Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Question
2.2. Protocol Registration
2.3. Literature Search Strategy
2.4. Selection Criteria
2.5. Data Extraction and Data Synthesis
2.6. Risk-of-Bias Assessment
2.7. Outcomes
3. Results
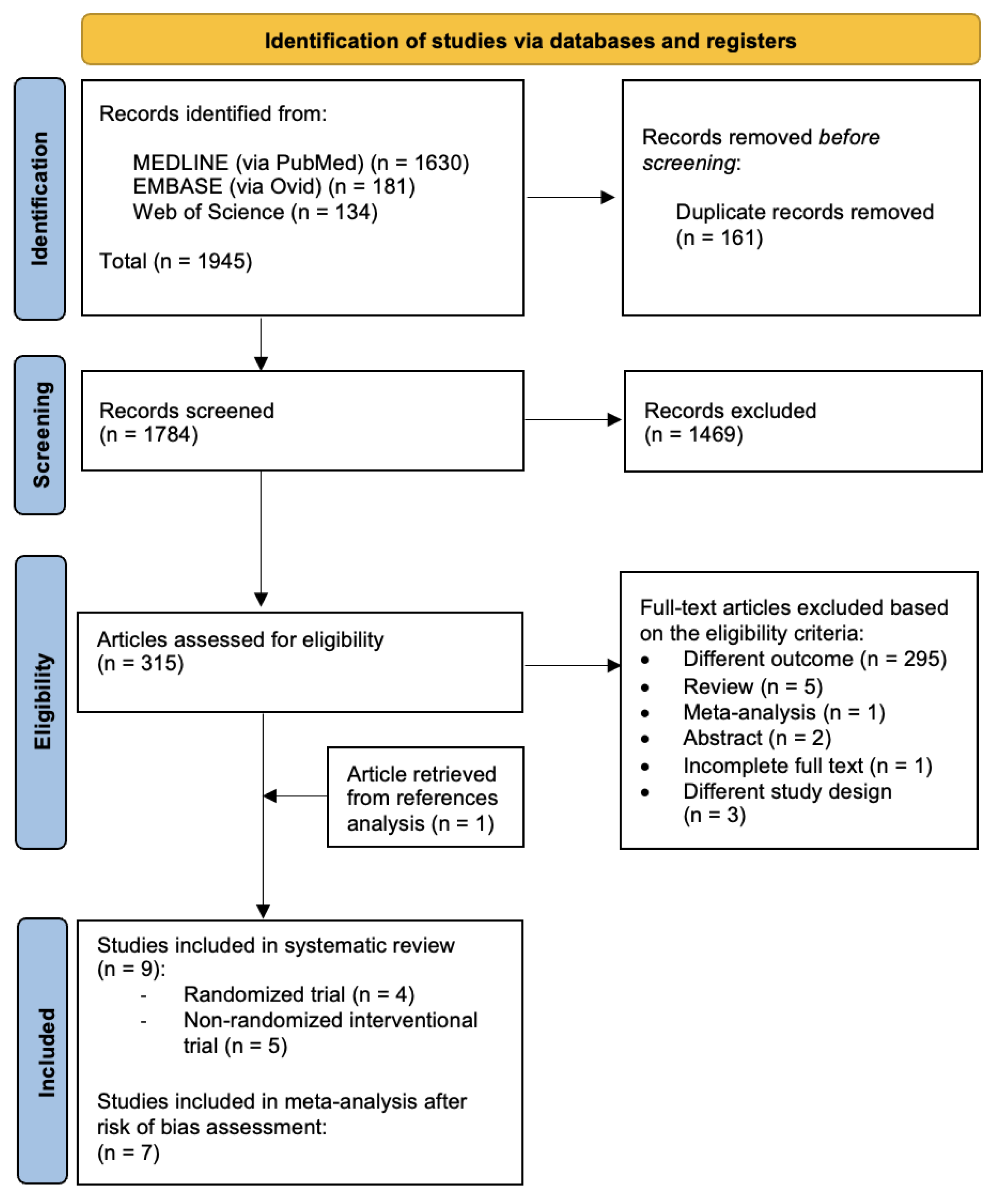
3.1. Study Selection
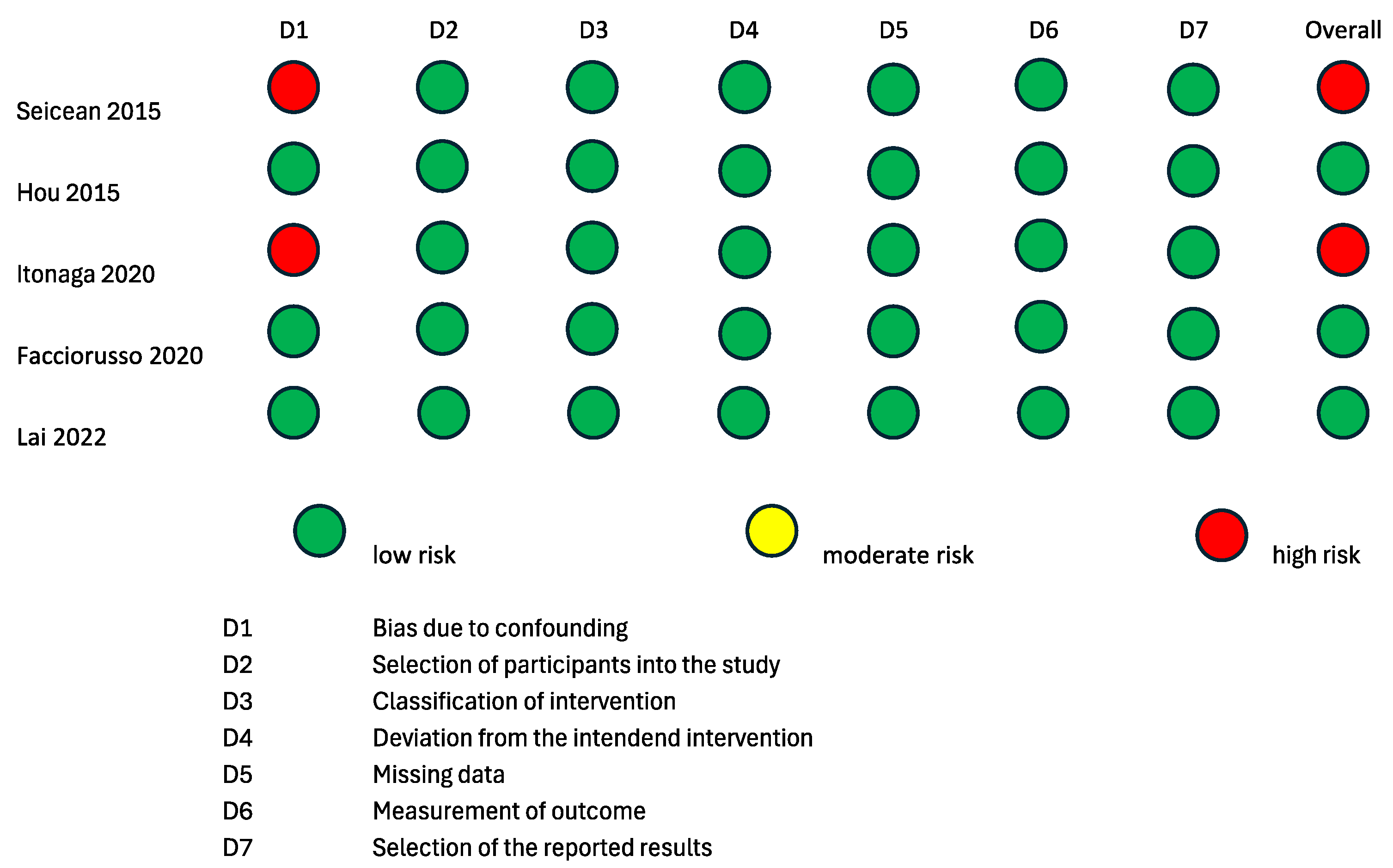
3.2. Risk-of-Bias Assessment
3.3. ECEUS vs. Standard FNA or Biopsy of Pancreatic Solid Lesions: Qualitative Summary
3.4. ECEUS vs. Standard FNA or Biopsy of Pancreatic Solid Lesions: Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Roessel, S.; Soer, E.C.; Daamen, L.A.; van Dalen, D.; Sarasqueta, A.F.; Stommel, M.W.; Molenaar, I.Q.; van Santvoort, H.C.; van de Vlasakker, V.C.; de Hingh, I.H.; et al. Preoperative misdiagnosis of pancreatic and periampullary cancer in patients undergoing pancreatoduodenectomy: A multicentre retrospective cohort study. Eur. J. Surg. Oncol. 2021, 47, 2525–2532. [Google Scholar] [CrossRef] [PubMed]
- Wolske, K.M.; Ponnatapura, J.; Kolokythas, O.; Burke, L.M.B.; Tappouni, R.; Lalwani, N. Chronic pancreatitis or pancreatic tumor? A problem-solving approach. Radiographics 2019, 39, 1965–1982. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.-M.; Deprez, P.H.; Jenssen, C.; Iglesias-Garcia, J.; Larghi, A.; Vanbiervliet, G.; Aithal, G.P.; Arcidiacono, P.G.; Bastos, P.; Carrara, S.; et al. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated January 2017. Endoscopy 2017, 49, 695–714. [Google Scholar] [CrossRef]
- Eloubeidi, M.A.; Decker, G.A.; Chandrasekhara, V.; Chathadi, K.V.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; Foley, K.; Hwang, J.H.; et al. The role of endoscopy in the evaluation and management of patients with solid pancreatic neoplasia Prepared by. Gastrointest. Endosc. 2016, 83, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Yousri, M.; Abusinna, E.; Tahoun, N.; Okasha, H.H.; El-Habashi, A.H. A Comparative Study of the Diagnostic Utility of Endoscopic Ultrasound-Guided Fine Needle Aspiration Cytology (EUS-FNA) versus Endoscopic Ultrasound-Guided Fine Needle Biopsy (EUS-FNB) in Pancreatic and Non-Pancreatic Lesions. Asian Pac. J. Cancer Prev. 2022, 23, 2151–2158. [Google Scholar] [CrossRef]
- Pagano, N.; Ricci, C.; Ingaldi, C.; Sadalla, S.; Fabbri, A.; Alberici, L.; Impellizeri, G.; Pallio, S.; Zagari, R.M.; De Leo, A.; et al. Performance of EUS-FNB in solid pancreatic masses: A lesson from 463 consecutive procedures and a practical nomogram. Updates Surg. 2022, 74, 945–952. [Google Scholar] [CrossRef]
- Van Riet, P.A.; Larghi, A.; Attili, F.; Rindi, G.; Nguyen, N.Q.; Ruszkiewicz, A.; Kitano, M.; Chikugo, T.; Aslanian, H.; Farrell, J.; et al. A multicenter randomized trial comparing a 25-gauge EUS fine-needle aspiration device with a 20-gauge EUS fine-needle biopsy device. Gastrointest. Endosc. 2019, 89, 329–339. [Google Scholar] [CrossRef]
- Facciorusso, A.; Bajwa, H.S.; Menon, K.; Buccino, V.R.; Muscatiello, N. Comparison between 22G aspiration and 22G biopsy needles for EUS-guided sampling of pancreatic lesions: A meta-analysis. Endosc. Ultrasound. 2020, 9, 167–174. [Google Scholar] [CrossRef]
- Farnes, I.; Paulsen, V.; Verbeke, C.S.; Tønnesen, C.J.; Aabakken, L.; Labori, K.J. Performance and safety of diagnostic EUS FNA/FNB and therapeutic ERCP in patients with borderline resectable and locally advanced pancreatic cancer—Results from a population-based, prospective cohort study. Scand. J. Gastroenterol. 2024, 59, 496–502. [Google Scholar] [CrossRef]
- Archibugi, L.; Ponz de Leon Pisani, R.; Petrone, M.C.; Balzano, G.; Falconi, M.; Doglioni, C.; Capurso, G.; Arcidiacono, P.G. Needle-Tract Seeding of Pancreatic Cancer after EUS-FNA: A Systematic Review of Case Reports and Discussion of Management. Cancers 2022, 14, 6130. [Google Scholar] [CrossRef]
- Yamashita, Y.; Kitano, M. Role of contrast-enhanced harmonic endoscopic ultrasonography (EUS) and EUS elastography in pancreatic lesions. Clin. Endosc. 2024, 57, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Eloubeidi, M.A.; Decker, G.A.; Chandrasekhara, V.; Chathadi, K.V.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; Foley, K.; Hwang, J.H.; et al. Contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration versus standard fine-needle aspiration in pancreatic masses: A meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2021, 15, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Li, Q.; Liu, Y.; Han, J.; Zheng, W.; Huang, Y.; Zheng, X.; Cao, L.; Zhou, J.H. Distinguishing intrahepatic cholangiocarcinoma from hepatocellular carcinoma in patients with and without risks: The evaluation of the LR-M criteria of contrast-enhanced ultrasound liver imaging reporting and data system version 2017. Eur. Radiol. 2020, 30, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.P.; Lee, W.J.; Meloni, M.F.; Clevert, D.A.; Chammas, M.C.; Tannapfel, A.; Forgione, A.; Piscaglia, F.; Dietrich, C.F. Contrast-Enhanced Ultrasound Features of Histopathologically Proven Hepatocellular Carcinoma in the Non-cirrhotic Liver: A Multicenter Study. Ultrasound Med. Biol. 2022, 48, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, M.; Takagi, T.; Hikichi, T.; Suzuki, R.; Watanabe, K.; Nakamura, J.; Kikuchi, H.; Konno, N.; Waragai, Y.; Watanabe, H.; et al. Conventional versus contrast-enhanced harmonic endoscopic ultrasonography-guided fine-needle aspiration for diagnosis of solid pancreatic lesions: A prospective randomized trial. Pancreatology 2015, 15, 538–541. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.R.; Jeong, S.H.; Kang, H.; Kim, E.J.; Kim, Y.S.; Cho, J.H. Comparison of contrast-enhanced versus conventional EUS-guided FNA/fine-needle biopsy in diagnosis of solid pancreatic lesions: A randomized controlled trial. Gastrointest. Endosc. 2021, 94, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Seicean, A.; Samarghitan, A.; Bolboacă, S.D.; Pojoga, C.; Rusu, I.; Rusu, D.; Sparchez, Z.; Gheorghiu, M.; Al Hajjar, N.; Seicean, R. Contrast-enhanced harmonic versus standard endoscopic ultrasound-guided fine-needle aspiration in solid pancreatic lesions: A single-center prospective randomized trial. Endoscopy 2020, 52, 1084–1090. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.T.; Chu, Y.L.; Wong, W.F.; Han, M.L.; Chen, C.C.; Jan, I.S.; Cheng, W.C.; Shun, C.T.; Tsai, M.C.; Cheng, T.Y.; et al. Randomized trial of contrast-enhanced harmonic guidance versus fanning technique for EUS-guided fine-needle biopsy sampling of solid pancreatic lesions. Gastrointest. Endosc. 2023, 97, 732–740. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Jin, Z.; Xu, C.; Zhang, M.; Zhu, J.; Jiang, F.; Li, Z. Contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of solid pancreatic lesions: A retrospective study. PLoS ONE 2015, 10, e0121236. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seicean, A.; Badea, R.; Moldovan-Pop, A.; Vultur, S.; Botan, E.C.; Zaharie, T.; Săftoiu, A.; Mocan, T.; Iancu, C.; Graur, F.; et al. Harmonic Contrast-Enhanced Endoscopic Ultrasonography for the Guidance of Fine-Needle Aspiration in Solid Pancreatic Masses. Ultraschall. Med. 2017, 38, 174–182. (In English) [Google Scholar] [CrossRef] [PubMed]
- Facciorusso, A.; Cotsoglou, C.; Chierici, A.; Mare, R.; Crinò, S.F.; Muscatiello, N. Contrast-Enhanced Harmonic Endoscopic Ultrasound-Guided Fine-Needle Aspiration versus Standard Fine-Needle Aspiration in Pancreatic Masses: A Propensity Score Analysis. Diagnostics 2020, 10, 792. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lai, J.H.; Lin, C.C.; Lin, H.H.; Chen, M.J. Is contrast-enhanced endoscopic ultrasound-guided fine needle biopsy better than conventional fine needle biopsy? A retrospective study in a medical center. Surg. Endosc. 2022, 36, 6138–6143. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Itonaga, M.; Kitano, M.; Kojima, F.; Hatamaru, K.; Yamashita, Y.; Tamura, T.; Nuta, J.; Kawaji, Y.; Shimokawa, T.; Tanioka, K.; et al. The usefulness of EUS-FNA with contrast-enhanced harmonic imaging of solid pancreatic lesions: A prospective study. J. Gastroenterol. Hepatol. 2020, 35, 2273–2280. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Author, Year | Study Design | Outcomes | Number of Patients | Procedure Type |
|---|---|---|---|---|
| Sugimoto et al., 2015 [15] | Prospective randomized |
| 40 | ECEUS-FNA (20 patients) - EUS-FNA (20 patients) |
| Cho et al., 2021 [16] | Prospective randomized |
| 240 | ECEUS-FNA (120 patients) - EUS-FNA (120 patients) |
| Kuo et al., 2023 [18] | Prospective randomized |
| 118 | ECEUS-FNB (59 patients) - EUS-FNB with fanning technique (59 patients) |
| Seicean et al., 2020 [17] | Prospective randomized |
| 148 | ECEUS-FNA (74 patients) - EUS-FNA (74 patients) |
| Hou et al., 2015 [19] | Retrospective cohort study |
| 163 | ECEUS-FNA (58 patients) - EUS-FNA (105 patients) |
| Itonaga et al., 2020 [23] | Prospective cohort study |
| 93 | ECEUS-FNA (93 patients) - EUS-FNA (93 patients) |
| Seicean et al., 2015 [20] | Prospective cohort study |
| 51 | ECEUS-FNA (51 patients) - EUS-FNA (51 patients) |
| Facciorusso et al., 2020 [21] | Prospective cohort study |
| 206 | ECEUS-FNA (103 patients) - EUS-FNA (103 patients) |
| Lai et al., 2022 [22] | Retrospective cohort study |
| 133 (115 PL/18 RL) | ECEUS-FNB (40 PL-8 RL) - EUS-FNB (75 PL-10 RL) |
| Author, Year | Age (Years, SD) | Sex (Male, %) | Study Population |
|---|---|---|---|
| Sugimoto et al., 2015 [15] | 68.53 ± 10.2 | 15 (37.5%) | Solid pancreatic lesions |
| Cho et al., 2021 [16] | 67.30 ± 11.8 | 127 (52.9%) | Solid pancreatic lesions |
| Kuo et al., 2023 [18] | 64.4 ± 12.1 | 72 (61%) | Solid pancreatic lesions |
| Seicean et al., 2020 [17] | 64.5 ± 11.3 | 84 (56.8%) | Solid pancreatic lesions |
| Hou et al., 2015 [19] | 55.65 ± 12.1 | 99 (60.7%) | Solid pancreatic lesions |
| Itonaga et al., 2020 [23] | 61.4 ± 27.6 | 50 (53.8%) | Solid pancreatic lesions |
| Seicean et al., 2015 [20] | 61 ± 22 | 40 (68.9%) | Solid pancreatic lesions |
| Facciorusso et al., 2020 [21] | 66 ± 6 ECEUS 66 ± 8 EUS | 113 (54.8%) | Solid pancreatic lesions |
| Lai et al., 2022 [22] | 63.64 ± 12.58 | 72 (46.5%) | Solid pancreatic lesions and retroperitoneal lymph nodes |
| Author, Year | N° of Established Diagnoses | N° of Adverse Events | ||
|---|---|---|---|---|
| ECEUS | EUS | ECEUS | EUS | |
| Sugimoto et al., 2015 [15] | 20/20 (100%) | 20/20 (100%) | 0/20 (0%) | 0/20 (0%) |
| Cho et al., 2021 [16] | 120/120 (100%) | 120/120 (100%) | 3/120 (2.5%) | 3/120 (2.5%) |
| Kuo et al., 2023 [18] | 59/59 (100%) | 59/59 (100%) | 1/59 (1.7%) | 1/59 (1.7%) |
| Seicean et al., 2020 [17] | 113/148 (76.4%) | 112/148 (75.7%) | NR | NR |
| Hou et al., 2015 [19] | 56/58 (96.7%) | 91/105 (86.7%) | 0/58 (0%) | 0/105 (0%) |
| Itonaga et al., 2020 [23] | NR | NR | 1/93 (1.1%) | 1/93 (1.1%) |
| Seicean et al., 2015 [20] | 45/51 (88.2%) | 41/51 (80.4%) | 0/51 (0%) | 0/51 (0%) |
| Facciorusso et al., 2020 [21] | 92/103 (89.3%) | 85/103 (82.5%) | 0/103 (0%) | 0/103 (0%) |
| Lai et al., 2022 [22] | 38/40 (95%) | 69/75 (92%) | NR | NR |
| Author, Year | Cumulative Diagnostic Accuracy with Each Needle Pass, ECEUS-FNA/FNB | Cumulative Diagnostic Accuracy with Each Needle Pass, EUS-FNA/FNB | ||
|---|---|---|---|---|
| Needle Pass | Accuracy (%) | Needle Pass | Accuracy (%) | |
| Sugimoto et al., 2015 [15] | 1 | 12/20 (60%) | 1 | 5/20 (25%) |
| ≤2 | 15/20 (75%) | ≤2 | 13/20 (65%) | |
| ≤3 | 18/20 (90%) | ≤3 | 19/20 (95%) | |
| ≤4 | 20/20 (100%) | ≤4 | 19/20 (95%) | |
| ≤5 | 20/20 (100%) | ≤5 | 20/20 (100%) | |
| Cho et al., 2021 [16] | 1 | 84/120 (70%) | 1 | 80/120 (66.7%) |
| ≤2 | 96/120 (80%) | ≤2 | 100/120 (83.3%) | |
| ≤3 | 102/120 (85%) | ≤3 | 106/120 (88.3%) | |
| ≤4 | 103/120 (85.8%) | ≤4 | 106/120 (88.3%) | |
| ≤5 | 103/120 (85.8%) | ≤5 | 106/120 (88.3%) | |
| Kuo et al., 2023 [18] | 1 | 45/59 (76.3%) | 1 | 45/59 (72.9%) |
| ≤2 | 54/59 (91.5%) | ≤2 | 54/59 (91.5%) | |
| ≤3 | 55/59 (93.2%) | ≤3 | 55/59 (93.2%) | |
| ≤4 | 57/59 (93.2%) | ≤4 | 57/59 (96.6%) | |
| ≤5 | 57/59 (96.6%) | ≤5 | 57/59 (96.6%) | |
| ≤6 | 58/59 (98.3%) | ≤6 | 58/59 (98.3%) | |
| Inconclusive Diagnosis, n (%) | Established Diagnosis, n (%) | Total, n | |
|---|---|---|---|
| EUS-FNA | 74 (11.8) | 556 (88.3) | 630 |
| ECEUS-FNA | 50 (9.1) | 498 (90.9) | 548 |
| Total | 124 (10.5) | 1054 (89.5) | 1178 |
| Inconclusive Diagnosis at First Needle Pass, n (%) | Established Diagnosis at First Needle Pass, n (%) | Total, n | |
|---|---|---|---|
| EUS-FNA | 69 (34.7) | 130 (65.3) | 199 |
| ECEUS-FNA | 58 (29.2) | 141 (70.9) | 199 |
| Total | 127 (31.9) | 271 (68.1) | 398 |
| EUS-FNA/FNB (n = 551) | ECEUS-FNA/FNB (n = 504) | Total (n = 849) | p | |
|---|---|---|---|---|
| Adverse events, n (%) | 5 (0.9) | 5 (1.0) | 10 (1.0) | 0.86 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esposto, G.; Massimiani, G.; Galasso, L.; Santini, P.; Borriello, R.; Mignini, I.; Ainora, M.E.; Nicoletti, A.; Zileri Dal Verme, L.; Gasbarrini, A.; et al. Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis. Cancers 2024, 16, 1658. https://doi.org/10.3390/cancers16091658
Esposto G, Massimiani G, Galasso L, Santini P, Borriello R, Mignini I, Ainora ME, Nicoletti A, Zileri Dal Verme L, Gasbarrini A, et al. Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis. Cancers. 2024; 16(9):1658. https://doi.org/10.3390/cancers16091658
Chicago/Turabian StyleEsposto, Giorgio, Giuseppe Massimiani, Linda Galasso, Paolo Santini, Raffaele Borriello, Irene Mignini, Maria Elena Ainora, Alberto Nicoletti, Lorenzo Zileri Dal Verme, Antonio Gasbarrini, and et al. 2024. "Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis" Cancers 16, no. 9: 1658. https://doi.org/10.3390/cancers16091658
APA StyleEsposto, G., Massimiani, G., Galasso, L., Santini, P., Borriello, R., Mignini, I., Ainora, M. E., Nicoletti, A., Zileri Dal Verme, L., Gasbarrini, A., Alfieri, S., Quero, G., & Zocco, M. A. (2024). Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis. Cancers, 16(9), 1658. https://doi.org/10.3390/cancers16091658







