Mindfulness Is Associated with the Metabolic Syndrome among Individuals with a Depressive Symptomatology
Abstract
:1. Introduction
2. Materials and Methods
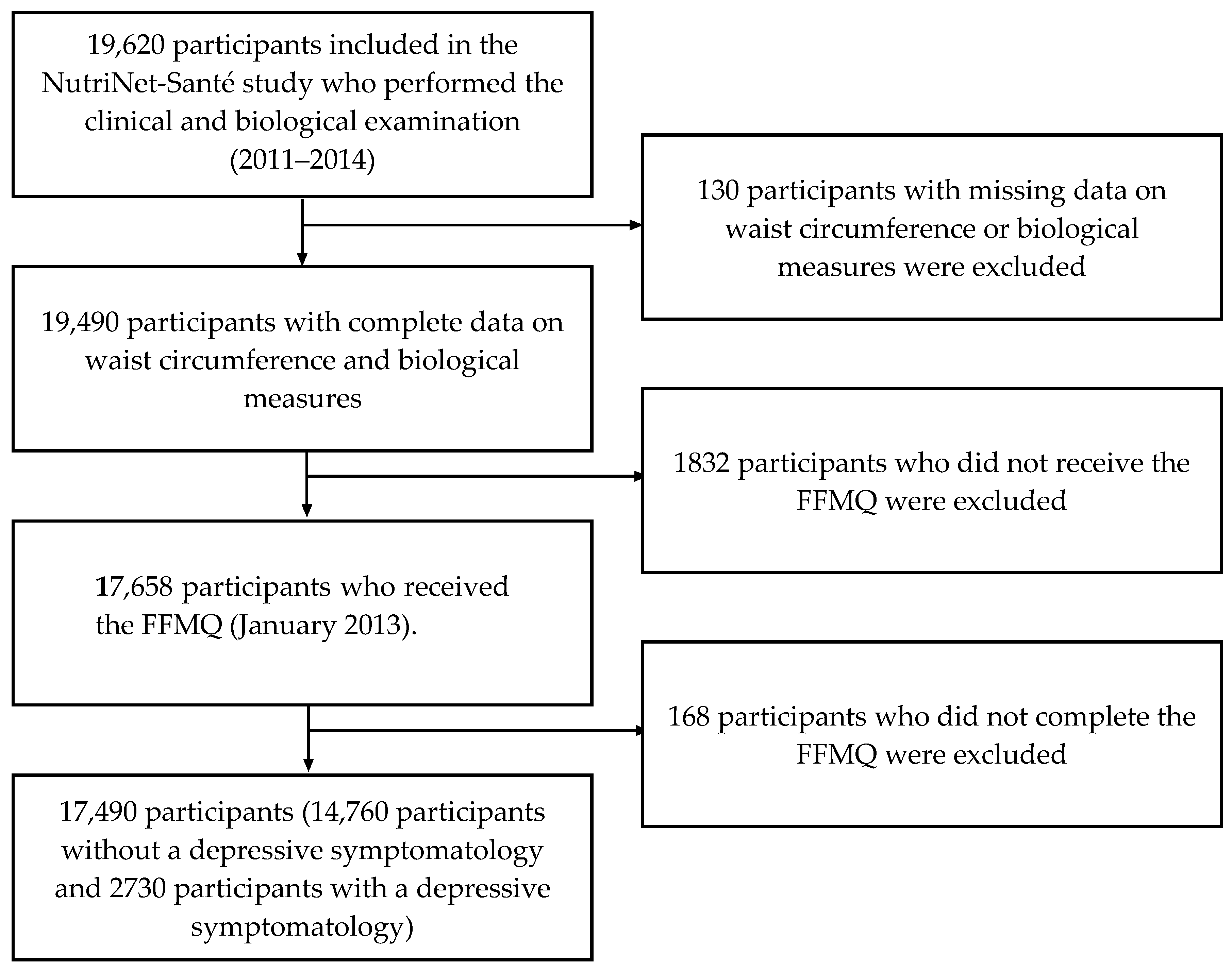
2.1. Study Population
2.2. Data Collection
2.2.1. Mindfulness
2.2.2. MetS and Cardiovascular Risk Factors
2.2.3. Depressive Symptomatology
2.2.4. Covariates: Sociodemographic and Lifestyle Data
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Sample
3.2. Association between Mindfulness and Its Subscales and the Metabolic Syndrome According to Depressive Symptomatology
3.3. Association between Mindfulness and Cardiovascular Risk Factors According to Depressive Symptomatology
4. Discussion
4.1. Mindfulness and the MetS
4.2. Mindfulness and Cardiovascular Risk Factors
4.3. Effect Modification by Depressive Symptomatology
4.4. Strengths and Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome. Diabetes Care 2005, 28, 1769–1778. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization, Ed.; World Health Organization: Geneva, Switzerland, 2009; ISBN 978-92-4-156387-1. [Google Scholar]
- Vernay, M.; Salanave, B.; De Peretti, C.; Druet, C.; Malon, A.; Deschamps, V.; Hercberg, S.; Castetbon, K. Metabolic syndrome and socioeconomic status in France: the French nutrition and health survey (ENNS, 2006–2007). Int. J. Public Health 2013, 58, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-C.; Li, T.-C.; Chang, P.-C.; Liu, C.-S.; Lin, W.-Y.; Wu, M.-T.; Li, C.-I.; Lai, M.-M.; Lin, C.-C. Association among cigarette smoking, metabolic syndrome, and its individual components: the metabolic syndrome study in Taiwan. Metabolism 2008, 57, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Gorely, T.; Davies, M.J.; Gray, L.J.; Khunti, K.; Wilmot, E.G.; Yates, T.; Biddle, S.J. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PLoS ONE 2012, 7, e34916. [Google Scholar] [CrossRef] [PubMed]
- Lutsey, P.L.; Steffen, L.M.; Stevens, J. Dietary intake and the development of the metabolic syndrome. Circulation 2008, 117, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Mommersteeg, P.M.; Kupper, N.; Denollet, J. Type D personality is associated with increased metabolic syndrome prevalence and an unhealthy lifestyle in a cross-sectional Dutch community sample. BMC Public Health 2010, 10, 714. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Costa, P.T.; Uda, M.; Ferrucci, L.; Schlessinger, D.; Terracciano, A. Personality and metabolic syndrome. Age 2010, 32, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.A.; Kuller, L.H. The relationship between psychological risk attributes and the metabolic syndrome in healthy women: antecedent or consequence? Metabolism 2002, 51, 1573–1577. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Chiesa, A.; Serretti, A. Mindfulness-Based Interventions for Chronic Pain: A Systematic Review of the Evidence. J. Altern. Complement. Med. 2011, 17, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Shennan, C.; Payne, S.; Fenlon, D. What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psychooncology 2011, 20, 681–697. [Google Scholar] [CrossRef] [PubMed]
- Bowen, S.; Chawla, N.; Collins, S.E.; Witkiewitz, K.; Hsu, S.; Grow, J.; Clifasefi, S.; Garner, M.; Douglass, A.; Larimer, M.E. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Subst. Abuse 2009, 30, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.M.G.; Alatiq, Y.; Crane, C.; Barnhofer, T.; Fennell, M.J.; Duggan, D.; Hepburn, S.; Goodwin, G. Mindfulness-based cognitive therapy (MBCT) in bipolar disorder: Preliminary evaluation of immediate effects on between-episode functioning. J. Affect. Disord. 2008, 107, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, G.M.; Méjean, C.; Bellisle, F.; Hercberg, S.; Péneau, S. Association between Mindfulness and Weight Status in a General Population from the NutriNet-Santé Study. PLoS ONE 2015, 10, e0127447. [Google Scholar] [CrossRef] [PubMed]
- Younge, J.O.; Leening, M.J.G.; Tiemeier, H.; Franco, O.H.; Kiefte-de Jong, J.; Hofman, A.; Roos-Hesselink, J.W.; Hunink, M.G.M. Association Between Mind-Body Practice and Cardiometabolic Risk Factors: The Rotterdam Study. Psychosom. Med. 2015, 77, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.G.; Taylor, A.G. The Metabolic Syndrome and Mind-Body Therapies: A Systematic Review. J. Nutr. Metab. 2011, 2011, e276419. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Bajaj, B.; Robins, R.W.; Pande, N. Mediating role of self-esteem on the relationship between mindfulness, anxiety, and depression. Personal. Individ. Differ. 2016, 96, 127–131. [Google Scholar] [CrossRef]
- Park, S.J.; Roh, S.; Hwang, J.; Kim, H.A.; Kim, S.; Lee, T.K.; Kang, S.H.; Ha, Y.J.; Jang, J.W.; Park, S. Association between depression and metabolic syndrome in korean women: Results from the korean national health and nutrition examination survey (2007–2013). J. Affect. Disord. 2016, 205, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Daskalopoulou, M.; George, J.; Walters, K.; Osborn, D.P.; Batty, G.D.; Stogiannis, D.; Rapsomaniki, E.; Pujades-Rodriguez, M.; Denaxas, S.; Udumyan, R. Depression as a risk factor for the initial presentation of twelve cardiac, cerebrovascular, and peripheral arterial diseases: data linkage study of 1.9 million women and men. PLoS ONE 2016, 11, e0153838. [Google Scholar] [CrossRef] [PubMed]
- Hercberg, S.; Castetbon, K.; Czernichow, S.; Malon, A.; Mejean, C.; Kesse, E.; Touvier, M.; Galan, P. The Nutrinet-Santé Study: A web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 2010, 10, 242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heeren, A.; Douilliez, C.; Peschard, V.; Debrauwere, L.; Philippot, P. Cross-cultural validity of the Five Facets Mindfulness Questionnaire: Adaptation and validation in a French-speaking sample. Rev. Eur. Psychol. Appl. Eur. Rev. Appl. Psychol. 2011, 61, 147–151. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist Circumference And Waist-Hip Ratio: Report of a WHO Expert Consultation, Geneva, 8–11 December 2008; World Health Organization: Geneva, Switzerland, 2011; ISBN 978-92-4-150149-1. [Google Scholar]
- Lassale, C.; Galan, P.; Julia, C.; Fezeu, L.; Hercberg, S.; Kesse-Guyot, E. Association between adherence to nutritional guidelines, the metabolic syndrome and adiposity markers in a French adult general population. PLoS ONE 2013, 8, e76349. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, D.; Waltz, J. Mindfulness and Health Behaviors. Mindfulness 2010, 1, 227–234. [Google Scholar] [CrossRef]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Le Moullec, N.; Deheeger, M.; Preziosi, P.; Monteiro, P.; Valeix, P.; Rolland-Cachera, M.; Potier de Courcy, G.; Christides, J.; Cherouvrier, F.; Galan, P. Validation of the photo manual used for the collection of dietary data in the SU. VI. MAX. study. Cah. Nutr. Diét. 1996, 31, 158–164. [Google Scholar]
- Etude Nutrinet-Santé. Table de Composition des Aliments de l’étude Nutrinet-Santé; Economica: Paris, France, 2013; ISBN 978-2-7178-6537-0. [Google Scholar]
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. 2000, 24, 1119. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Després, J.-P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef] [PubMed]
- Esmaillzadeh, A.; Kimiagar, M.; Mehrabi, Y.; Azadbakht, L.; Hu, F.B.; Willett, W.C. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am. J. Clin. Nutr. 2006, 84, 1489–1497. [Google Scholar] [CrossRef] [PubMed]
- Neufcourt, L.; Assmann, K.; Fezeu, L.; Touvier, M.; Graffouillère, L.; Shivappa, N.; Hébert, J.; Wirth, M.; Hercberg, S.; Galan, P. Prospective association between the dietary inflammatory index and metabolic syndrome: Findings from the SU. VI. MAX study. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Jordan, C.H.; Wang, W.; Donatoni, L.; Meier, B.P. Mindful eating: Trait and state mindfulness predict healthier eating behavior. Personal. Individ. Differ. 2014, 68, 107–111. [Google Scholar] [CrossRef]
- Marchiori, D.; Papies, E.K. A brief mindfulness intervention reduces unhealthy eating when hungry, but not the portion size effect. Appetite 2014, 75, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Beshara, M.; Hutchinson, A.D.; Wilson, C. Does mindfulness matter? Everyday mindfulness, mindful eating and self-reported serving size of energy dense foods among a sample of South Australian adults. Appetite 2013, 67, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.I.; Lalonde, J.K.; Coit, C.E.; Tsuang, M.T.; McElroy, S.L.; Crow, S.J.; Bulik, C.M.; Hudson, M.S.; Yanovski, J.A.; Rosenthal, N.R. Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. Am. J. Clin. Nutr. 2010, 91, 1568–1573. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, G.A.; Cook, L.; Spruijt-Metz, D.; Black, D.S. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes. Rev. 2014, 15, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Donofry, S.D.; Roecklein, K.A.; Wildes, J.E.; Miller, M.A.; Erickson, K.I. Alterations in emotion generation and regulation neurocircuitry in depression and eating disorders: A comparative review of structural and functional neuroimaging studies. Neurosci. Biobehav. Rev. 2016, 68, 911–927. [Google Scholar] [CrossRef] [PubMed]
- Goodall, K.; Trejnowska, A.; Darling, S. The relationship between dispositional mindfulness, attachment security and emotion regulation. Personal. Individ. Differ. 2012, 52, 622–626. [Google Scholar] [CrossRef]
- Troop, N.A.; Treasure, J.L. Psychosocial factors in the onset of eating disorders: Responses to life-events and difficulties. Br. J. Med. Psychol. 1997, 70, 373–385. [Google Scholar] [CrossRef] [PubMed]
- Abramowitz, J.S.; Tolin, D.F.; Street, G.P. Paradoxical effects of thought suppression: a meta-analysis of controlled studies. Clin. Psychol. Rev. 2001, 21, 683–703. [Google Scholar] [CrossRef]
- Johnston, L.; Bulik, C.M.; Anstiss, V. Suppressing thoughts about chocolate. Int. J. Eat. Disord. 1999, 26, 21–27. [Google Scholar] [CrossRef]
- Strober, M. Stressful life events associated with bulimia in anorexia nervosa. Empirical findings and theoretical speculations. Int. J. Eat. Disord. 1984, 3, 3–16. [Google Scholar] [CrossRef]
- Anicha, C.L.; Ode, S.; Moeller, S.K.; Robinson, M.D. Toward a cognitive view of trait mindfulness: Distinct cognitive skills predict its observing and nonreactivity facets. J. Pers. 2012, 80, 255–285. [Google Scholar] [CrossRef] [PubMed]
- Loucks, E.B.; Britton, W.B.; Howe, C.J.; Eaton, C.B.; Buka, S.L. Positive Associations of Dispositional Mindfulness with Cardiovascular Health: the New England Family Study. Int. J. Behav. Med. 2015, 22, 540–550. [Google Scholar] [CrossRef] [PubMed]
- Loucks, E.B.; Gilman, S.E.; Britton, W.B.; Gutman, R.; Eaton, C.B.; Buka, S.L. Associations of Mindfulness with Glucose Regulation and Diabetes. Am. J. Health Behav. 2016, 40, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Daubenmier, J.; Moran, P.J.; Kristeller, J.; Acree, M.; Bacchetti, P.; Kemeny, M.E.; Dallman, M.; Lustig, R.H.; Grunfeld, C.; Nixon, D.F.; et al. Effects of a mindfulness-based weight loss intervention in adults with obesity: A randomized clinical trial: Mindfulness-Based Weight Loss for Obesity. Obesity 2016, 24, 794–804. [Google Scholar] [CrossRef] [PubMed]
- Momeni, J.; Omidi, A.; Raygan, F.; Akbari, H. The effects of mindfulness-based stress reduction on cardiac patients’ blood pressure, perceived stress, and anger: a single-blind randomized controlled trial. J. Am. Soc. Hypertens. JASH 2016, 10, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Skilton, M.R.; Moulin, P.; Terra, J.-L.; Bonnet, F. Associations between anxiety, depression, and the metabolic syndrome. Biol. Psychiatry 2007, 62, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
- Goldbacher, E.M.; Bromberger, J.; Matthews, K.A. Lifetime History of Major Depression Predicts the Development of the Metabolic Syndrome in Middle-Aged Women. Psychosom. Med. 2009, 71, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.B.; Bravo, A.J.; Roos, C.R.; Pearson, M.R. Five facets of mindfulness and psychological health: evaluating a psychological model of the mechanisms of mindfulness. Mindfulness 2015, 6, 1021–1032. [Google Scholar] [CrossRef] [PubMed]
- Caspi, A.; Sugden, K.; Moffitt, T.E.; Taylor, A.; Craig, I.W.; Harrington, H.; McClay, J.; Mill, J.; Martin, J.; Braithwaite, A.; et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003, 301, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Song, H.; Tian, R.; Chen, L.; Zhang, W.; Qiang, Y. Association between occupational psychological stress and metabolic syndrome. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi Zhonghua Laodong Weisheng Zhiyebing Zazhi Chin. J. Ind. Hyg. Occup. Dis. 2015, 33, 88–92. [Google Scholar]
- Wingenfeld, K.; Kuehl, L.K.; Boeker, A.; Schultebraucks, K.; Ritter, K.; Hellmann-Regen, J.; Otte, C.; Spitzer, C. Stress reactivity and its effects on subsequent food intake in depressed and healthy women with and without adverse childhood experiences. Psychoneuroendocrinology 2017, 80, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Bohlmeijer, E.; ten Klooster, P.M.; Fledderus, M.; Veehof, M.; Baer, R. Psychometric Properties of the Five Facet Mindfulness Questionnaire in Depressed Adults and Development of a Short Form. Assessment 2011, 18, 308–320. [Google Scholar] [CrossRef] [PubMed]
| All n = 17,490 | No Depressive Symptomatology n = 14,760 | Depressive Symptomatology n = 2730 | P | |
|---|---|---|---|---|
| Women (%) | 71.8 | 70.0 | 81.9 | |
| Age (yr) | 54.9 ± 13.4 | 55.1 ± 13.6 | 53.9 ± 12.4 | <0.0001 |
| Education level (%) | 0.0028 | |||
| Primary | 2.9 | 2.9 | 2.9 | |
| Secondary | 31.3 | 31.1 | 32.1 | |
| Undergraduate | 27.3 | 27.0 | 29.4 | |
| Postgraduate | 33.6 | 34.1 | 31.0 | |
| Missing data | 4.8 | 4.9 | 4.7 | |
| Family status (%) | <0.0001 | |||
| Alone without a child | 23.8 | 22.2 | 32.3 | |
| Alone with child(ren) | 3.0 | 2.7 | 4.8 | |
| Living with a partner without a child | 55.4 | 57.0 | 46.4 | |
| Living with a partner with child(ren) | 17.6 | 17.9 | 16.3 | |
| Missing data | 0.2 | 0.1 | 0.2 | |
| Physical activity (%) | <0.0001 | |||
| Low | 19.7 | 18.7 | 25.0 | |
| Moderate | 41.2 | 41.0 | 41.9 | |
| High | 39.1 | 40.2 | 33.1 | |
| Missing data | 0.1 | 0.1 | 0.0 | |
| Smoking status (%) | <0.0001 | |||
| Never-smoker | 47.5 | 48.3 | 43.7 | |
| Former smoker | 42.5 | 42.4 | 42.8 | |
| Current smoker | 10.0 | 9.4 | 13.5 | |
| Energy intake (kcal/d) 2 | 1895.8 ± 510.3 | 1902.7 ± 511.0 | 1858.6 ± 504.8 | <0.0001 |
| Missing data (%) | 2.4 | 2.4 | 2.5 | |
| mPNNS-GS 3 | 8.02 ± 1.62 | 8.05 ± 1.61 | 7.92 ± 1.66 | 0.0002 |
| Mindfulness scores (1.0–5.0) 4 | 3.3 (1.1–5.0) | 3.4 (1.4–5.0) | 3.2 (1.1–4.8) | <0.0001 |
| Acting with awareness (1.0–5.0) | 3.6 (1.0–5.0) | 3.6 (1.0–5.0) | 3.4 (1.0–5.0) | <0.0001 |
| Describing (1.0–5.0) | 3.3 (1.0–5.0) | 3.3 (1.0–5.0) | 3.4 (1.0–5.0) | 0.85 |
| Observing (1.0–5.0) | 3.5 (1.0–5.0) | 3.5 (1.0–5.0) | 3.5 (1.0–5.0) | 0.14 |
| Non-judging (1.0–5.0) | 3.5 (1.0–5.0) | 3.5 (1.0–5.0) | 3.1 (1.0–5.0) | <0.0001 |
| Non-reactivity (1.0–5.0) | 2.9 (1.0–5.0) | 2.9 (1.0–5.0) | 2.7 (1.0–4.9) | <0.0001 |
| Metabolic syndrome (%) | 12.3 | 11.8 | 15.5 | <0.0001 |
| Elevated WC (≥94 cm for men. ≥80 cm for women) | 42.8 | 41.4 | 50.6 | <0.0001 |
| High blood pressure (SBP ≥ 130 and/or DBP ≥ 85 mm Hg) or treatment | 41.2 | 41.8 | 37.8 | <0.0001 |
| High triglycerides (≥150 mg/dL) or treatment | 10.2 | 9.7 | 13.0 | <0.0001 |
| Low HDL-cholesterol (<40 mg/dL for men. <50 mg/dL for women) or treatment | 9.9 | 9.2 | 13.5 | <0.0001 |
| High fasting blood glucose (≥100 mg/dL) or treatment | 13.5 | 13.5 | 13.3 | 0.84 |
| Models | No Depressive Symptomatology n = 14,760 | Depressive Symptomatology n = 2730 | |||
|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | ||
| Overall Mindfulness | Model 1 2 | 0.96 (0.84–1.09) | 0.51 | 0.71 (0.56–0.91) | 0.0072 |
| Model 2 3 | 1.01 (0.88–1.15) | 0.92 | 0.72 (0.56–0.92) | 0.0096 | |
| Model 3 4 | 1.02 (0.89–1.16) | 0.82 | 0.73 (0.57–0.93) | 0.012 | |
| Acting with awareness | Model 1 2 | 1.02 (0.94–1.10) | 0.68 | 0.89 (0.77–1.03) | 0.13 |
| Model 2 3 | 1.04 (0.96–1.13) | 0.33 | 0.90 (0.78–1.05) | 0.17 | |
| Model 3 4 | 1.04 (0.96–1.13) | 0.32 | 0.91 (0.78–1.05) | 0.20 | |
| Describing | Model 1 2 | 0.99 (0.92–1.07) | 0.82 | 0.91 (0.80–1.05) | 0.19 |
| Model 2 3 | 1.01 (0.94–1.08) | 0.84 | 0.91 (0.80–1.05) | 0.19 | |
| Model 3 4 | 1.01 (0.94–1.09) | 0.78 | 0.91 (0.80–1.05) | 0.20 | |
| Observing | Model 1 2 | 0.92 (0.85–0.99) | 0.030 | 0.90 (0.76–1.06) | 0.20 |
| Model 2 3 | 0.95 (0.88–1.03) | 0.19 | 0.90 (0.76–1.07) | 0.24 | |
| Model 3 4 | 0.95 (0.89–1.04) | 0.27 | 0.91 (0.77–1.07) | 0.26 | |
| Non-judging | Model 1 2 | 1.01 (0.94–1.09) | 0.71 | 0.86 (0.75–0.99) | 0.039 |
| Model 2 3 | 1.01 (0.94–1.09) | 0.74 | 0.86 (0.75–0.99) | 0.037 | |
| Model 3 4 | 1.01 (0.94–1.09) | 0.75 | 0.86 (0.75–0.99) | 0.040 | |
| Non-reactivity | Model 1 2 | 0.98 (0.89–1.07) | 0.61 | 0.75 (0.63–0.92) | 0.0040 |
| Model 2 3 | 1.00 (0.91–1.10) | 0.99 | 0.77 (0.64–0.93) | 0.0063 | |
| Model 3 4 | 1.00 (0.91–1.10) | 0.93 | 0.77 (0.64–0.94) | 0.0081 | |
| Models | No Depressive Symptomatology n = 14,760 | Depressive Symptomatology n = 2730 | |||
|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | ||
| Elevated WC (≥94 cm for men. ≥80 cm for women) | Model 1 2 | 0.85 (0.78–0.92) | <0.0001 | 0.77 (0.65–0.91) | 0.0028 |
| Model 2 3 | 0.89 (0.82–0.96) | 0.0050 | 0.78 (0.66–0.93) | 0.0064 | |
| Model 3 4 | 0.90 (0.83–0.98) | 0.012 | 0.80 (0.67–0.96) | 0.014 | |
| High blood pressure (SBP ≥ 130 and/or DBP ≥ 85 mm Hg) or treatment | Model 1 2 | 1.01 (0.93–1.11) | 0.78 | 0.86 (0.72–1.04) | 0.11 |
| Model 2 3 | 1.02 (0.93–1.11) | 0.68 | 0.88 (0.73–1.05) | 0.16 | |
| Model 3 4 | 1.03 (0.94–1.12) | 0.53 | 0.88 (0.73–1.06) | 0.18 | |
| High triglycerides (≥ 150 mg/dL) or treatment | Model 1 2 | 0.98 (0.85–1.12) | 0.74 | 0.84 (0.64–1.09) | 0.19 |
| Model 2 3 | 1.01 (0.88–1.16) | 0.88 | 0.82 (0.63–1.07) | 0.15 | |
| Model 3 4 | 1.01 (0.88–1.16) | 0.91 | 0.83 (0.63–1.08) | 0.16 | |
| Low HDL-cholesterol (<40 mg/dL for men. <50 mg/dL for women) or treatment | Model 1 2 | 1.03 (0.90–1.18) | 0.65 | 0.70 (0.54–0.92) | 0.0094 |
| Model 2 3 | 1.06 (0.92–1.21) | 0.43 | 0.72 (0.55–0.94) | 0.015 | |
| Model 3 4 | 1.05 (0.92–1.20) | 0.47 | 0.73 (0.55–0.95) | 0.019 | |
| High fasting blood glucose (≥100 mg/dL) or treatment | Model 1 2 | 1.02 (0.90–1.15) | 0.74 | 0.68 (0.53–0.87) | 0.0026 |
| Model 2 3 | 1.04 (0.92–1.17) | 0.57 | 0.68 (0.53–0.88) | 0.0032 | |
| Model 3 4 | 1.04 (0.92–1.18) | 0.54 | 0.69 (0.54–0.89) | 0.0045 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guyot, E.; Baudry, J.; Hercberg, S.; Galan, P.; Kesse-Guyot, E.; Péneau, S. Mindfulness Is Associated with the Metabolic Syndrome among Individuals with a Depressive Symptomatology. Nutrients 2018, 10, 232. https://doi.org/10.3390/nu10020232
Guyot E, Baudry J, Hercberg S, Galan P, Kesse-Guyot E, Péneau S. Mindfulness Is Associated with the Metabolic Syndrome among Individuals with a Depressive Symptomatology. Nutrients. 2018; 10(2):232. https://doi.org/10.3390/nu10020232
Chicago/Turabian StyleGuyot, Erika, Julia Baudry, Serge Hercberg, Pilar Galan, Emmanuelle Kesse-Guyot, and Sandrine Péneau. 2018. "Mindfulness Is Associated with the Metabolic Syndrome among Individuals with a Depressive Symptomatology" Nutrients 10, no. 2: 232. https://doi.org/10.3390/nu10020232





