Estimating Partnership Duration among MSM in Belgium—A Modeling Study
Abstract
1. Introduction
2. Methods
2.1. Data
2.2. Overview
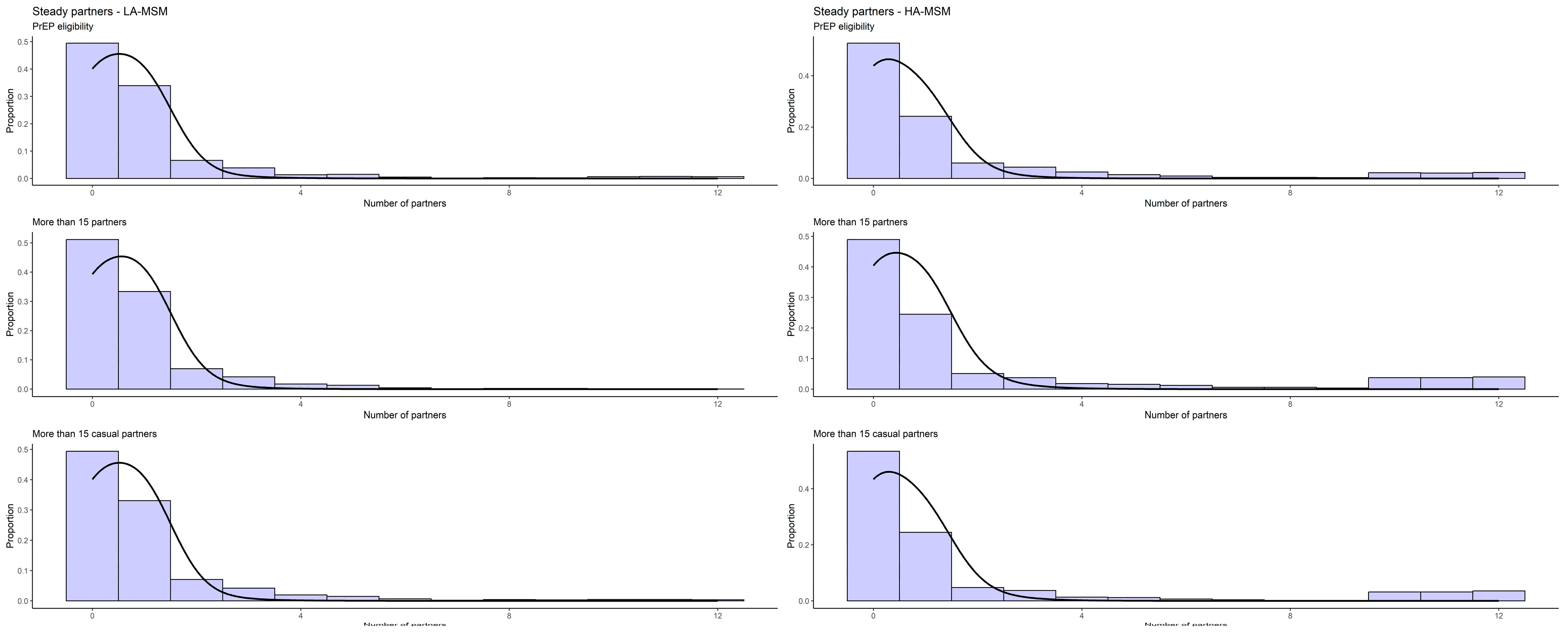
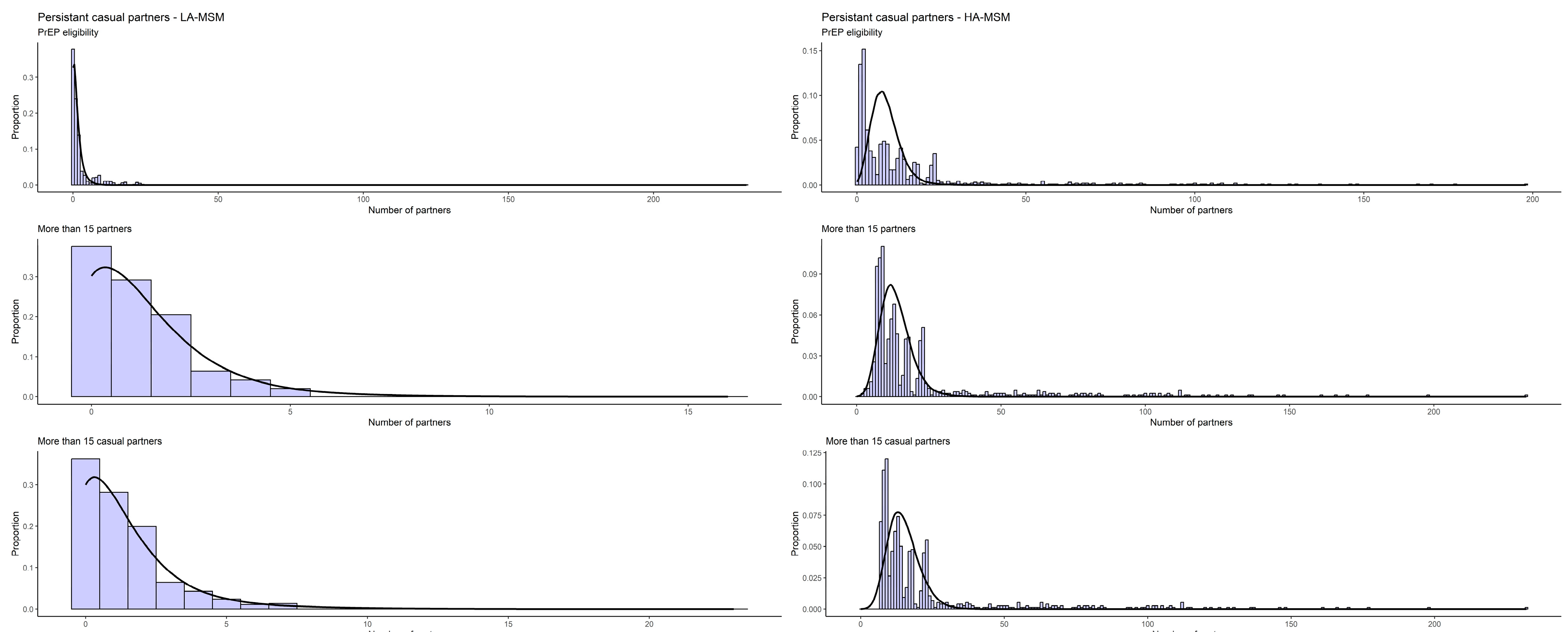
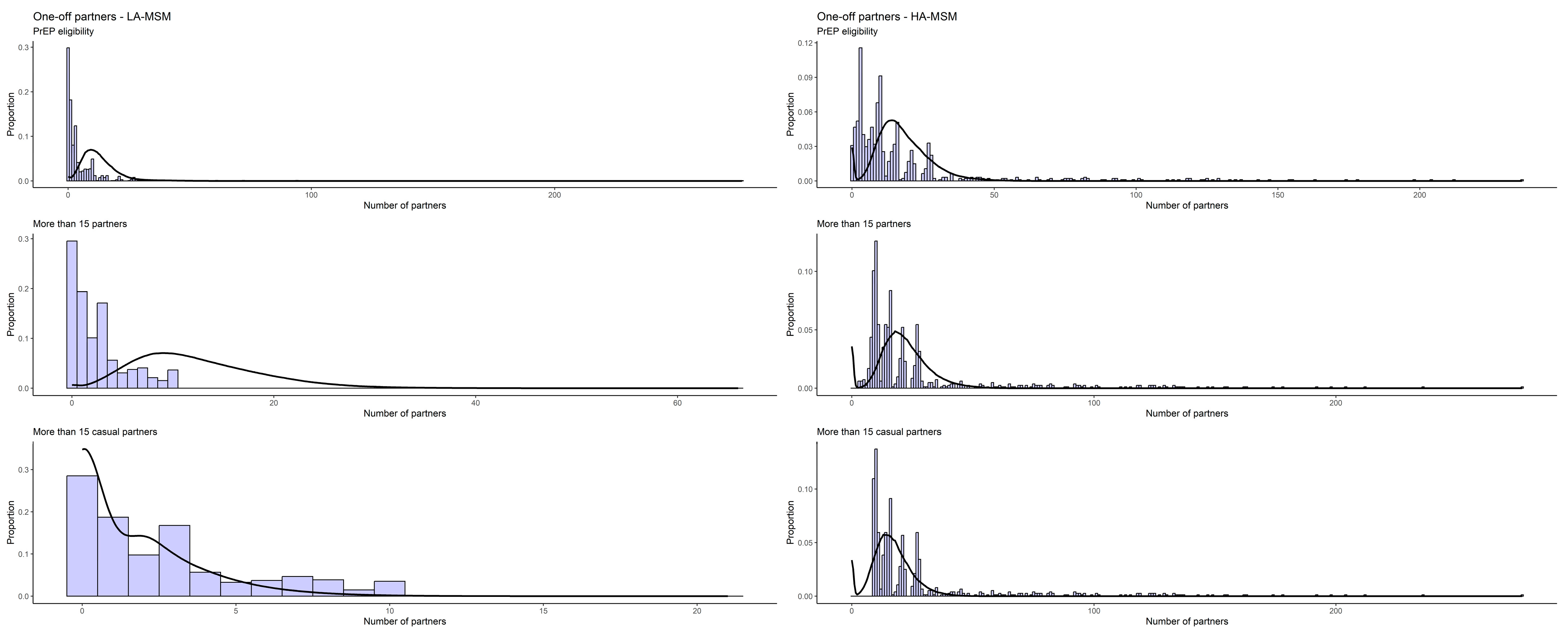
2.3. Partnership Formation and Homophily
2.4. Homophily
2.5. Sex Acts
2.6. Model Calibration
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Centre for Disease Prevention and Control (ECDC). Gonorrhoea. Annual Epidemiological Report for 2018; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2020; pp. 1–4. [Google Scholar]
- European Centre for Disease Prevention and Control (ECDC). Chlamydia Infection—Annual Epidemiological Report for 2019; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2022. [Google Scholar]
- Centre for Disease Prevention and Control (CDC). Sexually Transmitted Disease Surveillance 2019; Centre for Disease Prevention and Control (CDC): Atlanta, GA, USA, 2021. [Google Scholar]
- Centre for Disease Prevention and Control (CDC). Sexually Transmitted Disease Surveillance 2018; Centre for Disease Prevention and Control (CDC): Atlanta, GA, USA, 2019. [Google Scholar]
- Low, N.; Unemo, M.; Skov Jensen, J.; Breuer, J.; Stephenson, J.M. Molecular Diagnostics for Gonorrhoea: Implications for Antimicrobial Resistance and the Threat of Untreatable Gonorrhoea. PLoS Med. 2014, 11, e1001598. [Google Scholar] [CrossRef] [PubMed]
- Kirkcaldy, R.D.; Harvey, A.; Papp, J.R.; del Rio, C.; Soge, O.O.; Holmes, K.K.; Hook, E.W.; Kubin, G.; Riedel, S.; Zenilman, J.; et al. Neisseria gonorrhoeae Antimicrobial Susceptibility Surveillance—The Gonococcal Isolate Surveillance Project, 27 Sites, United States, 2014. MMWR. Surveill. Summ. 2016, 65, 1–19. [Google Scholar] [CrossRef]
- STD Prevention Conference [Press Release] New Warning Signs That Gonorrhea Treatment May Be Losing Effectiveness. 2016. Available online: https://www.cdc.gov/nchhstp/newsroom/2016/2016-std-prevention-conference-press-release.html (accessed on 8 December 2023).
- Buyze, J.; Vanden Berghe, W.; Hens, N.; Kenyon, C. Current Levels of Gonorrhoea Screening in MSM in Belgium May Have Little Effect on Prevalence: A Modelling Study. Epidemiol. Infect. 2018, 146, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Earnest, R.; Rönn, M.M.; Bellerose, M.; Gift, T.L.; Berruti, A.A.; Hsu, K.K.; Testa, C.; Zhu, L.; Malyuta, Y.; Menzies, N.A.; et al. Population-Level Benefits of Extragenital Gonorrhea Screening among Men Who Have Sex with Men: An Exploratory Modeling Analysis. Sex. Transm. Dis. 2020, 47, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Kretzschmar, M.; Van Duynhoven, Y.T.H.P.; Severijnen, A.J. Modeling Prevention Strategies for Gonorrhea and Chlamydia Using Stochastic Network Simulations. Am. J. Epidemiol. 1996, 144, 306–317. [Google Scholar] [CrossRef]
- Garnett, G.P.; Mertz, K.J.; Finelli, L.; Levine, W.C.; St Louis, M.E. The Transmission Dynamics of Gonorrhoea: Modelling the Reported Behaviour of Infected Patients from Newark, New Jersey. Philos. Trans. R. Soc. B Biol. Sci. 1999, 354, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Tuite, A.R.; Rönn, M.M.; Wolf, E.E.; Gift, T.L.; Chesson, H.W.; Berruti, A.; Galer, K.; Menzies, N.A.; Hsu, K.; Salomon, J.A. Estimated Impact of Screening on Gonorrhea Epidemiology in the United States: Insights from a Mathematical Model. Sex. Transm. Dis. 2018, 45, 713–722. [Google Scholar] [CrossRef]
- Jenness, S.M.; Weiss, K.M.; Goodreau, S.M.; Gift, T.; Chesson, H.; Hoover, K.W.; Smith, D.K.; Liu, A.Y.; Sullivan, P.S.; Rosenberg, E.S. Incidence of Gonorrhea and Chlamydia Following Human Immunodeficiency Virus Preexposure Prophylaxis among Men Who Have Sex with Men: A Modeling Study. Clin. Infect. Dis. 2017, 65, 712–718. [Google Scholar] [CrossRef]
- Yaesoubi, R.; Cohen, T.; Hsu, K.; Gift, T.L.; Chesson, H.; Salomon, J.A.; Grad, Y.H. Adaptive Guidelines for the Treatment of Gonorrhea to Increase the Effective Life Span of Antibiotics among Men Who Have Sex with Men in the United States: A Mathematical Modeling Study. PLoS Med. 2020, 17, e1003077. [Google Scholar] [CrossRef] [PubMed]
- Tuite, A.R.; Gift, T.L.; Chesson, H.W.; Hsu, K.; Salomon, J.A.; Grad, Y.H. Impact of Rapid Susceptibility Testing and Antibiotic Selection Strategy on the Emergence and Spread of Antibiotic Resistance in Gonorrhea. J. Infect. Dis. 2017, 216, 1141–1149. [Google Scholar] [CrossRef]
- Tsoumanis, A.; Van Dijck, C.; Hens, N.; Kenyon, C. Rethinking Screening Intensity in Terms of Reducing Prevalence or Increasing Selection Pressure for the Emergence of Resistant Gonorrhea: A Modeling Study of Men Who Have Sex with Men in Belgium. Open Forum Infect. Dis. 2023, 10, ofad165. [Google Scholar] [CrossRef] [PubMed]
- Bartelsman, M.; Vaughan, K.; van Rooijen, M.S.; de Vries, H.J.C.; Xiridou, M. Impact of Point-of-Care Management on the Transmission of Anogenital Gonococcal Infections among Men Who Have Sex with Men in Amsterdam: A Mathematical Modelling and Cost-Effectiveness Study. Sex. Transm. Infect. 2018, 94, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Duan, Q.; Carmody, C.; Donovan, B.; Guy, R.J.; Hui, B.B.; Kaldor, J.M.; Lahra, M.M.; Law, M.G.; Lewis, D.A.; Maley, M.; et al. Modelling Response Strategies for Controlling Gonorrhoea Outbreaks in Men Who Have Sex with Men in Australia. PLoS Comput. Biol. 2021, 17, e1009385. [Google Scholar] [CrossRef] [PubMed]
- Escobar, E.; Durgham, R.; Dammann, O.; Stopka, T. Agent-Based Computational Model of the Prevalence of Gonococcal Infections after the Implementation of HIV Pre-Exposure Prophylaxis Guidelines. Online J. Public Health Inform. 2015, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Fingerhuth, S.M.; Bonhoeffer, S.; Low, N.; Althaus, C.L. Antibiotic-Resistant Neisseria gonorrhoeae Spread Faster with More Treatment, Not More Sexual Partners. PLoS Pathog. 2016, 12, e1005611. [Google Scholar] [CrossRef]
- Fingerhuth, S.M.; Low, N.; Bonhoeffer, S.; Althaus, C.L. Detection of Antibiotic Resistance Is Essential for Gonorrhoea Point-of-Care Testing: A Mathematical Modelling Study. BMC Med. 2017, 15, 142. [Google Scholar] [CrossRef] [PubMed]
- Hui, B.; Fairley, C.K.; Chen, M.; Grulich, A.; Hocking, J.; Prestage, G.; Walker, S.; Law, M.; Regan, D. Oral and Anal Sex Are Key to Sustaining Gonorrhoea at Endemic Levels in MSM Populations: A Mathematical Model. Sex. Transm. Infect. 2015, 91, 365–369. [Google Scholar] [CrossRef]
- Hui, B.B.; Whiley, D.M.; Donovan, B.; Law, M.G.; Regan, D.G. Identifying Factors That Lead to the Persistence of Imported Gonorrhoeae Strains: A Modelling Study. Sex. Transm. Infect. 2017, 93, 221–225. [Google Scholar] [CrossRef]
- Hui, B.B.; Padeniya, T.N.; Rebuli, N.; Gray, R.T.; Wood, J.G.; Donovan, B.; Duan, Q.; Guy, R.; Hocking, J.S.; Lahra, M.M.; et al. A Gonococcal Vaccine Has the Potential to Rapidly Reduce the Incidence of Neisseria gonorrhoeae Infection among Urban Men Who Have Sex with Men. J. Infect. Dis. 2022, 225, 983–993. [Google Scholar] [CrossRef]
- Jones, J.; Weiss, K.; Mermin, J.; Dietz, P.; Rosenberg, E.S.; Gift, T.L.; Chesson, H.; Sullivan, P.S.; Lyles, C.; Bernstein, K.T.; et al. Proportion of Incident Human Immunodeficiency Virus Cases among Men Who Have Sex with Men Attributable to Gonorrhea and Chlamydia: A Modeling Analysis. Sex. Transm. Dis. 2019, 46, 357–363. [Google Scholar] [CrossRef]
- Kasaie, P.; Schumacher, C.M.; Jennings, J.M.; Berry, S.A.; Tuddenham, S.A.; Shah, M.S.; Rosenberg, E.S.; Hoover, K.W.; Gift, T.L.; Chesson, H.; et al. Gonorrhoea and Chlamydia Diagnosis as an Entry Point for HIV Pre-Exposure Prophylaxis: A Modelling Study. BMJ Open 2019, 9, e023453. [Google Scholar] [CrossRef]
- Reichert, E.; Grad, Y.H. Resistance and Prevalence Implications of Doxycycline Post-Exposure Prophylaxis for Gonorrhea Prevention in Men Who Have Sex with Men: A Modeling Study. medRxiv 2023. [Google Scholar] [CrossRef] [PubMed]
- Reichert, E.; Yaesoubi, R.; Rönn, M.M.; Gift, T.L.; Salomon, J.A.; Grad, Y.H. Resistance-Minimising Strategies for Introducing a Novel Antibiotic for Gonorrhoea Treatment: A Mathematical Modelling Study. Lancet Microbe 2023, 4, e781–e789. [Google Scholar] [CrossRef] [PubMed]
- Reitsema, M.; Hoek, A.J.V.; Van Der Loeff, M.S.; Hoornenborg, E.; Van Sighem, A.; Wallinga, J.; Van Benthem, B.; Xiridou, M. Preexposure Prophylaxis for Men Who Have Sex with Men in the Netherlands: Impact on HIV and Neisseria gonorrhoeae Transmission and Cost-Effectiveness. Aids 2020, 34, 621–630. [Google Scholar] [CrossRef]
- Reitsema, M.; Heijne, J.; Visser, M.; Van Sighem, A.; Schim Van Der Loeff, M.; Op De Coul, E.L.M.; Bezemer, D.; Wallinga, J.; Van Benthem, B.H.B.; Xiridou, M. Impact of Frequent Testing on the Transmission of HIV and N. Gonorrhoeae among Men Who Have Sex with Men: A Mathematical Modelling Study. Sex. Transm. Infect. 2020, 96, 361–367. [Google Scholar] [CrossRef]
- Riou, J.; Althaus, C.L.; Allen, H.; Cole, M.J.; Grad, Y.H.; Heijne, J.C.M.; Unemo, M.; Low, N. Projecting the Development of Antimicrobial Resistance in Neisseria gonorrhoeae from Antimicrobial Surveillance Data: A Mathematical Modelling Study. BMC Infect. Dis. 2023, 23, 252. [Google Scholar] [CrossRef]
- Spicknall, I.H.; Mayer, K.H.; Aral, S.O.; Romero-Severson, E.O. Assessing Uncertainty in an Anatomical Site-Specific Gonorrhea Transmission Model of Men Who Have Sex with Men. Sex. Transm. Dis. 2019, 46, 321–328. [Google Scholar] [CrossRef]
- Van Wifferen, F.; Hoornenborg, E.; Schim Van Der Loeff, M.F.; Heijne, J.; Van Hoek, A.J. Cost-Effectiveness of Two Screening Strategies for Chlamydia trachomatis and Neisseria gonorrhoeae as Part of the PrEP Programme in the Netherlands: A Modelling Study. Sex. Transm. Infect. 2021, 97, 607–612. [Google Scholar] [CrossRef]
- Voirin, N.; Allam, C.; Charre, C.; Fernandez, A.C.; Godinot, M.; Oria, F.; Pansu, A.; Chidiac, C.; Ne Salord, H.L.; Cotte, L. Optimizing Strategies for Chlamydia trachomatis and Neisseria gonorrhoeae Screening in Men Who Have Sex with Men: A Modeling Study. Clin. Infect. Dis. 2020, 70, 1966–1972. [Google Scholar] [CrossRef]
- Weiss, K.M.; Jones, J.S.; Anderson, E.J.; Gift, T.; Chesson, H.; Bernstein, K.; Workowski, K.; Tuite, A.; Rosenberg, E.S.; Sullivan, P.S.; et al. Optimizing Coverage vs Frequency for Sexually Transmitted Infection Screening of Men Who Have Sex with Men. Open Forum Infect. Dis. 2019, 6, ofz405. [Google Scholar] [CrossRef]
- Weiss, K.M.; Jones, J.S.; Katz, D.A.; Gift, T.L.; Bernstein, K.; Workowski, K.; Rosenberg, E.S.; Jenness, S.M. Epidemiological Impact of Expedited Partner Therapy for Men Who Have Sex with Men: A Modeling Study. Sex. Transm. Dis. 2019, 46, 697–705. [Google Scholar] [CrossRef]
- Whittles, L.K.; White, P.J.; Didelot, X. Estimating the Fitness Cost and Benefit of Cefixime Resistance in Neisseria gonorrhoeae to Inform Prescription Policy: A Modelling Study. PLoS Med. 2017, 14, e1002416. [Google Scholar] [CrossRef] [PubMed]
- Whittles, L.K.; White, P.J.; Didelot, X. Assessment of the Potential of Vaccination to Combat Antibiotic Resistance in Gonorrhea: A Modeling Analysis to Determine Preferred Product Characteristics. Clin. Infect. Dis. 2020, 71, 1912–1919. [Google Scholar] [CrossRef]
- Xiridou, M.; Heijne, J.; Adam, P.; de Coul, E.O.; Matser, A.; de Wit, J.; Wallinga, J.; van Benthem, B. How the Disruption in Sexually Transmitted Infection Care Due to the COVID-19 Pandemic Could Lead to Increased Sexually Transmitted Infection Transmission among Men Who Have Sex with Men in The Netherlands: A Mathematical Modeling Study. Sex. Transm. Dis. 2022, 49, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chow, E.P.F.; Ong, J.J.; Hoebe, C.J.P.A.; Zou, Z.; Hocking, J.S.; Fairley, C.K.; Zhang, L. Chlamydia trachomatis Transmission between the Oropharynx, Urethra and Anorectum in Men Who Have Sex with Men: A Mathematical Model. BMC Med. 2020, 18, 326. [Google Scholar] [CrossRef]
- Xu, X.; Chow, E.P.F.; Shen, M.; Zou, Z.; Wang, C.; Ong, J.J.; Fairley, C.K.; Zhang, L. Potential Effect of Antiseptic Mouthwash on the Incidence of Neisseria gonorrhoeae among Men Who Have Sex with Men: A Mathematical Modelling Study. BMJ Open 2021, 11, e052823. [Google Scholar] [CrossRef]
- Xu, X.; Chow, E.P.F.; Ong, J.J.; Hoebe, C.J.P.A.; Williamson, D.; Shen, M.; Kong, F.Y.S.; Hocking, J.S.; Fairley, C.K.; Zhang, L. Modelling the Contribution That Different Sexual Practices Involving the Oropharynx and Saliva Have on Neisseria gonorrhoeae Infections at Multiple Anatomical Sites in Men Who Have Sex with Men. Sex. Transm. Infect. 2021, 97, 183–189. [Google Scholar] [CrossRef]
- Zhang, L.; Regan, D.G.; Chow, E.P.F.; Gambhir, M.; Cornelisse, V.; Grulich, A.; Ong, J.; Lewis, D.A.; Hocking, J.; Fairley, C.K. Neisseria gonorrhoeae Transmission among Men Who Have Sex with Men: An Anatomical Site-Specific Mathematical Model Evaluating the Potential Preventive Impact of Mouthwash. Sex. Transm. Dis. 2017, 44, 586–592. [Google Scholar] [CrossRef]
- Zwart, J.M.; Mangen, M.J.J.; Bartelsman, M.; Van Rooijen, M.S.; De Vries, H.J.C.; Xiridou, M. Microscopic Examination of Gram-Stained Smears for Anogenital Gonorrhoea in Men Who Have Sex with Men Is Cost-Effective: Evidence from a Modelling Study. Sex. Transm. Infect. 2019, 95, 13–20. [Google Scholar] [CrossRef]
- Zienkiewicz, A.K.; Verschueren Van Rees, N.; Homer, M.; Ong, J.J.; Christensen, H.; Hill, D.; Looker, K.J.; Horner, P.; Hughes, G.; Turner, K.M.E. Agent-Based Modelling Study of Antimicrobial-Resistant Neisseria gonorrhoeae Transmission in Men Who Have Sex with Men: Towards Individualised Diagnosis and Treatment. Sex. Health 2019, 16, 514–522. [Google Scholar] [CrossRef]
- Barbee, L.A.; Khosropour, C.M.; Soge, O.O.; Hughes, J.P.; Haglund, M.; Yeung, W.; Golden, M.R. The Natural History of Rectal Gonococcal and Chlamydial Infections: The ExGen Study. Clin. Infect. Dis. 2022, 74, 1549–1556. [Google Scholar] [CrossRef]
- Barbee, L.A.; Soge, O.O.; Khosropour, C.M.; Haglund, M.; Yeung, W.; Hughes, J.; Golden, M.R. The Duration of Pharyngeal Gonorrhea: A Natural History Study. Clin. Infect. Dis. 2021, 73, 575–582. [Google Scholar] [CrossRef]
- Krivitsky, P.N.; Handcock, M.S.; Morris, M. Adjusting for Network Size and Composition Effects in Exponential-Family Random Graph Models. Stat. Methodol. 2011, 8, 319–339. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Lu, X. Network Evolution of a Large Online MSM Dating Community: 2005–2018. Int. J. Environ. Res. Public Health 2019, 16, 4322. [Google Scholar] [CrossRef]
- Currarini, S.; Vega Redondo, F. A Simple Model of Homophily in Social Networks; Department of Economics, University of Leicester: Leicester, UK, 2016. [Google Scholar]
- Cai, M.; Huang, G.; Kretzschmar, M.E.; Chen, X.; Lu, X. Extremely Low Reciprocity and Strong Homophily in the World Largest MSM Social Network. IEEE Trans. Netw. Sci. Eng. 2021, 8, 2279–2287. [Google Scholar] [CrossRef]
- Murase, Y.; Jo, H.H.; Török, J.; Kertész, J.; Kaski, K. Structural Transition in Social Networks: The Role of Homophily. Sci. Rep. 2019, 9, 4310. [Google Scholar] [CrossRef]
- Sullivan, P.S.; Rosenberg, E.S.; Sanchez, T.H.; Kelley, C.F.; Luisi, N.; Cooper, H.L.; Diclemente, R.J.; Wingood, G.M.; Frew, P.M.; Salazar, L.F.; et al. Explaining Racial Disparities in HIV Incidence in Black and White Men Who Have Sex with Men in Atlanta, GA: A Prospective Observational Cohort Study. Ann. Epidemiol. 2015, 25, 445–454. [Google Scholar] [CrossRef]
- Hernández-Romieu, A.C.; Sullivan, P.S.; Rothenberg, R.; Grey, J.; Luisi, N.; Kelley, C.F.; Rosenberg, E.S. Heterogeneity of HIV Prevalence among the Sexual Networks of Black and White Men Who Have Sex with Men in Atlanta. Sex. Transm. Dis. 2015, 42, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Prestage, G.P.; Hudson, J.; Bradley, J.; Down, I.; Sutherland, R.; Corrigan, N.; Grulich, A.E. TOMS—Three or More Study; National Centre in HIV Epidemiology and Clinical Research, University of New South Wales: Sydney, Australia, 2008. [Google Scholar]
- Heijman, T.; Geskus, R.B.; Davidovich, U.; Coutinho, R.A.; Prins, M.; Stolte, I.G. Less Decrease in Risk Behaviour from Pre-HIV to Post-HIV Seroconversion among MSM in the Combination Antiretroviral Therapy Era Compared with the Pre-Combination Antiretroviral Therapy Era. Aids 2012, 26, 489–495. [Google Scholar] [CrossRef]
- Heymans, R.; Matser, A.A.; Bruisten, S.M.; Heijman, T.; Geskus, R.B.; Speksnijder, A.G.C.L.; Davidovich, U.; De Vries, H.J.C.; Coutinho, R.A.; Van Der Loeff, M.F.S. Distinct Neisseria gonorrhoeae Transmission Networks among Men Who Have Sex with Men in Amsterdam, the Netherlands. J. Infect. Dis. 2012, 206, 596–605. [Google Scholar] [CrossRef]
- Weatherburn, P.; Hickson, F.; Reid, D.S.; Marcus, U.; Schmidt, A.J. European Men-Who-Have-Sex-with-Men Internet Survey (EMIS-2017): Design and Methods. Sex. Res. Soc. Policy 2020, 17, 543–557. [Google Scholar] [CrossRef]
- Krivitsky, P.N.; Handcock, M.S. A Separable Model for Dynamic Networks. J. R. Stat. Soc. Ser. B Stat. Methodol. 2014, 76, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.R.; Handcock, M.S.; Butts, C.T.; Goodreau, S.M.; Morris, M. Ergm: A Package to Fit, Simulate and Diagnose Exponential-Family Models for Networks. J. Stat. Softw. 2008, 24, nihpa54860. [Google Scholar] [CrossRef]
- Goodreau, S.M.; Carnegie, N.B.; Vittinghoff, E.; Lama, J.R.; Sanchez, J.; Grinsztejn, B.; Koblin, B.A.; Mayer, K.H.; Buchbinder, S.P. What Drives the US and Peruvian HIV Epidemics in Men Who Have Sex with Men (MSM)? PLoS ONE 2012, 7, e50522. [Google Scholar] [CrossRef]
- Hansson, D.; Strömdahl, S.; Leung, K.Y.; Britton, T. Introducing Pre-Exposure Prophylaxis to Prevent HIV Acquisition among Men Who Have Sex with Men in Sweden: Insights from a Mathematical Pair Formation Model. BMJ Open 2020, 10, e033852. [Google Scholar] [CrossRef]
- Cox, A.P.; Foss, A.M.; Shafer, L.A.; Nsubuga, R.N.; Vickerman, P.; Hayes, R.J.; Watts, C.; White, R.G. Attaining Realistic and Substantial Reductions in HIV Incidence: Model Projections of Combining Microbicide and Male Circumcision Interventions in Rural Uganda. Sex. Transm. Infect. 2011, 87, 635–639. [Google Scholar] [CrossRef]
- Buffel, V.; Reyniers, T.; Masquillier, C.; Thunissen, E.; Nöstlinger, C.; Laga, M.; Wouters, E.; Berghe, W.V.; Deblonde, J.; Vuylsteke, B. Awareness of, Willingness to Take PrEP and Its Actual Use Among Belgian MSM at High Risk of HIV Infection: Secondary Analysis of the Belgian European MSM Internet Survey. AIDS Behav. 2022, 26, 1793–1807. [Google Scholar] [CrossRef] [PubMed]
- Sherriff, N.S.; Jones, A.M.; Mirandola, M.; Gios, L.; Marcus, U.; Llewellyn, C.; Rosinska, M.; Folch, C.; Dias, S.F.; Toskin, I.; et al. Factors Related to Condomless Anal Intercourse between Men Who Have Sex with Men: Results from a European Bio-Behavioural Survey. J. Public Health 2020, 42, e174–e186. [Google Scholar] [CrossRef]
- Toni, T.; Welch, D.; Strelkowa, N.; Ipsen, A.; Stumpf, M.P.H. Approximate Bayesian Computation Scheme for Parameter Inference and Model Selection in Dynamical Systems. J. R. Soc. Interface 2009, 6, 187–202. [Google Scholar] [CrossRef]
- Held, L.; Hens, N.; O’Neil, P.; Wallinga, J. Handbook of Infectious Disease Data Analysis; Chapman and Hall/CRC: Boca Raton, FL, USA, 2020; ISBN 9781315222912. [Google Scholar]
- Beaumont, M.A.; Cornuet, J.M.; Marin, J.M.; Robert, C.P. Adaptive Approximate Bayesian Computation. Biometrika 2009, 96, 983–990. [Google Scholar] [CrossRef]
- Sisson, S.A.; Fan, Y.; Tanaka, M.M. Sequential Monte Carlo without Likelihoods. Proc. Natl. Acad. Sci. USA 2007, 104, 1760–1765, Correction in Proc. Natl. Acad. Sci. USA 2009, 106, 16889. [Google Scholar] [CrossRef]
- Jabot, F.; Faure, T.; Dumoulin, N. EasyABC: Efficient Approximate Bayesian Computation Sampling Schemes; INRAE: Paris, France, 2023. [Google Scholar]
- Mendez-Lopez, A.; Hickson, F.; Jansen, K.; Lachowsky, N.; Burns, F.; Folch, C.; Velter, A.; Weatherburn, P.; Marcus, U.; von Rüden, U.; et al. What Is the Empirical Basis for Converting Banded Ordinal Data on Numbers of Sex Partners among MSM into a Continuous Scale Level Variable? A Secondary Analysis of 13 Surveys across 17 Countries. BMC Med. Res. Methodol. 2022, 22, 59. [Google Scholar] [CrossRef] [PubMed]
- Kenyon, C.; Colebunders, R. Birds of a Feather: Homophily and Sexual Network Structure in Sub-Saharan Africa. Int. J. STD AIDS 2013, 24, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.; Le Guillou, A.; Gift, T.L.; Chesson, H.; Bernstein, K.T.; Delaney, K.P.; Lyles, C.; Berruti, A.; Sullivan, P.S.; Jenness, S.M. Effect of Screening and Treatment for Gonorrhea and Chlamydia on HIV Incidence among Men Who Have Sex with Men in the United States: A Modeling Analysis. Sex. Transm. Dis. 2022, 49, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.M.; Goodreau, S.M.; Morris, M.; Prasad, P.; Ramaraju, R.; Sanchez, T.; Jenness, S.M. Egocentric Sexual Networks of Men Who Have Sex with Men in the United States: Results from the ARTnet Study. Epidemics 2020, 30, 100386. [Google Scholar] [CrossRef] [PubMed]
- Hansson, D.; Strömdahl, S. Estimating Individual Action Dispositions Using Binary and Frequency Egocentric Sexual Network Data. Stat. Neerl. 2020, 74, 242–260. [Google Scholar] [CrossRef]
- Cao, B.; Saffer, A.J.; Yang, C.; Chen, H.; Peng, K.; Pan, S.W.; Durvasula, M.; Liu, C.; Fu, H.; Ong, J.J.; et al. MSM Behavior Disclosure Networks and HIV Testing: An Egocentric Network Analysis among MSM in China. AIDS Behav. 2019, 23, 1368–1374. [Google Scholar] [CrossRef]
| Target Statistics [71] | Estimated Statistics | |||
|---|---|---|---|---|
| Number of Partners in the Past 12 Months | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) |
| Overall | 15.8 (36.60) | 5 (2–15) | 16.8 (6.00) | 6 (2–19) |
| 11–20 | 16.4 (3.30) | 15 (14–20) | 16.4 (2.59) | 16 (15–19) |
| 21–30 | 27.8 (2.80) | 30 (25–30) | 27.8 (2.29) | 29 (26–30) |
| 31–40 | 38.6 (2.40) | 40 (37–40) | 38.3 (1.63) | 39 (37–40) |
| 41–50 | 49.6 (1.50) | 50 (50–50) | 49.1 (1.01) | 49 (49–50) |
| More than 50 | 128.2 (98.10) | 100 (75–150) | 129.0 (87.50) | 99.5 (55.25–172.50) |
| Prior | Weighted Mean (95% CI) | ||
|---|---|---|---|
| PrEP eligibility | Average duration of steady partnerships (in days) | Uniform (800, 2000) | 1409 (1357–1462) |
| Average duration of casual partnerships between (in days): | |||
| Uniform (4, 15) | 6 (6–6) | |
| Uniform (15, 500) | 251 (223–279) | |
| Uniform (10, 30) | 13 (12–13) | |
| Homophily rates | |||
| Uniform (0.55, 1) | 0.79 (0.76–0.81) | |
| Calculated from network | 0.90 | |
| Uniform (0.45, 1) | 0.65 (0.65–0.64) | |
| Calculated from network | 0.58 | |
| Uniform (0.45, 1) | 0.99 (0.98–0.99) | |
| Calculated from network | 0.99 | |
| >15 partners | Average duration of steady partnerships (in days) | Uniform (800, 2000) | 1065 (1031–1099) |
| Average duration of casual partnerships between (in days): | |||
| Uniform (3, 100) | 4 (4–4) | |
| Uniform (15, 500) | 299 (272–326) | |
| Uniform (5, 100) | 11 (11–11) | |
| |||
| Uniform (0.55, 1) | 0.75 (0.73–0.78) | |
| Calculated from network | 0.90 | |
| Uniform (0.60, 1) | 0.68 (0.67–0.69) | |
| Calculated from network | 0.35 | |
| Uniform (0.45, 1) | 0.98 (0.98–0.99) | |
| Calculated from network | 0.98 | |
| >15 casual partners | Average duration of steady partnerships (in days) | Uniform (800, 2000) | 1314 (1260–1367) |
| Average duration of casual partnerships between (in days): | |||
| Uniform (3, 100) | 4 (4–4) | |
| Uniform (15, 500) | 266 (244–289) | |
| Uniform (5, 100) | 8 (8–9) | |
| Homophily rates | |||
| Uniform (0.55, 1) | 0.77 (0.74–0.79) | |
| Calculated from network | 0.92 | |
| Uniform (0.45, 1) | 0.69 (0.68–0.7) | |
| Calculated from network | 0.48 | |
| Uniform (0.45, 1) | 0.98 (0.98–0.99) | |
| Calculated from network | 0.98 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsoumanis, A.; Vanden Berghe, W.; Hens, N.; Van Dijck, C. Estimating Partnership Duration among MSM in Belgium—A Modeling Study. Infect. Dis. Rep. 2024, 16, 435-447. https://doi.org/10.3390/idr16030032
Tsoumanis A, Vanden Berghe W, Hens N, Van Dijck C. Estimating Partnership Duration among MSM in Belgium—A Modeling Study. Infectious Disease Reports. 2024; 16(3):435-447. https://doi.org/10.3390/idr16030032
Chicago/Turabian StyleTsoumanis, Achilleas, Wim Vanden Berghe, Niel Hens, and Christophe Van Dijck. 2024. "Estimating Partnership Duration among MSM in Belgium—A Modeling Study" Infectious Disease Reports 16, no. 3: 435-447. https://doi.org/10.3390/idr16030032
APA StyleTsoumanis, A., Vanden Berghe, W., Hens, N., & Van Dijck, C. (2024). Estimating Partnership Duration among MSM in Belgium—A Modeling Study. Infectious Disease Reports, 16(3), 435-447. https://doi.org/10.3390/idr16030032






