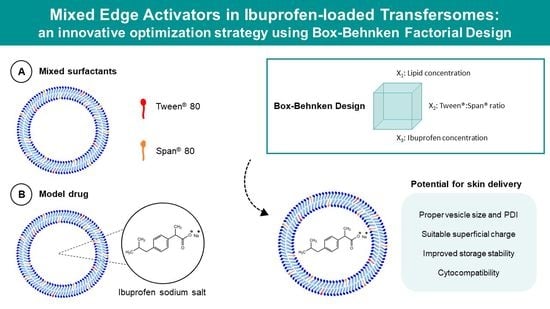
Mixed Edge Activators in Ibuprofen-Loaded Transfersomes: An Innovative Optimization Strategy Using Box–Behnken Factorial Design
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Solubility Studies
2.3. Preparation of Transfersomes and Liposomes
2.4. Optimization of IBU-Loaded Transfersomes
2.5. Characterization of Transfersomes and Liposomes
2.5.1. Vesicle Size, Polydispersity Index, and Zeta Potential
2.5.2. Encapsulation Efficiency and Loading Capacity
2.6. Stability Studies
2.7. Three-Dimensional Cell Culture
2.8. Viability Studies
2.9. Statistical Analysis
3. Results
3.1. Solubility of Ibuprofen Sodium Salt in Aqueous Media
3.2. Optimization of IBU-Loaded Transfersomes by a Box–Behnken Factorial Design
3.3. Transfersomes versus Liposomes: Characterization and Storage Stability
3.4. Transfersomes versus Liposomes: Viability Studies with HaCaT Spheroids
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Langan, S.M.; Irvine, A.D.; Weidinger, S. Atopic Dermatitis. Lancet 2020, 396, 345–360. [Google Scholar] [CrossRef]
- Greb, J.E.; Goldminz, A.M.; Elder, J.T.; Lebwohl, M.G.; Gladman, D.D.; Wu, J.J.; Mehta, N.N.; Finlay, A.Y.; Gottlieb, A.B. Psoriasis. Nat. Rev. Dis. Prim. 2016, 2, 16082. [Google Scholar] [CrossRef]
- Piccione, M.; Belloni Fortina, A.; Ferri, G.; Andolina, G.; Beretta, L.; Cividini, A.; De Marni, E.; Caroppo, F.; Citernesi, U.; Di Liddo, R. Xeroderma Pigmentosum: General Aspects and Management. J. Pers. Med. 2021, 11, 1146. [Google Scholar] [CrossRef]
- Lee, P.K.; Harwell, W.B.; Loven, K.H.; Phillips, T.J.; Whiting, D.A.; Andres, K.L.; Lee, J.H. Long-Term Clinical Outcomes Following Treatment of Actinic Keratosis with Imiquimod 5% Cream. Dermatol. Surg. 2006, 31, 659–664. [Google Scholar] [CrossRef]
- Cui, M.; Wiraja, C.; Chew, S.W.T.; Xu, C. Nanodelivery Systems for Topical Management of Skin Disorders. Mol. Pharm. 2021, 18, 491–505. [Google Scholar] [CrossRef]
- Hmingthansanga, V.; Singh, N.; Banerjee, S.; Manickam, S.; Velayutham, R.; Natesan, S. Improved Topical Drug Delivery: Role of Permeation Enhancers and Advanced Approaches. Pharmaceutics 2022, 14, 2818. [Google Scholar] [CrossRef]
- Roberts, M.S.; Cheruvu, H.S.; Mangion, S.E.; Alinaghi, A.; Benson, H.A.E.; Mohammed, Y.; Holmes, A.; van der Hoek, J.; Pastore, M.; Grice, J.E. Topical Drug Delivery: History, Percutaneous Absorption, and Product Development. Adv. Drug Deliv. Rev. 2021, 177, 113929. [Google Scholar] [CrossRef]
- N’Da, D. Prodrug Strategies for Enhancing the Percutaneous Absorption of Drugs. Molecules 2014, 19, 20780–20807. [Google Scholar] [CrossRef] [Green Version]
- Phatale, V.; Vaiphei, K.K.; Jha, S.; Patil, D.; Agrawal, M.; Alexander, A. Overcoming Skin Barriers through Advanced Transdermal Drug Delivery Approaches. J. Control Release 2022, 351, 361–380. [Google Scholar] [CrossRef]
- Ashtikar, M.; Nagarsekar, K.; Fahr, A. Transdermal Delivery from Liposomal Formulations–Evolution of the Technology over the Last Three Decades. J. Control Release 2016, 242, 126–140. [Google Scholar] [CrossRef]
- Sudhakar, K.; Fuloria, S.; Subramaniyan, V.; Sathasivam, K.V.; Azad, A.K.; Swain, S.S.; Sekar, M.; Karupiah, S.; Porwal, O.; Sahoo, A.; et al. Ultraflexible Liposome Nanocargo as a Dermal and Transdermal Drug Delivery System. Nanomaterials 2021, 11, 2557. [Google Scholar] [CrossRef]
- Mancuso, A.; Cristiano, M.C.; Fresta, M.; Paolino, D. The Challenge of Nanovesicles for Selective Topical Delivery for Acne Treatment: Enhancing Absorption Whilst Avoiding Toxicity. Int. J. Nanomed. 2020, 15, 9197–9210. [Google Scholar] [CrossRef]
- Mezei, M.; Gulasekharam, V. Liposomes-a Selective Drug Delivery System for the Topical Route of Administration I. Lotion Dosage Form. Life Sci. 1980, 26, 1473–1477. [Google Scholar] [CrossRef]
- Daraee, H.; Etemadi, A.; Kouhi, M.; Alimirzalu, S.; Akbarzadeh, A. Application of Liposomes in Medicine and Drug Delivery. Artif. Cells Nanomed. Biotechnol. 2016, 44, 381–391. [Google Scholar] [CrossRef]
- Opatha, S.A.T.; Titapiwatanakun, V.; Chutoprapat, R. Transfersomes: A Promising Nanoencapsulation Technique for Transdermal Drug Delivery. Pharmaceutics 2020, 12, 855. [Google Scholar] [CrossRef]
- Cevc, G.; Blume, G. Lipid Vesicles Penetrate into Intact Skin Owing to the Transdermal Osmotic Gradients and Hydration Force. Biochim. Biophys. Acta Biomembr. 1992, 1104, 226–232. [Google Scholar] [CrossRef]
- Cevc, G.; Schätzlein, A.; Blume, G. Transdermal Drug Carriers: Basic Properties, Optimization and Transfer Efficiency in the Case of Epicutaneously Applied Peptides. J. Control Release 1995, 36, 3–16. [Google Scholar] [CrossRef]
- Bnyan, R.; Khan, I.; Ehtezazi, T.; Saleem, I.; Gordon, S.; O’Neill, F.; Roberts, M. Surfactant Effects on Lipid-Based Vesicles Properties. J. Pharm. Sci. 2018, 107, 1237–1246. [Google Scholar] [CrossRef]
- Rajan, R.; Vasudevan, D.; Biju Mukund, V.; Jose, S. Transferosomes—A Vesicular Transdermal Delivery System for Enhanced Drug Permeation. J. Adv. Pharm. Technol. Res. 2011, 2, 138–143. [Google Scholar] [CrossRef]
- El Zaafarany, G.M.; Awad, G.A.S.; Holayel, S.M.; Mortada, N.D. Role of Edge Activators and Surface Charge in Developing Ultradeformable Vesicles with Enhanced Skin Delivery. Int. J. Pharm. 2010, 397, 164–172. [Google Scholar] [CrossRef]
- Moqejwa, T.; Marimuthu, T.; Kondiah, P.P.D.; Choonara, Y.E. Development of Stable Nano-Sized Transfersomes as a Rectal Colloid for Enhanced Delivery of Cannabidiol. Pharmaceutics 2022, 14, 703. [Google Scholar] [CrossRef]
- Guerreiro, Í.; Rodrigues, M.; Fernandes, A.S.; Rosado, C.; Pereira-Leite, C. Single versus Mixed Edge Activators in Caffeine-Loaded Transfersomes: Physicochemical and Cytotoxicity Assessment. Biomed. Biopharm. Res. 2021, 18, 85. [Google Scholar] [CrossRef]
- Fernández-García, R.; Lalatsa, A.; Statts, L.; Bolás-Fernández, F.; Ballesteros, M.P.; Serrano, D.R. Transferosomes as Nanocarriers for Drugs across the Skin: Quality by Design from Lab to Industrial Scale. Int. J. Pharm. 2020, 573, 118817. [Google Scholar] [CrossRef]
- Bezerra, M.A.; Santelli, R.E.; Oliveira, E.P.; Villar, L.S.; Escaleira, L.A. Response Surface Methodology (RSM) as a Tool for Optimization in Analytical Chemistry. Talanta 2008, 76, 965–977. [Google Scholar] [CrossRef]
- Magalhães, J.; Chaves, L.L.; Vieira, A.C.; Santos, S.G.; Pinheiro, M.; Reis, S. Optimization of Rifapentine-Loaded Lipid Nanoparticles Using a Quality-by-Design Strategy. Pharmaceutics 2020, 12, 75. [Google Scholar] [CrossRef] [Green Version]
- Jangdey, M.S.; Gupta, A.; Saraf, S.; Saraf, S. Development and Optimization of Apigenin-Loaded Transfersomal System for Skin Cancer Delivery: In Vitro Evaluation. Artif. Cells Nanomed. Biotechnol. 2017, 45, 1452–1462. [Google Scholar] [CrossRef] [Green Version]
- Tamilarasan, N.; Yasmin, B.M.; Anitha, P.; Umme, H.; Cheng, W.H.; Mohan, S.; Ramkanth, S.; Janakiraman, A.K. Box–Behnken Design: Optimization of Proanthocyanidin-Loaded Transferosomes as an Effective Therapeutic Approach for Osteoarthritis. Nanomaterials 2022, 12, 2954. [Google Scholar] [CrossRef]
- Júlio, A.; Costa, J.G.; Pereira-Leite, C.; Santos de Almeida, T. TransfersomILs: From Ionic Liquids to a New Class of Nanovesicular Systems. Nanomaterials 2021, 12, 7. [Google Scholar] [CrossRef]
- Vieira, J. Transfersomes as Delivery Systems of Ibuprofen for Transcutaneous Administration. Master’s Dissertation, Lusófona University, Lisbon, Portugal, 2021. [Google Scholar]
- Pereira-Leite, C.; Ventura, C. Optimization of Gallic Acid-Loaded Transfersomes Using a Box-Behnken Factorial Design. Biomed. Biopharm. Res. 2020, 17, 209–221. [Google Scholar] [CrossRef]
- Grit, M.; Crommelin, D.J.A. Chemical Stability of Liposomes: Implications for Their Physical Stability. Chem. Phys. Lipids 1993, 64, 3–18. [Google Scholar] [CrossRef]
- Duplessis, J.; Ramachandran, C.; Weiner, N.; Muller, D. The Influence of Lipid Composition and Lamellarity of Liposomes on the Physical Stability of Liposomes upon Storage. Int. J. Pharm. 1996, 127, 273–278. [Google Scholar] [CrossRef]
- Laureano, N.K.; Bernardi, L.; Bundrich, L.; Brand, L.M.; Visioli, F.; Lamers, M.L.; Rados, P.V. Development of an in Vitro Model to Study Tooth Cystogenesis. Int. Endod. J. 2019, 52, 1750–1757. [Google Scholar] [CrossRef]
- Brüningk, S.C.; Rivens, I.; Box, C.; Oelfke, U.; ter Haar, G. 3D Tumour Spheroids for the Prediction of the Effects of Radiation and Hyperthermia Treatments. Sci. Rep. 2020, 10, 1653. [Google Scholar] [CrossRef] [Green Version]
- Levis, K.A.; Lane, M.E.; Corrigan, O.I. Effect of Buffer Media Composition on the Solubility and Effective Permeability Coefficient of Ibuprofen. Int. J. Pharm. 2003, 253, 49–59. [Google Scholar] [CrossRef]
- Singh, B.; Kapil, R.; Nandi, M.; Ahuja, N. Developing Oral Drug Delivery Systems Using Formulation by Design: Vital Precepts, Retrospect and Prospects. Expert Opin. Drug Deliv. 2011, 8, 1341–1360. [Google Scholar] [CrossRef]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Hasanzadeh Davarani, F.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M. Impact of Particle Size and Polydispersity Index on the Clinical Applications of Lipidic Nanocarrier Systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef] [Green Version]
- Verma, D. Particle Size of Liposomes Influences Dermal Delivery of Substances into Skin. Int. J. Pharm. 2003, 258, 141–151. [Google Scholar] [CrossRef]
- Irfan, M.; Verma, S.; Ram, A. Preparation and Characterization of Ibuprofen Loaded Transferosome as a Novel Carrier for Transdermal Drug Delivery System. Asian J. Pharm. Clin. Res. 2012, 5, 162–165. [Google Scholar]
- Ahmed, T.A. Preparation of Transfersomes Encapsulating Sildenafil Aimed for Transdermal Drug Delivery: Plackett–Burman Design and Characterization. J. Liposome Res. 2015, 25, 1–10. [Google Scholar] [CrossRef]
- Kapoor, B.; Gupta, R.; Gulati, M.; Singh, S.K.; Khursheed, R.; Gupta, M. The Why, Where, Who, How, and What of the Vesicular Delivery Systems. Adv. Colloid Interface Sci. 2019, 271, 101985. [Google Scholar] [CrossRef]
- Boggara, M.B.; Mihailescu, M.; Krishnamoorti, R. Structural Association of Nonsteroidal Anti-Inflammatory Drugs with Lipid Membranes. J. Am. Chem. Soc. 2012, 134, 19669–19676. [Google Scholar] [CrossRef]
- Klicks, J.; von Molitor, E.; Ertongur-Fauth, T.; Rudolf, R.; Hafner, M. In Vitro Skin Three-Dimensional Models and Their Applications. J. Cell Biotechnol. 2017, 3, 21–39. [Google Scholar] [CrossRef] [Green Version]
- De Vuyst, E.; Salmon, M.; Evrard, C.; Lambert de Rouvroit, C.; Poumay, Y. Atopic Dermatitis Studies through In Vitro Models. Front. Med. 2017, 4. [Google Scholar] [CrossRef] [Green Version]
- Caddeo, C.; Manca, M.L.; Peris, J.E.; Usach, I.; Diez-Sales, O.; Matos, M.; Fernàndez-Busquets, X.; Fadda, A.M.; Manconi, M. Tocopherol-Loaded Transfersomes: In Vitro Antioxidant Activity and Efficacy in Skin Regeneration. Int. J. Pharm. 2018, 551, 34–41. [Google Scholar] [CrossRef]
- Asensio-Regalado, C.; Alonso-Salces, R.M.; Gallo, B.; Berrueta, L.A.; Era, B.; Pintus, F.; Caddeo, C. Tempranillo Grape Extract in Transfersomes: A Nanoproduct with Antioxidant Activity. Nanomaterials 2022, 12, 746. [Google Scholar] [CrossRef]
- Jiang, T.; Wang, T.; Li, T.; Ma, Y.; Shen, S.; He, B.; Mo, R. Enhanced Transdermal Drug Delivery by Transfersome-Embedded Oligopeptide Hydrogel for Topical Chemotherapy of Melanoma. ACS NANO 2018, 12, 9693–9701. [Google Scholar] [CrossRef]
- Demartis, S.; Anjani, Q.K.; Volpe-Zanutto, F.; Paredes, A.J.; Jahan, S.A.; Vora, L.K.; Donnelly, R.F.; Gavini, E. Trilayer Dissolving Polymeric Microneedle Array Loading Rose Bengal Transfersomes as a Novel Adjuvant in Early-Stage Cutaneous Melanoma Management. Int. J. Pharm. 2022, 627, 122217. [Google Scholar] [CrossRef]
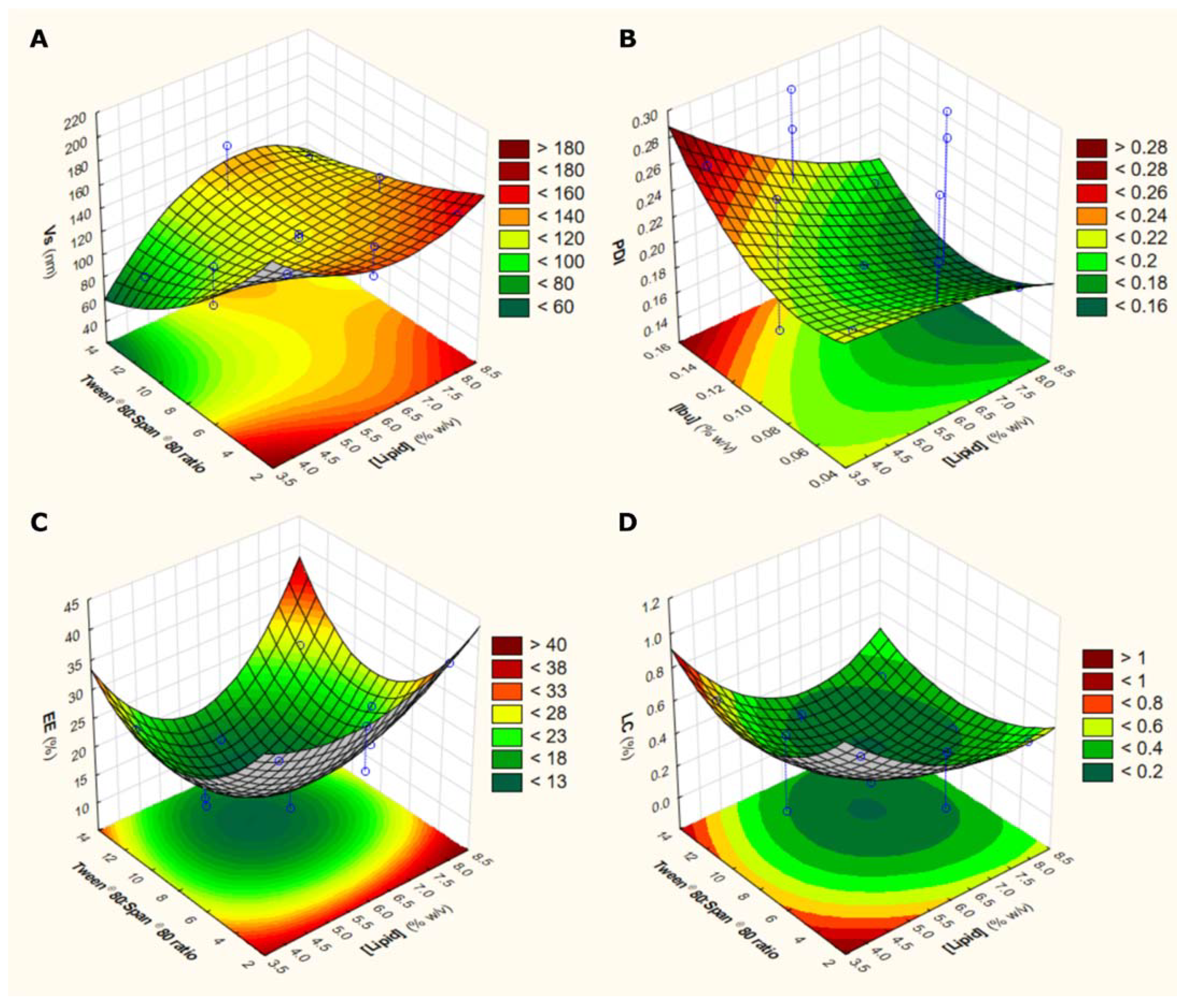


| Factors | Levels | ||
|---|---|---|---|
| −1 | 0 | 1 | |
| X1: Lipid concentration (% w/v) | 4 | 6 | 8 |
| X2: Tween® 80/Span® 80 ratio | 2.5:12.5 | 7.5:7.5 | 12.5:2.5 |
| X3: Ibuprofen concentration (% w/v) | 0.05 | 0.10 | 0.15 |
| Responses | Desirability | ||
| Low | Medium | High | |
| Y1: Vesicle size (nm) | 180 | 130 | 80 |
| Y2: Polydispersity index | 0.30 | 0.22 | 0.15 |
| Y3: Encapsulation efficiency (%) | 10 | 25 | 40 |
| Y4: Loading capacity (%) | 0.10 | 0.45 | 0.90 |
| Formulation # | Factors | Responses | |||||
|---|---|---|---|---|---|---|---|
| X1 | X2 | X3 | Y1 | Y2 | Y3 | Y4 | |
| 1 | 4 | (2.5:12.5) | 0.10 | 172 ± 36 | 0.17 ± 0.06 | 35 ± 1 | 0.88 ± 0.03 |
| 2 | 8 | (2.5:12.5) | 0.10 | 155 ± 1 | 0.26 ± 0.01 | 38 ± 2 | 0.50 ± 0.03 |
| 3 | 4 | (12.5:2.5) | 0.10 | 85 ± 1 | 0.27 ± 0.01 | 24 ± 2 | 0.63 ± 0.06 |
| 4 | 8 | (12.5:2.5) | 0.10 | 126 ± 5 | 0.28 ± 0.02 | 26 ± 3 | 0.34 ± 0.03 |
| 5 | 4 | (7.5:7.5) | 0.05 | 136 ± 7 | 0.21 ± 0.05 | 20 ± 6 | 0.26 ± 0.08 |
| 6 | 8 | (7.5:7.5) | 0.05 | 148 ± 1 | 0.18 ± 0.01 | 23 ± 2 | 0.15 ± 0.01 |
| 7 | 4 | (7.5:7.5) | 0.15 | 103 ± 3 | 0.26 ± 0.00 | 19 ± 1 | 0.71 ± 0.05 |
| 8 | 8 | (7.5:7.5) | 0.15 | 132 ± 3 | 0.19 ± 0.03 | 16 ± 2 | 0.29 ± 0.03 |
| 9 | 6 | (2.5:12.5) | 0.05 | 161 ± 6 | 0.23 ± 0.02 | 34 ± 2 | 0.34 ± 0.02 |
| 10 | 6 | (12.5:2.5) | 0.05 | 98 ± 2 | 0.28 ± 0.01 | 10 ± 3 | 0.08 ± 0.03 |
| 11 | 6 | (2.5:12.5) | 0.15 | 136 ± 2 | 0.26 ± 0.02 | 27 ± 2 | 0.67 ± 0.04 |
| 12 | 6 | (12.5:2.5) | 0.15 | 167 ± 6 | 0.29 ± 0.02 | 16 ± 1 | 0.32 ± 0.09 |
| 13 | 6 | (7.5:7.5) | 0.10 | 127 ± 3 | 0.19 ± 0.02 | 16 ± 2 | 0.26 ± 0.04 |
| 14 | 6 | (7.5:7.5) | 0.10 | 131 ± 3 | 0.18 ± 0.02 | 12 ± 1 | 0.19 ± 0.01 |
| 15 | 6 | (7.5:7.5) | 0.10 | 121 ± 1 | 0.19 ± 0.01 | 18 ± 1 | 0.30 ± 0.02 |
| Vs | PDI | EE | LC | |||||
|---|---|---|---|---|---|---|---|---|
| Coef. | p-Value | Coef. | p-Value | Coef. | p-Value | Coef. | p-Value | |
| Int. | 134.92 | 0.0001 | 0.240 | 0.0001 | 24.13 | 0.0015 | 0.431 | 0.0014 |
| X1 | 7.42 | 0.0584 | 0.008 | 0.0607 | 0.83 | 0.5692 | −0.156 | 0.0173 |
| X12 | 0.65 | 0.6708 | −0.001 | 0.6349 | −3.48 | 0.0551 | −0.084 | 0.0282 |
| X2 | −22.00 | 0.0072 | 0.027 | 0.0064 | −6.94 | 0.0296 | −0.119 | 0.0290 |
| X22 | −4.73 | 0.0689 | −0.028 | 0.0028 | −4.36 | 0.0363 | −0.084 | 0.0282 |
| X3 | −4.50 | 0.1385 | 0.013 | 0.0251 | −1.54 | 0.3343 | 0.146 | 0.0197 |
| X32 | −2.35 | 0.2141 | −0.011 | 0.0187 | 1.22 | 0.2893 | 0.033 | 0.1495 |
| X1X2 | 14.50 | 0.0288 | −0.020 | 0.0202 | −0.28 | 0.8822 | 0.023 | 0.5038 |
| X1X22 | 2.13 | 0.3548 | −0.025 | 0.0066 | −0.68 | 0.6193 | 0.018 | 0.4678 |
| X12X2 | 10.50 | 0.0275 | −0.005 | 0.1340 | −1.60 | 0.3015 | −0.025 | 0.3318 |
| X1X3 | 4.35 | 0.2333 | −0.010 | 0.0742 | −1.33 | 0.5038 | −0.078 | 0.1084 |
| X12X3 | 11.63 | 0.0226 | −0.002 | 0.3453 | 0.88 | 0.5291 | −0.003 | 0.9106 |
| X2X3 | 23.50 | 0.0113 | −0.005 | 0.2254 | 3.38 | 0.1757 | −0.023 | 0.5038 |
| R2 | 0.9943 | 0.9975 | 0.9794 | 0.9917 | ||||
| Optimized Formulation | Responses | Theoretical Responses 1 | Experimental Responses 2 |
|---|---|---|---|
| 4:(2.5:12.5):0.125 X1:(X2):X3 | Vs (nm) | 153.1 (130.0–176.3) | 166 ± 20 |
| PDI | 0.19 (0.16–0.21) | 0.23 ± 0.03 | |
| EE (%) | 32.6 (17.5–47.6) | 34 ± 9 | |
| LC (%) | 0.98 (0.73–1.24) | 1.1 ± 0.3 |
| Formulation | IBU (% w/v) | Tween® 80/Span® 80 ratio | Vs (nm) | PDI | ZP (mV) | EE (%) | LC (%) |
|---|---|---|---|---|---|---|---|
| [Unl-TR] | 0 | 2.5:12.5 | 151 ± 17 * | 0.25 ± 0.02 | −50 ± 3 | - | - |
| [IBU-TR] | 0.125 | 2.5:12.5 | 166 ± 20 ** | 0.23 ± 0.03 | −47 ± 6 | 34 ± 4 | 1.1 ± 0.3 |
| [Unl-Lip] | 0 | 0 | 106 ± 5 | 0.27 ± 0.01 | −44 ± 2 | - | - |
| [IBU-Lip] | 0.125 | 0 | 137 ± 20 | 0.29 ± 0.04 | −37 ± 8 | 30 ± 4 | 0.9 ± 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vieira, J.; Castelo, J.; Martins, M.; Saraiva, N.; Rosado, C.; Pereira-Leite, C. Mixed Edge Activators in Ibuprofen-Loaded Transfersomes: An Innovative Optimization Strategy Using Box–Behnken Factorial Design. Pharmaceutics 2023, 15, 1209. https://doi.org/10.3390/pharmaceutics15041209
Vieira J, Castelo J, Martins M, Saraiva N, Rosado C, Pereira-Leite C. Mixed Edge Activators in Ibuprofen-Loaded Transfersomes: An Innovative Optimization Strategy Using Box–Behnken Factorial Design. Pharmaceutics. 2023; 15(4):1209. https://doi.org/10.3390/pharmaceutics15041209
Chicago/Turabian StyleVieira, João, Jéssica Castelo, Marta Martins, Nuno Saraiva, Catarina Rosado, and Catarina Pereira-Leite. 2023. "Mixed Edge Activators in Ibuprofen-Loaded Transfersomes: An Innovative Optimization Strategy Using Box–Behnken Factorial Design" Pharmaceutics 15, no. 4: 1209. https://doi.org/10.3390/pharmaceutics15041209