Coffee Intake Decreases Risk of Postmenopausal Breast Cancer: A Dose-Response Meta-Analysis on Prospective Cohort Studies
Abstract
:1. Introduction
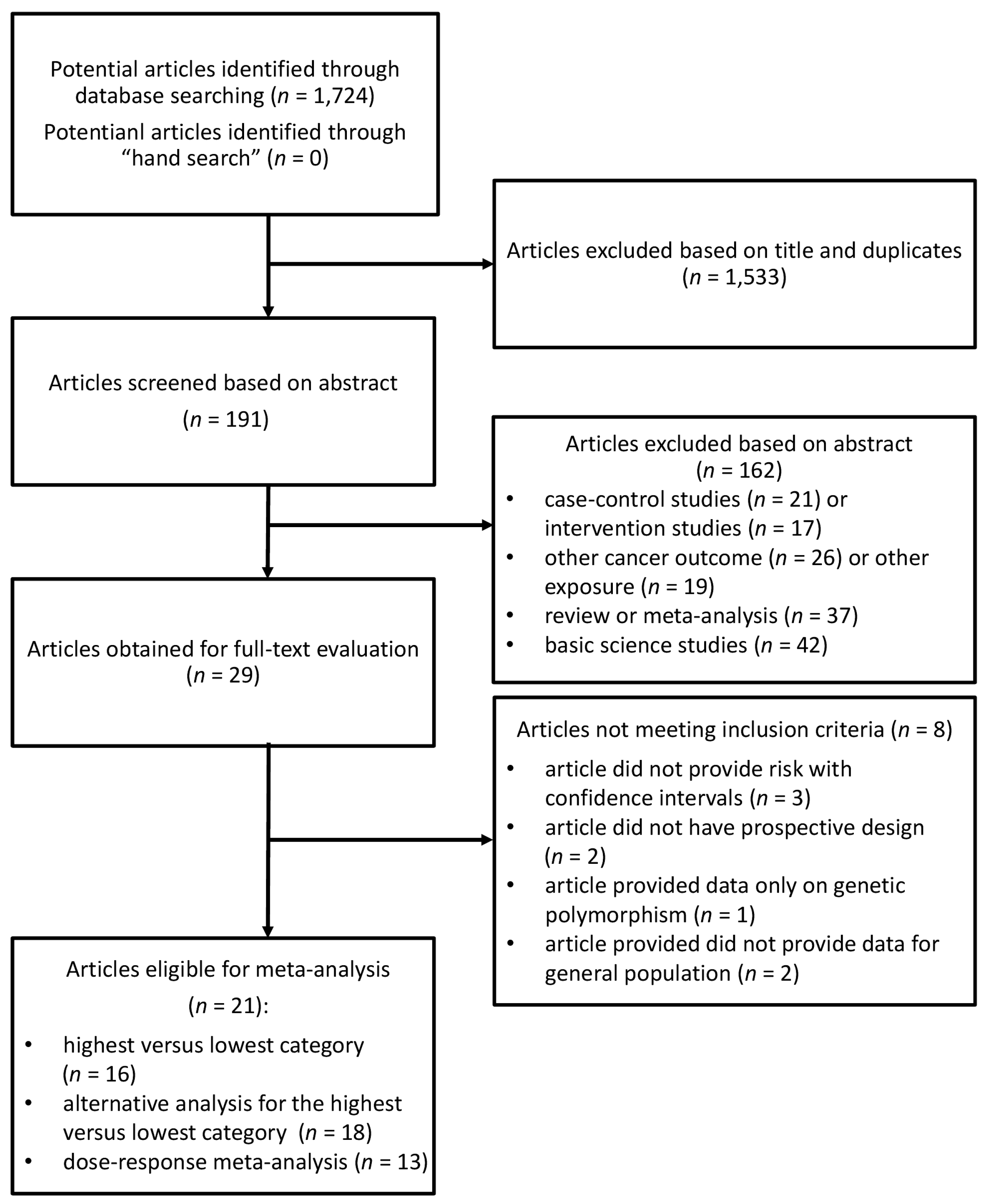
2. Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
3.1. Study Characteristics
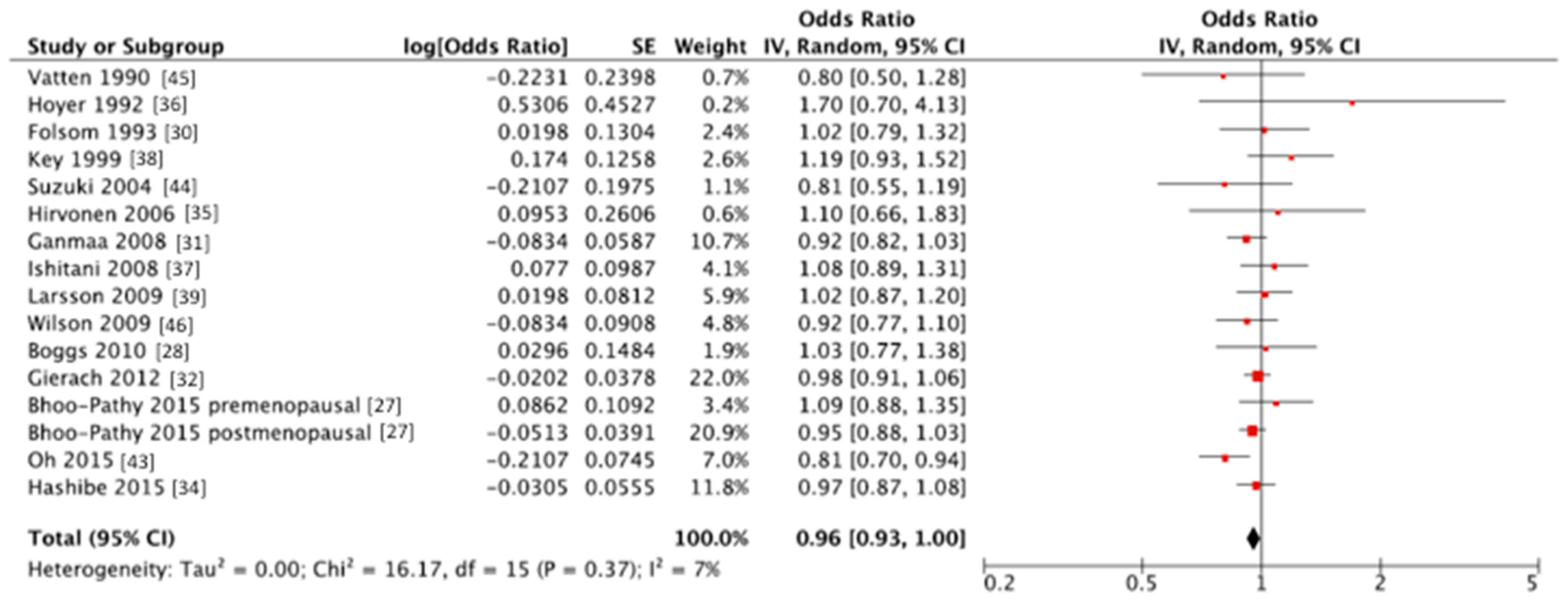
3.2. Summary Relative Risk for the High vs. Lowest Category of Coffee Consumption
3.3. Dose-Response Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Boyle, P.; Levin, B. World Cancer Report; IARC (International Agency for Research on Cancer) Press: Lyon, France, 2008; ISBN 9789283204237. [Google Scholar]
- Ban, K.A.; Godellas, C.V. Epidemiology of breast cancer. Surg. Oncol. Clin. N. Am. 2014, 23, 409–422. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Shi, A.; Lu, C.; Song, T.; Zhang, Z.; Zhao, J. Breast Cancer: Epidemiology and Etiology. Cell Biochem. Biophys. 2015, 72, 333–338. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Available online: http://globocan.iarc.fr/Default.aspx (accessed on 15 October 2017).
- Coleman, M.P.; Quaresma, M.; Berrino, F.; Lutz, J.M.; De Angelis, R.; Capocaccia, R.; Baili, P.; Rachet, B.; Gatta, G.; Hakulinen, T.; et al. Cancer survival in five continents: A worldwide population-based study (CONCORD). Lancet Oncol. 2008, 9, 730–756. [Google Scholar] [CrossRef]
- Siegel, R.; Naishadham, D.; Jemal, A. Cancer statistics, 2012. CA Cancer J. Clin. 2012, 62, 10–29. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Godos, J.; Galvano, F.; Giovannucci, E.L. Coffee, caffeine and health outcomes: An umbrella review. Annu. Rev. Nutr. 2017, 37, 131–156. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Sciacca, S.; Pajak, A.; Martinez-Gonzalez, M.A.; Giovannucci, E.L.; Galvano, F. Coffee consumption and risk of all-cause, cardiovascular and cancer mortality in smokers and non-smokers: A dose-response meta-analysis. Eur. J. Epidemiol. 2016, 31, 1191–1205. [Google Scholar] [CrossRef] [PubMed]
- Tajik, N.; Tajik, M.; Mack, I.; Enck, P. The potential effects of chlorogenic acid, the main phenolic components in coffee, on health: A comprehensive review of the literature. Eur. J. Nutr. 2017, 56, 2215–2244. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Pluchinotta, F.R.; Marventano, S.; Buscemi, S.; Li Volti, G.; Galvano, F.; Grosso, G. Coffee components and cardiovascular risk: Beneficial and detrimental effects. Int. J. Food Sci. Nutr. 2014, 65, 925–936. [Google Scholar] [CrossRef] [PubMed]
- Bohn, S.K.; Blomhoff, R.; Paur, I. Coffee and cancer risk, epidemiological evidence and molecular mechanisms. Mol. Nutr. Food Res. 2014, 58, 915–930. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.R.; Willett, W.C.; Vaidya, R.L.; Michels, K.B. An Adolescent and Early Adulthood Dietary Pattern Associated with Inflammation and the Incidence of Breast Cancer. Cancer Res. 2017, 77, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Alicandro, G.; Tavani, A.; La Vecchia, C. Coffee and cancer risk: A summary overview. Eur. J. Cancer Prev. 2017, 26, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Malerba, S.; Turati, F.; Galeone, C.; Pelucchi, C.; Verga, F.; La Vecchia, C.; Tavani, A. A meta-analysis of prospective studies of coffee consumption and mortality for all causes, cancers and cardiovascular diseases. Eur. J. Epidemiol. 2013, 28, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Je, Y.; Giovannucci, E. Coffee consumption and risk of endometrial cancer: Findings from a large up-to-date meta-analysis. Int. J. Cancer 2012, 131, 1700–1710. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.O.; Crowe, F.; Cairns, B.J.; Reeves, G.K.; Beral, V. Tea and coffee and risk of endometrial cancer: Cohort study and meta-analysis. Am. J. Clin. Nutr. 2015, 101, 570–578. [Google Scholar] [CrossRef] [PubMed]
- Braem, M.G.; Onland-Moret, N.C.; Schouten, L.J.; Tjonneland, A.; Hansen, L.; Dahm, C.C.; Overvad, K.; Lukanova, A.; Dossus, L.; Floegel, A.; et al. Coffee and tea consumption and the risk of ovarian cancer: A prospective cohort study and updated meta-analysis. Am. J. Clin. Nutr. 2012, 95, 1172–1181. [Google Scholar] [CrossRef] [PubMed]
- Li, X.J.; Ren, Z.J.; Qin, J.W.; Zhao, J.H.; Tang, J.H.; Ji, M.H.; Wu, J.Z. Coffee consumption and risk of breast cancer: An up-to-date meta-analysis. PLoS ONE 2013, 8, e52681. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Wu, Y.; Jiang, X. Coffee and caffeine intake and breast cancer risk: An updated dose-response meta-analysis of 37 published studies. Gynecol. Oncol. 2013, 129, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Degrees of Evidence by the Joint WHO/FAO Expert Consultation. Available online: http://www.who.int/nutrition/topics/5_population_nutrient/en/#diet5.1.2 (accessed on 15 October 2017).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Ottawa Health Research Institute: Ottawa, ON, Canada, 1999. [Google Scholar]
- Greenland, S. Quantitative methods in the review of epidemiologic literature. Epidemiol. Rev. 1987, 9, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Longnecker, M.P. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am. J. Epidemiol. 1992, 135, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Orsini, N.; Bellocco, R.; Greenland, S. Generalized least squares for trend estimation of summarized dose-response data. Stata J. 2006, 6, 40–57. [Google Scholar]
- Orsini, N.; Li, R.; Wolk, A.; Khudyakov, P.; Spiegelman, D. Meta-analysis for linear and nonlinear dose-response relations: Examples, an evaluation of approximations and software. Am. J. Epidemiol. 2012, 175, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Bhoo Pathy, N.; Peeters, P.; van Gils, C.; Beulens, J.W.; van der Graaf, Y.; Bueno-de-Mesquita, B.; Bulgiba, A.; Uiterwaal, C.S. Coffee and tea intake and risk of breast cancer. Breast Cancer Res. Treat. 2010, 121, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Bhoo-Pathy, N.; Peeters, P.H.; Uiterwaal, C.S.; Bueno-de-Mesquita, H.B.; Bulgiba, A.M.; Bech, B.H.; Overvad, K.; Tjonneland, A.; Olsen, A.; Clavel-Chapelon, F.; et al. Coffee and tea consumption and risk of pre- and postmenopausal breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Breast Cancer Res. 2015, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Boggs, D.A.; Palmer, J.R.; Stampfer, M.J.; Spiegelman, D.; Adams-Campbell, L.L.; Rosenberg, L. Tea and coffee intake in relation to risk of breast cancer in the Black Women’s Health Study. Cancer Causes Control 2010, 21, 1941–1948. [Google Scholar] [CrossRef] [PubMed]
- Fagherazzi, G.; Touillaud, M.S.; Boutron-Ruault, M.C.; Clavel-Chapelon, F.; Romieu, I. No association between coffee, tea or caffeine consumption and breast cancer risk in a prospective cohort study. Public Health Nutr. 2011, 14, 1315–1320. [Google Scholar] [CrossRef] [PubMed]
- Folsom, A.R.; McKenzie, D.R.; Bisgard, K.M.; Kushi, L.H.; Sellers, T.A. No association between caffeine intake and postmenopausal breast cancer incidence in the Iowa Women’s Health Study. Am. J. Epidemiol. 1993, 138, 380–383. [Google Scholar] [CrossRef] [PubMed]
- Ganmaa, D.; Willett, W.C.; Li, T.Y.; Feskanich, D.; van Dam, R.M.; Lopez-Garcia, E.; Hunter, D.J.; Holmes, M.D. Coffee, tea, caffeine and risk of breast cancer: A 22-year follow-up. Int. J. Cancer 2008, 122, 2071–2076. [Google Scholar] [CrossRef] [PubMed]
- Gierach, G.L.; Freedman, N.D.; Andaya, A.; Hollenbeck, A.R.; Park, Y.; Schatzkin, A.; Brinton, L.A. Coffee intake and breast cancer risk in the NIH-AARP diet and health study cohort. Int. J. Cancer 2012, 131, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Harris, H.R.; Bergkvist, L.; Wolk, A. An estrogen-associated dietary pattern and breast cancer risk in the Swedish Mammography Cohort. Int. J. Cancer 2015, 137, 2149–2154. [Google Scholar] [CrossRef] [PubMed]
- Hashibe, M.; Galeone, C.; Buys, S.S.; Gren, L.; Boffetta, P.; Zhang, Z.F.; La Vecchia, C. Coffee, tea, caffeine intake and the risk of cancer in the PLCO cohort. Br. J. Cancer 2015, 113, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, T.; Mennen, L.I.; de Bree, A.; Castetbon, K.; Galan, P.; Bertrais, S.; Arnault, N.; Hercberg, S. Consumption of antioxidant-rich beverages and risk for breast cancer in French women. Ann. Epidemiol. 2006, 16, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, A.P.; Engholm, G. Serum lipids and breast cancer risk: A cohort study of 5207 Danish women. Cancer Causes Control 1992, 3, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Ishitani, K.; Lin, J.; Manson, J.E.; Buring, J.E.; Zhang, S.M. Caffeine consumption and the risk of breast cancer in a large prospective cohort of women. Arch. Intern. Med. 2008, 168, 2022–2031. [Google Scholar] [CrossRef] [PubMed]
- Key, T.J.; Sharp, G.B.; Appleby, P.N.; Beral, V.; Goodman, M.T.; Soda, M.; Mabuchi, K. Soya foods and breast cancer risk: A prospective study in Hiroshima and Nagasaki, Japan. Br. J. Cancer 1999, 81, 1248–1256. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Bergkvist, L.; Wolk, A. Coffee and black tea consumption and risk of breast cancer by estrogen and progesterone receptor status in a Swedish cohort. Cancer Causes Control 2009, 20, 2039–2044. [Google Scholar] [CrossRef] [PubMed]
- Lukic, M.; Licaj, I.; Lund, E.; Skeie, G.; Weiderpass, E.; Braaten, T. Coffee consumption and the risk of cancer in the Norwegian Women and Cancer (NOWAC) Study. Eur. J. Epidemiol. 2016, 31, 905–916. [Google Scholar] [CrossRef] [PubMed]
- Michels, K.B.; Holmberg, L.; Bergkvist, L.; Wolk, A. Coffee, tea and caffeine consumption and breast cancer incidence in a cohort of Swedish women. Ann. Epidemiol. 2002, 12, 21–26. [Google Scholar] [CrossRef]
- Nilsson, L.M.; Johansson, I.; Lenner, P.; Lindahl, B.; Van Guelpen, B. Consumption of filtered and boiled coffee and the risk of incident cancer: A prospective cohort study. Cancer Causes Control 2010, 21, 1533–1544. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.K.; Sandin, S.; Strom, P.; Lof, M.; Adami, H.O.; Weiderpass, E. Prospective study of breast cancer in relation to coffee, tea and caffeine in Sweden. Int. J. Cancer 2015, 137, 1979–1989. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Tsubono, Y.; Nakaya, N.; Suzuki, Y.; Koizumi, Y.; Tsuji, I. Green tea and the risk of breast cancer: Pooled analysis of two prospective studies in Japan. Br. J. Cancer 2004, 90, 1361–1363. [Google Scholar] [CrossRef] [PubMed]
- Vatten, L.J.; Solvoll, K.; Loken, E.B. Coffee consumption and the risk of breast cancer. A prospective study of 14,593 Norwegian women. Br. J. Cancer 1990, 62, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Wilson, K.M.; Mucci, L.A.; Cho, E.; Hunter, D.J.; Chen, W.Y.; Willett, W.C. Dietary acrylamide intake and risk of premenopausal breast cancer. Am. J. Epidemiol. 2009, 169, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, G.; Chirumbolo, S. Role of oxidative stress and antioxidants in daily nutrition and human health. Nutrition 2017, 33, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Godos, J.; Lamuela-Raventos, R.; Ray, S.; Micek, A.; Pajak, A.; Sciacca, S.; D’Orazio, N.; Del Rio, D.; Galvano, F. A comprehensive meta-analysis on dietary flavonoid and lignan intake and cancer risk: Level of evidence and limitations. Mol. Nutr. Food Res. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Galvano, F.; Giovannucci, E.L. Dietary Flavonoid and Lignan Intake and Mortality in Prospective Cohort Studies: Systematic Review and Dose-Response Meta-Analysis. Am. J. Epidemiol. 2017, 185, 1304–1316. [Google Scholar] [CrossRef] [PubMed]
- Liang, N.; Kitts, D.D. Antioxidant property of coffee components: Assessment of methods that define mechanisms of action. Molecules 2014, 19, 19180–19208. [Google Scholar] [CrossRef] [PubMed]
- Kotsopoulos, J.; Eliassen, A.H.; Missmer, S.A.; Hankinson, S.E.; Tworoger, S.S. Relationship between caffeine intake and plasma sex hormone concentrations in premenopausal and postmenopausal women. Cancer 2009, 115, 2765–2774. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Schulze, M.B.; Hu, F.B.; Hankinson, S.E.; Holmes, M.D. A dietary pattern derived to correlate with estrogens and risk of postmenopausal breast cancer. Breast Cancer Res. Treat. 2012, 132, 1157–1162. [Google Scholar] [CrossRef] [PubMed]
- Sisti, J.S.; Hankinson, S.E.; Caporaso, N.E.; Gu, F.; Tamimi, R.M.; Rosner, B.; Xu, X.; Ziegler, R.; Eliassen, A.H. Caffeine, coffee and tea intake and urinary estrogens and estrogen metabolites in premenopausal women. Cancer Epidemiol. Biomark. Prev. 2015, 24, 1174–1183. [Google Scholar] [CrossRef] [PubMed]
- Nagata, C.; Kabuto, M.; Shimizu, H. Association of coffee, green tea and caffeine intakes with serum concentrations of estradiol and sex hormone-binding globulin in premenopausal Japanese women. Nutr. Cancer 1998, 30, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Chuffa, L.G.; Lupi-Junior, L.A.; Costa, A.B.; Amorim, J.P.; Seiva, F.R. The role of sex hormones and steroid receptors on female reproductive cancers. Steroids 2017, 118, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Federation, E.C. Coffee Consumption in Europe. Available online: http://www.ecf-coffee.org/about-coffee/coffee-consumption-in-europe (accessed on 15 October 2017).
- Palmioli, A.; Ciaramelli, C.; Tisi, R.; Spinelli, M.; De Sanctis, G.; Sacco, E.; Airoldi, C. Natural Compounds in Cancer Prevention: Effects of Coffee Extracts and Their Main Polyphenolic Component, 5-O-Caffeoylquinic Acid, on Oncogenic Ras Proteins. Chem. Asian J. 2017, 12, 2457–2466. [Google Scholar] [CrossRef] [PubMed]
- Marventano, S.; Salomone, F.; Godos, J.; Pluchinotta, F.; Del Rio, D.; Mistretta, A.; Grosso, G. Coffee and tea consumption in relation with non-alcoholic fatty liver and metabolic syndrome: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2016, 35, 1269–1281. [Google Scholar] [CrossRef] [PubMed]
- Lutsey, P.L.; Steffen, L.M.; Stevens, J. Dietary intake and the development of the metabolic syndrome: The Atherosclerosis Risk in Communities study. Circulation 2008, 117, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Driessen, M.T.; Koppes, L.L.; Veldhuis, L.; Samoocha, D.; Twisk, J.W. Coffee consumption is not related to the metabolic syndrome at the age of 36 years: The Amsterdam Growth and Health Longitudinal Study. Eur. J. Clin. Nutr. 2009, 63, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.S.; Chang, Y.F.; Liu, P.Y.; Chen, C.Y.; Tsai, Y.S.; Wu, C.H. Smoking, habitual tea drinking and metabolic syndrome in elderly men living in rural community: The Tianliao old people (TOP) study 02. PLoS ONE 2012, 7, e38874. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, H.; Mure, K.; Nishio, N.; Kitano, N.; Nagai, N.; Takeshita, T. Relationship between coffee consumption and prevalence of metabolic syndrome among Japanese civil servants. J. Epidemiol. 2012, 22, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Takami, H.; Nakamoto, M.; Uemura, H.; Katsuura, S.; Yamaguchi, M.; Hiyoshi, M.; Sawachika, F.; Juta, T.; Arisawa, K. Inverse correlation between coffee consumption and prevalence of metabolic syndrome: Baseline survey of the Japan Multi-Institutional Collaborative Cohort (J-MICC) Study in Tokushima, Japan. J. Epidemiol. 2013, 23, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, P.R.; Ferrari, G.S.; Ferrari, C.K. Diet, sleep and metabolic syndrome among a legal Amazon population, Brazil. Clin. Nutr. Res. 2015, 4, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Stepaniak, U.; Micek, A.; Topor-Madry, R.; Pikhart, H.; Szafraniec, K.; Pajak, A. Association of daily coffee and tea consumption and metabolic syndrome: Results from the Polish arm of the HAPIEE study. Eur. J. Nutr. 2015, 54, 1129–1137. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, A.T.; Thomsen, M.; Nordestgaard, B.G. Coffee intake and risk of obesity, metabolic syndrome and type 2 diabetes: A Mendelian randomization study. Int. J. Epidemiol. 2015, 44, 551–565. [Google Scholar] [CrossRef] [PubMed]
- Suliga, E.; Koziel, D.; Ciesla, E.; Rebak, D.; Gluszek, S. Coffee consumption and the occurrence and intensity of metabolic syndrome: A cross-sectional study. Int. J. Food Sci. Nutr. 2017, 68, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Micek, A.; Grosso, G.; Polak, M.; Kozakiewicz, K.; Tykarski, A.; Puch Walczak, A.; Drygas, W.; Kwasniewska, M.; Pajak, A. Association between tea and coffee consumption and prevalence of metabolic syndrome in Poland—Results from the WOBASZ II study (2013–2014). Int. J. Food Sci. Nutr. 2017, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pan, M.H.; Tung, Y.C.; Yang, G.; Li, S.; Ho, C.T. Molecular mechanisms of the anti-obesity effect of bioactive compounds in tea and coffee. Food Funct. 2016, 7, 4481–4491. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.M.; Lima, D.R. Coffee consumption, obesity and type 2 diabetes: A mini-review. Eur. J. Nutr. 2016, 55, 1345–1358. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wen, Y.Y.; Li, Z.R.; Luo, D.L.; Zhang, X.H. The molecular mechanisms between metabolic syndrome and breast cancer. Biochem. Biophys. Res. Commun. 2016, 471, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Feola, A.; Ricci, S.; Kouidhi, S.; Rizzo, A.; Penon, A.; Formisano, P.; Giordano, A.; Di Carlo, A.; Di Domenico, M. Multifaceted Breast Cancer: The Molecular Connection With Obesity. J. Cell. Physiol. 2017, 232, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Baspinar, B.; Eskici, G.; Ozcelik, A.O. How coffee affects metabolic syndrome and its components. Food Funct. 2017, 8, 2089–2101. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Galvano, F.; Pajak, A.; Mistretta, A. Factors associated with metabolic syndrome in a mediterranean population: Role of caffeinated beverages. J. Epidemiol. 2014, 24, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Saxena, N.K.; Sharma, D. Multifaceted leptin network: The molecular connection between obesity and breast cancer. J. Mammary Gland Biol. Neoplasia 2013, 18, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Quagliariello, V.; Rossetti, S.; Cavaliere, C.; Di Palo, R.; Lamantia, E.; Castaldo, L.; Nocerino, F.; Ametrano, G.; Cappuccio, F.; Malzone, G.; et al. Metabolic syndrome, endocrine disruptors and prostate cancer associations: Biochemical and pathophysiological evidences. Oncotarget 2017, 8, 30606–30616. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, K.; Yatsuya, H.; Muramatsu, T.; Toyoshima, H.; Murohara, T.; Tamakoshi, K. Association of coffee consumption with serum adiponectin, leptin, inflammation and metabolic markers in Japanese workers: A cross-sectional study. Nutr. Diabetes 2012, 2, e33. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Galvano, F.; Boffetta, P. Health risk factors associated with meat, fruit and vegetable consumption in cohort studies: A comprehensive meta-analysis. PLoS ONE 2017, 12, e0183787. [Google Scholar] [CrossRef] [PubMed]
- Mourouti, N.; Kontogianni, M.D.; Papavagelis, C.; Panagiotakos, D.B. Diet and breast cancer: A systematic review. Int. J. Food Sci. Nutr. 2015, 66, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Shield, K.D.; Soerjomataram, I.; Rehm, J. Alcohol Use and Breast Cancer: A Critical Review. Alcohol. Clin. Exp. Res. 2016, 40, 1166–1181. [Google Scholar] [CrossRef] [PubMed]
- Sui, Z.; Zheng, M.; Zhang, M.; Rangan, A. Water and Beverage Consumption: Analysis of the Australian 2011–2012 National Nutrition and Physical Activity Survey. Nutrients 2016, 8, 678. [Google Scholar] [CrossRef] [PubMed]
- Gibson, S.; Shirreffs, S.M. Beverage consumption habits “24/7” among British adults: Association with total water intake and energy intake. Nutr. J. 2013, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Mistura, L.; D’Addezio, L.; Turrini, A. Beverage Consumption Habits in Italian Population: Association with Total Water Intake and Energy Intake. Nutrients 2016, 8, 674. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Sanchez-Villegas, A.; Ortega, R.M.; Aranceta-Bartrina, J.; Gil, A.; Gonzalez-Gross, M.; Varela-Moreiras, G.; Serra-Majem, L. Beverage Consumption Habits and Association with Total Water and Energy Intakes in the Spanish Population: Findings of the ANIBES Study. Nutrients 2016, 8, 232. [Google Scholar] [CrossRef] [PubMed]
- Nissensohn, M.; Sanchez-Villegas, A.; Serra-Majem, L. Beverage consumption habits amongst the Spanish population: Association with total water and energy intake. Findings of the ANIBES study. Nutr. Hosp. 2015, 32 (Suppl. S2), 10325. [Google Scholar] [CrossRef] [PubMed]
- De Szabo Edelenyi, F.; Druesne-Pecollo, N.; Arnault, N.; Gonzalez, R.; Buscail, C.; Galan, P. Characteristics of Beverage Consumption Habits among a Large Sample of French Adults: Associations with Total Water and Energy Intakes. Nutrients 2016, 8, 627. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Bes-Rastrollo, M.; Galvano, F.; Martinez-Gonzalez, M.A. Long-Term Coffee Consumption Is Associated with Decreased Incidence of New-Onset Hypertension: A Dose-Response Meta-Analysis. Nutrients 2017, 9, 890. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Bella, F.; Godos, J.; Sciacca, S.; Del Rio, D.; Ray, S.; Galvano, F.; Giovannucci, E.L. Possible role of diet in cancer: Systematic review and multiple meta-analyses of dietary patterns, lifestyle factors and cancer risk. Nutr. Rev. 2017, 75, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Caprioli, G.; Cortese, M.; Sagratini, G.; Vittori, S. The influence of different types of preparation (espresso and brew) on coffee aroma and main bioactive constituents. Int. J. Food Sci. Nutr. 2015, 66, 505–513. [Google Scholar] [CrossRef] [PubMed]

| Author, Year | Cohort Name, Country | Years of Study, Follow-Up | Cases; Total Population | RR (95%CI) for Highest vs. Lowest Category of Coffee Consumption | Adjustments |
|---|---|---|---|---|---|
| Vatten, 1990 [45] | National Health Screening Service, Norway | 1974-NR, 12 years (mean) | 155; 14,593 | ≥7 cups/day vs. ≤2 cups/day; RR = 0.80 (0.50, 1.40) | Age. |
| Hoyer, 1992 [36] | The Glostrup Population Studies, Denmark | 1964–1990, 26 years (maximum) | 51; 5207 | ≥7 cups/day vs. ≤2 cups/day; RR = 1.70 (0.70, 4.30) | Social class, age at menarche, menopause status, number of full-term pregnancies, height, weight, BMI, alcohol, smoking. |
| Folsom, 1993 [30] | Iowa Women’s Health Study, USA | 1986–1990, 5 years | 580; 34,388 | ≥4 cups/day vs. 0 cups/day; RR = 1.02 (0.79, 1.30) | Age, waist/hip ratio, number of live births, age at first live birth, age at menarche, FHBC (family history of breast cancer), family history × waist/hip ratio and family history × number of live births. |
| Key, 1999 [38] | The Radiation Effects Research Foundation’s Life Span Study, Japan | 1969–1993, 24 years (maximum) | 427; 34,759 | ≥5 cups/week vs. ≤1 cups/week; RR = 1.19 (0.93, 1.52) | Age, calendar period, city, age at time of bombings, radiation dose. |
| Michels, 2002 [41] | Swedish Mammography Cohort, Sweden | 1987–1997, 9.5 years | 1271; 59,036 | ≥4 cups/day vs. ≤1 cup/day; HR = 0.94 (0.75, 1.28) | Age, family history of breast cancer, height, BMI, education, parity, age at first birth, alcohol consumption, total caloric intake. |
| Suzuki, 2004 [44] | Cohort I-Cohort II, Japan | 1984-NR Cohort I, 9 years;1990-NR Cohort II, 7 years | 103; 8799 Cohort I; 119; 11,288 Cohort II | ≥1 cup/day vs. never; RR = 0.81 (0.55, 1.18) | Age, types of health insurance, age at menarche, menopausal status, age at first birth, parity, mother’s history of breast cancer, smoking, alcohol drinking, BMI, consumption frequencies of black tea. |
| Hirvonen, 2006 [35] | Supplementation en Vitamines et Mineraux Antioxydants (SU.VI.MAX), France | 1994–2002, 6.6 years (median) | 95; 4396 | ≥3 cups/day vs. ≤1 cup/day; RR = 1.10 (0.66, 1.84) | Age, smoking, number of children, use of oral contraception, family history of breast cancer, menopausal status. |
| Ganmaa, 2008 [31] | National Health Service I, USA | 1976–2002, 22 years | 5272; 85,987 | ≥4 cups/day vs. <1 cup/month; RR = 0.92 (0.82, 1.03) | Age months, smoking status, BMI, physical activity, height, alcohol intake, family history of breast cancer in mother or a sister, history of benign breast disease, menopausal status, age at menopause, use of hormone therapy, age at menarche, parity and age at first birth, weight change after 18, duration of postmenopausal hormone use, tea intake. |
| Ishitani, 2008 [37] | Women’s Health Study, USA | 1992–2004, 10 years (average) | 1188; 38,432 | ≥4 cups/day vs. almost never; RR = 1.08 (0.89, 1.30) | Age, randomized treatment assignment, BMI, physical activity, total energy intake, alcohol intake, multivitamin use, age at menopause, age at menarche, age at first pregnancy lasting ≥6months, number of pregnancies lasting ≥6months, menopausal status, postmenopausal hormone use, prior hysterectomy, prior bilateral oophorectomy, smoking status, family history of breast cancer in mother or a sister, history of benign breast disease. |
| Larsson, 2009 [39] | Swedish Mammography Cohort (SMC), Sweden | 1987–2007, 17.4 years (mean) | 2952; 61,433 | ≥4 cups/day vs. <1 cup/day; RR = 1.02 (0.87, 1.20) | Age, education, BMI, height, parity, age at first birth, age at menarche, age at menopause, use of oral contraceptives, use of postmenopausal hormones, family history of breast cancer and intakes of total energy, alcohol and tea. |
| Wilson, 2009 [46] | National Health Service II, USA | 1991–2005, 14 years | 1179; 90,628 | ≥3 cups/day vs. <1 cup/day; RR = 0.92 (0.77, 1.11) | BMI, height, OC use, parity and age at first birth, age at menarche, family history of breast cancer, history of benign breast disease, smoking, physical activity, animal fat, glycaemic load, alcohol and energy. |
| Bhoo-Pathy, 2010 [26] | European Prospective Investigation into Cancer and Nutrition (EPIC-NL), Netherlands | 1993–2007, 9.6 years (average) | 681; 27,323 | >5 cups/day vs. <1 cup/day; HR = 0.94 (0.72, 1.24) | Age, smoking status, educational status, BMI, alcohol intake, energy intake, energy-adjusted saturated fat intake, energy-adjusted fibre intake, tea intake, physical activity level, ever prior use of oral contraceptives, presence of hypercholesterolemia, family history of breast cancer, age at menarche, parity and cohort. |
| Boggs, 2010 [28] | Black Women’s Health Study, USA | 1995–2007, 12 years | 1268; 52,062 | ≥4 cups/day vs. never; RR = 1.03 (0.77, 1.39) | Age, energy intake, age at menarche, BMI at age 18, family history of breast cancer, education, geographic region, parity, age at first birth, oral contraceptive use, menopausal status, age at menopause, female hormone use, vigorous activity, smoking status, alcohol intake. |
| Nilsson, 2010 [42] | Västerbotten Intervention Programme (VIP), Sweden | 1992–2007, 15 years (maximum) | 587; 32,178 | ≥4 cups/day vs. <1 cup/day; HR = 0.92 (0.68, 1.25) | Age, sex, BMI, smoking, education, recreational physical activity. |
| Fagherazzi, 2011 [29] | Etude Epidémiologique auprès de femmes de l’Education Nationale (E3N), France | 1993–2005, 11 years (median) | 2868; 67,703 | >3 cups/day vs. never; HR = 1.02 (0.90, 1.16) | Age, total energy intake, ever use of oral contraceptives, age at menarche, age at menopause, number of children, age at first pregnancy, history of breast cancer in the family and years of schooling, current use of postmenopausal hormone therapy (for postmenopausal women only), personal history of benign breast disease, menopausal status, BMI. |
| Gierach, 2012 [32] | NIH-AARP Diet and Health Cohort Study, USA | 1995–2006, 9.8 years (average) | 9915; 198,404 | ≥4 cups/day vs. never; RR = 0.98 (0.91, 1.07) | Age, race/ethnicity, education, BMI, smoking status and dose, alcohol, proportion of total energy from fat, age at first live birth, menopausal hormone therapy use, history of breast biopsy, family history of breast cancer. |
| Bhoo-Pathy, 2015 [27] | European Prospective Investigation into Cancer and Nutrition (EPIC), Multicentre | 1992–2010, 11 years (average) | 10,198; 335,060 | Highest quartile vs lowest quartile; HR = 1.00 (0.98, 1.03) for premenopausal women; HR = 0.99 (0.98, 0.99) for postmenopausal women | Age at menarche, ever use of oral contraceptives, age at first delivery, ever breastfeeding, smoking status, educational level, physical activity level, alcohol intake, height, weight, energy intake from fat source, energy intake from non-fat source, total saturated fat intake, total fibre intake, ever-use of postmenopausal hormones. |
| Harris, 2015 [33] | Swedish Mammography Cohort (SMC), Sweden | 1987–2012, 15 years | 1603; 37,004 | Highest quartile vs lowest quartile; HR = 0.86 (0.72, 1.04) | Age, energy intake, height, BMI, education, oral contraceptive use, hormone replacement therapy use, age at menarche, age at menopause, family history of breast cancer, history of benign breast disease, smoking status, physical activity, alcohol intake. |
| Hashibe, 2015 [34] | Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial, USA | 1992–2011, 13 years (maximum) | 1703; 50,563 | ≥2 cups/day vs. <1 cup/day; RR = 0.97 (0.87, 1.08) | Age, sex, race and education, drinking frequency. |
| Oh, 2015 [43] | Swedish Women’s Lifestyle and Health study, Sweden | 1991–2012, 11 years (average) | 1395; 42,099 | ≥5 cups/day vs. ≤2 cups/day; RR = 0.81 (0.70, 0.94) | Age, BMI, duration of breastfeeding, alcohol consumption. |
| Lukic, 2016 [40] | Norwegian Women and Cancer study (NOWAC), Norway | 1991–2013, 13.1 years (average) | 3277; 91,767 | ≥7 cups/day vs. ≤1 cup/day; HR = 0.87 (0.71, 1.06) | Menopausal status, smoking status, age at smoking initiation, number of pack-years, exposure to cigarette smoke during childhood, duration of education, BMI, physical activity level, alcohol consumption, number of children, age at first birth, ever use of oral contraceptives, duration of oral contraceptive use, use of hormone replacement therapy, maternal history of breast cancer, total energy intake, intake of fibres, intake of processed meat, intake of red meat, height, participation in mammography screening. |
| Subgroup | No. of Datasets | RR (95% CI) | I2 | Pheterogeneity |
|---|---|---|---|---|
| Total | 16 | 0.96 (0.93, 1.00) | 7% | 0.37 |
| (Alternative analysis) | 18 | 0.96 (0.93, 1.00) | 0% | 0.48 |
| Geographical location | ||||
| North America | 7 | 0.97 (0.93, 1.02) | 0% | 0.84 |
| Europe | 7 | 0.95 (0.87, 1.05) | 36% | 0.15 |
| Asia | 2 | 1.01 (0.70, 1.47) | 63% | 0.10 |
| Menopausal status | ||||
| Premenopausal | 8 | 0.98 (0.89, 1.07) | 0% | 0.46 |
| Postmenopausal | 8 | 0.92 (0.88, 0.98) | 0% | 0.57 |
| Receptor status | ||||
| ER+/PR+ | 5 | 0.97 (0.89, 1.07) | 0% | 0.40 |
| ER+/PR- or ER-/PR+ | 5 | 0.98 (0.82, 1.17) | 0% | 0.60 |
| ER-/PR- | 5 | 0.92 (0.79, 1.07) | 0% | 0.82 |
| Coffee type | ||||
| Caffeinated | 6 | 0.96 (0.91, 1.01) | 0% | 0.45 |
| Decaffeinated | 6 | 0.97 (0.90, 1.04) | 0% | 0.67 |
| BMI | ||||
| <25 kg/m2 | 5 | 0.98 (0.87, 1.10) | 0% | 0.42 |
| ≥25 kg/m2 | 5 | 0.91 (0.79, 1.04) | 0% | 0.69 |
| Duration of follow-up | ||||
| <10 years | 3 | 0.97 (0.80, 1.18) | 0% | 0.55 |
| ≥10 years | 13 | 0.97 (0.92, 1.01) | 20% | 0.24 |
| Adjustment for smoking | ||||
| No | 7 | 0.95 (0.86, 1.05) | 41% | 0.12 |
| Yes | 9 | 0.97 (0.93, 1.01) | 0% | 0.67 |
| Adjustment for alcohol intake | ||||
| No | 5 | 1.02 (0.88, 1.19) | 0% | 0.41 |
| Yes | 11 | 0.96 (0.92, 1.00) | 13% | 0.32 |
| Adjustment for physical activity | ||||
| No | 10 | 0.97 (0.90, 1.04) | 27% | 0.20 |
| Yes | 6 | 0.96 (0.91, 1.01) | 0% | 0.58 |
| Adjustment for education | ||||
| No | 10 | 0.95 (0.87, 1.04) | 32% | 0.16 |
| Yes | 6 | 0.98 (0.93, 1.02) | 0% | 0.86 |
| No. of Datasets (No. of Studies) | Coffee Intake (Cups/Day) | I2 (%) | Pheterogeneity | Pnon-linearity | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||||
| Total | ||||||||||||
| Non-linear | 13 (13) | Ref. | 0.98 (0.94, 1.03) | 0.97 (0.88, 1.06) | 0.96 (0.84, 1.11) | 0.96 (0.79, 1.16) | 0.95 (0.75, 1.22) | 0.95 (0.71, 1.28) | 0.95 (0.67, 1.34) | - | 0.69 | 0.52 |
| Linear | 13 (13) | Ref. | 0.99 (0.98, 1.00) | 0.98 (0.96, 0.99) | 0.97 (0.94, 0.99) | 0.96 (0.93, 0.99) | 0.95 (0.91, 0.98) | 0.93 (0.89, 0.98) | 0.92 (0.88, 0.98) | - | 0.58 | NA |
| Postmenopausal | ||||||||||||
| Non-linear | 6 (6) | Ref. | 1.00 (0.96, 1.04) | 0.99 (0.93, 1.05) | 0.96 (0.89, 1.03) | 0.92 (0.84, 1.00) | 0.88 (0.79, 0.99) | 0.85 (0.74, 0.97) | 0.82 (0.69, 0.96) | 0 | 0.71 | 0.14 |
| Linear | 6 (6) | Ref. | 0.97 (0.95, 1.00) | 0.95 (0.90, 1.00) | 0.92 (0.86, 1.00) | 0.90 (0.82, 0.99) | 0.88 (0.78, 0.99) | 0.85 (0.74, 0.99) | 0.83 (0.70, 0.99) | 39.6 | 0.14 | NA |
| BMI > 25 kg/m2 | ||||||||||||
| Non-linear | 5 (5) | Ref. | 0.98 (0.91, 1.06) | 0.97 (0.86, 1.10) | 0.97 (0.84, 1.12) | 0.97 (0.82, 1.14) | 0.97 (0.80, 1.18) | 0.97 (0.76, 1.24) | 0.97 (0.72, 1.30) | 10.1 | 0.35 | 0,77 |
| Linear | 5 (5) | Ref. | 0.99 (0.96, 1.02) | 0.98 (0.92, 1.05) | 0.97 (0.88, 1.08) | 0.96 (0.84, 1.10) | 0.95 (0.81, 1.13) | 0.95 (0.77, 1.16) | 0.94 (0.74, 1.19) | 39 | 0.16 | |
| ER-/PR- | ||||||||||||
| Non-linear | 5 (4) | Ref. | 0.93 (0.84, 1.04) | 0.9 (0.76, 1.07) | 0.91 (0.77, 1.08) | 0.94 (0.79, 1.11) | 0.97 (0.79, 1.19) | 1.00 (0.77, 1.30) | 1.04 (0.75, 1.43) | 0 | 0.88 | 0.25 |
| Linear | 5 (4) | Ref. | 0.99 (0.95, 1.03) | 0.98 (0.91, 1.06) | 0.97 (0.86, 1.10) | 0.97 (0.82, 1.13) | 0.96 (0.78, 1.17) | 0.95 (0.75, 1.20) | 0.94 (0.71, 1.24) | 66.3 | 0.43 | NA |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lafranconi, A.; Micek, A.; De Paoli, P.; Bimonte, S.; Rossi, P.; Quagliariello, V.; Berretta, M. Coffee Intake Decreases Risk of Postmenopausal Breast Cancer: A Dose-Response Meta-Analysis on Prospective Cohort Studies. Nutrients 2018, 10, 112. https://doi.org/10.3390/nu10020112
Lafranconi A, Micek A, De Paoli P, Bimonte S, Rossi P, Quagliariello V, Berretta M. Coffee Intake Decreases Risk of Postmenopausal Breast Cancer: A Dose-Response Meta-Analysis on Prospective Cohort Studies. Nutrients. 2018; 10(2):112. https://doi.org/10.3390/nu10020112
Chicago/Turabian StyleLafranconi, Alessandra, Agnieszka Micek, Paolo De Paoli, Sabrina Bimonte, Paola Rossi, Vincenzo Quagliariello, and Massimiliano Berretta. 2018. "Coffee Intake Decreases Risk of Postmenopausal Breast Cancer: A Dose-Response Meta-Analysis on Prospective Cohort Studies" Nutrients 10, no. 2: 112. https://doi.org/10.3390/nu10020112






