Novel Procedure for Designing and 3D Printing a Customized Surgical Template for Arthrodesis Surgery on the Sacrum
Abstract
:1. Introduction
2. Purpose
3. Materials and Methods
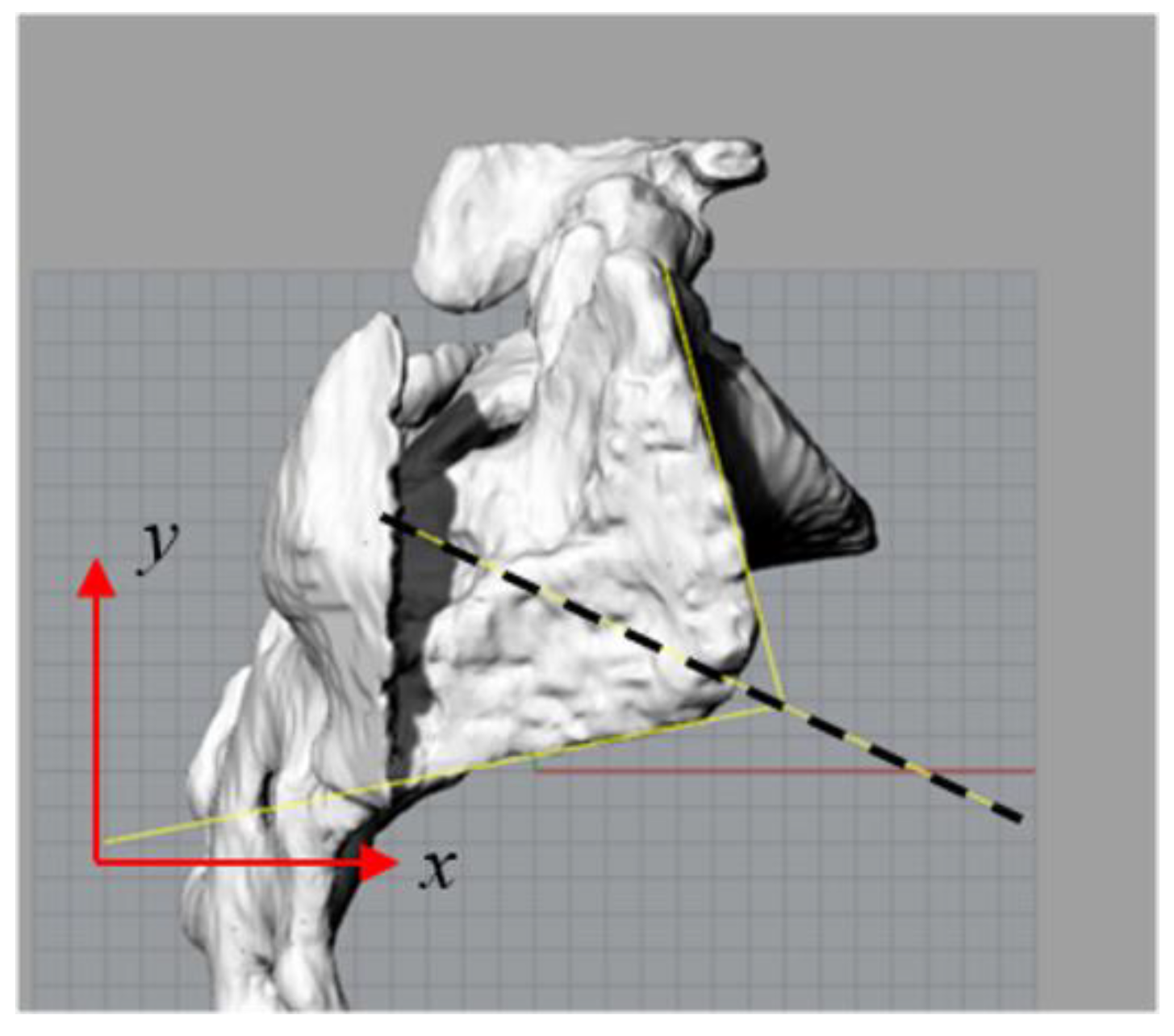
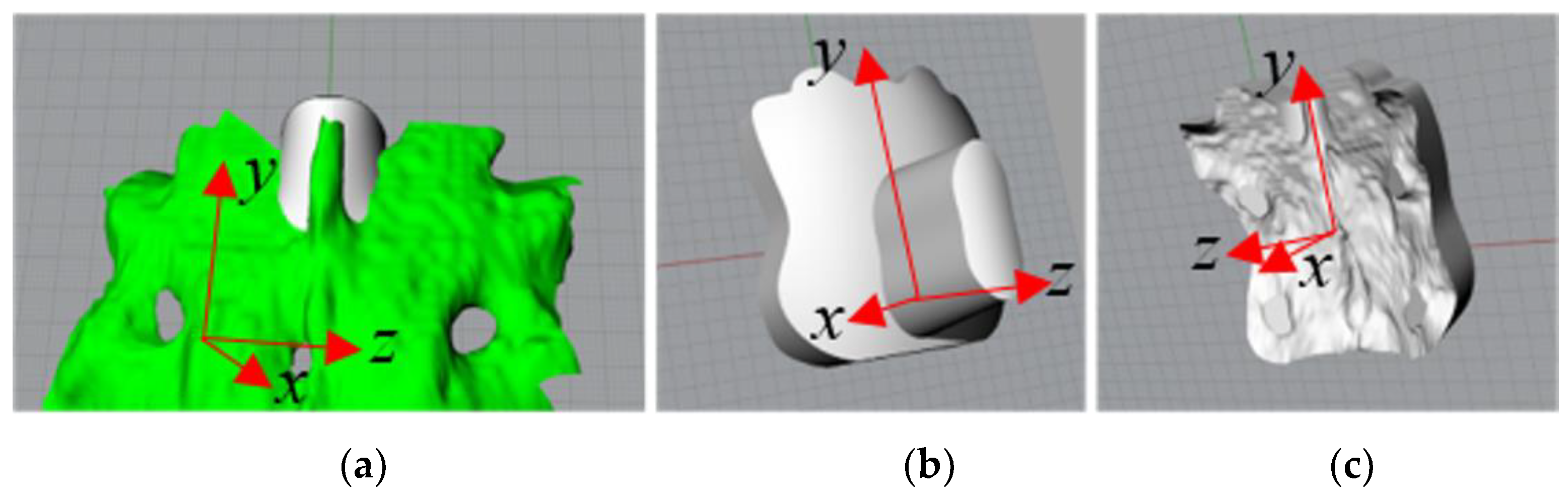
3.1. 3D Reconstruction of the Entry Zone
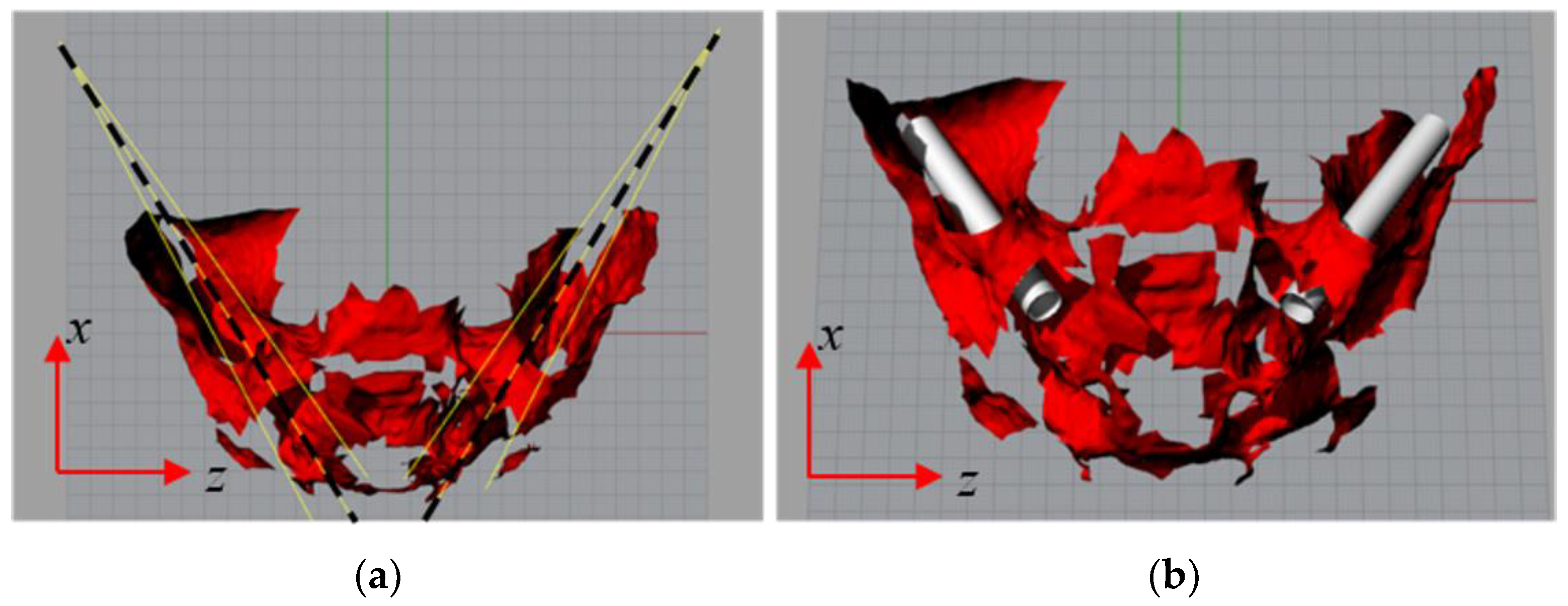
3.2. Procedure for Determining the Insertion Directions
- The external surface of the sacrum, as the sacrum-iliac joint could be laterally damaged, resulting in the appearance of pain. Dorsally, the sacral nerves protruding from the foramina could also be damaged;
- The interiors canaliculi that connect the dorsal and ventral foramina in which the sacral nerves are located;
- The surface delimiting the sacral canal that contains the sacral nerves.
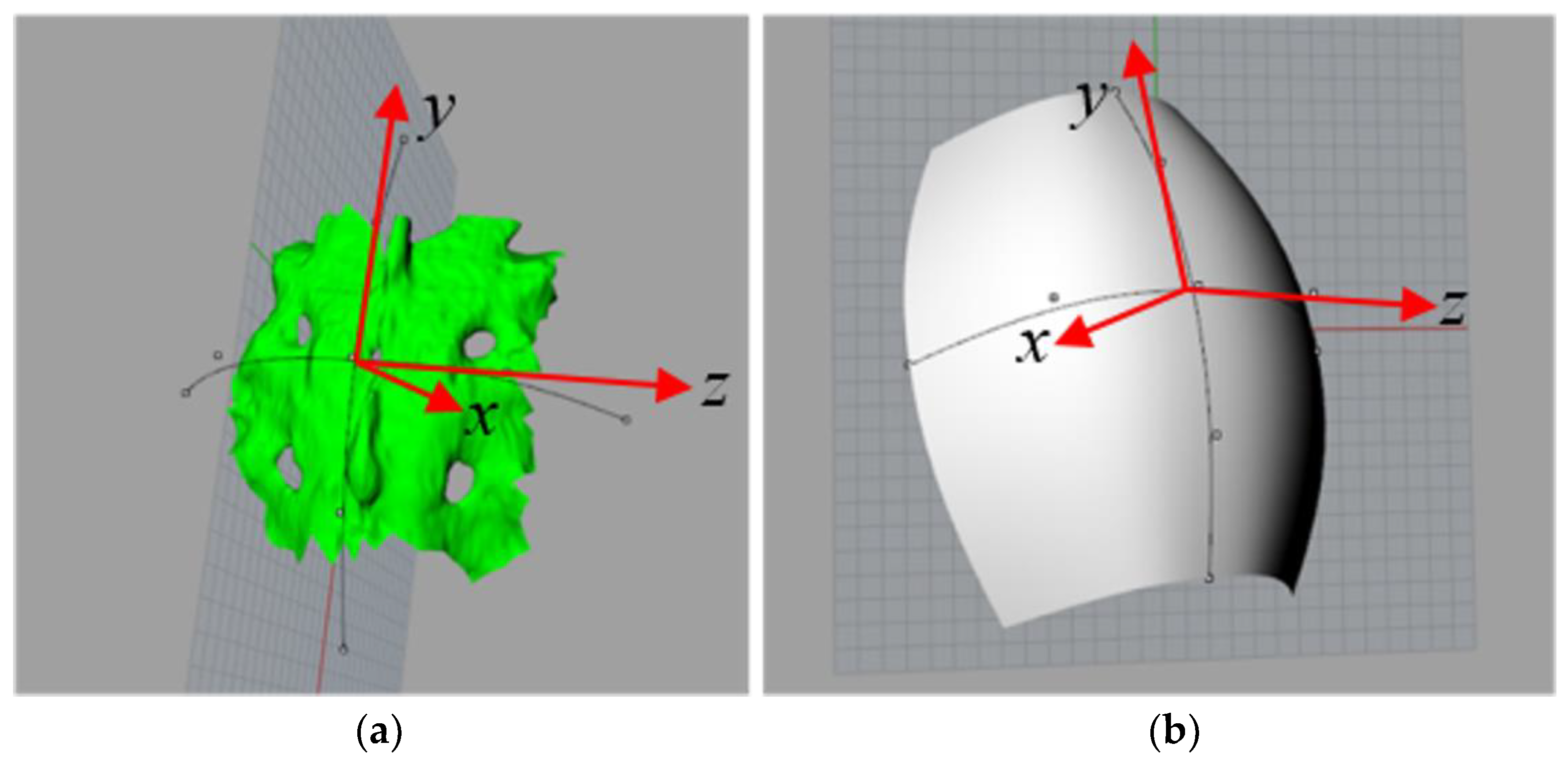
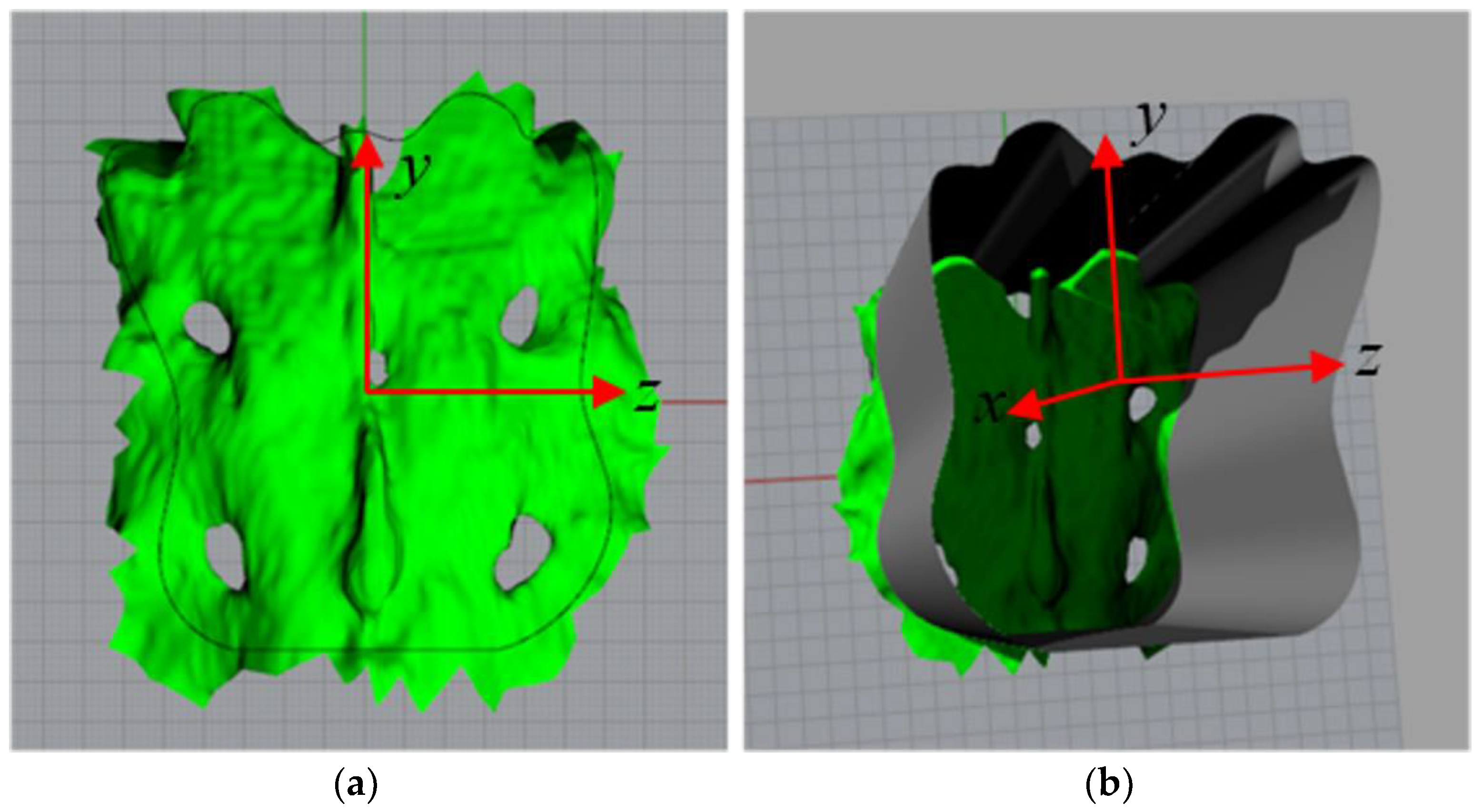
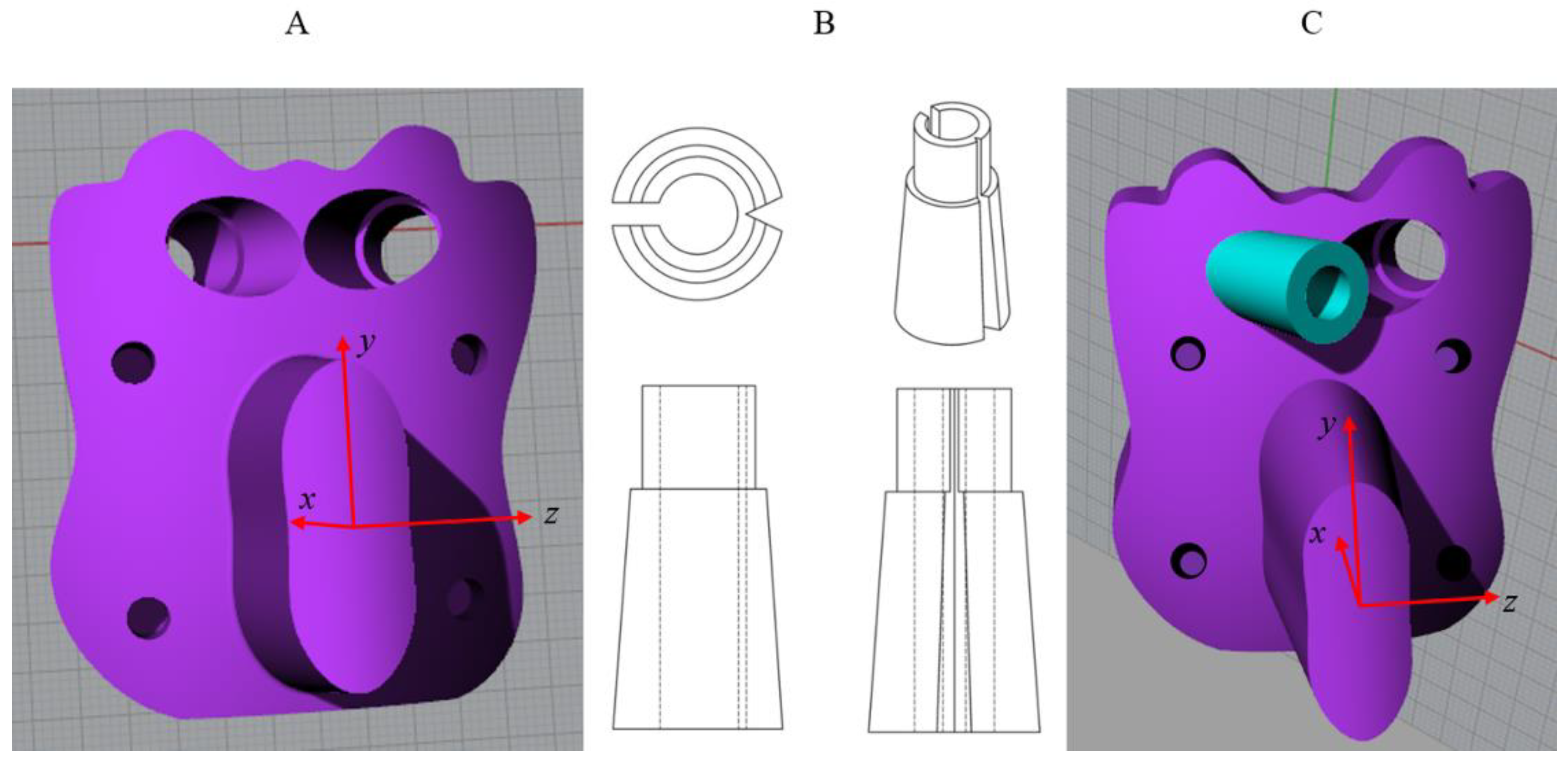
3.3. 3D Modelling of the Template
3.4. 3D Reconstruction of the Entry Zone
3.5. Error Chain Analysis
3.6. Generation of the Template
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Popescu, D.; Laptoiu, D. Rapid prototyping for patient-specific surgical orthopaedics guides: A systematic literature review. Proc. Inst. Mech. Eng. H 2016, 230, 495–515. [Google Scholar] [CrossRef] [PubMed]
- Popescu, D.; Anania, D.F.; Amza, C.G; Cicic, D.T. Design and rapid manufacturing of patient-specific spinal surgical guides: A survey. Proc. Manuf. Syst. 2012, 7, 2067–9238. [Google Scholar]
- Wang, J.C.; Mummaneni, P.V.; Haid, R.W. Current treatment strategies for the painful lumbar motion segment: Posterolateral fusion versus interbody fusion. Spine 2005, 30 (Suppl. S16), 33–43. [Google Scholar] [CrossRef]
- Barrey, C.Y.; Boissiere, L.; D’Acunzi, G.; Perrin, G. One-stage combined lumbo-sacral fusion, by anterior then posterior approach: Clinical and radiological results. Eur. Spine J. 2013, 22, 957–964. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 2015, 1, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.; Ossendorf, C.; Gruszka, D.; Hofmann, A.; Rommens, P.M. Fragility fractures of the sacrum: How to identify and when to treat surgically? Eur. J. Trauma Emerg. Surg. 2015, 41, 349–362. [Google Scholar] [CrossRef] [PubMed]
- Tjardes, T.; Paffrath, T.; Baethis, H.; Shafizadeh, S.; Steinhausen, E.; Steinbuechel, T.; Rixen, D.; Bouillon, B. Computer assisted percutaneous placement of augmented iliosacral screws. Spine 2008, 33, 1497–1500. [Google Scholar] [CrossRef] [PubMed]
- Oberkircher, L.; Masaeli, A.; Bliemel, C.; Debus, F.; Ruchholtz, S.; Krüger, A. Primary stability of three different iliosacral screw fixation techniques in osteoporotic cadaver specimens—A biomechanical investigation. Spine J. 2016, 16, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Richter, P.H.; Gebhard, F.; Dehner, C.; Scola, A. Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 2016, 47, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Lieberman, I.H. Robotic-guided sacro-pelvic fixation using S2 alar-iliac screws: Feasibility and accuracy. Eur. Spine J. 2017, 26, 720–725. [Google Scholar] [CrossRef] [PubMed]
- Bibb, R.; Eggbeer, D.; Evans, P.; Bocca, A.; Sugar, A. Rapid manufacture of custom-fitting surgical guides. Rapid Prototyp. J. 2009, 15, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Van Brussel, K.; Vander Sloten, J.; Van Audekercke, R. Medical image based design of an individualized surgical guide for pedicle screw insertion. In Proceedings of the 18th Annual Conference of the IEEE Engineering in Medicine and Biology Society, Amsterdam, The Netherlands, 31 October–3 November 1996. [Google Scholar]
- Berry, E.; Cuppone, M.; Porada, S.; Millner, P.A.; Rao, A.; Chiverton, N.; Seedhom, B.B. Personalised image-based templates for intra-operative guidance. Proc. Inst. Mech. Eng. H 2005, 219, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Popescu, D.; Amza, C.G.; Anania, D.; Cicic, D.T. Intelligent x-ray based training system for pedicle screw placement in lumbar vertebrae. Acad. J. Manuf. Eng. 2011, 9, 94–100. [Google Scholar]
- Goffin, J.; Van Brussel, K.; Martens, K.; Vander Sloten, J.; Van Audekercke, R.; Smet, M.H. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1-C2. Spine 2001, 26, 1343–1347. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Xu, Y.Q.; Zhang, Y.Z.; Xie, L.; Guo, H.; Li, D.P. A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur. Spine J. 2009, 18, 1379–1385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, S.; Xu, Y.Q.; Zhang, Y.Z.; Li, Y.B.; Shi, J.H.; Chen, G.P.; Chen, Y.B. Rapid prototyping drill guide template for lumbar pedicle screw placement. Chin. J. Traumatol. 2009, 12, 177–180. [Google Scholar] [PubMed]
- Lu, S.; Xu, Y.Q.; Chen, G.P.; Zhang, Y.Z.; Lu, D.; Chen, Y.B.; Shi, J.H.; Xu, X.M. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput. Surg. 2011, 16, 240–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugawara, T.; Higashiyama, N.; Kaneyama, S.; Takabatake, M.; Watanabe, N.; Uchida, F.; Sumi, M.; Mizoi, K. Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine. J. Neurosurg. Spine 2013, 19, 185–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaneyama, S.; Sugawara, T.; Sumi, M. Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine 2015, 40, E341–E348. [Google Scholar] [CrossRef] [PubMed]
- Wiker, R.B.; Tedla, B. Methods and Systems for Image-Guided Placement of Implants. U.S. Patent 20040240715A1, 2 December 2004. [Google Scholar]
- Pacheco, H.O. Method for Determining Size and Placement of Pedicle Screw in Spinal Surgery. China Patent 1960680B, 8 September 2010. [Google Scholar]
- Popescu, D.; Parpala, R.C.; Laptoiu, D.C.; Antoniac, I. Computer-aided technique for determining spinal pedicle screw size and optimal insertion trajectory. In Proceedings of the 21st International DAAAM Symposium, Zadar, Croatia, 20–23 October 2010; Volume 21, pp. 527–533. [Google Scholar]
- Solitro, G.F.; Amirouche, F. Innovative approach in the development of computer assisted algorithm for spine pedicle screw placement. Méd. Eng. Phys. 2016, 38, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Naddeo, F.; Cataldo, E.; Naddeo, A.; Cappetti, N.; Narciso, N. An automatic and patient-specific algorithm to design the optimal insertion direction of pedicle screws for spine surgery templates. Med. Biol. Eng. Comput. 2017, 55, 1549–1562. [Google Scholar] [CrossRef] [PubMed]
- Mazda, K.; Khairouni, A.; Penneçot, G.F.; Bloch, J. The ideal position of sacral transpedicular endplate screws in Jackson’s intrasacral fixation: An anatomic study of 50 sacral specimens. Spine 1998, 23, 2123–2126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.Z.; Lu, S.; Xu, Y.Q.; Shi, J.H; Li, Y.B.; Feng, Z.L. Application of navigation template to fixation of sacral fracture using three-dimensional reconstruction and reverse engineering technique. Chin. J. Traumatol. 2009, 12, 214–217. [Google Scholar] [PubMed]
- Schoenefeld, R.J.; Gutierrez, R.C.; Mellinger, P.A. Patient-Specific Sacroiliac Guides and Associated Methods. U.S. Patent 20130053854A1, 28 February 2013. [Google Scholar]
- Chen, B.; Zhang, Y.; Xiao, S.; Gu, P.; Lin, X. Personalized image-based templates for iliosacral screw insertions: A pilot study. Int. J. Méd. Robot. Comput. Assist. Surg. 2012, 8, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Merc, M.; Drstvenšek, I.; Vogrin, M.; Brajlih, T.; Rečnik, G. Use of rapid prototyping drill guide template for pedicle screw placement. Zdrav. Vestn. 2013, 82, 395–401. [Google Scholar]
- Merc, M.; Drstvensek, I.; Vogrin, M.; Brajlih, T.; Friedrich, T.; Recnik, G. Error rate of multi-level rapid prototyping trajectories for pedicle screw placement in lumbar and sacral spine. Chin. J. Traumatol. 2014, 17, 261–266. [Google Scholar] [PubMed]
- Éltes, P.E.; Lazary, A.; Varga, P.P. Finite element analysis based lumbosacral revision surgery using an individual navigation template. Glob. Spine J. 2016, 06 (Suppl. S1). [Google Scholar] [CrossRef]
- Merc, M.; Recnik, G.; Krajnc, Z. Lumbar and sacral pedicle screw placement using a template does not improve the midterm pain and disability outcome in comparison with free-hand method. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Baldino, L.; Naddeo, F.; Cardea, S.; Naddeo, A.; Reverchon, E. FEM modeling of the reinforcement mechanism of hydroxyapatite in plla scaffolds produced by supercritical drying, for tissue engineering applications. J. Mech. Behav. Biomed. Mater. 2015, 51, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Naddeo, F.; Baldino, L.; Cardea, S.; Naddeo, A.; Reverchon, E. Optimization of an ad hoc realized space frame structured RVE for FEM modeling of nanoporous biopolymeric scaffolds obtained by supercritical fluids assisted process. Chem. Eng. Trans. 2016, 49, 169–174. [Google Scholar]
- Naddeo, F.; Cappetti, N.; Naddeo, A. Novel load adaptive algorithm based procedure for 3D printing of cancellous bone-inspired structures. Compos. Part B Eng. 2017, 115, 60–69. [Google Scholar] [CrossRef]
- Nottmeier, E.W.; Pirris, S.M.; Balseiro, S.; Fenton, D. Three-dimensional image-guided placement of S2 alar screws to adjunct or salvage lumbosacral fixation. Spine J. 2010, 10, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Zindrick, M.R.; Wiltse, L.L.; Widell, E.H.; Thomas, J.C.; Holland, W.R.; Field, B.T.; Spencer, C.W. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin. Orthop. Relat. Res. 1986, 203, 99–112. [Google Scholar] [CrossRef]
- Ebraheim, N.A.; Lu, J.; Yang, H.; Heck, B.E.; Yeasting, R.A. Anatomic considerations of the second sacral vertebra and dorsal screw placement. Surg. Radiol. Anat. 1997, 19, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Pishnamaz, M.; Dienstknecht, T.; Hoppe, B.; Garving, C.; Lange, H.; Hildebrand, F.; Kobbe, P.; Pape, H.C. Assessment of pelvic injuries treated with ilio-sacral screws: Injury severity and accuracy of screw positioning. Int. Orthop. 2016, 40, 1495–1501. [Google Scholar] [CrossRef] [PubMed]
- Italian Statistics Database. Available online: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_OSPEDSSN (accessed on 20 June 2017).


© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naddeo, F.; Naddeo, A.; Cappetti, N.; Cataldo, E.; Militio, R. Novel Procedure for Designing and 3D Printing a Customized Surgical Template for Arthrodesis Surgery on the Sacrum. Symmetry 2018, 10, 334. https://doi.org/10.3390/sym10080334
Naddeo F, Naddeo A, Cappetti N, Cataldo E, Militio R. Novel Procedure for Designing and 3D Printing a Customized Surgical Template for Arthrodesis Surgery on the Sacrum. Symmetry. 2018; 10(8):334. https://doi.org/10.3390/sym10080334
Chicago/Turabian StyleNaddeo, Francesco, Alessandro Naddeo, Nicola Cappetti, Emilio Cataldo, and Riccardo Militio. 2018. "Novel Procedure for Designing and 3D Printing a Customized Surgical Template for Arthrodesis Surgery on the Sacrum" Symmetry 10, no. 8: 334. https://doi.org/10.3390/sym10080334





