1. Introduction
At present, as China faces the issue of the rapidly aging population and increasing of chronic diseases, the reduction of hospitalization costs becomes more and more urgent in China. Home health care has shown its potential possibilities in China as the new service model. It provides continuous effective health care that patients could obtain in hospitals; meanwhile, it also decreases the average hospitalization rate and saves the corresponding medical expenses. During the last decade, as a proven and useful method for reducing hospitalization costs, home health care service has experienced a significant growth in the USA and many European countries. Unlike the hospital health care services, home health care service providers (community hospitals, home care companies, etc.) can offer door-to-door services, such as family bed services, palliative care and day care services, which can improve patient satisfaction by breaking through the limit of fixed locations and optimizing the utilization of medical resources. Home health care services have a great significance as they could meet the clinical and psychological care demands in a personal environment of high quality services and save medical and social resources for conventional hospitalization.
The gap between the need for health care services and the capabilities of current Chinese health care resources is still immense, and the aging population makes the problem even worse. As the world’s most densely-populated country, China’s population was equivalent to 18.47% of the total world population as of 25 January 2017, based on the latest United Nations estimates. However, according to the report from China Daily, the medical resources of China only accounted for about three percent of the world’s medical resources. In recent decades, China’s demographic landscape has been thoroughly redrawn by unprecedented population changes, and the problem of a rapidly aging population has become more severe. The elderly population has grown substantially, and its share has reached about 10.5% of the total population in China. In particular, 80%–90% of the elderly population suffered from various chronic diseases, which has brought about the tremendous pressure on pension funds. According to China’s elderly population and the aging career statistics in 2015, the elderly aged 60 years and older increased to 212 million, accounting for 15.5% of China's total population, which was significantly higher than the ratio in the traditional standard aging society (10%). Meanwhile, the pension services have been comprehensively increased, including pension beds, day care institutions and meal-aid services. It can be seen that these kind of medical and pension services serving the community and family would play important roles in health care in the aspects of relieving pension pressure, easing the tension between limited medical resources and increasing medical needs and improving the quality of pension and health care services.
Most studies in China focused on the qualitative description of home health care services while paying little attention to resource management or scheduling optimization in family medical care. Actually, despite a vast range of prospects in home health care services, as well as its application and development in China, relevant management optimization methods designed to make the operation of home health care more reasonable and effective are still scarce. Compared with the traditional service industry, home health care service has its own features, as well as troubles in scheduling management.
In the resource management and scheduling of home health care service, we should take various uncertain factors such as the uncertain demand, stochastic traveling time and high randomness of service time into account. In addition, there are many real constraints (time windows limit, care service priority, service consistency, workload balance, and so on). The factors mentioned above bring difficulties and challenges to home health care service management and scheduling compared with the traditional hospitalization. Therefore, it is necessary to explore research on scientific management and scheduling optimization methods to solve the problems of high randomness and a dynamic environment by taking the features of a structural network into consideration.
According to the existing research of home health care, combined with practical difficulties and features, this paper focuses on the scheduling optimization of home health care service by considering patients’ priorities and time windows.
The rest of this paper will be organized as follows. A literature review is presented in
Section 2.
Section 3 describes the scheduling optimization model. The genetic algorithm with local search is provided in
Section 4.
Section 5 provides the empirical analysis and relevant results. Finally, the conclusion will be given in
Section 6.
2. Literature Review
Many scholars have conducted research in the application of home health care. Chahed et al. [
1] pointed out that resource planning is very important in the operation of home care organizations by properly managing human and physical resources so as to avoid the flow or the progress from poor efficiency, medical delay and low-quality service. Eveborn et al. [
2,
3], Bertels and Fahle [
4], Thomsen [
5] and Bennett and Erera [
6] studied a program of human resources in home care, but they did not consider the consistency of medical service requirement. Bard and Purnomo [
7,
8] developed an integer programming model for the problem of scheduling nurses by using the branch and bound algorithm, the column generation method and the Lagrangian relaxation technique. Belien and Demeulemeester [
9] integrated the scheduling of nurses and the operating room and solved it by the column generation method. Punnakitikashem et al. [
10] established a scheduling model that involves nurses’ favor and medical contraction. Hertz and Lahrichi [
11] proposed a two-stage mixed programming model to distribute medical resources. Brunner et al. [
12,
13] made a plan of physicians’ flexible scheduling. In order to make arrangements in advance, many researchers established a stochastic patients’ scheduling programming model to examine patients’ situations [
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25]; however, most of those studies ignored the characteristics of the home care system.
Borsani and Matta [
26] proposed a human resource scheduling model of home health service in 2006. In 2009, Kergosien [
27] proposed the home health care problem and extended the multiple traveling salesman problem. The article considers time windows (ti ∈ [ei, li], the earliest and the latest starting time of service i), personnel continuity and other restrictions. Bachouch and Hajri-Gabouj [
28] proposed the optimal task assignment model for home health service in 2010. Although the article has taken into account the factors and key constraints, such as balancing the workload of nurses, job skills and time windows of the working day (for full-time nurses), it does not consider the condition of cost minimization. A brief summary of the related literature is shown in
Table 1.
In addition, Ran Liu et al. [
36] proposed a periodic vehicle routing problem, so as to reduce the total scheduling cost. Rasmussen et al. [
37] provided the crew scheduling problem of home care based on preference-based visit clustering and temporal Dependencies. This article mainly focused on how to allocate the home health medical staff for patients in home visits to improve the overall service level. Apparently, more work needs to be done for the above proposed problem in the article. Cappanera and Scutellà [
38] provided the optimization problem of home care model generation. In order to optimize the home care service, it also proposed that in the allocation of home care medical staff, factors such as the capacity constraint of compatibility should be considered, and the home visiting for patients should be included in the scheduled route. Matta et al. [
39] simulated the home care service centers from the perspective of operation management and discussed the operational framework of home health service and the hierarchical structure of the operation management decision. Yalcindag et al. [
40] studied the problems of the assignment of medical staff and route scheduling in home care service and discussed how to solve the problems of personnel assignment and route scheduling though two-phase approaches while proving continuous (long-term) service. The purposes of this article were to explain the reasonability of these two different approaches and apply them to the doctor-seeing procedures for the assumption of a single region. Specially, the above mentioned article focused on the interaction between personnel assignment and routes. The assignment output results were included in the route scheduling inputs. During the personnel assignment, the mathematical programming model (MPM) and two different policies were used to balance the workload. Moreover, the route problem was solved by the travelling salesman model (TSM). However, this article did not consider the route scheduling problem if the selected place was much smaller. Lanzarone et al. [
29] provided a patient stochastic model to support human resource planning of home care service. This article provided a nursing path for the patient of the stochastic model, which offered the main variable data prediction on the basis of the historical data of the home care structure. Nevertheless, both continuous (long-term) care service and workload balance still need further improvement. Nickel et al. [
41] provided the problems of medium-term or long-term planning to support the home care service and discussed how to make medium-and-short-term plans (e.g., optimal weekly plan) by combining common heuristic algorithm and constraint model (CHACM) based on the historical data. However, it is necessary to support the research topic by using the actual data. Lanzarone et al. [
42] provided the problem of operations management for home care service and discussed how to balance the workload of the medical staff by selecting the mathematical programming model (MPM) of a specific category. This model took some features, such as continuous services, skills of the medical staff and geographic areas of the home health service into consideration. However, considering that the patient demands are either stochastic or certain, the stochastic patient demands cannot be satisfied in the above article. Yuan et al. [
43] provided the home care time arrangement and route scheduling problems under random service time. The article minimized the travel cost and the predicted tardiness penalty by establishing a stochastic programming model (SPM) and suggested that the branch and bound method (BBM) could solve the problem.
Akjiratikarl et al. [
44] adopted the particle swarm optimization (PSO)-based algorithm to solve the home care worked scheduling problem. Duque et al. [
45] presented a decision support system for the home care service planning problem by considering the service level and travelling distance. Braekers et al. [
46] provided the method of the trade-off of cost and service level and formulated a bi-objective scheduling problem. Rest and Hirsch [
47] presented a model for daily scheduling of a real-world home health care problem. Redjem and Marcon [
48] developed a heuristic method for solving caregivers’ routing of home care services. Yalçındağ et al. [
49] adopted a data-driven methodology for estimating uncertainties in traveling times so as to solve the patient assignment problem. Mankowska et al. [
50] presented a model for the routing and scheduling problem of home health care by considering interdependent services. Trautsamwieser and Hirsch [
51] provided a model for optimizing the daily nurse scheduling of home care services. Nguyen and Montemanni [
52] presented two mixed integer linear programming models to solve the home care services planning problem. Addis et al. [
53] discussed how to deal with uncertainty factors by adopting the cardinality-constrained method for the health care optimization problem.
This study aims to carry out more extensive research by considering several real situations based on the existing articles. The primary model and calculation method are presented in
Section 3.
3. The Scheduling Optimization Model
3.1. Problem Definition
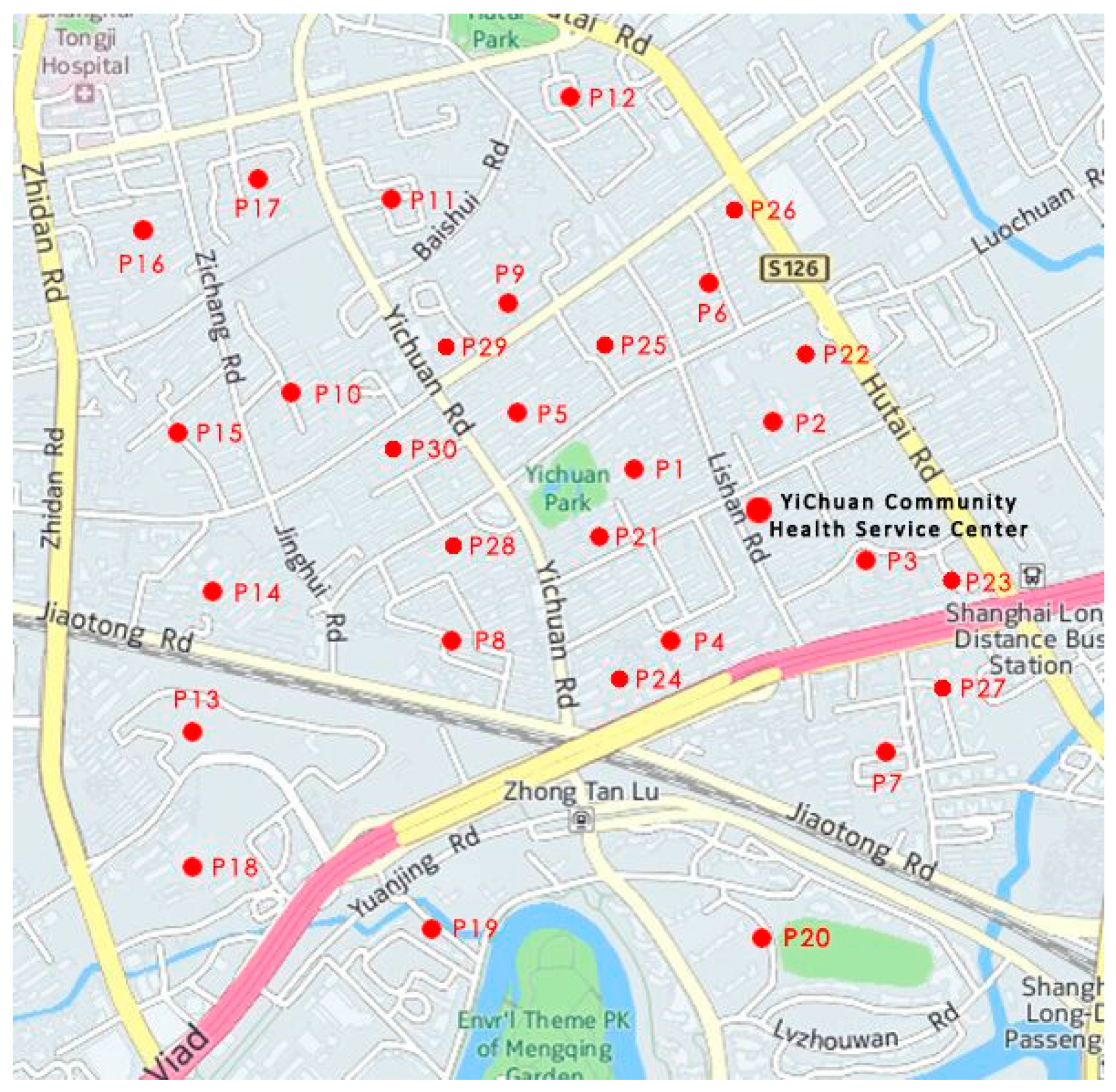
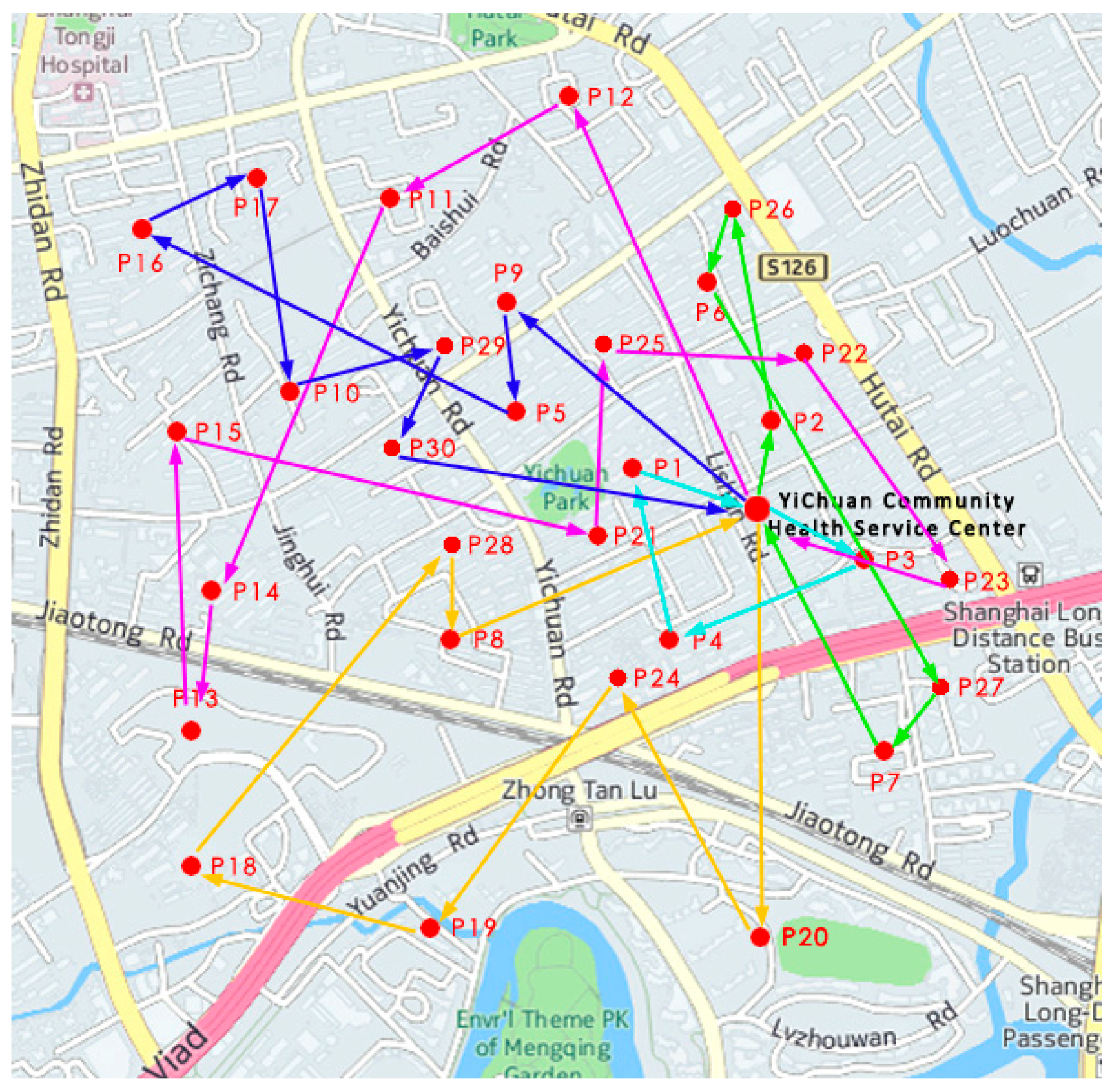
At present, home health care in Shanghai, China, mainly relies on the family doctor studio in community health care service centers. A family doctor studio is equipped with 2–3 general medical practitioners, who would provide medical care according to patients’ appointments. The types of services are divided into family beds and health records. On average, a doctor may visit 10–15 families that have signed health care service contracts with family doctors. According to the “Guiding Opinions on Promoting the Contractual Healthcare Services from Family Doctors” issued by the State Council of China, the home health care services are regulated based on health care contracts. Residents and families shall choose a team of family doctors to sign the health care service agreements, in which the content, manner and time limit of the contractual health care services, as well as the responsibilities, rights and obligations of both parties and other relevant matters have been clearly defined. In principle, the contractual health care service is valid in a one-year term. When the original contracts expire, residents and families can choose to extent the contracts or change health-care providers. After the completion of the medical care for all patients, the service personnel will return to the family doctor studio.
Therefore, this scheduling problem can be abstracted as a multiple traveling salesman problem (MTSP). MTSP is defined as: “there are n nodes and m traveling salesmen, who start working from a particular starting point. After the salesmen have visited the destinations, they come back to the starting point. The goal is to find such an amount of access paths, which satisfy the requirements that each salesman can visit a place only once in order to minimize the total cost” [
54]. This paper aims to construct a model with time windows to solve the personnel scheduling problem of home health care services.
3.2. Mathematical Programming Model
One of the common problems in home care service is how to schedule the medical staff and arrange their routes to minimize the travel cost, as well as service cost. This paper attempts to establish a route scheduling model to solve this problem.
The model is constructed based on the following basic assumptions:
- (1)
Only one type of service is required by each patient per time;
- (2)
The time that it takes the doctors to reach any two patients respectively is the same;
- (3)
Service will be started immediately after the medical staff arrive at the patients’ homes;
- (4)
Medical staff are enough to meet all demands.
Subscripts:
i represents the previous service-required place (departure place);
j represents the next service-required place (destination) (i, j ∈ P = {0, 1, …, n};
0 represents the service center;
h represents the medical staff (h = 1, …, H);
k represents the type of service (k = 1, …, K);
Parameters:
c1ij represents the travel cost from place i to place j to provide service to patients;
c2hk represents the cost for medical staff h to provide the k-th service;
tij represents the travel time from service center i to service-required place j;
τj represents the execution time of the service required by the j-th patient;
wi represents the required waiting time of the service personnel arriving at service nodes early;
ei represents that patient i can accept the earliest starting time;
li represents that the patient can accept the latest starting time, which constitutes the time window requirements of the provision of each patient service;
Si represents the time that the medical staff take to reach service-required place i, and S1 = e1;
Di represents the time that the medical staff take to leave service-required place i; , in which ei represents the earliest starting time accepted by the i-th patient; li represents the latest starting time accepted by the i-th patient;
yjhk represents whether the service k can be provided by the medical staff h for the service-required place j (0: no, 1: yes), and yjhk is the input parameter;
rij represents whether the service-required place j has priority over the service-required place i (0: yes, 1: no), and rij is the input parameter that can be determined in advance;
Decision Variables:
The mathematic model is given as follows:
The constraints are given as follows:
Formula (1) in the purposed model is to minimize the travel cost (C1), service cost (C2) and penalty cost and fully meet all patients’ demands at the same time.
Constraint (2) represents that each patient should be serviced by medical staff exactly once.
Constraint (3) represents that the medical staff must leave immediately after reaching one service-required place.
Constraints (4) and (5) represent that the medical staff only can leave and return to the service-required place once, respectively.
Constraints (6) denotes the sub-tour elimination constraint.
Constraints (7)–(9) represent the time window constraint.
Constraint (7) calculates the required waiting time of the service personnel arriving at the service nodes early.
Constraint (8) gives the time of delivery service personnel arriving at each demand point.
Constraint (9) calculates the penalty of the medical staff if they arrived early or late at the demand points, in which p is the penalty coefficient of arriving early and q is the penalty coefficient of arriving late.
Constraint (10) represents that the medical staff can offer visiting services only if he or she is a licensed qualified health care professional.
Constraint (11) is the time window restriction, which restricts the earliest departure time at each service-required place for the medical staff. Priority r represents that the medical staff must leave for the service-required place with higher priority to provide service. The priority levels in the analytical approach of this paper are identified and determined by the seriousness of the patients’ conditions. In other words, we ensure that patients with more serious conditions are accorded higher priority in medical treatment. Specifically, we divide patients into two categories with different priorities: emergency patients and non-emergency patients. Emergency patients are the top priority compared to non-emergency patients. If the serious conditions of emergency patients are equivalent, the priority classes are comprehensively determined based on factors, such as the appointment time of patients, the location of patients and the medical resources of health care service centers. The priority levels of non-emergency patients are usually determined by the appointment time of patients.
Constraints (12) and (13) represent the value ranges of the variables.
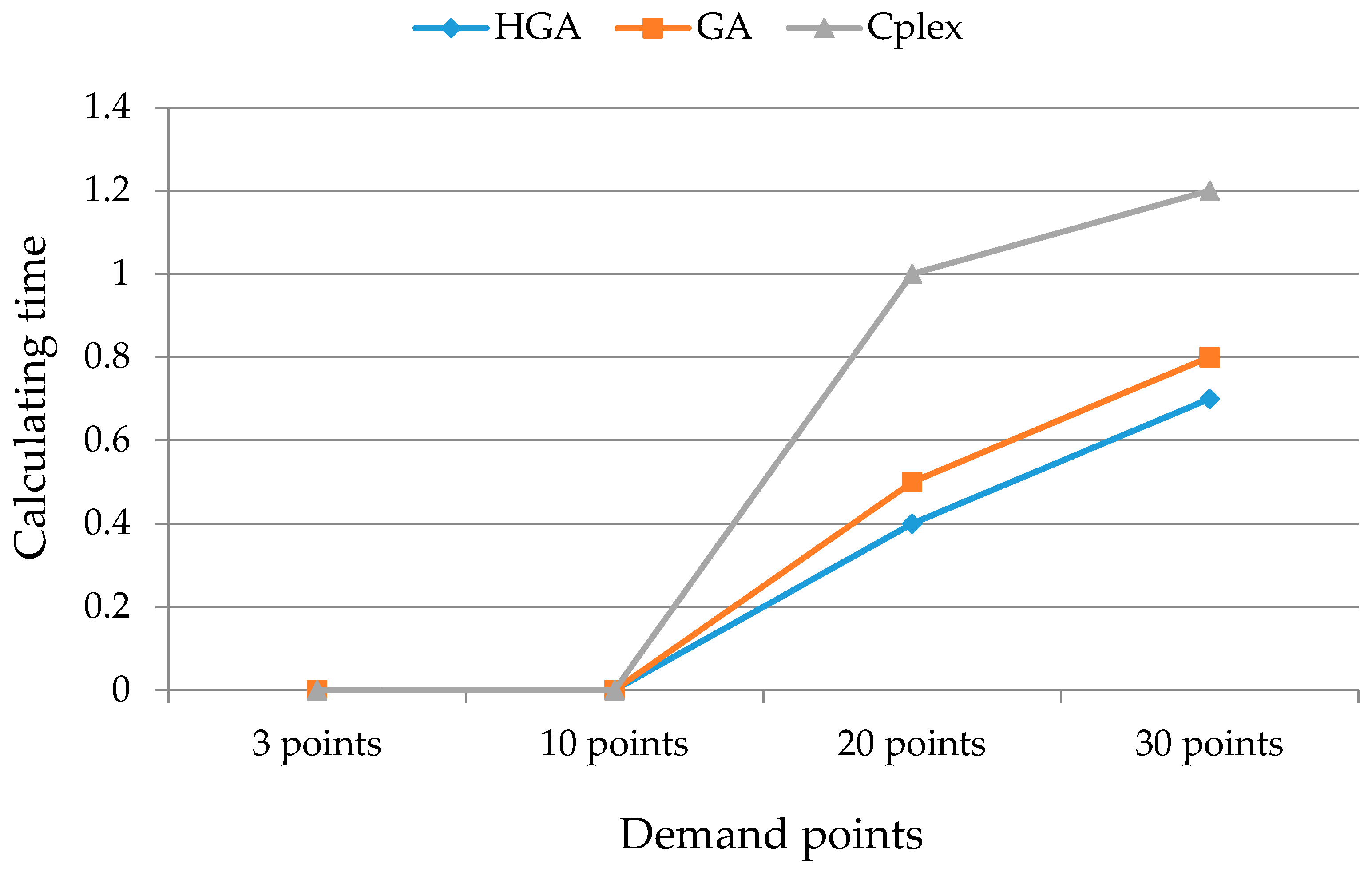
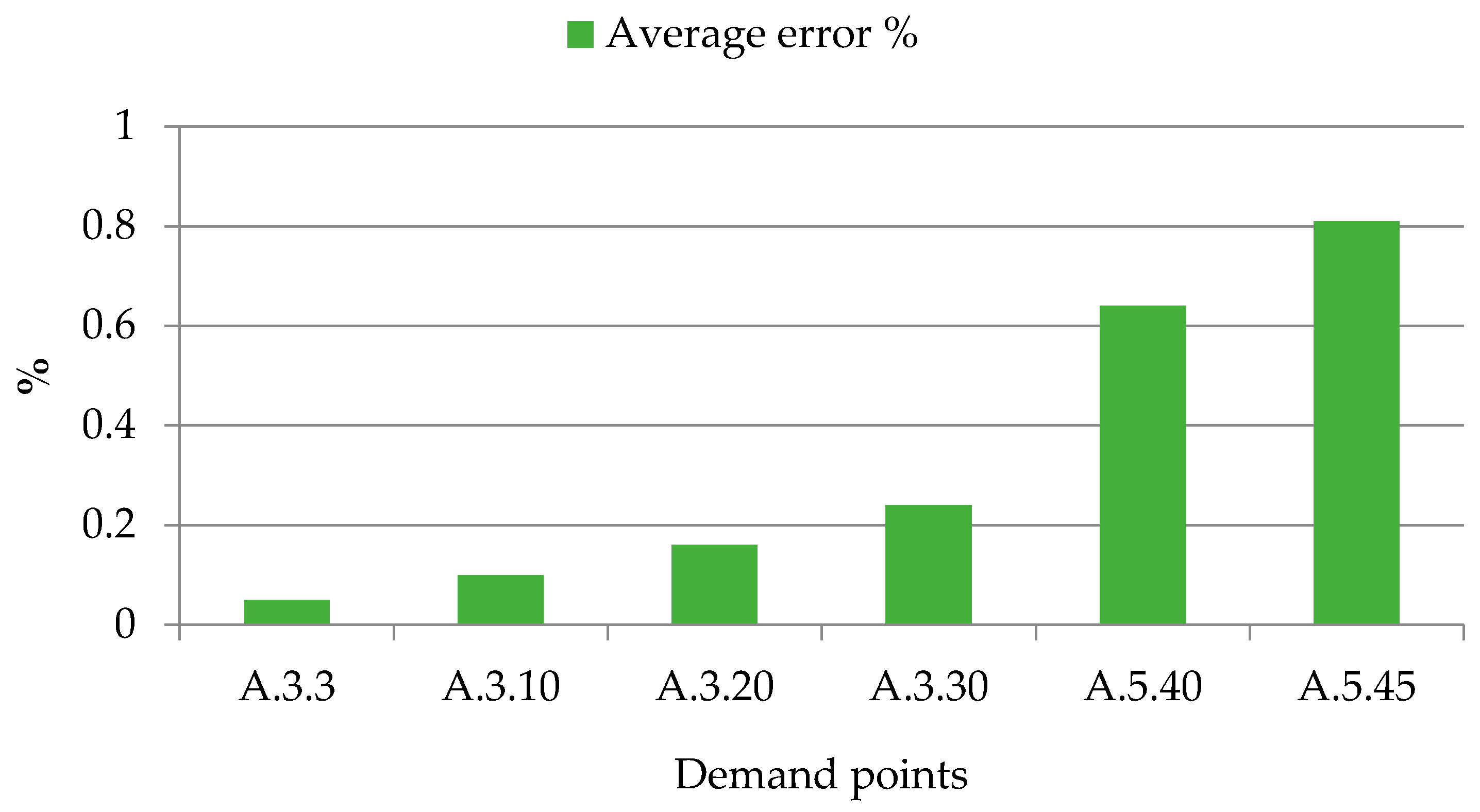
4. The Genetic Algorithm with Local Search
The proposed model in this paper is the variation of a multi-traveling salesman problem. If we relaxed the constraint of patients’ priorities, the problem of “scheduling optimization of home health care service considering patients’ priorities and time windows” will turn into the “multiple travelling salesman problem (MTSP) with time windows” [
55]. Since the traveling salesman problem (TSP) with time windows has been proven to be a strongly NP-hard problem [
56,
57], we can concluded that the problem for our research is also NP-hard. Namely, “under the assumption of the P ≠ NP, we cannot find an algorithm which can get the optimal solution in polynomial time.” Although the optimal solution can be obtained by the exact algorithm, its running time is exponentially complex. Therefore, the improved genetic algorithm can be used to solve the constructed model during the large-scale solution.
The genetic algorithm is a kind of random search method, which is based on the survival of the fittest and evolved from the biological world. Goldberg summed up a basic genetic algorithm, and its structure is simple, which is the basis of other genetic algorithms and the prototype [
58]. A population-based algorithm enhanced with a local search structure is applied to the research problem in this paper for the following three reasons: first, the method of the hybrid genetic algorithm (HGA), which integrates GA (the global optimization algorithm) with local search (the local optimization), has been adopted by many scholars to solve the problem of home health care [
59,
60,
61,
62]; second, compared to the tabu search/path-relinking (TS/PR), the method of HGA requires shorter computational time to solve the problem, but it obtains solutions with lower quality in the same computational time limit [
63,
64,
65,
66]; third, the problem proposed in this paper is mainly to meet the time requirements of families in health care services, which can be solved by the method of HGA [
49,
67]. However, considering the advantages of TS/PR, we would try to adopt TS/PR to deal with the research problem in our future research to further improve the quality of solutions.
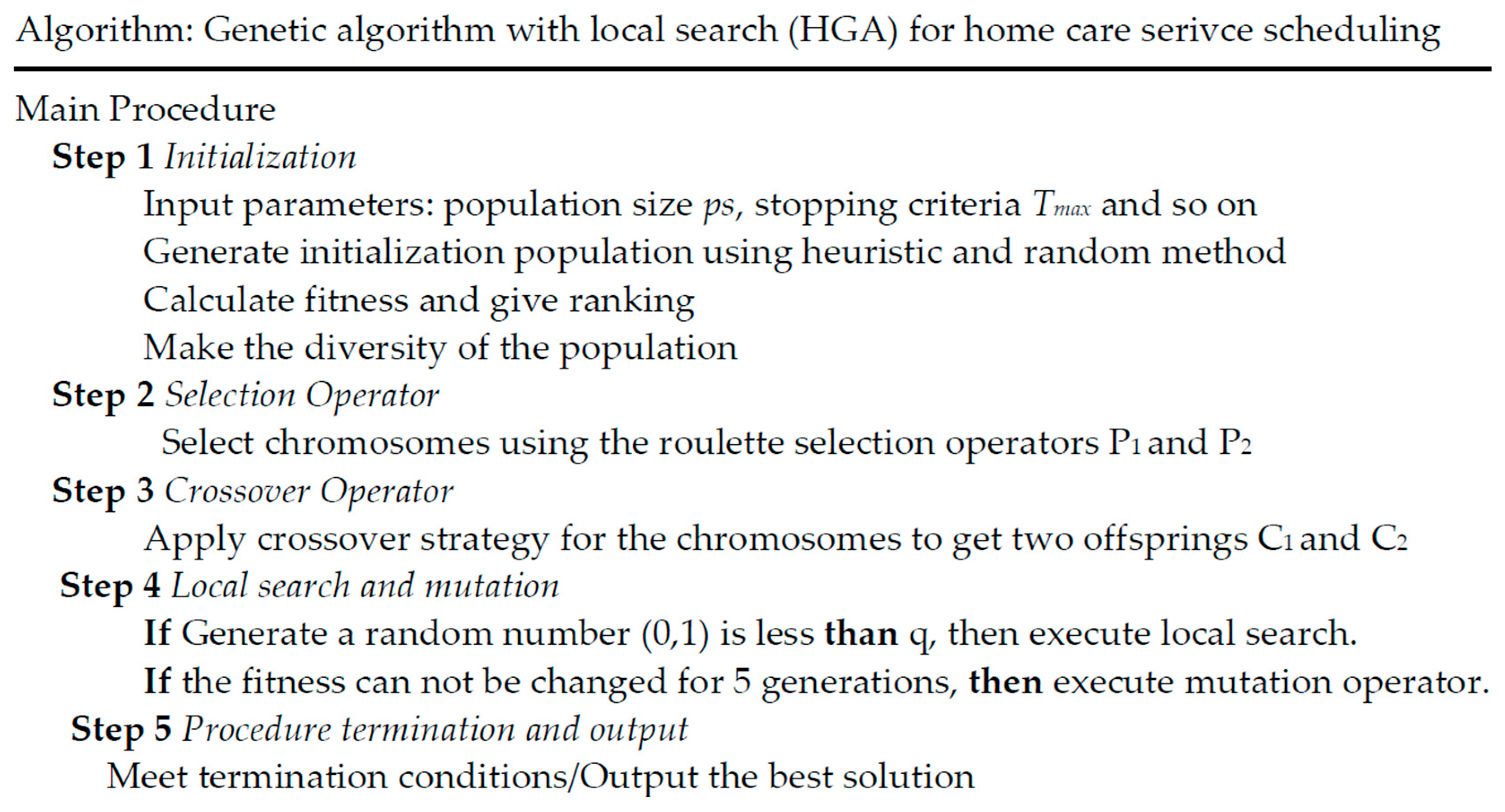
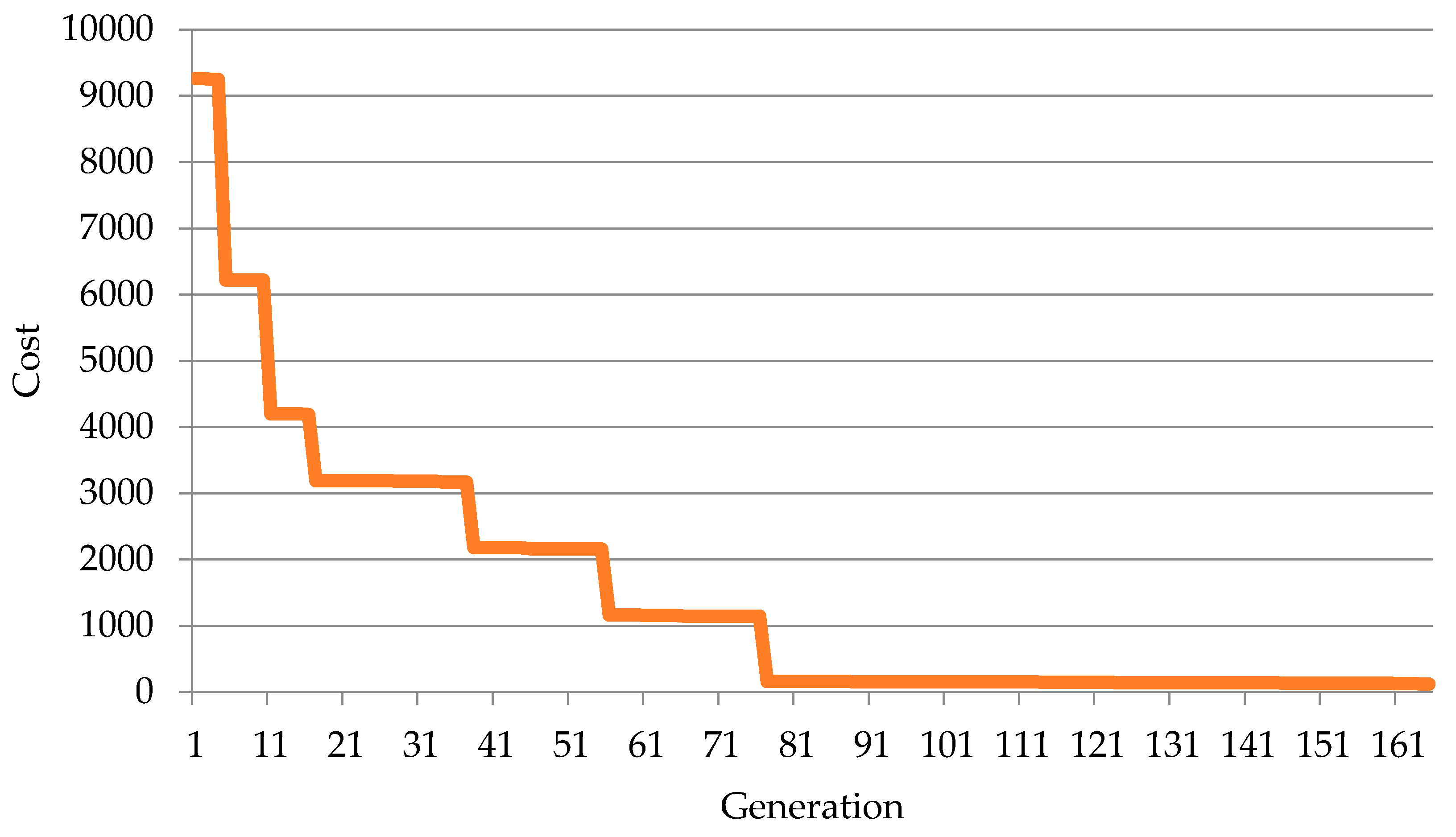
This paper refers to the basic genetic algorithm with local search, and the constructed iterative process is shown in
Figure 1.
Several main procedures can be given as follows:
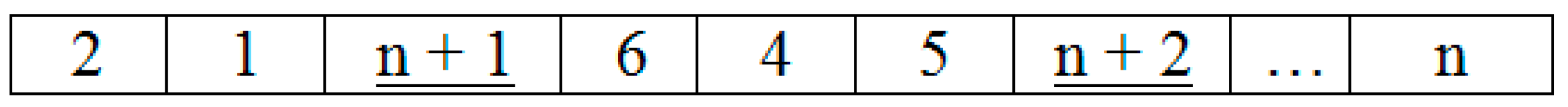
(1) The population structure and chromosome coding:
The first step is to initialize the population of chromosomes, and the key problem is how to encode the chromosomes. In order to solve the MTSP problem using the genetic algorithm, the general method is converting MTSP to the TSP problem; that is, the virtual symbol is added for coding.
Assume that Point 0 represents that there is no demand for the health service center of home care service staff, while points 1, ...,
n represent that there are 1, ...,
n demand points for the
m-th service personnel to visit. Then, a total of
m − 1 virtual symbols are to be set, respectively,
n + 1, ...,
n + (
m – 1). Each virtual symbol appearing in the medical personnel access path indicates that the medical staff return to the health service center to form a loop.
Figure 2 represents the chromosome encoding. Specifically, the first medical staff would return to the health service center after visiting Point 2 and then Point 1; the second medical staff would return to health service center after visiting Point 6, Point 4 and then Point 5.
During the coding, we need to pay attention to avoid the problem of medical staff working overtime, as well as the ordinary sub-path of the situation, that is, the medical staff did not visit any demand points directly before they return to the health service center. In the programming, the fitness of these two cases will be set to the maximum value to eliminate such a chromosome.
(2) Selection operator:
The selection operator is used to reproduce the individuals who have a high degree of adaptability from the old population to the new population. The target of this model is to minimize the cost; therefore, the fitness function f(x) = 10/Z is used for the fitness of the chromosome.
The roulette selection operator is used in this paper [
68]. It uses the proportion of each individual’s fitness to determine the probability of its future generations. The execution of a selection operator is like spinning the wheel to select a chromosome. In addition, the best individual elitist preservation strategy is considered in this paper [
69], which is selected on behalf of the population to the highest degree of individual and directly copied to the offspring. It ensures the best individual smoothly enters into the next generation and thereby speeds up the convergence of the population and improves the efficiency of the algorithm.
(3) Crossover operator:
The relevant crossover strategy is adopted in this paper [
70,
71,
72], which can increase the population diversity without changing any certain part’s order of its parent. This method will speed up the algorithm convergence. The specific steps are given as follows:
Randomly select A code from Parent Generation B; keep them in the corresponding location of the Filial Generation A. In order to ensure that two of the same chromosome can cross to produce different offspring, we consider switching the third part of Parent Generation A with the first part of Parent Generation B. After that, the rest of the parts of Filial Generation A can be selected from Parent Generation B in order (skip existing codes), and the selection of Filial Generation B is one in the same way.
Before crossing:
Parent Generation A: 872,139 | 546
Parent Generation B: 983 | 567,142
After crossing:
Filial Generation A: 721,546 | 983
Filial Generation B: 546 | 983,712
(4) Local search and mutation:
The local search is adopted with a fixed probability in HGA. If a generated random number (0, 1) is less than
q, then the local search will be executed. The two-opt exchange will be used for local search; more detailed information can be found in [
73,
74,
75,
76]. The two-opt exchange for our research is executed in the case of a single route by replacing two of its arcs in the tour using two other arcs [
77,
78]. For example, let us assume that there is a single route consisting of many demand nodes with a given order for one health care service center, and the {(
p,
p + 1); (
q,
q + 1)} is traversed in this order, which forms a crisscross [
79]. The two-opt exchange will eliminate the crisscross of the arcs (
p,
p + 1), (
q,
q + 1) by replacing them with (
p,
q), (
p + 1,
q + 1) to reconnect a new route [
80]. The same method can be used for multiple different routes for the local search. Especially, if the fitness cannot be changed for 10 generations, then the system will execute the mutation operator. For mutation operation, the multiple exchange mutation operator is adopted. We randomly select two parts from the chromosomes, then exchange the gene from the two parts and repeat the process a few times.
(5) Terminate evolution conditions:
Considering that the genetic algorithm is an iterative process, we must set the appropriate termination of the evolution conditions to terminate the algorithm. When the algorithm meets the termination conditions set, individuals who have the largest fitness during the evolutionary process will be given as the optimal solution, and the calculation will be terminated.
In this paper, we set up the following two termination rules:
- (1)
It has reached the predefined evolution generations, namely 3000 generations.
- (2)
The best individual of the population cannot obtain more improvements in 200 consecutive generations.
6. Conclusions
Under the constraint of scarce medical resources, home health care can offer convenient and effective medical services to the elderly and other special groups with less investment. In addition, reasonable arrangements for nurses and their routes not only can reduce input costs, but also can improve the degree of patient satisfaction. In order to solve this problem, this paper conduct research on the scheduling optimization problem of home health care. The proposed model can optimize the scheduling of home health care staff, and the genetic algorithm with local search was used to solve this model. In addition, some uncertainties of services and traveling time should be considered in the further study. In particular, how to establish a stochastic programming model to find the most effective solutions to the problem will be an important research direction.
Notably, it is also necessary to compare the home health care system vs. the hospital system for a period of time to comprehensively analyze the advantages and disadvantages of the home health care system. Although there are several comparisons in the literature between the home health care system and the hospital system, more detailed comparisons are still needed to provide policy implications for the development of home health care. For instance, Benbassat and Taragin [
86] found that the home health care system can reduce readmissions and improve the care quality with less expenditure. Starfield and Shi [
87] considered effectiveness, costs and equity for home health care and found that better health and lower overall costs of care could be achieved by home health care. Bruce et al. [
88] found that “poor medical and functional status for the patient” is the major disadvantage of home health care compared to the hospital system. In this paper, we mainly focus on the improvement of the efficiency, as well as the quality of home health care based on the proposed model and methodology. In order to test the effectiveness of the proposed model, we conducted a survey about the implementation effect of the optimization method and found that the home care system can reduce the care cost and improve patient satisfaction by providing more efficient and convenient services. Considering the big data requirements, we will try to compare the home health care system vs. the hospital system for a period of time in our future research.
In addition, we would like to consider more factors, such as the workload of the medical staff, in order to balance the time window constraints and the optimal allocation of health care personnel using the improved intelligent optimization algorithm [
89,
90] according to the actual needs of the situation [
91,
92] in the future research.