Improving Blood Transfusion Practices in a Community Hospital Setting: Our Experience with Real-Time Clinical Decision Support
Abstract
:1. Introduction
2. Materials and Methods
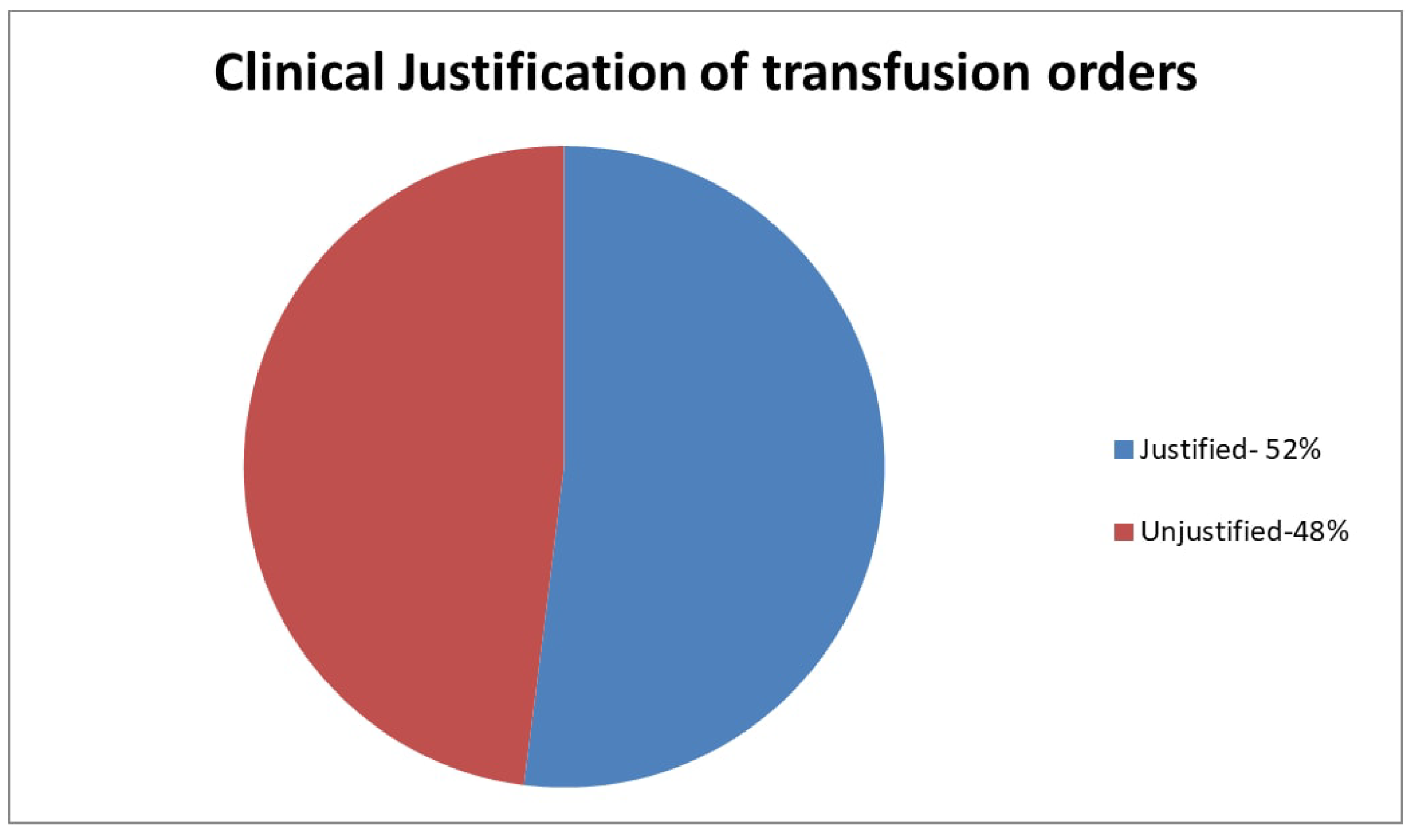
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Josephson, C.D.; Glynn, S.A.; Kleinman, S.H.; Blajchman, M.A.; State of the Science Symposium Transfusion Medicine Committee. A multidisciplinary “think tank”: The top 10 clinical trial opportunities in transfusion medicine from the National Heart, Lung and Blood Institute-sponsored 2009 state-of-the-science symposium. Transfusion 2011, 51, 828–841. [Google Scholar] [CrossRef] [PubMed]
- Shander, A.; Fink, A.; Javidroozi, M.; Erhard, J.; Farmer, S.L.; Corwin, H.; Goodnough, L.T.; Hofmann, A.; Isbister, J.; Ozawa, S.; et al. Appropriateness of allogeneic red blood cell transfusion: The international consensus conference on transfusion outcomes. Transfus. Med. Rev. 2011, 25, 232–246. [Google Scholar] [CrossRef] [PubMed]
- Callum, J.L.; Waters, J.H.; Shaz, B.H.; Sloan, S.R.; Murphy, M.F. The AABB recommendations for the Choosing Wisely campaign of the American Board of Internal Medicine. Transfusion 2014, 54, 2344–2351. [Google Scholar] [CrossRef] [PubMed]
- Choosing Wisely. Available online: http://www.choosingwisely.org/clinicians-lists (accessed on 10 March 2018).
- The Joint Commission. Implementation Guide for the Joint Commission Patient Blood Management Performance Measures. Available online: https://www.jointcommission.org/assets/1/6/ (accessed on 10 March 2018).
- Goodnough, L.T.; Shah, N. The next chapter in patient blood management. Real-time clinical decision support. Am. J. Clin. Pathol. 2014, 142, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Goodnough, L.T.; Shieh, L.; Hadhazy, E.; Cheng, N.; Khari, P.; Maggio, P. Improved blood utilization using real-time clinical decision support. Transfusion 2014, 54, 1358–1365. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.L.; Guyatt, G.; Heddle, N.M.; Grossman, B.J.; Cohn, C.S.; Fung, M.K.; Gernsheimer, T.; Holcomb, J.B.; Kaplan, L.J.; Katz, L.M.; et al. Clinical Practice Guidelines from the AABB: Red Blood Cell Transfusions Thresholds and storage. JAMA 2016, 316, 2025–2035. [Google Scholar] [CrossRef] [PubMed]
- Proceedings from the National Summit on Overuse. 24 September 2012. The Joint Commission. Physician Consortium for Performance Improvement. Available online: https://www.jointcommission.org/assets/National_Summit_overuse.PFD (accessed on 29 June 2018).
- Ansari, S.; Szallasi, A. Blood management by transfusion triggers: When less is more. Blood Transfus. 2012, 10, 28–33. [Google Scholar] [PubMed]
- De Leon, E.M.B.; Szallasi, A. “Transfusion indication RBC (PMB-02)”: Gap analysis of a Joint Commission Patient Blood Management Measure at a community hospital. Blood Transfus. 2014, 12 (Suppl. 1), s187–s190. [Google Scholar] [PubMed]
- Szallasi, A.; Jha, R. The role of the Blood Bank in patient blood management: Transfusion triggers shine in 10-year blood utilization data. F1000Research 2015, 4, 894. [Google Scholar] [CrossRef]
- Gardner, R.M.; Christiansen, P.D.; Tate, K.E.; Laub, M.B.; Holmes, S.R. Computerized continuous quality improvement methods used to optimize blood transfusions. In Proceedings of the Annual Symposium on Computer Application in Medical Care, Washington, DC, USA, 30 October–3 November 1993; pp. 166–170. [Google Scholar]
- Jenkins, I.; Doucet, J.J.; Clay, B.; Kopko, P.; Fipps, D.; Hemmen, E.; Paulson, D. Transfusing Wisely: Clinical decision support improves blood transfusion practices. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 389–395. [Google Scholar] [CrossRef] [PubMed]




© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sardar, M.; Azharuddin, M.; Subedi, A.; Ghatage, P.; Du, D.; Szallasi, A. Improving Blood Transfusion Practices in a Community Hospital Setting: Our Experience with Real-Time Clinical Decision Support. Med. Sci. 2018, 6, 67. https://doi.org/10.3390/medsci6030067
Sardar M, Azharuddin M, Subedi A, Ghatage P, Du D, Szallasi A. Improving Blood Transfusion Practices in a Community Hospital Setting: Our Experience with Real-Time Clinical Decision Support. Medical Sciences. 2018; 6(3):67. https://doi.org/10.3390/medsci6030067
Chicago/Turabian StyleSardar, Muhammad, Muhammad Azharuddin, Ananta Subedi, Prateek Ghatage, Doantarang Du, and Arpad Szallasi. 2018. "Improving Blood Transfusion Practices in a Community Hospital Setting: Our Experience with Real-Time Clinical Decision Support" Medical Sciences 6, no. 3: 67. https://doi.org/10.3390/medsci6030067
APA StyleSardar, M., Azharuddin, M., Subedi, A., Ghatage, P., Du, D., & Szallasi, A. (2018). Improving Blood Transfusion Practices in a Community Hospital Setting: Our Experience with Real-Time Clinical Decision Support. Medical Sciences, 6(3), 67. https://doi.org/10.3390/medsci6030067




