Factors Influencing Parental Engagement in an Early Childhood Obesity Prevention Program Implemented at Scale: The Infant Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Context: The Infant Program
2.2. Study Site Selection
2.3. Recruitment of Program Service Providers
2.4. Recruitment of Program Participants
2.5. Qualitative Interviews and Thematic Analysis
3. Results
3.1. Description of Study Participants
3.1.1. Program Service Providers
3.1.2. Program Participants
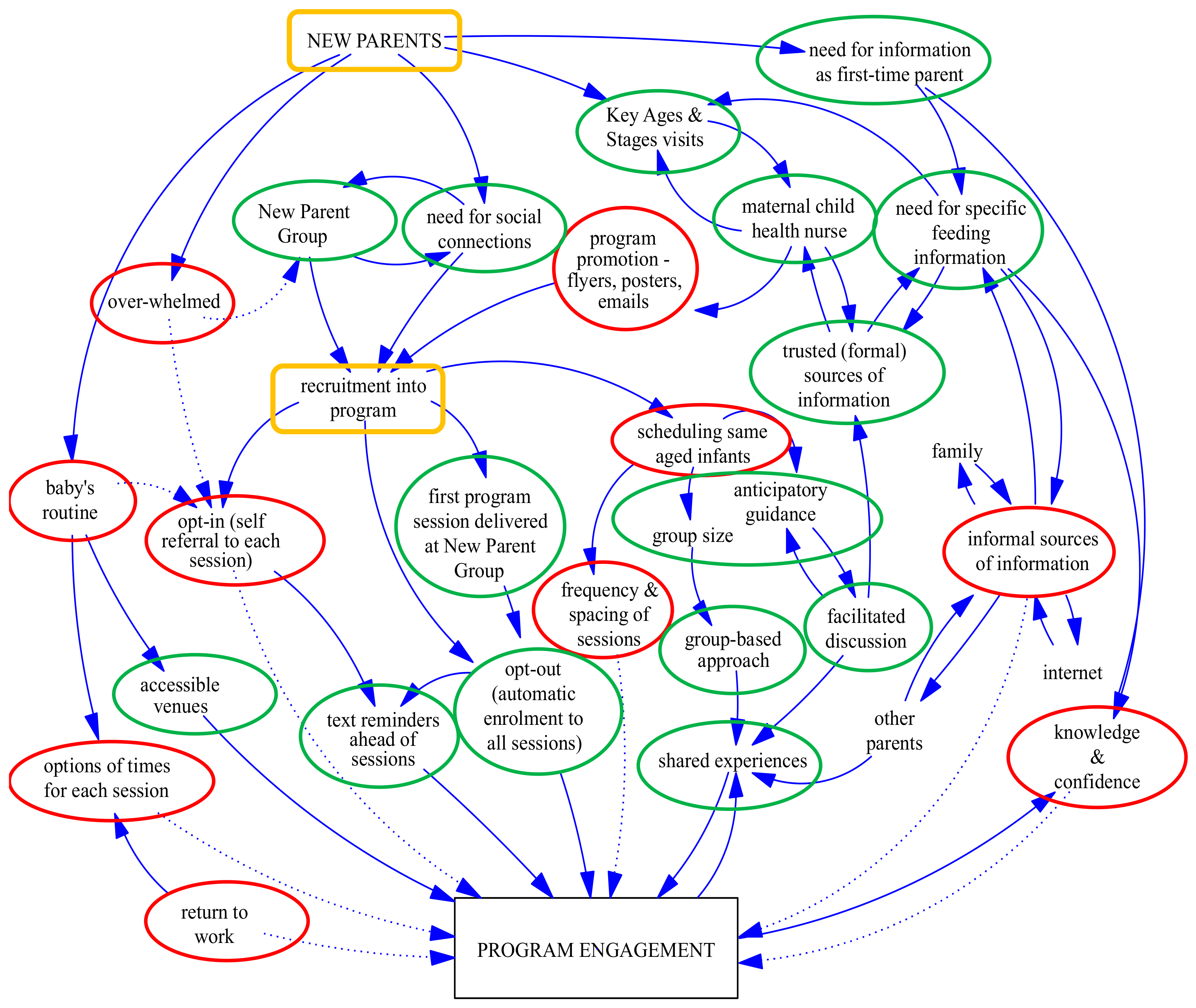
3.2. Factors Influencing Parental Engagement
3.2.1. Theme: Transition to Parenthood
“It’s something I would recommend [to new parents]. There were a lot of things that I was, like, ‘oh now we can do this’ and ‘I should be doing this’. It was really good. I took a lot of notes”(low attendee, urban 12)
“I learned a lot from it. I knew nothing about solids or how to introduce them or when to introduce them. I walked away with a clearer idea … That was the first place that I really learned about that. If I hadn’t gone there I don’t know where I actually would have learned that except from a relative”(high attendee, urban 9)
“It was just nice to have somebody there who was going through the same thing really … you didn’t feel judged because you were all going through that, yeah, having that level of friendship really helped”(high attendee, rural 14)
“I know it’s really good to get out of the house, but I just felt—and there’s so much pressure to do it. I actually felt like a bit of a failure, because I wasn’t getting there”(non-attendee, regional 2)
“I’d attend if it wasn’t his sleep time. I wasn’t going to wake him to go”(low attendee, regional 3)
3.2.2. Theme: Program Processes
- Program promotion and referral
- Program recruitment
“I think it’s probably the best way, I would say between 80 and 90% of parents going to those groups would actually express interest … and that cut out a lot of the admin of me trying to follow-up with people, because they were already coming together”(program service provider, regional 5)
“It probably helped hearing about it in the [new parent] group, because I think I went along to at least the first session with some other mums from the same group”(low attendee, urban 13)
“I’ve got a 2 year gap between my two, so my little one is 6 months old, and there are things that you forget … Perhaps a little refresher course”(low attendee, rural 18)
“It would be great to be able to attend as a second or third time mum for a refresher”(high attendee, rural 23)
“I don’t think we’re doing a fabulous job of reaching, perhaps, vulnerable families as well as we could be, because they’re not necessarily the families that are going to participate in a new parents group for whatever reason … We’ve probably got the groups there that we could partner with, and I think that’s been one of my really big learnings—don’t try and do it yourself, partner with the agencies that are already in contact with those groups, because there’s absolutely no point in setting it up and doing it yourself”(program service provider, rural 8)
“Often what it takes to engage those more vulnerable families is a lot more work. A lot more time—probably more funding in terms of you know—you’d often need an interpreter. Sometimes you would need an extra staff member, potentially to run a program or to run a session if you had families there who were, you know, English as a second language”(program service provider, regional 6)
- Program enrolment
- Program scheduling and delivery
“I’m still sort of thinking how we could do that … engage a bit better with fathers … as far as what their working arrangements are”(program service provider, regional 5)
“It’s difficult because your baby obviously does sometimes change their sleep patterns and that sort of thing … It would have been nice to have a bit more options for time”(low attendee, urban 1)
“I thought maybe it would be nice to have two sessions, one in the afternoon and one in the morning, not necessarily on the same day, because that might be really difficult, but maybe in the same week. Just to give parents an option … even after-hours so dads might be able to come”(high attendee, urban 5)
“I think getting a critical mass of babies at the right age is actually quite difficult … and that is the case for a number of [rural] areas. I think you need a really good system for that, otherwise it becomes all-consuming”(program service provider, rural 8)
“It was going to be age appropriate … If someone had have just thrown a book at us when the kids were born, it wouldn’t have been helpful”(high attendee, rural 11)
“The real advantage of these groups is that you do build that trust, and families do feel supported”(program service provider, regional 5)
“I’m a bit of a shy person, so I liked that I could just sit there quietly but still feel part of it. There was no pressure. People asked questions; I didn’t have to, because other people asked valid questions. Then there were conversations going on. It was nice to hear that everyone is on the same page as you”(low attendee, urban 11)
“The main thing I got out of it was listening to other people, their experiences … some real reassurance I suppose and knowing that you were in the same situation as other people, having the same week as other new mums”(high attendee, rural 11)
“It would have been good to have extra information emailed to you if you couldn’t attend a session”(high attendee, regional 4)
“Perhaps it could be recorded … like if someone misses a session or you want to re-look at something … or be available online”(high attendee, rural 8)
“I’ve stuck it [handout] on the fridge … from the first session and I still refer to it. It’s good to have something to take away because it’s just really overwhelming”(low attendee, urban 10)
“They [participants] were often quite surprised to hear the recommendations were no screen time up to two years, and there were lots of questions about ‘well what do we do as parents then for our own sanity?’”(program service provider, regional 6)
“I guess I was a bit disappointed, it didn’t really tell me anything that I didn’t already know. I guess I expected to get more hands on experience out of it. I felt like it was really just general healthy eating guidelines”(low attendee, regional 3, university)
“Parts of it were great and I got a lot out of it but there were parts where I just thought, ‘I feel a bit judged now’. It was like ‘this is the recommendation’”(low attendee, urban 12, university)
“Three months is a long time in between … if we were to condense it into a shorter timeframe that would be helpful because really, you know, they really need the advice maybe monthly”(program service provider, regional 5)
“We weren’t getting many 15 and 18 month attendees … now we go to the 12 month and we send them out a text message with a link to the [program] website so they can still have access to the information, and they’re more than welcome to call up”(program service provider, rural 7)
4. Discussion
5. Study Implications
- Broader program promotion through multiple channels, with more information about program content and benefits
- Earlier program promotion during pregnancy and through initial home visits/home support service, with an opportunity to address potential barriers to attendance
- Continued program promotion and referral through trusted sources of information and support, especially maternal and child health services with routine contact
- Cross-promotion and referral through interagency collaborations, especially to reach vulnerable parents
- Recruitment through established groups, especially new parent groups, with existing social bonds and groups reaching vulnerable parents
- Easy, “opt out” enrolment processes, with automated text reminders a week in advance reminding parents of the focus of the next session
- Alignment of program messages with maternal and child health services, to reach those not attending, and reinforce messages for those attending the program
- Program facilitation by maternal and child health nurses and dietitians for their specific expertise, and continuity of group facilitators to build relationships
- Program adaptations to deliver all sessions within 12 months, to accommodate parents returning to work
- Where feasible, providing a variety of session times (mornings, afternoons, evenings), accompanied by online program delivery and resources, to ensure a reliable source of information and to support a flexible mode of delivery (web-cam, app), especially for working parents, fathers, and geographically dispersed communities
6. Strengths and Limitations
7. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Moore, T.; Arefadib, N.; Deery, A.; Keyes, M.; West, S. The First Thousand Days: An Evidence Paper; Murdoch Children’s Research Institute: Melbourne, Australia, 2017. [Google Scholar]
- Blake-Lamb, T.; Locks, L.; Perkins, M.; Woo Baidal, J.; Cheng, E.; Taveras, E. Interventions for Childhood Obesity in the First 1000 Days A Systematic Review. Am. J. Prev. Med. 2016, 50, 780–789. [Google Scholar] [CrossRef] [PubMed]
- WHO. Report of the Commission on Ending Childhood Obesity; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- UNICEF. Levels and Trends in Child Malnutrition: Key Findings of the 2015 Edition; UNICEF; World Health Organisation; World Bank: New York, NY, USA, 2015. [Google Scholar]
- ABS. National Health Survey First Results, 2014–15; Australian Bureau of Statistics: Canberra, Australia, 2015. [Google Scholar]
- Walls, H.; Magliano, D.; Stevenson, C.; Backholer, K.; Mannan, H.; Shaw, J.; Peeters, A. Projected progression of the prevalence of obesity in Australia. Obesity 2012, 20, 872–878. [Google Scholar] [CrossRef] [PubMed]
- AIHW. Australia’s Health 2014. Series 14 Cat No. AUS 178; Australian Institute of Health and Welfare: Canberra, Australia, 2014. [Google Scholar]
- WHO. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Armstrong-Heimsoth, A.; Johnson, M.; McCulley, A.; Basinger, M.; Maki, K. Davison D: Good Googling: A consumer health literacy program empowering parents to find quality health information online. J. Consum. Health Internet 2017, 21, 111–124. [Google Scholar] [CrossRef]
- Cowgill, B.; Chung, P.; Thompson, L.; Elijah, J.; Lamb, S.; Garcia, V.; Bastani, R. Parents’ views on engaging families of middle school students in obesity prevention and control in a multiethnic population. Prev. Chronic Dis. 2014, 11, E54. [Google Scholar] [CrossRef] [PubMed]
- Devolin, M.; Phelps, D.; Duhaney, T.; Benzies, K.; Hildebrandt, C.; Rikhy, S.; Churchill, J. Information and support needs among parents of young children in a region of Canada: A cross-sectional survey. Public Health Nurs. 2013, 30, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Barimani, M.; Vikstrom, A.; Rosander, M.; Forslund Frykedal, K.; Berlin, A. Facilitating and inhibiting factors in transition to parenthood-ways in which health professionals can support parents. Scand. J. Caring Sci. 2017, 31, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Cook, F.; Seymour, M.; Giallo, R.; Cann, W.; Nicholson, J.M.; Green, J.; Hiscock, H. Comparison of methods for recruiting and engaging parents in online interventions: Study protocol for the Cry Baby infant sleep and settling program. BMC Pediatr. 2015, 15, 174. [Google Scholar] [CrossRef] [PubMed]
- Vine, M.; Hargreaves, M.; Briefel, R.; Orfield, C. Expanding the role of primary care in the prevention and treatment of childhood obesity: A review of clinic- and community-based recommendations and interventions. J. Obes. 2013, 2013, 172035. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Calam, R.; Latham, A. Intention to attend parenting programmes: Does ethnicity make a difference? J. Children’s Serv. 2011, 6, 45–58. [Google Scholar] [CrossRef]
- Kelleher, E.; Davoren, M.; Harrington, J.; Shiely, F.; Perry, I.; McHugh, S. Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: A systematic review. Obes. Rev. 2017, 18, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Nobles, J.; Griffiths, C.; Pringle, A.; Gately, P. Design programmes to maximise participant engagement: A predictive study of programme and participant characteristics associated with engagement in paediatric weight management. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 76. [Google Scholar] [CrossRef] [PubMed]
- Ballantyne, M.; Benzies, K.; Rosenbaum, P.; Lodha, A. Mothers’ and health care providers’ perspectives of the barriers and facilitators to attendance at Canadian neonatal follow-up programs. Child Care Health Dev. 2015, 41, 722–733. [Google Scholar] [CrossRef] [PubMed]
- Koerting, J.; Smith, E.; Knowles, M.; Latter, S.; Elsey, H.; McCann, D.; Thompson, M.; Sonuga-Barke, E. Barriers to, and facilitators of, parenting programmes for childhood behaviour problems: A qualitative synthesis of studies of parents’ and professionals’ perceptions. Eur. Child Adolesc. Psychiatry 2013, 22, 653–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ingoldsby, E. Review of interventions to improve family engagement and retention in parent and child mental health programs. J. Child Fam. Stud. 2010, 19, 629–645. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.; Placa, V.; Hunter, S. Barriers to Inclusion and Successful Engagement of Parents in Mainstream Services; Joseph Rowntree Foundation: York, UK, 2007. [Google Scholar]
- Goldfield, S.; Wright, M.; Oberkliad, F. Parents, infants and health care: Utilization of health services in the first 12 months of life. Paediatrics 2003, 39, 249–253. [Google Scholar] [CrossRef]
- Victoria Government. Maternal and Child Health Service Guidelines; Department of Education and Early Childhood Development: Melbourne, Australia, 2011.
- Victoria Government. Maternal and Child Health Services Annual Report: Statewide 2015–2016; Department of Education and Training: Melbourne, Australia, 2016.
- Coatsworth, J.; Duncan, L.; Pantin, H.; Szapocznik, J. Patterns of retention in a preventive intervention with ethnic minority families. J. Prim. Prev. 2006, 27, 171–193. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Korfmacher, J.; Hans, S. Change over time in young mothers’ engagement with a community-based doula home visiting program. Child. Youth Serv. Rev. 2016, 69, 116–126. [Google Scholar] [CrossRef]
- Brand, T.; Jungmann, T. Participant characteristics and process variables predict attrition from a home-based early intervention program. Early Child. Res. Q. 2014, 29, 155–167. [Google Scholar] [CrossRef]
- MediBank Private Limited. Identifying Effective Strategies to Increase Recruitment and Retention in Community-Based Health Promotion Programs; Deakin University’s Centre for Physical Activity and Nutrition: Melbourne, Australia, 2012. [Google Scholar]
- Victoria Government. Parental Engagement—A Review of the Literature: Supported Playgroups and Parent Groups Initiative (SPPI); Department of Education and Early Childhood Development: Melbourne, Australia, 2011.
- Ogg, J.; Shaffer-Hudkins, E.; Childres, J.; Feldman, M.; Agazzi, H.; Armstrong, K. Attendance and implementation of strategies in a behavioral parent-training program: Comparisons between English and Espanol programs. Infant Ment. Health J. 2014, 35, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Hartman, M.; Hosper, K.; Stronks, K. Targeting physical activity and nutrition interventions towards mothers with young children: A review on components that contribute to attendance and effectiveness. Public Health Nutr. 2011, 14, 1364–1381. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, K.; Cowley, S. An effective programme is not enough: A review of factors associated with poor attendance and engagement with parenting support programmes. Child. Soc. 2012, 26, 138–149. [Google Scholar] [CrossRef]
- Williams, S.; Van Lippevelde, W.; Magarey, A.; Moores, C.; Croyden, D.; Esdaile, E.; Daniels, L. Parent engagement and attendance in PEACH QLD-an up-scaled parent-led childhood obesity program. BMC Public Health 2017, 17, 559. [Google Scholar] [CrossRef] [PubMed]
- Lovell, J. How parents process child health and nutrition information: A grounded theory model. Appetite 2016, 97, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Morrissey-Kane, E.; Prinz, R. Engagement in child and adolescent treatment: The role of parental cognitions and attributions. Clin. Child Fam. Psychol. Rev. 1999, 2, 183–198. [Google Scholar] [CrossRef] [PubMed]
- La Placa, V.; Corlyon, J. Barriers to inclusion and successful engagement of parents in mainstream services: Evidence and research. J. Children’s Serv. 2014, 9, 220–234. [Google Scholar] [CrossRef]
- NSW Government. Active Engagement: Strategies to Increase Service Participation by Vulnerable Families; Department of Community Services: Sydney, Australia, 2005.
- Kulik, N.; Thomas, E.; Iovan, S.; McKeough, M.; Kendzierski, S.; Leatherwood, S. Access to primary care child weight management programs: Urban parent barriers and facilitators to participation. J. Child Health Care 2017, 21, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.; Adair, P.; Coffey, M.; Harris, R.; Burnside, G. Identifying the participant characteristics that predict recruitment and retention of participants to randomised controlled trials involving children: A systematic review. Trials 2016, 17, 294. [Google Scholar] [CrossRef] [PubMed]
- Lunn, P.; Roberts, S.; Spence, A.; Hesketh, K.; Campbell, K. Mothers’ perceptions of Melbourne InFANT Program: Informing future practice. Health Promot. Int. 2016, 31, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Mytton, J.; Ingram, J.; Manns, S.; Thomas, J. Facilitators and barriers to engagement in parenting programs: A qualitative systematic review. Health Educ. Behav. 2014, 41, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Successful Qualitative Research; Sage Publications Ltd.: Thousand Oaks, CA, USA, 2013; pp. 28–31. [Google Scholar]
- Campbell, K.; Lioret, S.; McNaughton, S.; Crawford, D.; Salmon, J.; Ball, K.; McCallum, Z. A parent-focused intervention to reduce infant obesity risk behaviors: A randomized trial. Paediatrics 2013, 131, 652–660. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Hesketh, K.; Crawford, D.; Salmon, J.; Ball, K.; McCallum, Z. The Infant Feeding Activity and Nutrition Trial (InFANT): An early intervention to prevent childhood obesity-Cluster-randomised controlled trial. BMC Public Health 2008, 8, 103. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Hesketh, K. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes. Rev. 2007, 8, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; de Silva-Sanigorski, A.; Hall, B.; Brown, T.; Campbell, K.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, CD001871. [Google Scholar] [CrossRef] [PubMed]
- Spence, A.; Campbell, K.; Crawford, D.; McNaughton, S.; Hesketh, K. Mediators of improved child diet quality following a health promotion intervention: The Melbourne InFANT Program. Inter. J. Behav. Nutr. Phys. Act. 2014, 11, 137. [Google Scholar] [CrossRef] [PubMed]
- Lioret, S.; Campbell, K.; Crawford, D.; Spence, A.; Hesketh, K.; McNaughton, A. A parent focused child obesity prevention intervention improves some mother obesity risk behaviors: The Melbourne InFANT Program. Inter. J. Behav. Nutr. Phys. Act. 2012, 9, 100. [Google Scholar] [CrossRef] [PubMed]
- Spence, A.; McNaughton, S.; Lioret, S.; Hesketh, K.; Crawford, D.; Campbell, K. A health promotion intervention can affect diet quality in early childhood. J. Nutr. 2013, 143, 1672–1678. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.; Ball, K.; Hesketh, K.; McNaughton, S.; Salmon, J.; Crawford, D.; Lioret, S.; Campbell, K. Variation in outcomes of the Melbourne Infant, Feeding, Activity and Nutrition Trial (InFANT) Program according to maternal education and age. Prev. Med. 2014, 58, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Laws, R.; Hesketh, K.; Ball, K.; Cooper, C.; Vrljic, K.; Campbell, K. Translating an early childhood obesity prevention program for local community implementation: A case study of the Melbourne InFANT Program. BMC Public Health 2016, 16, 748. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Hesketh, K.; McNaughton, S.; Ball, K.; McCallum, Z.; Lynch, J.; Crawford, D. The extended Infant Feeding, Activity and Nutrition Trial (InFANT Extend) Program: A cluster-randomized controlled trial of an early intervention to prevent childhood obesity Energy balance-related behaviors. BMC Public Health 2016, 16, 166. [Google Scholar] [CrossRef] [PubMed]
- Loudon, K.; Buchanan, S.; Ruthven, I. The everyday life information seeking behaviours of first-time mothers. J. Doc. 2016, 72, 24–46. [Google Scholar] [CrossRef]
- Downing, K.L.; Campbell, K.J.; Van Der Pligt, P.; Hesketh, K.D. Facilitator and Participant Use of Facebook in a Community-Based Intervention for Parents: The InFANT Extend Program. Child. Obes. 2017, 13, 443–454. [Google Scholar] [CrossRef] [PubMed]
- Litterbach, E.K.; Russell, C.G.; Taki, S.; Denney-Wilson, E.; Campbell, K.J.; Laws, R.A. Factors Influencing Engagement and Behavioral Determinants of Infant Feeding in an mHealth Program: Qualitative Evaluation of the Growing Healthy Program. JMIR Mhealth Uhealth 2017, 5, e196. [Google Scholar] [CrossRef] [PubMed]
- Taki, S.; Lymer, S.; Russell, C.; Campbell, K.; Laws, R.; Ong, K.; Elliott, R.; Denney-Wilson, E. Assessing user engagement of an mHealth intervention: Development and implementation of the Growing Healthy App Engagement Index. JMIR Mhealth Uhealth 2017, 5, e89. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.; Gibbons, K.; Arnup, S.; Volders, E.; Naughton, G. Early childhood nutrition, active outdoor play and sources of information for families living in highly socially disadvantaged locations. J. Paediatr. Child Health 2015, 51, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Guerra-Reyes, L.; Christie, V.; Prabhakar, A.; Harris, A.; Siek, K. Postpartum health information seeking using mobile phones: Experiences of low-income mothers. Mater. Child Health J. 2016, 20 (Suppl. 1), 13–21. [Google Scholar] [CrossRef] [PubMed]
- Doty, J.; Dworking, J.; Connell, J. Examining digital differences: Parents’ online activities. Fam. Sci. Rev. 2012, 17, 18–39. [Google Scholar] [CrossRef]
- Mittal, P. Centering Parenting: Pilot Implementation of a Group Model for Teaching Family Medicine Residents Well-Child Care. Perm. J. 2011, 15, 40–41. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.; Hesketh, K.; Van Der Pligt, P.; Cameron, A.; Crawford, D.; Campbell, K. Fathers’ perspectives on the diets and physical activity behaviours of their young children. PLoS ONE 2017, 12, e0179210. [Google Scholar] [CrossRef] [PubMed]
- Laws, R.; Campbell, K.; van der Pligt, P.; Ball, K.; Lynch, J.; Russell, G.; Taylor, R.; Denney-Wilson, E. Obesity prevention in early life: An opportunity to better support the role of Maternal and Child Health Nurses in Australia. BMC Nurs. 2015, 14, 26. [Google Scholar] [CrossRef] [PubMed]
| Study Site | Rural | Regional | Urban |
|---|---|---|---|
| Source of referral | Maternal and child health nurse | ||
| Program promotion and recruitment | First session of Infant Program run at last meeting of new parent group | Short presentation at last session of new parent group | At 8-week maternal and child health visit; posters, pamphlets and flyers at new parent group venues |
| Enrolment process | Automatically enrolled into all sessions with option to opt out | Expression of interest form at last session of new parent group—enrolled for first session; responsibility of parent to enrol for subsequent sessions | Written invitation to all new parent group participants with program information; responsibility of parent to enrol for sessions |
| Program sessions | Six 1.5 h sessions at 3-monthly intervals when infant is 3–18 months of age | ||
| Program facilitators | Dietitians | Social workers | Maternal and child health nurse; dietitian |
| Program venues | First session at new parent group venue; all other sessions at community health service | Range of local community venues | Range of local community venues |
| Program reminders | Text message reminder sent | ||
| Program Participants by Study Site | Surveys—Number (%) | Interviews—Number (%) | School/High School Certificate | Trade/Apprenticeship Certificate/Diploma | University Degree | |||
|---|---|---|---|---|---|---|---|---|
| Sur. | Inter. | Sur. | Inter. | Sur. | Inter. | |||
| Total Attendees | 53 | 32 | 6 | 3 | 17 | 11 | 30 | 18 |
| rural | 26 (49.1%) | 13 (40.6%) | 3 | 2 | 7 | 3 | 15 | 8 |
| regional | 7 (13.2%) | 4 (12.5%) | 0 | 0 | 3 | 1 | 4 | 3 |
| urban | 20 (37.7%) | 15 (46.9) | 3 | 1 | 7 | 7 | 11 | 7 |
| Non Attendees | 7 (13.2%) | 2 (6.3%) | 1 | 1 | 1 | 0 | 5 | 1 |
| rural | 1 (14.3%) | 1 (50.0%) | 1 | 1 | 0 | 0 | 1 | 0 |
| regional | 2 (28.6%) | 1 (50.0%) | 0 | 0 | 1 | 0 | 2 | 1 |
| urban | 2 (28.6%) | 0 (0.0%) | 0 | 0 | 0 | 0 | 2 | 0 |
| Low Attendees | 22 (41.5%) | 15 (46.9%) | 0 | 0 | 6 | 4 | 16 | 11 |
| rural | 9 (40.9%) | 5 (33.3%) | 0 | 0 | 2 | 1 | 7 | 4 |
| regional | 3 (13.6%) | 2 (13.3%) | 0 | 0 | 1 | 0 | 2 | 2 |
| urban | 10 (45.5%) | 8 (53.3%) | 0 | 0 | 3 | 3 | 7 | 5 |
| High Attendees | 24 (45.3%) | 15 (46.9%) | 5 | 2 | 10 | 7 | 9 | 6 |
| rural | 15 (62.5%) | 7 (46.7%) | 3 | 1 | 5 | 2 | 7 | 4 |
| regional | 1 (4.2%) | 1 (6.7%) | 0 | 0 | 1 | 1 | 0 | 0 |
| urban | 8 (33.3%) | 7 (46.7%) | 2 | 1 | 4 | 4 | 2 | 2 |
| Themes | Enablers | Barriers |
|---|---|---|
| Transition to Parenthood (personal factors) | Need for information as a first-time parent | Being overwhelmed |
| Need for specific infant feeding information | Baby’s routine | |
| Need for social connections | Informal sources of information (family; internet; friends) | |
| Growing confidence as a parent | ||
| Returning to work | ||
| Program Processes (organisational factors) | Referral through maternal and child health service | Limited awareness of program |
| Recruitment via new parent groups | Recruitment of parents not attending new parent groups | |
| Opt-out (automatic) enrolment | Opt-in (self-referral) enrolment | |
| Text reminder notifications | Scheduling same-age infants | |
| Accessible venues | Limited session options (days/times) | |
| Program Processes (program factors) | Formal sources of information (maternal and child health nurse; dietitian) | Group facilitator parenting expertise |
| Group-based approach (shared experiences) | Aspects of program content | |
| Anticipatory guidance (timely information) | Frequency and spacing of sessions |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Love, P.; Laws, R.; Litterbach, E.; Campbell, K.J. Factors Influencing Parental Engagement in an Early Childhood Obesity Prevention Program Implemented at Scale: The Infant Program. Nutrients 2018, 10, 509. https://doi.org/10.3390/nu10040509
Love P, Laws R, Litterbach E, Campbell KJ. Factors Influencing Parental Engagement in an Early Childhood Obesity Prevention Program Implemented at Scale: The Infant Program. Nutrients. 2018; 10(4):509. https://doi.org/10.3390/nu10040509
Chicago/Turabian StyleLove, Penelope, Rachel Laws, Eloise Litterbach, and Karen J. Campbell. 2018. "Factors Influencing Parental Engagement in an Early Childhood Obesity Prevention Program Implemented at Scale: The Infant Program" Nutrients 10, no. 4: 509. https://doi.org/10.3390/nu10040509





