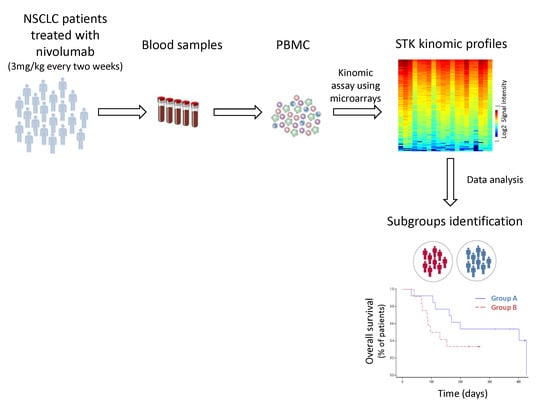
Differential Kinase Activation in Peripheral Blood Mononuclear Cells from Non-Small-Cell Lung Cancer Patients Treated with Nivolumab
Abstract
:1. Introduction
2. Results
2.1. Patients
2.2. Basal Kinomic Activity Profiles in NSCLC Patients
2.3. Comparison between Baseline Kinomic Profiles from Healthy Volunteers and NSCLC Patients
2.4. Inhibition Profiles in NSCLC Patients at Day 14
2.5. Relationship between Efficacy and Kinomic Profile
3. Discussion
4. Methods
4.1. Population and Study Design
4.2. Ethics Statement
4.3. Treatment Schedule
4.4. Efficacy Assessment
4.5. Nivolumab Concentration Assay in Plasma
4.6. Sample Collection and Processing for Kinomic Profiling
4.7. Statistical Analysis
4.7.1. Kinomic Approach
4.7.2. Survival Endpoint
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, F.R.; Suda, K.; Wiens, J.; Bunn, P.A. New and emerging targeted treatments in advanced non-small-cell lung cancer. Lancet 2016, 388, 1012–1024. [Google Scholar] [CrossRef]
- Pennell, N.A. Understanding the Rationale for Immunotherapy in Non-Small Cell Lung Cancer. Semin. Oncol. 2015, 42, S3–S10. [Google Scholar] [CrossRef]
- Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 2012, 12, 252–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brahmer, J.; Reckamp, K.L.; Baas, P.; Crinò, L.; Eberhardt, W.E.E.; Poddubskaya, E.; Antonia, S.; Pluzanski, A.; Vokes, E.E.; Holgado, E.; et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 373, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Borghaei, H.; Paz-Ares, L.; Horn, L.; Spigel, D.R.; Steins, M.; Ready, N.E.; Chow, L.Q.; Vokes, E.E.; Felip, E.; Holgado, E.; et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015, 373, 1627–1639. [Google Scholar] [CrossRef]
- Goeree, R.; Villeneuve, J.; Goeree, J.; Penrod, J.R.; Orsini, L.; Tahami Monfared, A.A. Economic evaluation of nivolumab for the treatment of second-line advanced squamous NSCLC in Canada: A comparison of modeling approaches to estimate and extrapolate survival outcomes. J. Med. Econ. 2016, 19, 630–644. [Google Scholar] [CrossRef]
- Matter-Walstra, K.; Schwenkglenks, M.; Aebi, S.; Dedes, K.; Diebold, J.; Pietrini, M.; Klingbiel, D.; von Moos, R.; Gautschi, O. Swiss Group for Clinical Cancer Research A Cost-Effectiveness Analysis of Nivolumab versus Docetaxel for Advanced Nonsquamous NSCLC Including PD-L1 Testing. J. Thorac. Oncol. 2016, 11, 1846–1855. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef]
- Carbone, D.P.; Reck, M.; Paz-Ares, L.; Creelan, B.; Horn, L.; Steins, M.; Felip, E.; van den Heuvel, M.M.; Ciuleanu, T.-E.; Badin, F.; et al. First-Line Nivolumab in Stage IV or Recurrent Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 376, 2415–2426. [Google Scholar] [CrossRef] [PubMed]
- Saelen, M.G.; Flatmark, K.; Folkvord, S.; De Wijn, R.; Rasmussen, H.; Fodstad, Ø.; Ree, A.H. Tumor kinase activity in locally advanced rectal cancer: Angiogenic signaling and early systemic dissemination. Angiogenesis 2011, 14, 481–489. [Google Scholar] [CrossRef]
- Folkvord, S.; Flatmark, K.; Dueland, S.; De Wijn, R.; Groholt, K.K.; Hole, K.H.; Nesland, J.M.; Ruijtenbeek, R.; Boender, P.J.; Johansen, M.; et al. Prediction of response to preoperative chemoradiotherapy in rectal cancer by multiplex kinase activity profiling. Int. J. Radiat. Oncol. Biol. Phys. 2010, 78, 555–562. [Google Scholar] [CrossRef]
- Noé, G.; Bellesoeur, A.; Thomas-Schoemann, A.; Naji, F.; Puszkiel, A.; Huillard, O.; Saidu, N.; Alexandre, J.; Goldwasser, F.; Blanchet, B.; et al. Clinical and kinomic analysis identifies peripheral blood mononuclear cells as a potential pharmacodynamic biomarker in metastatic renal cell carcinoma patients treated with sunitinib. Oncotarget 2016, 7, 67507–67520. [Google Scholar] [CrossRef] [Green Version]
- Anderson, J.C.; Willey, C.D.; Mehta, A.; Welaya, K.; Chen, D.; Duarte, C.W.; Ghatalia, P.; Arafat, W.; Madan, A.; Sudarshan, S.; et al. High Throughput Kinomic Profiling of Human Clear Cell Renal Cell Carcinoma Identifies Kinase Activity Dependent Molecular Subtypes. PLoS ONE 2015, 10, e0139267. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.C.; Taylor, R.B.; Fiveash, J.B.; de Wijn, R.; Gillespie, G.Y.; Willey, C.D. Kinomic alterations in atypical meningioma. Med. Res. Arch. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.C.; Minnich, D.J.; Dobelbower, M.C.; Denton, A.J.; Dussaq, A.M.; Gilbert, A.N.; Rohrbach, T.D.; Arafat, W.; Welaya, K.; Bonner, J.A.; et al. Kinomic profiling of electromagnetic navigational bronchoscopy specimens: A new approach for personalized medicine. PLoS ONE 2014, 9, e116388. [Google Scholar]
- Tahiri, A.; Roe, K.; Ree, A.H.; de Wijn, R.; Risberg, K.; Busch, C.; Lonning, P.E.; Kristensen, V.; Geisler, J.; Roe, K.; et al. Differential Inhibition of Ex-Vivo Tumor Kinase Activity by Vemurafenib in BRAF (V600E) and BRAF Wild-Type Metastatic Malignant Melanoma. PLoS ONE 2013, 8, e0072692. [Google Scholar] [CrossRef] [PubMed]
- Hilhorst, R.; Schaake, E.; van Pel, R.; Nederlof, R.; Houkes, L.; Mommersteeg, M.; de Wijn, R.; van den Heuvel, R.; Baas, P.; Ruijtenbeek, R.; et al. Blind prediction of response to erlotinib in early stage non-small cell lung cancer (NSCLC) in a neoadjuvant setting based on kinase activity profiles. J. Clin. Oncol. 2010, 29, 10521. [Google Scholar] [CrossRef]
- Hilhorst, R.; Schaake, E.; Pel, V.; Nederlof, P.; Houkes, L.; de Wijn, R.; Ruijtenbeek, R.; van den Heuvel, M.; Baas, P.; Klomp, H.M. Application of kinase activity profiles to predict response to erlotinib in a neoadjuvant setting in early stage non-small-cell lung cancer (NSCLC). J. Clin. Oncol. 2011, 28, 10566. [Google Scholar] [CrossRef]
- Sacher, A.G.; Gandhi, L. Biomarkers for the Clinical Use of PD-1/PD-L1 Inhibitors in Non–Small-Cell Lung Cancer. JAMA Oncol. 2016, 2, 1217–1222. [Google Scholar] [CrossRef]
- Paulsen, E.-E.; Kilvaer, T.K.; Khanehkenari, M.R.; Al-Saad, S.; Hald, S.M.; Andersen, S.; Richardsen, E.; Ness, N.; Busund, L.-T.; Bremnes, R.M.; et al. Assessing PDL-1 and PD-1 in Non-Small Cell Lung Cancer: A Novel Immunoscore Approach. Clin. Lung Cancer 2016, 18, 220–233. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Fishman, M.N.; Escudier, B.; McDermott, D.F.; Drake, C.G.; Kluger, H.; Stadler, W.M.; Perez-Gracia, J.L.; McNeel, D.G.; Curti, B.; et al. Immunomodulatory Activity of Nivolumab in Metastatic Renal Cell Carcinoma. Clin. Cancer Res. 2016, 22, 5461–5471. [Google Scholar] [CrossRef] [Green Version]
- Chevolet, I.; Speeckaert, R.; Schreuer, M.; Neyns, B.; Krysko, O.; Bachert, C.; Hennart, B.; Allorge, D.; van Geel, N.; Van Gele, M.; et al. Characterization of the in vivo immune network of IDO, tryptophan metabolism, PD-L1, and CTLA-4 in circulating immune cells in melanoma. Oncoimmunology 2015, 4, e982382. [Google Scholar] [CrossRef]
- Jacquelot, N.; Roberti, M.P.; Enot, D.P.; Rusakiewicz, S.; Ternès, N.; Jegou, S.; Woods, D.M.; Sodré, A.L.; Hansen, M.; Meirow, Y.; et al. Predictors of responses to immune checkpoint blockade in advanced melanoma. Nat. Commun. 2017, 8, 592. [Google Scholar] [CrossRef]
- Tanizaki, J.; Haratani, K.; Hayashi, H.; Chiba, Y.; Nakamura, Y.; Yonesaka, K.; Kudo, K.; Kaneda, H.; Hasegawa, Y.; Tanaka, K.; et al. Peripheral Blood Biomarkers Associated with Clinical Outcome in Non–Small Cell Lung Cancer Patients Treated with Nivolumab. J. Thorac. Oncol. 2018, 13, 97–105. [Google Scholar] [CrossRef]
- Diem, S.; Schmid, S.; Krapf, M.; Flatz, L.; Born, D.; Jochum, W.; Templeton, A.J.; Früh, M. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer 2017, 111, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Cedrés, S.; Torrejon, D.; Martínez, A.; Martinez, P.; Navarro, A.; Zamora, E.; Mulet-Margalef, N.; Felip, E. Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clin. Transl. Oncol. 2012, 14, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Voron, T.; Colussi, O.; Marcheteau, E.; Pernot, S.; Nizard, M.; Pointet, A.-L.; Latreche, S.; Bergaya, S.; Benhamouda, N.; Tanchot, C.; et al. VEGF-A modulates expression of inhibitory checkpoints on CD8+ T cells in tumors. J. Exp. Med. 2015, 212, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Tartour, E.; Pere, H.; Maillere, B.; Terme, M.; Merillon, N.; Taieb, J.; Sandoval, F.; Quintin-Colonna, F.; Lacerda, K.; Karadimou, A.; et al. Angiogenesis and immunity: A bidirectional link potentially relevant for the monitoring of antiangiogenic therapy and the development of novel therapeutic combination with immunotherapy. Cancer Metastasis Rev. 2011, 30, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Patsoukis, N.; Li, L.; Sari, D.; Petkova, V.; Boussiotis, V.A. PD-1 increases PTEN phosphatase activity while decreasing PTEN protein stability by inhibiting casein kinase 2. Mol. Cell. Biol. 2013, 33, 3091–3098. [Google Scholar] [CrossRef]
- Parry, R.V.; Chemnitz, J.M.; Frauwirth, K.A.; Lanfranco, A.R.; Braunstein, I.; Kobayashi, S.V.; Linsley, P.S.; Thompson, C.B.; Riley, J.L. CTLA-4 and PD-1 Receptors Inhibit T-Cell Activation by Distinct Mechanisms. Mol. Cell. Biol. 2005, 25, 9543–9553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abiko, K.; Matsumura, N.; Hamanishi, J.; Horikawa, N.; Murakami, R.; Yamaguchi, K.; Yoshioka, Y.; Baba, T.; Konishi, I.; Mandai, M. IFN-γ from lymphocytes induces PD-L1 expression and promotes progression of ovarian cancer. Br. J. Cancer 2015, 112, 1501–1509. [Google Scholar] [CrossRef]
- Huang, W.-C.; Hung, M.-C. Induction of Akt activity by chemotherapy confers acquired resistance. J. Formos. Med. Assoc. 2009, 108, 180–194. [Google Scholar] [CrossRef]
- Yan, Z.-X.; Zheng, Z.; Xue, W.; Zhao, M.-Z.; Fei, X.-C.; Wu, L.-L.; Huang, L.-M.; Leboeuf, C.; Janin, A.; Wang, L.; et al. MicroRNA181a Is Overexpressed in T-Cell Leukemia/Lymphoma and Related to Chemoresistance. Biomed Res. Int. 2015, 2015, 197241. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Shen, C.; Zhu, B.; Shi, F.; Eisen, H.N.; Chen, J. Persistent Antigen and Prolonged AKT-mTORC1 Activation Underlie Memory CD8 T Cell Impairment in the Absence of CD4 T Cells. J. Immunol. 2015, 195, 1591–1598. [Google Scholar] [CrossRef] [PubMed]
- Puszkiel, A.; Noé, G.; Boudou-Rouquette, P.; Le Cossec, C.; Arrondeau, J.; Giraud, S.; Alexandre, J.; Vidal, M.; Goldwasser, F.; Blanchet, B. Evaluation of the interindividual variability in plasma nivolumab level in non-small-lung cancer outpatients: Preliminary results. Ann. Oncol. 2016, 27. [Google Scholar] [CrossRef]




| Characteristics | n = 28 |
|---|---|
| Demographic data | |
| Sex | |
| Male | 17 (61%) |
| Female | 11 (39%) |
| Age (years) Age > 70 years-old | 67 (63–69) 6 (21%) |
| BMI (kg/m2) Lean Body mass (kg) | 22.9 (19.9–24.1) 49.4 (42.2–56.4) |
| Smoking status | |
| Current smoker | 6 (21%) |
| Former smoker | 17 (61%) |
| Never smoker | 3 (11%) |
| Not available | 2 (7%) |
| ECOG performance status | |
| 0–1 | 14 (50%) |
| 2 | 14 (50%) |
| Non-small-cell lung cancer characteristics | |
| Histological tumor type | |
| Squamous cell carcinoma | 8 (29%) |
| Adenocarcinoma | 20 (71%) |
| Metastasis Synchronous Metachronous Initial surgery Yes No Number of previous treatment lines 1 2 >2 | 19 (68%) 9 (32%) 10 (36%) 18 (64%) 14 (50%) 8 (29%) 6 (21%) |
| Previous Targeted Therapy | |
| Tyrosine Kinase Inhibitor a | 4 (14%) |
| Monoclonal antibody (bevacizumab) | 11 (39%) |
| None | 14 (50%) |
| Number of metastatic sites | |
| 1 | 4 (14%) |
| 2 | 15 (54%) |
| ≥3 | 9 (32%) |
| Cerebral metastasis | |
| Yes | 9 (32%) |
| No | 19 (68%) |
| Baseline Biological Data | |
| Haemoglobin (g/dL) | 12.9 (11.6–14.3) |
| Platelets (×109/L) | 231 (204–298) |
| Lymphocytes (×109/L) | 1.26 (0.98–1.65) |
| Neutrophils (×109/L) | 5.38 (4.28–6.32) |
| Lymphopenia (<1 × 109/L) before Nivolumab, n (%) LDH Increased above ULN Normal Non available | 8 (29%) 12 (43%) 10 (36%) 6 (21%) |
| Characteristics | Cluster A (n = 14) | Cluster B (n = 14) | p Value |
|---|---|---|---|
| Sex (female) (%) | 50.0 | 71.4 | 0.44 |
| Age (years old) | 66 (63–74) | 68 (62–69) | 1.0 |
| Total body weight (kg) | 65 (53–68) | 71 (62–74) | 0.038 |
| ECOG performance status | 0.26 | ||
| 0–1 | 9 (64%) | 5 (36%) | |
| >1 | 5 (36%) | 9 (64%) | |
| Current/former Smoker (%) | 77.0 | 100.0 | 0.22 |
| Histological tumor type | 1.0 | ||
| Adenocarcinoma | 10 (71.4%) | 10 (71.4%) | |
| Squamous cell carcinoma | 4 (28.6%) | 4 (28.6%) | |
| PD-L1 TC score | 0.5 (0–5) | 10 (1.5–75) | 0.045 |
| Presence of molecular alteration * (%) | 36.4 | 27.3 | 1.0 |
| Time to metastasis (days) | 0 (0–243) | 0 (0–273) | 0.74 |
| Number of metastatic sites | 1.0 | ||
| 1–2 | 10 (71.4%) | 9 (64.3%) | |
| >2 | 4 (28.6%) | 5 (35.7%) | |
| Number of previous treatment line | 0.71 | ||
| 1–2 | 6 (42.9%) | 8 (57.1%) | |
| >2 | 8 (57.1%) | 6 (42.9%) | |
| Previous targeted therapy | |||
| Tyrosine kinase inhibitor (%) | 21.4 | 7.4 | 0.59 |
| Bevacizumab (%) | 36.0 | 43.0 | 1.0 |
| Corticosteroids treatment (%) | 14.3 | 21.4 | 1.0 |
| Baseline biological characteristics | |||
| C reactive protein (mg/L) | 10.4 (1.3–15.4) | 5.4 (3.2–31.9) | 0.73 |
| LDH (UI) | 218 (193–267) | 210 (197–303) | 0.84 |
| Albumin (g/L) | 42 (40–45) | 38 (36–42) | 0.07 |
| Neutrophils count (cells/mm3) | 5180 (3820–6310) | 5850 (5160–6350) | 0.57 |
| Lymphocytes count (cells/mm3) | 1510 (1050–2020) | 1140 (610–1460) | 0.09 |
| Neutrophils-lymphocytes ratio (NLR) | 4.1 (2.3–5.4) | 5.1 (3.6–7.0) | 0.23 |
| CD3+ cells count (cells/mm3) | 1069 (750–1402) | 822 (447–959) | 0.14 |
| CD4+ cells count (cells/mm3) | 701 (301–914) | 460 (235–640) | 0.17 |
| CD8+ cells count (cells/mm3) | 365 (218–439) | 137 (95–327) | 0.023 |
| B cells count (cells/mm3) | 114 (88–204) | 92 (34–170) | 0.13 |
| NK count (cells/mm3) | 129 (82–145) | 101 (64–153) | 0.47 |
| Proportion of CD3+ cells (%) | 77.9 (70.9–85.6) | 84.2 (76.7–90.8) | 0.22 |
| Proportion of CD4+ cells (%) | 43.5 (36.6–54.7) | 61.9 (35.2–69.2) | 0.21 |
| Proportion of CD8+ cells (%) | 27.8 (17.9–35.5) | 18.0 (10.4–36.7) | 0.18 |
| Proportion of NK cells (%) | 9.2 (5.0–14.0) | 9.6 (6.1–15.7) | 0.66 |
| Proportion of B cells (%) | 11.2 (6.6–21.9) | 10.6 (7.7–13.0) | 0.56 |
| Characteristics | Cluster C (n = 10) | Cluster D (n = 18) | p Value |
|---|---|---|---|
| Sex (female) (%) | 70.0 | 55.5 | 0.69 |
| Age (years old) | 68 (64–70) | 65 (62–69) | 0.43 |
| Total body weight (kg) | 68 (61–71) | 68 (54–73) | 0.90 |
| ECOG performance status | 0.24 | ||
| 0–1 | 3 (30%) | 11 (61.1%) | |
| >1 | 7 (70%) | 7 (38.9%) | |
| Current/former Smoker (%) | 88.9 | 88.2 | 1.0 |
| Histological tumor type | 0.40 | ||
| Adenocarcinoma | 6 (60.0%) | 14 (77.8%) | |
| Squamous cell carcinoma | 4 (40.0%) | 4 (22.2%) | |
| Presence of molecular alteration * (%) | 33.3 | 31.3 | 1.0 |
| Time to metastasis (days) | 0 (0–92) | 0 (0–273) | 0.82 |
| Number of metastatic sites, | 0.42 | ||
| 1–2 | 8 (80%) | 11 (61.1%) | |
| >2 | 2 (20%) | 7 (38.9%) | |
| Number of previous treatment line, | 1.0 | ||
| 1–2 | 5 (50%) | 9 (50%) | |
| >2 | 5 (50%) | 9 (50%) | |
| Previous targeted therapy | |||
| Tyrosine kinase inhibitors (%) | 20.0 | 11.1 | 0.60 |
| Bevacizumab (%) | 0 | 55.6 | 0.011 |
| Corticosteroids treatment (%) | 0 | 27.8 | 0.13 |
| Biological characteristics on day 14 | |||
| Plasma concentration of nivolumab (mg/L) on day 14 | 15.8 (13.0–22.9) | 15.9 (12.4–18.8) | 0.58 |
| C reactive protein (mg/L) | 6.5 (1.6–19.9) | 11.9 (5.3–28.3) | 0.40 |
| LDH (UI) | 265 (198–305) | 198 (168–244) | 0.28 |
| Albumin (g/L) | 39 (36–41) | 36 (34–40) | 0.25 |
| Neutrophils count (cells/mm3) | 5160 (4580–5870) | 4960 (4560–5980) | 0.92 |
| Lymphocytes count (cells/mm3) | 990 (860–1230) | 1330 (790–1650) | 0.41 |
| Neutrophils-lymphocytes ratio (NLR) | 4.25 (3.60–7.80) | 4.20 (3.20–6.20) | 0.71 |
| CD3+ cells count (cells/mm3) | 702 (637–846) | 894 (503–1222) | 0.29 |
| CD4+ cells count (cells/mm3) | 541 (394–618) | 609 (207–806) | 0.76 |
| CD8+ cells count (cells/mm3) | 140 (102–288) | 339 (195–453) | 0.05 |
| B cells count (cells/mm3) | 92 (59–122) | 90 (59–184) | 1.0 |
| NK count (cells/mm3) | 113 (100–160) | 106 (68–177) | 0.66 |
| Proportion of CD3+ cells (%) | 81.3 (75.2–94.4) | 80.1 (60.6–88.7) | 0.76 |
| Proportion of CD4+ cells (%) | 52.8 (43.4–59.4) | 43.0 (31.9–56.4) | 0.18 |
| Proportion of CD8+ cells (%) | 17.0 (14.6–27.0) | 29.4 (17.9–42.1) | 0.11 |
| Proportion of NK cells (%) | 11.1 (8.5–15.5) | 9.8 (5.5–16.2) | 0.50 |
| Proportion of B cells (%) | 10.2 (5.9–11.7) | 8.3 (5.9–14.6) | 0.54 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noé, G.; Bellesoeur, A.; Golmard, L.; Thomas-Schoemann, A.; Boudou-Rouquette, P.; Tiako Meyo, M.; Puszkiel, A.; Arrondeau, J.; Alexandre, J.; Goldwasser, F.; et al. Differential Kinase Activation in Peripheral Blood Mononuclear Cells from Non-Small-Cell Lung Cancer Patients Treated with Nivolumab. Cancers 2019, 11, 762. https://doi.org/10.3390/cancers11060762
Noé G, Bellesoeur A, Golmard L, Thomas-Schoemann A, Boudou-Rouquette P, Tiako Meyo M, Puszkiel A, Arrondeau J, Alexandre J, Goldwasser F, et al. Differential Kinase Activation in Peripheral Blood Mononuclear Cells from Non-Small-Cell Lung Cancer Patients Treated with Nivolumab. Cancers. 2019; 11(6):762. https://doi.org/10.3390/cancers11060762
Chicago/Turabian StyleNoé, Gaëlle, Audrey Bellesoeur, Lisa Golmard, Audrey Thomas-Schoemann, Pascaline Boudou-Rouquette, Manuela Tiako Meyo, Alicja Puszkiel, Jennifer Arrondeau, Jérome Alexandre, François Goldwasser, and et al. 2019. "Differential Kinase Activation in Peripheral Blood Mononuclear Cells from Non-Small-Cell Lung Cancer Patients Treated with Nivolumab" Cancers 11, no. 6: 762. https://doi.org/10.3390/cancers11060762