; Pekow, C.; Vasbinder, M.A. Administration of substances to laboratory animals: Routes of administration and factors to consider. J. Am. Assoc. Lab. Anim. Sci. 2011, 50, 600–613. [Google Scholar]
- Levin-Arama, M.; Abraham, L.; Waner, T.; Harmelin, A.; Steinberg, D.M.; Lahav, T.; Harlev, M. Subcutaneous Compared with Intraperitoneal KetamineXylazine for Anesthesia of Mice. J. Am. Assoc. Lab. Anim. Sci. 2016, 55, 794–800. [Google Scholar]
- Parasuraman, S.; Raveendran, R.; Kesavan, R. Blood sample collection in small laboratory animals. J. Pharmacol. Pharmacother. 2010, 1, 87. [Google Scholar] [CrossRef]
- NC3Rs. National Centre for the Replacement, Refinement and Reduction of Animals in Research. Available online: https://www.nc3rs.org.uk/3rs-resources/blood-sampling/blood-sampling-mouse (accessed on 11 May 2023).
- Riss, T.L.; Moravec, R.A.; Niles, A.L.; Duellman, S.; Benink, H.A.; Worzella, T.J.; Minor, T.J. Cell Viability Assays. Assay Guidance Manual. Available online: https://www.ncbi.nlm.nih.gov/books/NBK144065/?report=reader (accessed on 5 June 2023).
- Rice, N.C.; Rauscher, N.A.; Wilkins, W.L.; Lippner, D.S.; Rockwood, G.A.; Myers, T.M. Behavioural and physiological assessments of dimethyl trisulfide treatment for acute oral sodium cyanide poisoning. Basic Clin. Pharmacol. Toxicol. 2019, 125, 289–303. [Google Scholar] [CrossRef]
- Stahl, F.R.; Jung, R.; Jazbutyte, V.; Ostermann, E.; Tödter, S.; Brixel, R.; Kemmer, A.; Halle, S.; Rose-John, S.; Messerle, M.; et al. Laboratory diagnostics of murine blood for detection of mouse cytomegalovirus (MCMV)-induced hepatitis. Sci. Rep. 2018, 8, 14823. [Google Scholar] [CrossRef] [PubMed]
- Charles River Laboratories. BALB/C Mouse Hematology. Available online: https://www.criver.com/sites/default/files/resources/doc_a/BALBcMouseClinicalPathologyData.pdf (accessed on 5 June 2023).
- Dubey, V.K.; Madan, S.; Rajput, S.K.; Singh, A.T.; Jaggi, M.; Mittal, A.K. Single and repeated dose (28 days) intravenous toxicity assessment of bartogenic acid (an active pentacyclic triterpenoid) isolated from Barringtonia racemosa (L.) fruits in mice. Curr. Res. Toxicol. 2022, 3, 100057. [Google Scholar] [CrossRef] [PubMed]
- Santos, E.W.; de Oliveira, D.C.; Hastreiter, A.; da Silva, G.B.; Beltran, J.S.d.O.; Tsujita, M.; Crisma, A.R.; Neves, S.M.P.; Fock, R.A.; Borelli, P. Hematological and biochemical reference values for C57BL/6, Swiss Webster and BALB/c mice. Braz. J. Veter- Res. Anim. Sci. 2016, 53, 138–145. [Google Scholar] [CrossRef]
- Provencher Bolliger, A.; Everds, N.E.; Zimmerman, K.L.; Moore, D.M.; Smith, S.A.; Barnhart, K.F. Hematology of laboratory animals. In Schalm’s Veterinary Hematology, 6th ed.; Weiss, D., Wardrop, J., Schalm, O.W., Eds.; Wiley–Blackwell: Hoboken, NJ, USA, 2010; pp. 852–887. [Google Scholar]
- Silva-Santana, G.; Bax, J.C.; Fernandes, D.C.S.; Bacellar, D.T.L.; Hooper, C.; Dias, A.A.S.O.; Silva, C.B.; de Souza, A.M.; Ramos, S.; Santos, R.A.; et al. Clinical hematological and biochemical parameters in Swiss, BALB/c, C57BL/6 and B6D2F1 Mus musculus. Anim. Model. Exp. Med. 2020, 3, 304–315. [Google Scholar] [CrossRef] [PubMed]
- Mathers, R.A.; Evans, G.O.; Bleby, J. Platelet measurements in rat, dog and mouse blood samples using the Sysmex XT-2000iV. Comp. Clin. Pathol. 2013, 22, 815–821. [Google Scholar] [CrossRef]
- Iversen, N.K.; Malte, H.; Baatrup, E.; Wang, T. The normal acid–base status of mice. Respir. Physiol. Neurobiol. 2012, 180, 252–257. [Google Scholar] [CrossRef]
- Thal, S.C.; Plesnila, N. Non-invasive intraoperative monitoring of blood pressure and arterial pCO2 during surgical anesthesia in mice. J. Neurosci. Methods 2007, 159, 261–267. [Google Scholar] [CrossRef]
- Lee, E.J.; Woodske, M.E.; Zou, B.; O’Donnell, C.P.; Loeven, A.M.; Receno, C.N.; Cunningham, C.M.; DeRuisseau, L.R.; Lim, D.C.; Brady, D.C.; et al. Dynamic arterial blood gas analysis in conscious, unrestrained C57BL/6J mice during exposure to intermittent hypoxia. J. Appl. Physiol. 2009, 107, 290–294. [Google Scholar] [CrossRef]
- Burns, D.P.; Roy, A.; Lucking, E.F.; McDonald, F.B.; Gray, S.; Wilson, R.J.; Edge, D.; O’Halloran, K.D. Sensorimotor control of breathing in the mdx mouse model of Duchenne muscular dystrophy. J. Physiol. 2017, 595, 6653–6672. [Google Scholar] [CrossRef]
- Schwarzkopf, T.M.; Horn, T.; Lang, D.; Klein, J. Blood gases and energy metabolites in mouse blood before and after cerebral ischemia: The effects of anesthetics. Exp. Biol. Med. 2013, 238, 84–89. [Google Scholar] [CrossRef]
- Svenson, K.L.; Von Smith, R.; Magnani, P.A.; Suetin, H.R.; Paigen, B.; Naggert, J.K.; Li, R.; Churchill, G.A.; Peters, L.L. Multiple trait measurements in 43 inbred mouse strains capture the phenotypic diversity characteristic of human populations. J. Appl. Physiol. 2007, 102, 2369–2378. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.S.; Walter, G.L.; Walker, R.M. Clinical pathology in non-clinical toxicology testing. In Haschek and Rousseaux’s Handbook of Toxicologic Pathology; Haschek, M.W., Rousseaux, G.C., Wallig, A.M., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 565–594. [Google Scholar] [CrossRef]
- Subramanian, K.; Sankaramourthy, D.; Gunasekaran, M. Toxicity studies related to medicinal plants. In Natural Products and Drug Discovery; Mandal, C.S., Mandal, V., Konishi, T., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 491–505. [Google Scholar] [CrossRef]
- Al Shoyaib, A.; Archie, S.R.; Karamyan, V.T. Intraperitoneal Route of Drug Administration: Should it Be Used in Experimental Animal Studies? Pharm. Res. 2019, 37, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Tamargo, J.; Le Heuzey, J.-Y.; Mabo, P. Narrow therapeutic index drugs: A clinical pharmacological consideration to flecainide. Eur. J. Clin. Pharmacol. 2015, 71, 549–567. [Google Scholar] [CrossRef] [PubMed]
- Buehler, G. History of Bioequivalence for Critical Dose Drugs. Office of Pharmacological Science. US Food and Drug Administration (13 April 2010). Available online: www.fda.gov (accessed on 18 May 2023).
- U.S. Food and Drug Administration. CFR-Code of Federal Register 21, Section 320.33 (21CFR320.33). Criteria and Evidence to Assess Actual or Potential Bioequivalence Problems; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2014.
- Collinsworth, K.A.; Kalman, S.M.; Harrison, D.C. The Clinical Pharmacology of Lidocaine as an Antiarrhythymic Drug. Circulation 1974, 50, 1217–1230. [Google Scholar] [CrossRef] [PubMed]
- Campbell, T.J.; Williams, K.M. Therapeutic drug monitoring: Antiarrhythmic drugs. Br. J. Clin. Pharmacol. 1998, 46, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Pessini, P.G.d.S.; de Souza, P.R.K.; Chagas, C.d.S.; Sampaio, E.G.; Neves, D.S.; Petri, G.; Fonseca, F.L.A.; da Silva, E.B. Hematological reference values and animal welfare parameters of BALB/C-FMABC (Mus musculus) inoculated with Ehrlich tumor kept in the vivarium at ABC Medical School. Anim. Model. Exp. Med. 2020, 3, 32–39. [Google Scholar] [CrossRef]
- Kim, H.; Zuo, G.; Lee, S.K.; Lim, S.S. Acute and subchronic toxicity study of nonpolar extract of licorice roots in mice. Food Sci. Nutr. 2020, 8, 2242–2250. [Google Scholar] [CrossRef]
- Nemzek, J.A.; Bolgos, G.L.; Williams, B.A.; Remick, D.G. Differences in normal values for murine white blood cell counts and other hematological parameters based on sampling site. Inflamm. Res. 2001, 50, 523–527. [Google Scholar] [CrossRef]
- Shahsavani, D.; Kazerani, H.R.; Kaveh, S.; Gholipour-Kanani, H. Determination of some normal serum parameters in starry sturgeon (Acipenser stellatus Pallas, 1771) during spring season. Comp. Clin. Pathol. 2010, 19, 57–61. [Google Scholar] [CrossRef]
- Mehta, A.K.; Arora, N.; Gaur, S.N.; Singh, B.P. Acute toxicity assessment of choline by inhalation, intraperitoneal and oral routes in Balb/c mice. Regul. Toxicol. Pharmacol. 2009, 54, 282–286. [Google Scholar] [CrossRef]
- Ribeiro-Alves, M.A.; Gordan, P.A. Diagnosis of anemia in patients with chronic kidney disease. Braz. J. Nephrol. 2014, 36, 9–12. [Google Scholar] [CrossRef]
- Weiss, D.J.; Wardrop, K.J. Schalm’s Veterinary Hematology, 6th ed.; Weiss, D.J., Wardrop, K.J., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2010. [Google Scholar]
- Shrimanker, I.; Bhattarai, S. Electrolytes; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Hopkins, E.; Sanvictores, T.; Sharma, S. Physiology, Acid Base Balance; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Schumann, G.; Bonora, R.; Ceriotti, F.; Ferard, G.; Ferrero, C.A.; Franck, P.F. Reference procedure for the measurement of catalytic concentration of gamma-glutamyltransferase. Clin. Chem. Lab. Med. 2002, 40, 734–738. [Google Scholar] [CrossRef]
- Barbosa, B.D.S.; Praxedes, A.; Lima, M.A.; Pimentel, M.M.L.; Santos, F.A.; Brito, P.D.; Lelis, I.C.N.G.; de Macedo, M.F.; Bezerra, M.B. Haematological and Biochemical Profile of Balb-c Mice. Acta Sci. Veter. 2017, 45, 1477. [Google Scholar] [CrossRef]
- Levey, A.S.; Perrone, R.D.; E Madias, N. Serum Creatinine and Renal Function. Annu. Rev. Med. 1988, 39, 465–490. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Meyer, M.; Turk, T.R.; Wilde, B.; Feldkamp, T.; Assert, R.; Wu, K.; Kribben, A.; Witzke, O. Serum cystatin C in mouse models: A reliable and precise marker for renal function and superior to serum creatinine. Nephrol. Dial. Transplant. 2009, 24, 1157–1161. [Google Scholar] [CrossRef]
- Junghanns, M.K. Aids to diagnosis. In Essentials of Avian Medicine and Sugery, 3rd ed.; Blackwell Publishing: Hoboken, NJ, USA, 2007; pp. 56–71. [Google Scholar] [CrossRef]
- Zhang, Y.; Ye, J. Mitochondrial inhibitor as a new class of insulin sensitizer. Acta Pharm. Sin. B 2012, 2, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.A.; Perry, J.B.; Allen, M.E.; Sabbah, H.N.; Stauffer, B.L.; Shaikh, S.R.; Cleland, J.G.; Colucci, W.S.; Butler, J.; Voors, A.A.; et al. Expert consensus document: Mitochondrial function as a therapeutic target in heart failure. Nat. Rev. Cardiol. 2017, 14, 238–250. [Google Scholar] [CrossRef]
- Varga, Z.V.; Ferdinandy, P.; Liaudet, L.; Pacher, P. Drug-induced mitochondrial dysfunction and cardiotoxicity. Am J Physiol Heart Circ. Physiol. 2015, 309, H1453–H1467. [Google Scholar] [CrossRef]
- Zhang, Q.; Porto, N.M.; Guilhon, C.C.; Giorno, T.B.S.; Alviano, D.S.; Agra, M.D.F.; Fernande, D.P.; Boylan, F. Pharmacognostic study on Elsholtzia ciliata (Thumb.) Hyl: Anatomy, phytochemistry and pharmacological activities. Pharmaceuticals 2021, 14, 1152. [Google Scholar] [CrossRef]
- World Health Organization. Reasearch Guidelines for Evaluating the Safety and Efficacy of Herbal Medicines; World Health Organization, Regional Office for the Western Pacific: Manila, Philippines, 1993. [Google Scholar]
- Coon, J.T.; Ernst, E. Panax ginseng: A systematic review of adverse effects and drug interactions. Drug Saf. 2002, 25, 323–344. [Google Scholar] [CrossRef]
- Ernst, E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John’s Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann. Intern. Med. 2002, 136, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Ang-Lee, M.K.; Moss, J.; Yuan, C.S. Herbal medicines and perioperative care. JAMA 2001, 286, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Marwick, C. Trials reveal no benefit, possible harm of beta carotene and vitamin A for lung cancer prevention. JAMA 1996, 275, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Haller, C.A.; Benowitz, N.L. Adverse cardiovascular and central nervous system events associated with dietary supplements containing ephedra alkaloids. N. Engl. J. Med. 2000, 343, 1833–1838. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.B. A report of 2 cases of Nux Vomica poisoning. GuangMing J. Tradit. Chin. Med. 1998, 13, 52. [Google Scholar]





| Group | n | Dose (μL) | Concentration | Degree of Liver Damage | Dead (n) | Mortality (%) | ||
|---|---|---|---|---|---|---|---|---|
| (μL/mL) | No (0) | Minor (1) | Major (2) | |||||
| EC1 | 4 | 1 | 0.63 | 4 | 0 | 0 | 0 | 0 |
| EC2 | 4 | 3 | 1.9 | 4 | 0 | 0 | 0 | 0 |
| EC3 | 4 | 5 | 3.2 | 3 | 1 | 0 | 0 | 0 |
| EC4 | 4 | 10 | 6.3 | 2 | 2 | 0 | 1 | 25 |
| EC5 | 4 | 20 | 12.7 | 0 | 1 | 3 | 2 | 50 |
| Weight | Saline | Olive Oil | E. ciliata | Extract | |||
|---|---|---|---|---|---|---|---|
| (g) | C1 | C2 | EC1 | EC2 | EC3 | EC4 | EC5 |
| 0.01 μL | 0.03 μL | 0.1 μL | 0.3 μL | 1 μL | |||
| Body | 27.12 ± 1.75 | 28.92 ± 0.98 | 29.69 ± 1.05 | 29.54 ± 0.33 | 29.93 ± 0.15 * | 29.98 ± 0.55 * | 29.22 ± 0.43 |
| Liver | 1.48 ± 0.28 | 1.77 ± 0.05 | 1.97 ± 0.10 * | 1.99 ± 0.04 * | 2.0 ± 0.06 * | 1.85 ± 0.08 * | 1.83 ± 0.05 * |
| Heart | 0.21 ± 0.01 | 0.22 ± 0.01 | 0.23 ± 0.01 | 0.22 ± 0.01 | 0.23 ± 0.01 | 0.22 ± 0.01 | 0.23 ± 0.02 |
| Spleen | 0.13 ± 0.01 | 0.16 ± 0.00 * | 0.16 ± 0.01 * | 0.15 ± 0.00 | 0.16 ± 0.00 * | 0.15 ± 0.01 * | 0.15 ± 0.00 # |
| Kidney | 0.29 ± 0.03 | 0.30 ± 0.01 | 0.31 ± 0.01 | 0.32 ± 0.00 | 0.32 ± 0.01 | 0.31 ± 0.01 | 0.32 ± 0.01 |
| Lung | 0.21 ± 0.02 | 0.22 ± 0.01 | 0.23 ± 0.01 | 0.21 ± 0.01 | 0.23 ± 0.00 | 0.23 ± 0.01 | 0.23 ± 0.01 |
| Brain | 0.42 ± 0.02 | 0.42 ± 0.01 | 0.42 ± 0.01 | 0.42 ± 0.00 | 0.43 ± 0.01 | 0.43 ± 0.01 | 0.43 ± 0.01 |
| Blood | Saline | Olive Oil | E. ciliata | Extract | Range | Ref. | |||
|---|---|---|---|---|---|---|---|---|---|
| Parameters | C1 | C2 | EC1 | EC2 | EC3 | EC4 | EC5 | ||
| 0.01 μL | 0.03 μL | 0.1 μL | 0.3 μL | 1 μL | |||||
| WBC | 7.6 ± 1.44 | 6.4 ± 0.81 | 3.9 ± 1.02 *# | 3.1 ± 0.50 *# | 3.9 ± 0.59 *# | 3.5 ± 0.67 *# | 4.2 ± 0.76 *# | 2.5–14.5 | [39,40] |
| LYM | 6.0 ± 1.17 | 4.7 ± 0.63 | 2.8 ± 0.80 *# | 2.2 ± 0.40 *# | 2.7 ± 0.43 *# | 2.5 ± 0.47 *# | 3.2 ± 0.76 * | 2.2–12.8 | [39,40] |
| MON | 1.2 ± 0.23 | 1.2 ± 0.25 | 0.72 ± 0.14 | 0.66 ± 0.10 *# | 0.72 ± 0.11 | 0.64 ± 0.14 *# | 0.62 ± 0.06 *# | 0.0–1.3 | [39,40] |
| NEU | 0.45 ± 0.10 | 0.48 ± 0.02 | 0.34 ± 0.08 | 0.30 ± 0.03 # | 0.42 ± 0.12 | 0.34 ± 0.07 | 0.32 ± 0.07 | 0.03–3.8 | [39,40] |
| LYM% | 75.7 ± 4.70 | 73.3 ± 2.89 | 72.7 ± 1.60 | 68.8 ± 2.05 | 70.6 ± 2.63 | 58.9 ± 12.94 | 75.0 ± 3.77 | 48.8–83 | [40,41] |
| MON% | 13.8 ± 0.51 | 14.5 ± 3.99 | 19.2 ± 1.73 * | 21.7 ± 1.48 *# | 18.8 ± 1.19 * | 17.7 ± 1.32 * | 16.0 ± 2.08 | 0.1–14.3 | [40,41] |
| NEU% | 8.2 ± 2.87 | 8.1 ± 1.15 | 8.1 ± 1.12 | 9.5 ± 0.86 | 11.2 ± 2.04 | 10.6 ± 1.14 | 9.1 ± 2.08 | 1.7–39.1 | [39,40] |
| RBC | 7.4 ± 0.17 | 6.2 ± 0.36 * | 6.0 ± 0.28 * | 6.0 ± 0.23 * | 6.6 ± 0.29 * | 6.7 ± 0.24 * | 6.9 ± 0.36 | 6.9–12 | [40,41] |
| HGB | 14.6 ± 0.80 | 13.6 ± 9.01 | 12.9 ± 5.38 | 13.4 ± 7.22 | 14.2 ± 5.56 | 14.4 ± 3.67 | 15.1 ± 8.95 | 11.5–21 | [40,41] |
| HCT | 36.5 ± 1.78 | 33.4 ± 2.0 | 32.1 ± 2.0 | 32.8 ± 1.0 | 35.9 ± 2.0 | 35.8 ± 1.0 | 37.9 ± 2.0 | 31–68 | [40,41] |
| MCV | 49.6 ± 1.69 | 53.7 ± 0.44 * | 53.8 ± 0.51 * | 54.7 ± 0.47 * | 54.4 ± 0.16 * | 53.7 ± 0.48 * | 53.4 ± 0.64 * | 41.5–64 | [40,42] |
| MCH | 18.5 ± 0.27 | 21.8 ± 0.34 * | 21.7 ± 0.50 * | 22.3 ± 0.38 * | 21.5 ± 0.42 * | 21.5 ± 0.36 * | 22.0 ± 0.52 * | 13.2–19 | [40,41] |
| MCHC | 38.3 ± 1.09 | 40.5 ± 0.56 * | 40.4 ± 1.28 | 40.8 ± 0.81 * | 40.6 ± 1.75 | 40.1 ± 0.71 | 41.1 ± 0.53 * | 30–38 | [39,43] |
| RDW | 16.5 ± 0.54 | 15.0 ± 0.18 * | 15.2 ± 0.27 * | 15.1 ± 0.16 * | 15.1 ± 0.05 * | 15.0 ± 0.18 * | 15.4 ± 0.28 * | 12–23 | [40,41] |
| PLT | 735.0 ± 58.7 | 624.6 ± 88.9 | 647.8 ± 83.72 | 626.8 ± 86.33 | 707.6 ± 35.6 | 651.4 ± 5.51 * | 630.2 ± 91.45 | 420–1698 | [40,41] |
| MPV | 5.9 ± 0.09 | 6.4 ± 0.20 * | 6.4 ± 0.15 * | 6.3 ± 0.31 | 6.2 ± 0.27 | 6.2 ± 0.35 | 6.3 ± 0.18 * | 5.6–7.4 | [39,44] |
| PCT | 0.46 ± 0.05 | 0.43 ± 0.06 | 0.41 ± 0.05 | 0.39 ± 0.04 | 0.44 ± 0.02 | 0.40 ± 0.03 | 0.40 ± 0.06 | 0.1–1.1 | [39,45] |
| PDW | 15.8 ± 1.79 | 13.5 ± 0.13 * | 13.2 ± 0.43 * | 13.5 ± 0.38 | 13.2 ± 0.34 * | 13.0 ± 0.20 * | 13.5 ± 0.58 | - | - |
| Serum Parameters | Saline | Olive Oil | E. ciliata | Extract | Range | Ref. | |||
|---|---|---|---|---|---|---|---|---|---|
| C1 | C2 | EC1 | EC2 | EC3 | EC4 | EC5 | |||
| 0.01 μL | 0.03 μL | 0.1 μL | 0.3 μL | 1 μL | |||||
| pH | 7.2 ± 0.02 | 7.1 ± 0.07 | 7.0 ± 0.03 * | 7.0 ± 0.02 * | 7.0 ± 0.05 * | 7.1 ± 0.05 | 7.0 ± 0.05 * | 7.2–7.4 | [46] |
| pCO2 | 45.4 ± 1.79 | 52.6 ± 10.35 | 65.6 ± 3.10 * | 72.1 ± 4.64 *# | 68.2 ± 4.69 * | 63.2 ± 6.33 * | 64.7 ± 7.88 * | 30–45 | [46] |
| pO2 | 76.0 ± 5.13 | 71.4 ± 33.26 | 50.2 ± 4.99 * | 42.5 ± 6.39 * | 37.9 ± 3.18 * | 48.0 ± 12.09 * | 57.5 ± 13.29 | 75–133 | [47,48] |
| cHCO3− | 20.7 ± 2.05 | 15.9 ± 0.98 * | 16.0 ± 1.21 * | 17.7 ± 0.59 | 17.9 ± 1.11 | 19.6 ± 0.5 # | 17.0 ± 1.95 | 18–22 | [46,49] |
| BE (ecf) | −9.1 ± 1.69 | −13.5 ± 1.33 * | −15.4 ± 1.69 * | −13.5 ± 0.62 * | −13.0 ± 1.87 | −9.9 ± 1.15 | −13.9 ± 2.6 | - | - |
| cSO2 | 67.8 ± 8.60 | 65.2 ± 15.7 | 61.8 ± 4.79 | 50.4 ± 10.29 | 46.6 ± 5.69 * | 58.1 ± 11.52 | 64.0 ± 10.42 | - | - |
| Na+ | 142.7 ± 2.19 | 150.4 ± 2.4 * | 157.2 ± 1.2 *# | 156.4 ± 2.62 *# | 151.8 ± 3.61 * | 151.6 ± 1.69 * | 153.4 ± 3.26 * | 125–187 | [39,40] |
| K+ | 5.2 ± 0.17 | 5.2 ± 0.38 | 5.5 ± 0.24 | 4.7 ± 0.21 * | 5.1 ± 0.36 | 5.0 ± 0.37 | 5.3 ± 0.29 | 3.1–12.2 | [39,40] |
| Ca2+ | 0.75 ± 0.10 | 0.59 ± 0.09 | 0.87 ± 0.05 # | 0.77 ± 0.05 | 0.79 ± 0.08 | 0.77 ± 0.07 | 0.73 ± 0.1 | 0.4–2.5 | [39,42] |
| Cl− | 117.8 ± 1.56 | 119.6 ± 0.51 | 122.8 ± 2.67 * | 117.8 ± 1.36 | 119.4 ± 1.29 | 118.8 ± 0.97 | 120.4 ± 1.94 | 107–139 | [39,40] |
| CTCO2 | 22.1 ± 2.34 | 17.0 ± 1.03 * | 17.5 ± 1.14 * | 19.3 ± 0.63 # | 19.2 ± 0.97 | 20.7 ± 0.4 # | 18.3 ± 1.88 | 21–23.4 | [49] |
| Hct | 36.7 ± 1.56 | 32.6 ± 0.81 * | 34.6 ± 0.87 | 35.4 ± 0.8 # | 35.0 ± 1.87 | 36.0 ± 1.18 # | 35.0 ± 1.73 | 31–68 | [40,41] |
| cHgb | 12.6 ± 0.45 | 11.1 ± 0.25 * | 11.8 ± 0.34 | 12.0 ± 0.21 # | 11.9 ± 0.62 | 12.2 ± 0.43 # | 11.9 ± 0.60 | 11.5–20 | [40,41] |
| BE (b) | −8.2 ± 0.61 | −13.2 ± 1.50 * | −15.7 ± 1.64 * | −14.1 ± 0.54 * | −13.4 ± 1.78 * | −10.3 ± 1.19 * | −14.3 ± 2.5 * | - | - |
| Glu | 215.2 ± 14.7 | 144.8 ± 18.2 * | 161.4 ± 24.52 * | 134.6 ± 14.3 * | 152.6 ± 13.4 * | 170.0 ± 25.91 * | 163.4 ± 24.86 * | 75–279 | [42,50] |
| Lac | 4.5 ± 0.16 | 8.6 ± 1.44 * | 10.6 ± 1.25 * | 10.8 ± 1.30 * | 9.9 ± 0.89 * | 8.5 ± 0.65 * | 10.7 ± 1.88 * | 2.5–4.6 | [46,51] |
| BUN | 19.0 ± 0.37 | 15.6 ± 1.33 * | 15.0 ± 0.89 * | 16.0 ± 1.10 * | 15.8 ± 0.97 * | 16.4 ± 0.98 * | 16.0 ± 1.48 * | 7–28 | [40,41] |
| Clinical | Saline | Olive Oil | E. ciliata | Extract | Range | Ref. | |||
|---|---|---|---|---|---|---|---|---|---|
| Parameters | C1 | C2 | EC1 | EC2 | EC3 | EC4 | EC5 | ||
| 0.01 μL | 0.03 μL | 0.1 μL | 0.3 μL | 1 μL | |||||
| AST | 107.0 ± 26.0 | 204.0 ± 94.60 | 165.0 ± 25.0 * | 100.6 ± 5.0 | 133.4 ± 19.0 | 131.8 ± 14.90 | 165.0 ± 45.91 | 55–352 | [40,41] |
| ALT | 60.7 ± 35.40 | 42.5 ± 11.5 | 45.5 ± 12.5 | 51.0 ± 5.3 | 41.6 ± 5.0 | 39.6 ± 4.5 | 50.3 ± 16.5 | 41–131 | [40,41] |
| CREA | 0.44 ± 0.24 | 0.49 ± 0.19 | 0.711 ± 0.045 | 0.673 ± 0.050 | 0.706 ± 0.037 | 0.675 ± 0.009 | 0.787 ± 0.06 *# | 0.2–0.7 | [40,50] |
| TGL | 83.6 ± 10.73 | 138.9 ± 8.20 * | 136.5 ± 25.10 * | 132.6 ± 13.11 * | 120.2 ± 6.90 * | 123.3 ± 9.82 * | 132.8 ± 28.65 * | 42–155 | [41,42] |
| HDL | 35.9 ± 2.43 | 49.5 ± 16.02 | 36.3 ± 1.71 | 39.8 ± 1.36 | 38.9 ± 2.71 | 39.3 ± 2.43 | 39.4 ± 2.28 | 35–126 | [39,52] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mačianskienė, R.; Zigmantaitė, V.; Andriulė, I.; Pangonytė, D.; Sadauskienė, I.; Arandarčikaitė, O.; Stankevičius, A.; Grigas, J.; Pautienius, A.; Treinys, R.; et al. Acute and Sub-Chronic Intraperitoneal Toxicity Studies of the Elsholtzia ciliata Herbal Extract in Balb/c Mice. Pharmaceutics 2023, 15, 2417. https://doi.org/10.3390/pharmaceutics15102417
Mačianskienė R, Zigmantaitė V, Andriulė I, Pangonytė D, Sadauskienė I, Arandarčikaitė O, Stankevičius A, Grigas J, Pautienius A, Treinys R, et al. Acute and Sub-Chronic Intraperitoneal Toxicity Studies of the Elsholtzia ciliata Herbal Extract in Balb/c Mice. Pharmaceutics. 2023; 15(10):2417. https://doi.org/10.3390/pharmaceutics15102417
Chicago/Turabian StyleMačianskienė, Regina, Vilma Zigmantaitė, Inga Andriulė, Dalia Pangonytė, Ilona Sadauskienė, Odeta Arandarčikaitė, Arūnas Stankevičius, Juozas Grigas, Arnoldas Pautienius, Rimantas Treinys, and et al. 2023. "Acute and Sub-Chronic Intraperitoneal Toxicity Studies of the Elsholtzia ciliata Herbal Extract in Balb/c Mice" Pharmaceutics 15, no. 10: 2417. https://doi.org/10.3390/pharmaceutics15102417





