Simultaneous Prediction Method for Intestinal Absorption and Metabolism Using the Mini-Ussing Chamber System
Abstract
:1. Introduction
2. Gastrointestinal Fluid Volumes and Composition
2.1. Intestinal Fluid Volumes
2.2. Gastrointestinal pH, Buffering Ability and Osmolality
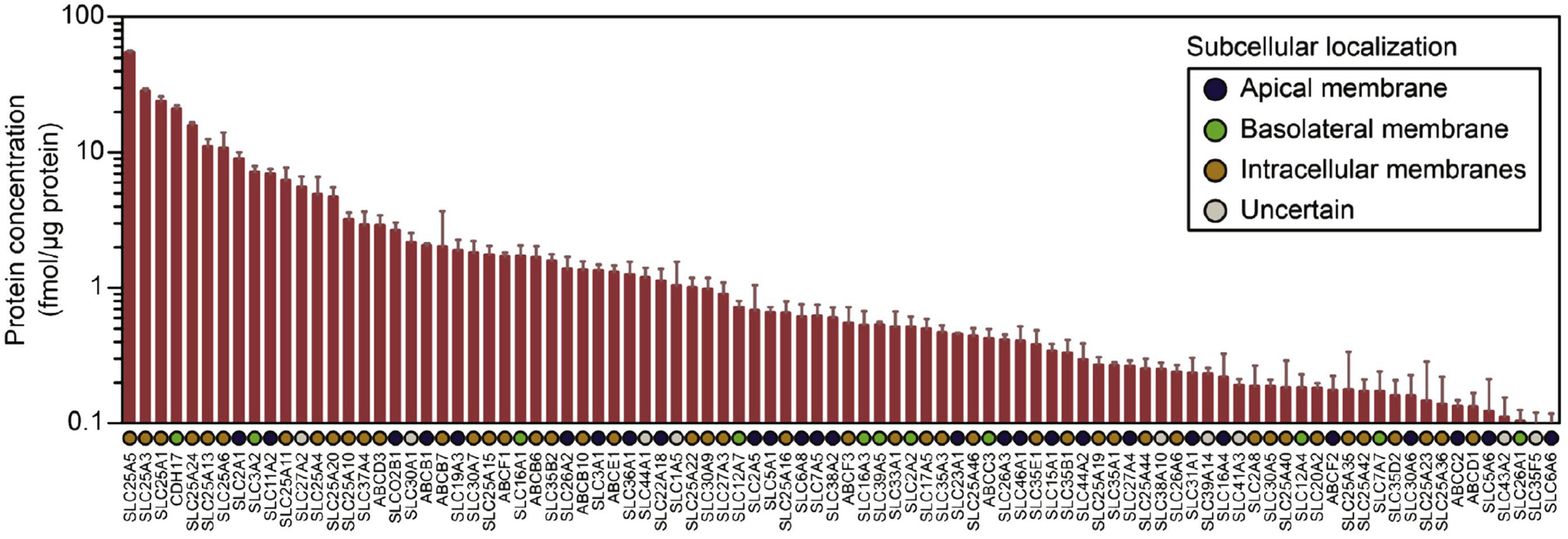
3. Intestinal Transporters and Epithelial Metabolism Enzymes
4. The Simultaneous Prediction of Human Intestinal Absorption and Metabolism Using the Transport Index (TI)
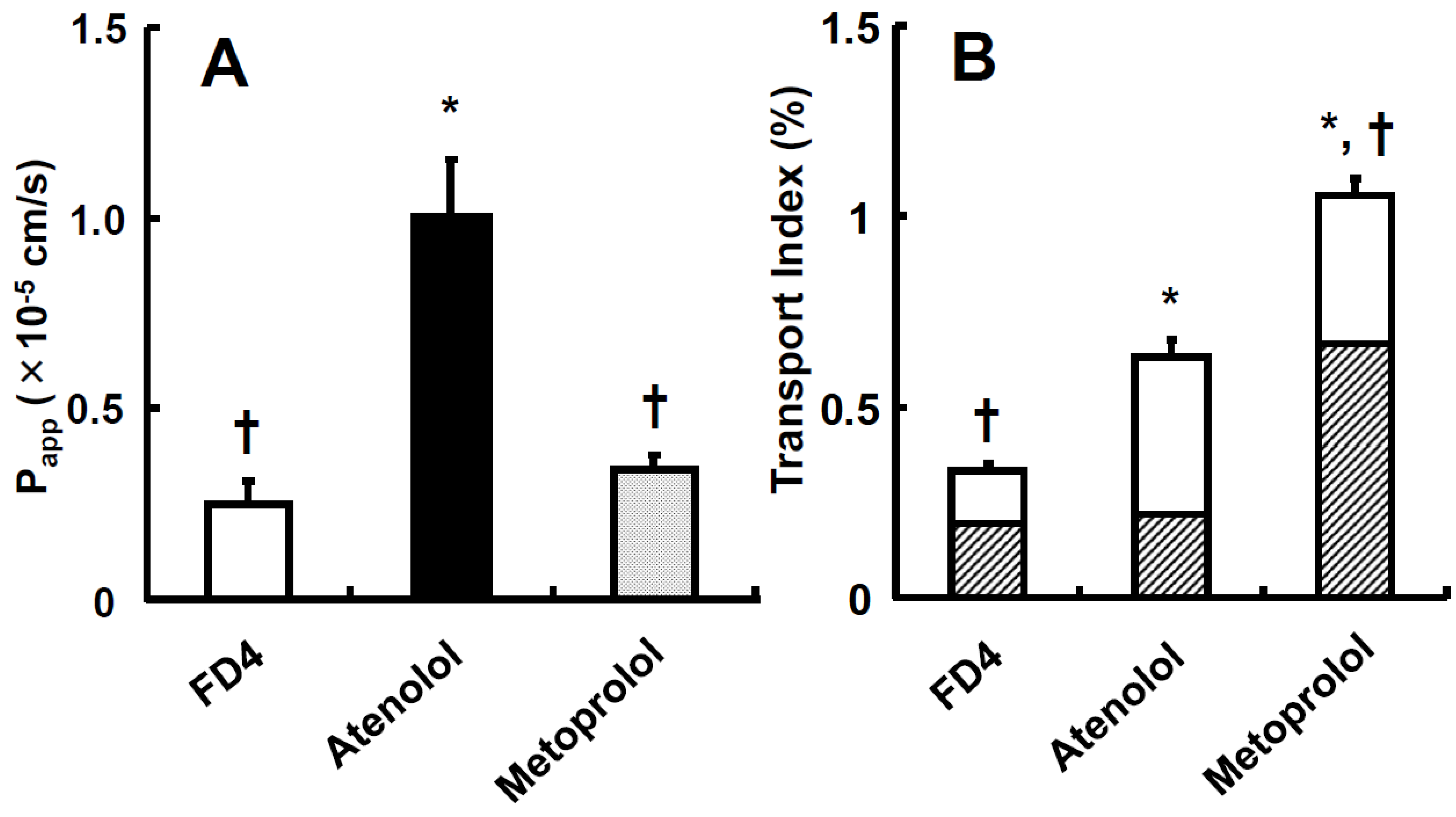
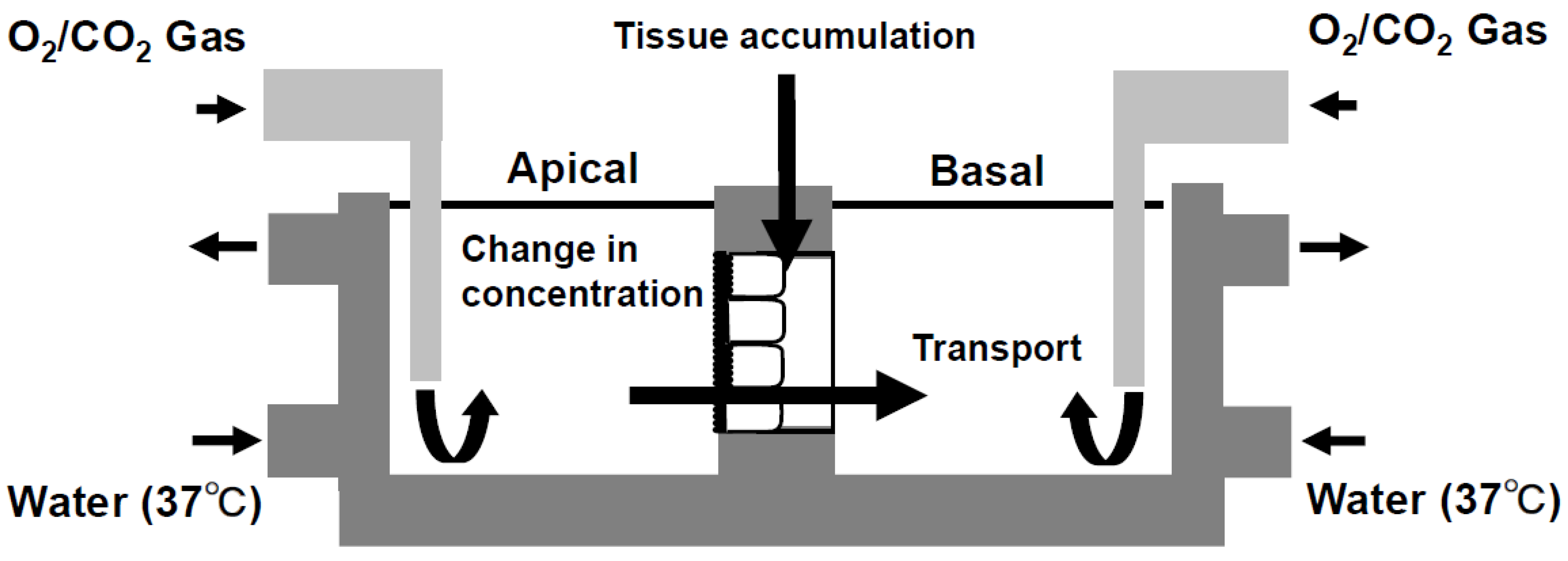
4.1. The Calculation of the Transport Index (TI)
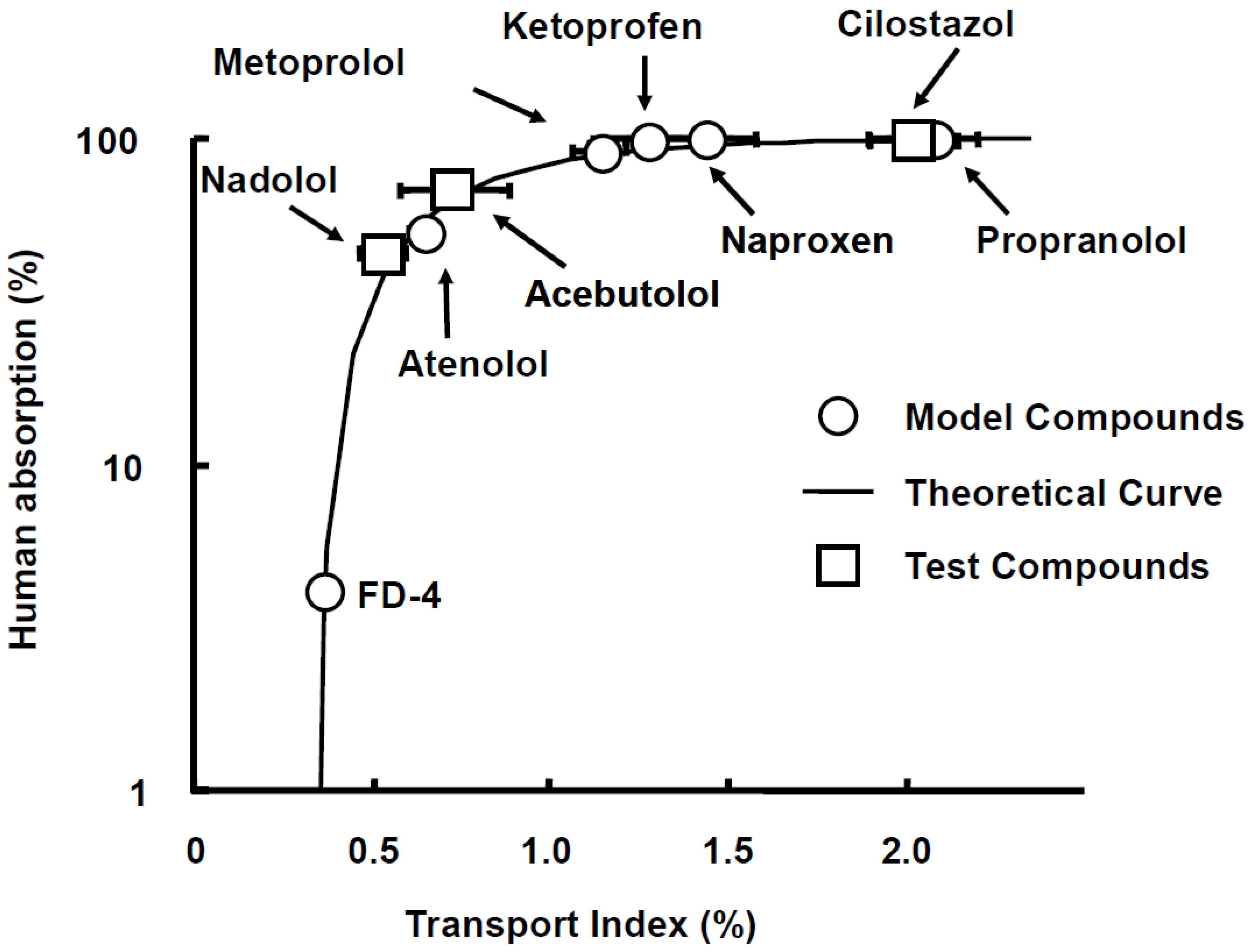
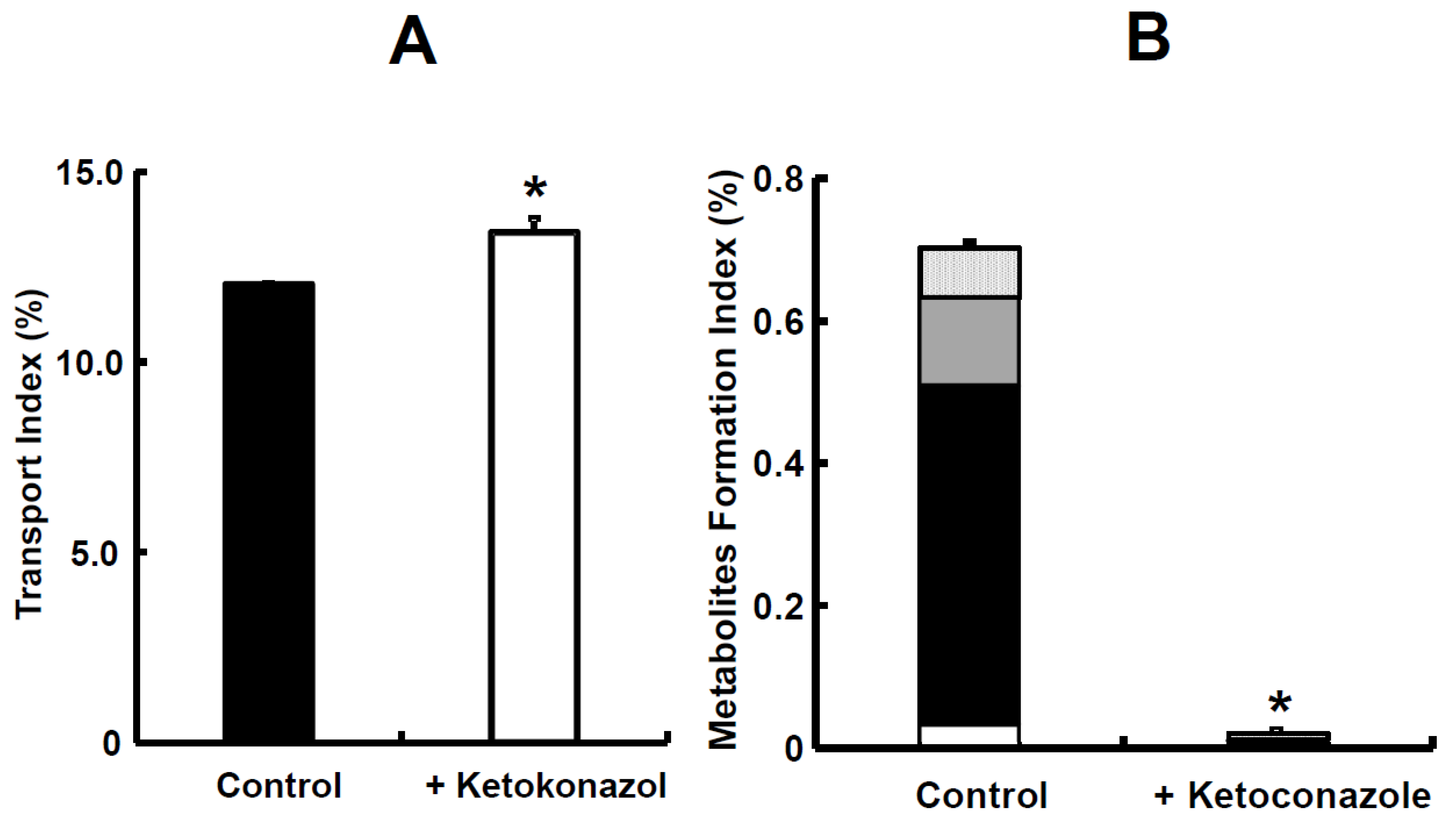
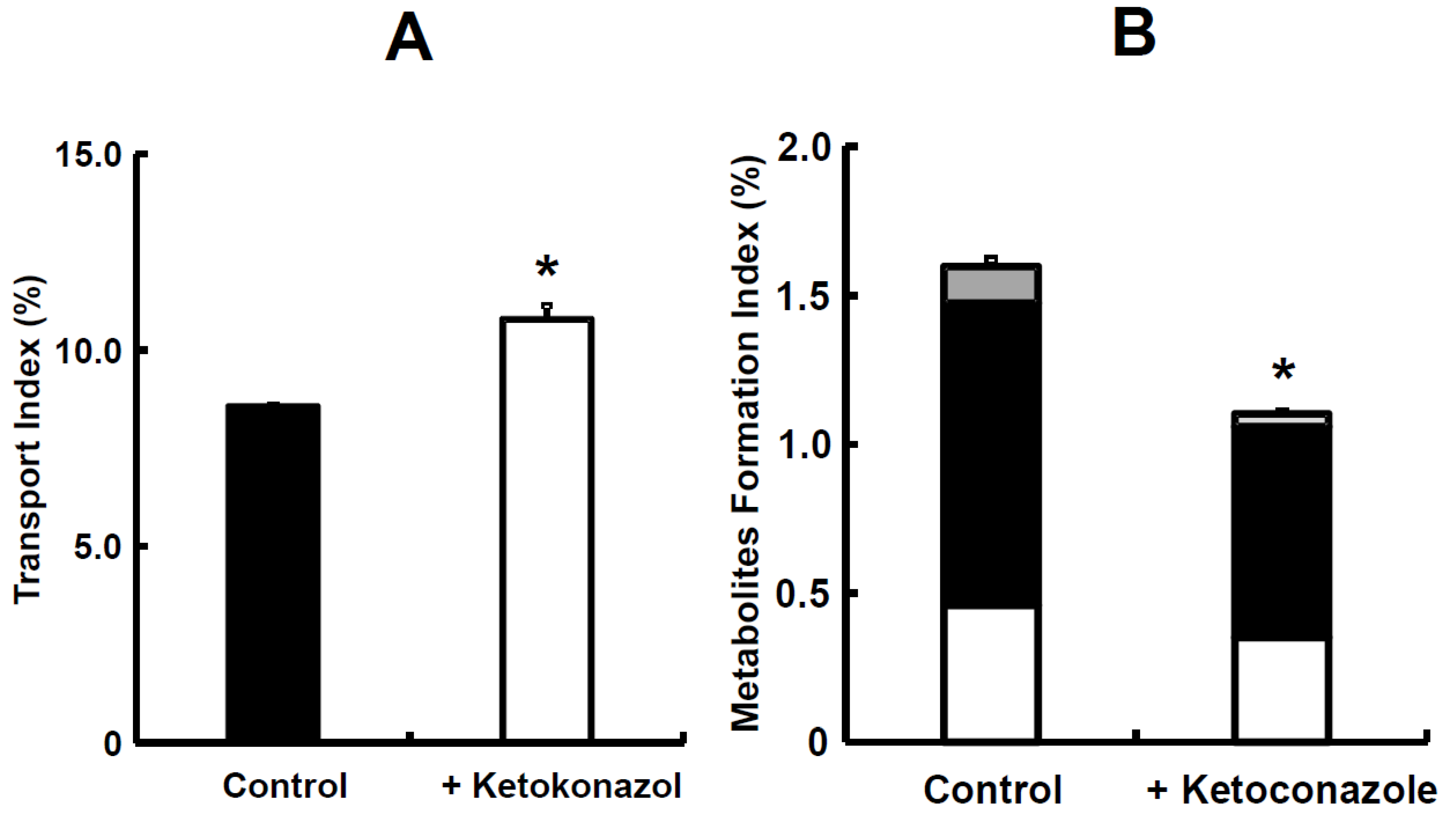
4.2. The Simultaneous Prediction of Intestinal Absorption and Metabolism Using the Transport Index (TI)
5. The Simultaneous Prediction of Intestinal Absorption and Metabolism Using Metabolites Formation Index (MFI)
5.1. The Calculation of Metabolites Formation Index (MFI)
5.2. The Simultaneous Prediction of Intestinal Absorption and Metabolism Using the Metabolites Formation Index (MFI)
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferraro, E.; Drago, J.Z.; Modi, S. Implementing antibody-drug conjugates (ADCs) in HER2-positive breast cancer: State of the art and future directions. Breast Cancer Res. 2021, 23, 84. [Google Scholar] [CrossRef]
- Keam, S.J. Trastuzumab Deruxtecan: First Approval. Drugs 2020, 80, 501–508. [Google Scholar] [CrossRef]
- Shastry, M.; Jacob, S.; Rugo, H.S.; Hamilton, E. Antibody-drug conjugates targeting TROP-2: Clinical development in metastatic breast cancer. Breast 2022, 66, 169–177. [Google Scholar] [CrossRef]
- Gorovits, B.; Baltrukonis, D.J.; Bhattacharya, I.; Birchler, M.A.; Finco, D.; Sikkema, D.; Vincent, M.S.; Lula, S.; Marshall, L.; Hickling, T.P. Immunoassay methods used in clinical studies for the detection of anti-drug antibodies to adalimumab and infliximab. Clin. Exp. Immunol. 2018, 192, 348–365. [Google Scholar] [CrossRef]
- Melsheimer, R.; Geldhof, A.; Apaolaza, I.; Schaible, T. Remicade® (infliximab): 20 years of contributions to science and medicine. Biol. Targets Ther. 2019, 13, 139–178. [Google Scholar] [CrossRef]
- Swain, S.M.; Shastry, M.; Hamilton, E. Targeting HER2-positive breast cancer: Advances and future directions. Nat. Rev. Drug Discov. 2023, 2, 101–126. [Google Scholar] [CrossRef]
- Li, X.; Craven, T.W.; Levine, P.M. Cyclic peptide screening methods for preclinical drug discovery. J. Med. Chem. 2022, 65, 11913–11926. [Google Scholar] [CrossRef]
- Lau, J.L.; Dunn, M.K. Therapeutic peptides: Historical perspectives, current development trends, and future directions. Bioorg. Med. Chem. 2018, 26, 2700–2707. [Google Scholar] [CrossRef]
- Kumar, S.; Mittal, A.; Babu, D.; Mittal, A. Herbal Medicines for diabetes management and its secondary complications. Curr. Diabetes Rev. 2021, 17, 437–456. [Google Scholar] [CrossRef]
- Pandey, M.; Choudhury, H.; Yi, C.X.; Mun, C.W.; Phing, G.K.; Rou, G.X.; Singh, B.J.K.A.A.J.; Jhee, A.N.A.; Chin, L.K.; Kesharwani, P.; et al. Recent updates on novel approaches in insulin drug delivery: A Review of Challenges and Pharmaceutical Implications. Curr. Drug Targets 2018, 19, 1782–1800. [Google Scholar] [CrossRef]
- Caffa, I.; Spagnolo, V.; Vernieri, C.; Valdemarin, F.; Becherini, P.; Wei, M.; Brandhorst, S.; Zucal, C.; Driehuis, E.; Ferrando, L.; et al. Fasting-mimicking diet and hormone therapy induce breast cancer regression. Nature 2020, 583, 620–624. [Google Scholar] [CrossRef]
- Fiedler, D.S. Pharmacokinetics, pharmacodynamics and drug-drug interactions of new anti-migraine drugs-lasmiditan, gepants, and calcitonin-gene-related peptide (CGRP) receptor monoclonal antibodies. Pharmaceutics 2020, 12, 1180. [Google Scholar] [CrossRef]
- Karsdal, M.A.; Henriksen, K.; Arnold, M.; Christiansen, C. Calcitonin: A drug of the past or for the future? Physiologic inhibition of bone resorption while sustaining osteoclast numbers improves bone quality. BioDrugs 2008, 22, 137–144. [Google Scholar] [CrossRef]
- Arnolds, S.; Heise, T. Inhaled insulin. Best Pract. Res. Clin. Endocrinol. Metab. 2007, 21, 555–571. [Google Scholar] [CrossRef]
- Artursson, P.; Karlsson, J. Correlation between oral drug absorption in humans and apparent drug permeability coefficient in human intestinal epithelial (caco-2) cells. Biochem. Biophys. Res. Commun. 1991, 175, 880–885. [Google Scholar] [CrossRef]
- Yee, S. In vitro permeability across Caco-2 cells (colonic) can predict in vivo (small intestinal) absorption in man-fact or myth. Pharm. Res. 1997, 14, 763–766. [Google Scholar] [CrossRef]
- Rozehnal, V.; Nakai, D.; Hoepner, U.; Fischer, T.; Kamiyama, E.; Takahashi, M.; Yasuda, S.; Mueller, J. Human small intestinal and colonic tissue mounted in the Ussing chamber as a tool for characterizing the intestinal absorption of drugs. Eur. J. Pharm. Sci. 2012, 46, 367–373. [Google Scholar] [CrossRef]
- Pratha, V.S.; Thompson, S.M.; Hogan, D.L.; Paulus, P.; Dreilinger, A.D.; Barrett, K.E.; Isenberg, J.I. Utility of endoscopic biopsy samples to quantitate human duodenal ion transport. J. Lab. Clin. Med. 1998, 132, 512–518. [Google Scholar] [CrossRef]
- Kisser, B.; Mangelsen, E.; Wingolf, C.; Partecke, L.I.; Heidecke, C.D.; Tannergren, C.; Oswald, S.; Keiser, M. The Ussing chamber assay to study drug metabolism and transport in the human intestine. Curr. Protoc. Pharmacol. 2017, 77, 7–17. [Google Scholar] [CrossRef]
- Haslam, I.S.; O’Reilly, D.A.; Sherlock, D.J.; Kauser, A.; Womack, C.; Coleman, T. Pancreatoduodenectomy as a source of human small intestine for Ussing chamber investigations and comparative studies with rat tissue. Biopharm. Drug Dispos. 2011, 32, 210–221. [Google Scholar] [CrossRef]
- Nilsson, M.; Brock, C.; Poulsen, J.L.; Bindslev, N.; Hansen, M.B.; Christrup, L.L.; Drewes, A.M. Short-term oxycodone treatment does not affect electrogenic ion transport in isolated mucosa from the human rectosigmoid colon. Scand. J. Gastroenterol. 2016, 51, 538–547. [Google Scholar] [CrossRef]
- Warners, M.J.; Vlieg-Boerstra, B.J.; Verheij, J.; van Hamersveld, P.H.P.; van Rhijn, B.D.; Van Ampting, M.T.J.; Harthoorn, L.F.; de Jonge, W.J.; Smout, A.J.P.M.; Bredenoord, A.J. Esophageal and small intestinal mucosal integrity in eosinophilic esophagitis and response to an elemental diet. Am. J. Gastroenterol. 2017, 112, 1061–1071. [Google Scholar] [CrossRef]
- Haslam, I.S.; Wright, J.A.; O’Reilly, D.A.; Sherlock, D.J.; Coleman, T.; Simmons, N.L. Intestinal ciprofloxacin efflux: The role of breast cancer resistance protein (ABCG2). Drug Metab. Dispos. 2011, 39, 2321–2328. [Google Scholar] [CrossRef]
- Lautenschläger, C.; Schmidt, C.; Lehr, C.M.; Fischer, D.; Stallmach, A. PEG-functionalized microparticles selectively target inflamed mucosa in inflammatory bowel disease. Eur. J. Pharm. Biopharm. 2013, 85, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Ussing, H.H.; Zerahn, K. Active transport of sodium as the source of electric current in the short-circuited isolated frog skin. Acta Physiol. Scand. 1951, 23, 110–127. [Google Scholar] [CrossRef]
- Ungell, A.L.; Nylander, S.; Bergstrand, S.; Sjoberg, A.; Lennernäs, H. Membrane transport of drugs in different regions of the intestinal tract of the rat. J. Pharm. Sci. 1998, 87, 360–366. [Google Scholar] [CrossRef]
- Ungell, A.L.; Abrahamsson, B. Biopharmaceutical Support in Candidate Drug Selection. In Pharmaceutical Performulation and Formulation: A Practical Guide from Candidate Drug Selection to Commercial Dosage Form; Gibson, M., Ed.; HIS Health Group: Engelwood, NJ, USA, 2001; pp. 97–143. [Google Scholar]
- Miyake, M.; Koga, T.; Kondo, S.; Yoda, N.; Emoto, C.; Mukai, T.; Toguchi, H. Prediction of drug intestinal absorption in human using the Ussing chamber system: A comparison of intestinal tissues from animals and humans. Eur. J. Pharm. Sci. 2016, 96, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Miyake, M.; Toguchi, H.; Nishibayashi, T.; Higaki, K.; Sugita, A.; Koganei, K.; Kamada, N.; Kitazume, T.M.; Hisamatsu, T.; Sato, T.; et al. Establishment of novel prediction system of intestinal absorption in humans using human intestinal tissues. J. Pharm. Sci. 2013, 102, 2564–2571. [Google Scholar] [CrossRef]
- Ungell, A.L. Transport Studies Using Intestinal Tissue Ex-Vivo. In Cell Culture Models of Biological Barriers; In Vitro Test Systems for Drug Absorption and Delivery; Lehr, C.M., Ed.; Taylor & Francis: New York, NY, USA, 2002; pp. 164–188. [Google Scholar]
- Michiba, K.; Maeda, K.; Kurimori, K.; Enomoto, T.; Shimomura, O.; Takeuchi, T.; Nishiyama, H.; Oda, T.; Kusuhara, H. Characterization of the human intestinal drug transport with Ussing chamber system incorporating freshly isolated human jejunum. Drug Metab. Dispos. 2021, 49, 84–93. [Google Scholar] [CrossRef]
- Michiba, K.; Maeda, K.; Shimomura, O.; Miyazaki, Y.; Hashimoto, S.; Oda, T.; Kusuhara, H. Usefulness of human jejunal spheroid-derived differentiated intestinal epithelial cells for the prediction of intestinal drug absorption in humans. Drug Metab. Dispos. 2022, 50, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Miyake, M.; Kondo, S.; Koga, T.; Yoda, N.; Nakazato, S.; Emoto, C.; Mukai, T.; Toguchi, H. Evaluation of intestinal metabolism and absorption using the Ussing chamber system equipped with intestinal tissue from rats and dogs. Eur. J. Pharm. Biopharm. 2018, 122, 49–53. [Google Scholar] [CrossRef]
- Kondo, S.; Miyake, M. Simultaneous prediction of intestinal absorption and metabolism using the mini-Ussing chamber system. J. Pharm. Sci. 2019, 108, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Nakai, D.; Miyake, M.; Hashimoto, A. Comparison of the intestinal drug permeation and accumulation between normal human intestinal tissues and human intestinal tissues with ulcerative colitis. J. Pharm. Sci. 2020, 109, 1623–1626. [Google Scholar] [CrossRef] [PubMed]
- Nakai, D.; Miyake, M. The change of the electrophysiological parameters using human intestinal tissues from ulcerative colitis and Crohn’s disease. J. Pharmacol. Sci. 2022, 150, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Colliver, J.A.; Marrero, T.C.; Roush, J.R. Assessment of age- related acid aspiration risk factors in pediatric, adult, and geriatric patients. Anesth. Analg. 1985, 64, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Stillhart, C.; Asteriadis, A.; Bocharova, E.; Eksteen, G.; Harder, F.; Kusch, J.; Tzakri, T.; Augustijns, P.; Matthys, C.; Vertzoni, M.; et al. The impact of advanced age on gastrointestinal characteristics that are relevant to oral drug absorption: An AGePOP review. Eur. J. Pharm. Sci. 2023, 187, 106452. [Google Scholar] [CrossRef]
- Pedersen, P.B.; Vilmann, P.; Bar-Shalom, D.; Müllertz, A.; Baldursdottir, S. Characterization of fasted human gastric fluid for relevant rheological parameters and gastric lipase activities. Eur. J. Pharm. Biopharm. 2013, 85, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Dressman, J.B.; Berardi, R.R.; Dermentzoglou, L.C.; Russell, T.L.; Schmaltz, S.P.; Barnett, J.L.; Jarvenpaa, K.M. Upper gastrointestinal (GI) pH in young, healthy men and women. Pharm. Res. 1990, 7, 756–761. [Google Scholar] [CrossRef]
- Russell, T.L.; Berardi, R.R.; Barnett, J.L.; Dermentzoglou, L.C.; Jarvenpaa, K.M.; Schmaltz, S.P.; Dressman, J.B. Upper gastrointestinal pH in seventy-nine healthy, elderly, North American men and women. Pharm. Res. 1993, 10, 187–196. [Google Scholar] [CrossRef]
- Feldman, M.; Cryer, B.; Mcarthur, K.E.; Huet, B.A.; Lee, E. Effects of aging and gastritis on gastric acid and pepsin secretion in humans: A prospective study. Gastroenterology 1996, 110, 1043–1052. [Google Scholar] [CrossRef]
- Katelaris, P.H.; Seow, F.; Lin, B.P.; Napoli, J.; Ngu, M.C.; Jones, D.B. Effect of age, Helicobacter pylori infection, and gastritis with atrophy on serum gastrin and gastric acid secretion in healthy men. Gut 1993, 34, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Annaert, P.; Brouwers, J.; Bijnens, A.; Lammert, F.; Tack, J.; Augustijns, P. Ex vivo permeability experiments in excised rat intestinal tissue and in vitro solubility measurements in aspirated human intestinal fluids support age-dependent oral drug absorption. Eur. J. Pharm. Sci. 2010, 39, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Vertzoni, M.; Sulaiman, S.; Goumas, K.; Kersten, E.; Anlahr, J.; Muenster, U.; Reppas, C. Characteristics of contents of lower intestine in the 65–74 years of age range could impact the performance of safe and efficacious modified release products. J. Pharm. Sci. 2021, 110, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Reppas, C.; Karatza, E.; Goumas, C.; Markopoulos, C.; Vertzoni, M. Characterization of contents of distal ileum and cecum to which drugs/drug products are exposed during bioavailability/bioequivalence studies in healthy adults. Pharm. Res. 2015, 32, 3338–3349. [Google Scholar] [CrossRef] [PubMed]
- Diakidou, A.; Vertzoni, M.; Goumas, K.; Söderlind, E.; Abrahamsson, B.; Dressman, J.; Reppas, C. Characterization of the contents of ascending colon to which drugs are exposed after oral administration to healthy adults. Pharm. Res. 2009, 26, 2141–2151. [Google Scholar] [CrossRef] [PubMed]
- Müller, J.; Keiser, M.; Drozdzik, M.; Oswald, S. Expression, regulation and function of intestinal drug transporters: An update. Biol. Chem. 2017, 398, 175–192. [Google Scholar] [CrossRef] [PubMed]
- Meixner, E.; Goldmann, U.; Sedlyarov, V.; Scorzoni, S.; Rebsamen, M.; Girardi, E.; Superti-Furga, G. A substrate-based ontology for human solute carriers. Mol. Syst. Biol. 2020, 16, e9652. [Google Scholar] [CrossRef]
- Youhanna, S.; Lauschke, V.M. The past, present and future of intestinal in vitro cell systems for drug absorption studies. J. Pharm. Sci. 2021, 110, 50–65. [Google Scholar] [CrossRef]
- Pan, Y.; Omori, K.; Ali, I.; Tachikawa, M.; Terasaki, T.; Brouwer, K.L.R.; Nicolazzo, J.A. Altered expression of small intestinal drug transporters and hepatic metabolic enzymes in a mouse model of familial Alzheimer’s disease. Mol. Pharm. 2018, 15, 4073–4083. [Google Scholar] [CrossRef]
- Viennois, E.; Pujada, A.; Zen, J.; Merlin, D. Function, regulation, and pathophysiological relevance of the POT superfamily, specifically PepT1 in inflammatory bowel disease. Compr. Physiol. 2018, 8, 731–760. [Google Scholar]
- Phang-Lyn, S.; Llerena, V.A. Biochemistry, Biotransformation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Wegler, C.; Wiśniewski, J.R.; Robertsen, I.; Christensen, H.; Hertel, J.K.; Hjelmesaeth, J.; Jansson-Löfmark, R.; Åsberg, A.; Andersson, T.B.; Artursson, P. Drug Disposition Protein Quantification in Matched Human Jejunum and Liver from Donors With Obesity. Clin. Pharmacol. Ther. 2022, 111, 1142–1154. [Google Scholar] [CrossRef]
- Peters, S.A.; Jones, C.R.; Ungell, A.L.; Hatley, O.J. Predicting drug extraction in the human gut wall: Assessing contributions from drug metabolizing enzymes and transporter proteins using preclinical models. Clin. Pharmacokinet. 2016, 55, 673–696. [Google Scholar] [CrossRef]
- Lindell, M.; Karlsson, M.O.; Lennernäs, H.; Påhlman, L.; Lang, M.A. Variable expression of CYP and P-gp genes in the human small intestine. Eur. J. Clin. Investig. 2003, 33, 493–499. [Google Scholar] [CrossRef]
- Lown, K.S.; Mayo, R.R.; Leichtman, A.B.; Hsiao, H.L.; Turgeon, D.K.; Schmiedlin-Ren, P.; Brown, M.B.; Guo, W.; Rossi, S.J.; Benet, L.Z.; et al. Role of intestinal P-glycoprotein (mdr1) in interpatient variation in the oral bioavailability of cyclosporine. Clin. Pharmacol. Ther. 1997, 62, 248–260. [Google Scholar] [CrossRef]
- Larsen, U.L.; Hyldahl Olesen, L.; Guldborg Nyvold, C.; Eriksen, J.; Jakobsen, P.; Østergaard, M.; Autrup, H.; Andersen, V. Human intestinal P-glycoprotein activity estimated by the model substrate digoxin. Scand. J. Clin. Lab. Investig. 2007, 67, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Miki, Y.; Suzuki, T.; Tazawa, C.; Blumberg, B.; Sasano, H. Steroid and xenobiotic receptor (SXR), cytochrome P450 3A4 and multidrug resistance gene 1 in human adult and fetal tissues. Mol. Cell Endocrinol. 2005, 231, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Couto, N.; Al-Majdoub, Z.M.; Gibson, S.; Davies, P.J.; Achour, B.; Harwood, M.D.; Carlson, G.; Barber, J.; Rostami-Hodjegan, A.; Warhurst, G. Quantitative proteomics of clinically relevant drug-metabolizing enzymes and drug transporters and their intercorrelations in the human small intestine. Drug Metab. Dispos. 2020, 48, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, E.; Tachikawa, M.; Declèves, X.; Uchida, Y.; Bouillot, J.L.; Poitou, C.; Oppert, J.M.; Mouly, S.; Bergmann, J.F.; Terasaki, T.; et al. Quantitative atlas of cytochrome P450, UDP-glucuronosyltransferase, and transporter proteins in jejunum of morbidly obese subjects. Mol. Pharm. 2016, 13, 2631–2640. [Google Scholar] [CrossRef]
- Drozdzik, M.; Czekawy, I.; Oswald, S.; Drozdzik, A. Intestinal drug transporters in pathological states: An overview. Pharmacol. Rep. 2020, 72, 1173–1194. [Google Scholar] [CrossRef] [PubMed]
- Oswald, S.; Gröer, C.; Drozdzik, M.; Siegmund, W. Mass spectrometry-based targeted proteomics as a tool to elucidate the expression and function of intestinal drug transporters. AAPS J. 2013, 15, 1128–1140. [Google Scholar] [CrossRef] [PubMed]
- Prasad, B.; Unadkat, J.D. Optimized approaches for quantification of drug transporters in tissues and cells by MRM proteomics. AAPS J. 2014, 16, 634–648. [Google Scholar] [CrossRef] [PubMed]
- Kuroha, M.; Azumano, A.; Kuze, Y.; Shimoda, M.; Kokue, E. Effect of multiple dosing of ketoconazole on pharmacokinetics of midazolam, a cytochrome P-450 3A substrate in beagle dogs. Drug Metab. Dispos. 2002, 30, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Kotegawa, T.; Laurijssens, B.E.; Von Moltke, L.L.; Cotreau, M.M.; Perloff, M.D.; Venkatakrishnan, K.; Warrington, J.S.; Granda, B.W.; Harmatz, J.S.; Greenblatt, D.J. In vitro, pharmacokinetic, and pharmacodynamic interactions of ketoconazole and midazolam in the rat. J. Pharmacol. Exp. Ther. 2002, 302, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Kuroha, M.; Kuze, Y.; Shimoda, M.; Kokue, E. In vitro characterization of the inhibitory effects of ketoconazole on metabolic activities of cytochrome P-450 in canine hepatic microsomes. Am. J. Vet. Res. 2002, 63, 900–905. [Google Scholar] [CrossRef]
- Tian, D.D.; Leonowens, C.; Cox, E.J.; González-Pérez, V.; Frederick, K.S.; Scarlett, Y.V.; Fisher, M.B.; Paine, M.F. Indinavir increases midazolam N-glucuronidation in humans: Identification of an alternate CYP3A inhibitor using an in vitro to in vivo approach. Drug Metab. Dispos. 2019, 47, 724–731. [Google Scholar] [CrossRef]
- Brings, A.; Lehmann, M.L.; Foerster, K.I.; Burhenne, J.; Weiss, J.; Haefeli, W.E.; Czock, D. Perpetrator effects of ciclosporin (P-glycoprotein inhibitor) and its combination with fluconazole (CYP3A inhibitor) on the pharmacokinetics of rivaroxaban in healthy volunteers. Br. J. Clin. Pharmacol. 2019, 85, 1528–1537. [Google Scholar] [CrossRef]
- Greenblatt, D.J.; Harmatz, J.S. Ritonavir is the best alternative to ketoconazole as an index inhibitor of cytochrome P450-3A in drug-drug interaction studies. Br. J. Clin. Pharmacol. 2015, 80, 342–350. [Google Scholar] [CrossRef]
- Eriksson, O. Effects of standard diuretics and ortho-vanadate on sodium transport across isolated frog skin. Acta Physiol. Scand. 1984, 122, 249–260. [Google Scholar] [CrossRef]
- Larsen, R.; Mertz-Nielsen, A.; Hansen, M.B.; Poulsen, S.S.; Bindslev, N. Novel modified Ussing chamber for the study of absorption and secretion in human endoscopic biopsies. Acta Physiol. Scand. 2001, 173, 213–222. [Google Scholar] [CrossRef]
- Sjöberg, Å.; Lutz, M.; Tannergren, C.; Wingolf, C.; Borde, A.; Ungell, A.L. Comprehensive study on regional human intestinal permeability and prediction of fraction absorbed of drugs using the Ussing chamber technique. Eur. J. Pharm. Sci. 2013, 48, 166–180. [Google Scholar] [CrossRef]
- Patel, N.; Polak, S.; Jamei, M.; Rostami-Hodjegan, A.; Turne, D.B. Quantitative prediction of formulation-specific food effects and their population variability from in vitro data with the physiologically-based ADAM model: A case study using the BCS/BDDCS Class II drug nifedipine. Eur. J. Pharm. Sci. 2014, 16, 240–249. [Google Scholar] [CrossRef]
- Dorababu, M.; Nishimura, A.; Prabha, T.; Naruhashi, K.; Sugioka, N.; Takada, K.; Shibata, N. Effect of cyclosporine on drug transport and pharmacokinetics of nifedipine. Biomed. Pharmacother. 2009, 63, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Komura, H.; Iwaki, M. Species differences in in vitro and in vivo small intestinal metabolism of CYP3A substrates. J. Pharm. Sci. 2008, 97, 1775–1800. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, T.; Amano, N.; Kubo, Y.; Ono, M.; Kato, Y.; Fujita, H.; Kimura, Y.; Tsuji, A. Asymmetric intestinal first-pass metabolism causes minimal oral bioavailability of midazolam in cynomolgus monkey. Drug Metab. Dispos. 2007, 35, 1275–1284. [Google Scholar] [CrossRef] [PubMed]
- Yoshisue, K.; Nagayama, S.; Shindo, T.; Kawaguchi, Y. Effects of 5-fluorouracil on the drug-metabolizing enzymes of the small intestine and the consequent drug interaction with nifedipine in rats. J. Pharmacol. Exp. Ther. 2001, 297, 1166–1175. [Google Scholar] [PubMed]



| Population (Age Range, Number of Participants) | pH [Median (Range)] | Reference | |
|---|---|---|---|
| Fasted Condition 1 | Fed Condition 2 | ||
| Young adults (21–35 years; n = 24) | 1.7 (1.4–2.1) | 5.0 (4.3–5.4) | [40] |
| Young adults (20–39 years; n = 5) | 1.67 (1.24–5.95) | --- | [39] |
| Adults (40–59 years; n = 6) | 1.79 (1.29–4.52) | --- | [39] |
| Older adults (60–79 years; n = 8) | 2.12 (1.12–4.26) | --- | [39] |
| Older adults (≧65 years; n = 79) | 1.3 (1.1–1.6) | 4.9 (3.9–5.5) | [41] |
| Intestinal Segment | Population (Age Range, Number of Patients) | pH [Median (Range)] | Reference | |
|---|---|---|---|---|
| Fasted Condition 1 | Fed Condition 2 | |||
| Duodenum | Young adults (21–35 years; n = 24) Young adults (18–25 years; n = 8) | 6.1 (5.8–6.5) 6.84 (5.41–7.13) | 6.3 (6.0–6.7) | [40,44] |
| Older adults (65–83 years; n = 75) Older adults (62–72 years; n = 7) | 6.5 * (6.2–6.7) 6.71 (6.50–7.28) | 6.5 * (6.4–6.7) | [41,44] | |
| Distal ileum | Young adults (22–42 years; n = 12) | 8.0 (7.0–8.7) | 8.1 (7.3–8.4) | [46] |
| Older adults (65–70 years; n = 6 fasted, n = 4 fed) | 7.9 (7.2–8.6) | 6.7 * (6.1–7.9) | [45] | |
| Proximal colon | Young adults (19–28 years; n = 12) | 7.8 (6.4–8.4) | 6.0 (5.3–7.9) | [47] |
| Older adults (65–70 years; n = 8 fasted, n = 7 fed) | 6.4 ** (6.1–7.6) | 5.8 (5.7–6.4) | [45] | |
| Intestinal Segment | Age group (Age Range, Number of Patients) | Buffer Capacity [mmol/L/ΔpH] | Reference | |
|---|---|---|---|---|
| Fasted Condition 1 | Fed Condition 2 | |||
| Distal ileum | Young adults (22–42 years; n = 6 fasted, n = 7 fed) | 8.9 ± 3.6 | 15.2 ± 8.4 | [46] |
| Older adults (65–70 years; n = 2 fed) | No data | 20 and 35 * | [45] | |
| Proximal colon | Young adults (19–28 years; n = 12) | 21.5 ± 7.9 | 38.0 ± 16.0 | [47] |
| Older adults (65–70 years; n = 5) | 45.0 ± 17.0 ** | 56.0 ± 11.0 | [45] | |
| Intestinal Segment | Age Group (Age Range, Number of Subjects) | Osmolarity [mOsm/kg] | Reference | |
|---|---|---|---|---|
| Fasted Condition 1 | Fed Condition 2 | |||
| Duodenum | Young adults (18–25 years; n = 8) | 226 ± 35 | --- | [44] |
| Older adults (62–72 years; n = 7) | 215 ± 37 | --- | [44] | |
| Distal ileum | Young adults (22–42 years; n = 12) | 60 ± 50 | 252 ± 245 | [46] |
| Older adults (65–70 years; n = 5 fasted, n = 4 fed) | 128 ± 56 * | 193 ± 68 | [45] | |
| Proximal colon | Young adults (19–28 years; n = 11) | 81 ± 102 | 224 ± 125 | [47] |
| Older adults (65–70 years; n = 4 fasted, n = 7 fed) | 299 ± 49 * | 264 ± 76 | [45] | |
| Jejunum | ||
|---|---|---|
| Median (Min–Max) | n | |
| CYP3A4 | 13.4 (5–25.3) | 37 |
| CYP27A1 | 5.9 (4–10.2) | 37 |
| CYP4F2 | 5.4 (1.6–15.5) | 37 |
| CYP2S1 | 4.5 (1.6–7.5) | 37 |
| CYP2C9 | 1.5 (0.4–23.5) | 37 |
| CYP3A5 | 0.9 (0.1–3) | 37 |
| CYP20A1 | 0.8 (0.5–1.4) | 37 |
| CYP2C18 | 0.5 (0.2–6) | 35 |
| CYP4F12 | 0.5 (0.1–3.8) | 37 |
| CYP2D6; CYP2D7 | 0.4 (0.1–1.7) | 32 |
| CYP2J2 | 0.3 (0.1–0.9) | 37 |
| CYP1A1 | 0.2 (0–3.1) | 35 |
| CYP2C19 | 0.2 (0–0.6) | 34 |
| TAP2 (ABCB3) | 2.2 (0.7–4.3) | 37 |
| TAP1 (ABCB2) | 1.5 (0.8–3.4) | 37 |
| ABCB1 | 0.9 (0.3–1.9) | 37 |
| ABCG2 | 0.6 (0.3–1.5) | 37 |
| ABCC3 | 0.3 (0.1–0.5) | 37 |
| ABCC2 | 0.1 (0–0.2) | 37 |
| ABCC4 | 0.04 (0.003–0.1) | 37 |
| SLC15A1 | 0.9 (0.4–1.5) | 37 |
| SLC16A1 | 0.8 (0.3–1.7) | 37 |
| SLC19A3 | 0.04 (0.02–0.1) | 13 |
| SLC29A1 | 0.04 (0.02–0.1) | 17 |
| SLC51A | 0.2 (0.03–0.6) | 37 |
| SLC51B | 0.3 (0.2–0.6) | 21 |
| SLCO2B1 | 0.02 (0.01–0.2) | 14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kondo, S.; Miyake, M. Simultaneous Prediction Method for Intestinal Absorption and Metabolism Using the Mini-Ussing Chamber System. Pharmaceutics 2023, 15, 2732. https://doi.org/10.3390/pharmaceutics15122732
Kondo S, Miyake M. Simultaneous Prediction Method for Intestinal Absorption and Metabolism Using the Mini-Ussing Chamber System. Pharmaceutics. 2023; 15(12):2732. https://doi.org/10.3390/pharmaceutics15122732
Chicago/Turabian StyleKondo, Satoshi, and Masateru Miyake. 2023. "Simultaneous Prediction Method for Intestinal Absorption and Metabolism Using the Mini-Ussing Chamber System" Pharmaceutics 15, no. 12: 2732. https://doi.org/10.3390/pharmaceutics15122732





