The Obesity Paradox: Associations between the Body Mass Index and Self-Perceived Health, Depression Status, and Pain Level in Older People
Abstract
1. Introduction
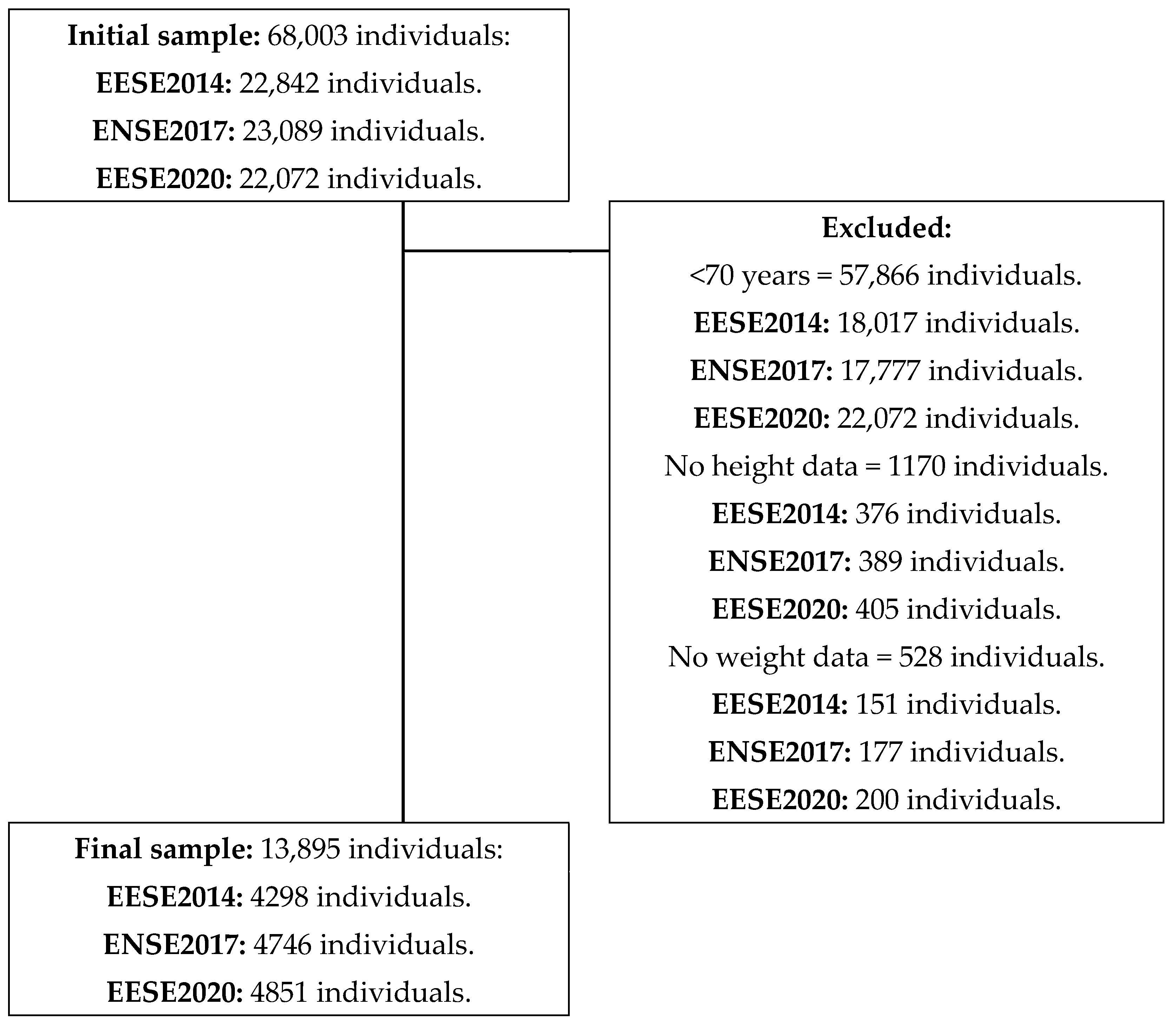
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Procedures
2.4. Statistical Analysis
3. Results
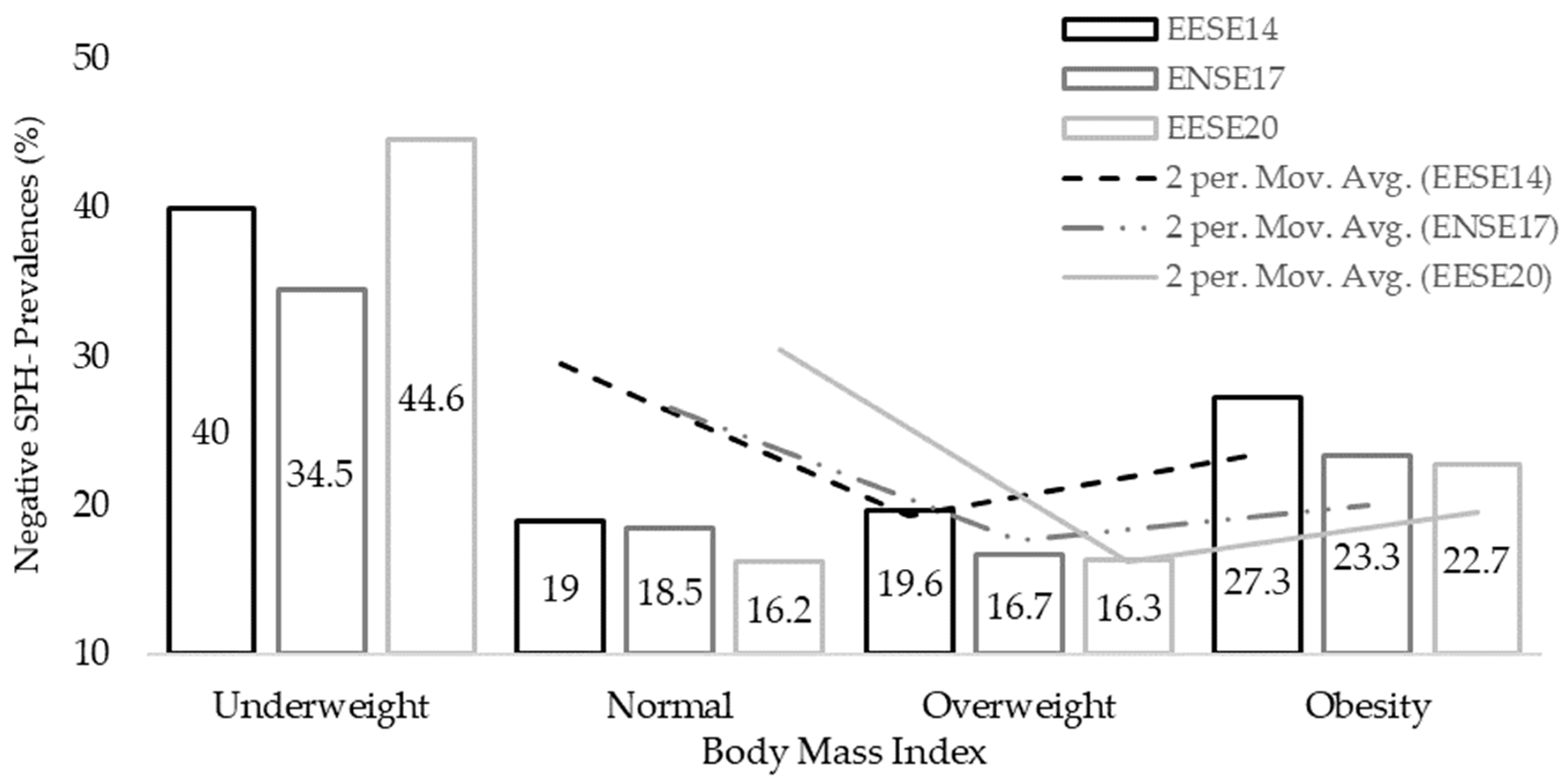
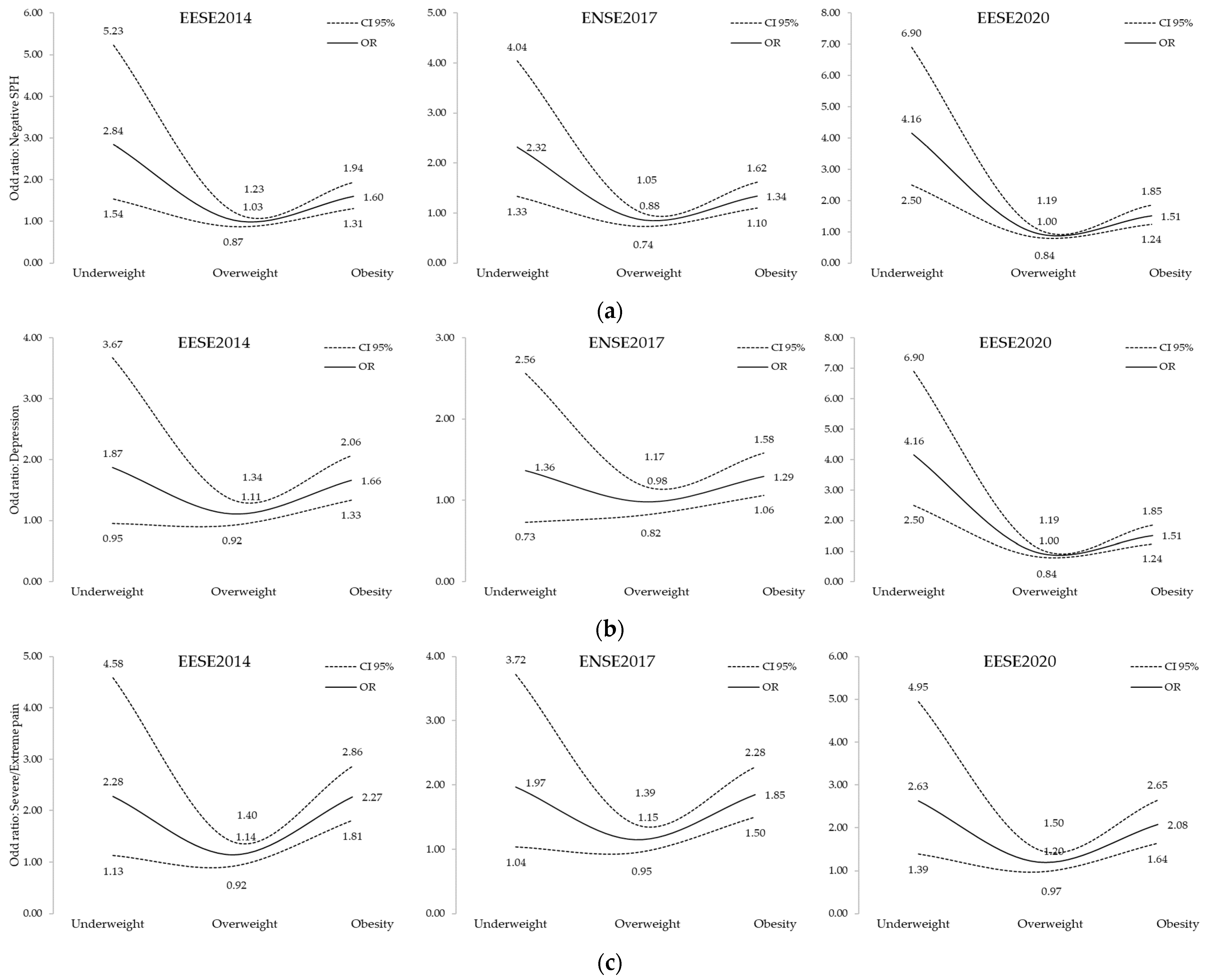
3.1. Self-Perceived Health
3.2. Depression Status
3.3. Pain Degree
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. World Population Prospects The 2017 Revision Key Findings and Advance Tables; Department of Economic and Social Affairs Population Division, United Nations: New York, NY, USA, 2017. [Google Scholar]
- Campisi, J.; Kapahi, P.; Lithgow, G.J.; Melov, S.; Newman, J.C.; Verdin, E. From Discoveries in Ageing Research to Therapeutics for Healthy Ageing. Nature 2019, 571, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Mijnarends, D.M.; Schols, J.M.G.A.; Meijers, J.M.M.; Tan, F.E.S.; Verlaan, S.; Luiking, Y.C.; Morley, J.E.; Halfens, R.J.G. Instruments to Assess Sarcopenia and Physical Frailty in Older People Living in a Community (Care) Setting: Similarities and Discrepancies. J. Am. Med. Dir. Assoc. 2015, 16, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Prausmüller, S.; Heitzinger, G.; Pavo, N.; Spinka, G.; Goliasch, G.; Arfsten, H.; Gabler, C.; Strunk, G.; Hengstenberg, C.; Hülsmann, M.; et al. Malnutrition Outweighs the Effect of the Obesity Paradox. J. Cachexia Sarcopenia Muscle 2022, 13, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Reijnierse, E.M.; Trappenburg, M.C.; Blauw, G.J.; Verlaan, S.; de van der Schueren, M.A.E.; Meskers, C.G.M.; Maier, A.B. Common Ground? The Concordance of Sarcopenia and Frailty Definitions. J. Am. Med. Dir. Assoc. 2016, 17, 371.e7–371.e12. [Google Scholar] [CrossRef] [PubMed]
- Batsis, J.A.; Villareal, D.T. Sarcopenic Obesity in Older Adults: Aetiology, Epidemiology and Treatment Strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Litchford, M.D. Counteracting the Trajectory of Frailty and Sarcopenia in Older Adults. Nutr. Clin. Pract. 2014, 29, 428–434. [Google Scholar] [CrossRef]
- Bray, G.A.; Kim, K.K.; Wilding, J.P.H.; World Obesity Federation. Obesity: A Chronic Relapsing Progressive Disease Process. A Position Statement of the World Obesity Federation. Obes. Rev. 2017, 18, 715–723. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.J.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The Obesity Transition: Stages of the Global Epidemic. Lancet Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]
- Palacios-Ceña, D.; Alonso-Blanco, C.; Jiménez-Garcia, R.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Pileño-Martinez, E.; Fernández-de-Las-Peñas, C. Time Trends in Leisure Time Physical Activity and Physical Fitness in Elderly People: 20 Year Follow-up of the Spanish Population National Health Survey (1987–2006). BMC Public Health 2011, 11, 799. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief. 2017, 288, 1–8. [Google Scholar]
- Payne, M.E.; Porter Starr, K.N.; Orenduff, M.; Mulder, H.S.; McDonald, S.R.; Spira, A.P.; Pieper, C.F.; Bales, C.W. Quality of Life and Mental Health in Older Adults with Obesity and Frailty: Associations with a Weight Loss Intervention. J. Nutr. Health Aging 2018, 22, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Adult Obesity Complications: Challenges and Clinical Impact—PMC. 2020. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7309384/ (accessed on 8 November 2022).
- Machón, M.; Vergara, I.; Dorronsoro, M.; Vrotsou, K.; Larrañaga, I. Self-Perceived Health in Functionally Independent Older People: Associated Factors. BMC Geriatr. 2016, 16, 66. [Google Scholar] [CrossRef] [PubMed]
- Pereira-de-Sousa, A.M.; López-Rodríguez, J.A. Salud autopercibida en ancianos jóvenes españoles y portugueses tras la recesión según la Encuesta Europea de Salud: Un estudio transversal. Aten. Primaria 2021, 53, 102064. [Google Scholar] [CrossRef] [PubMed]
- Dostálová, R.; Stillman, C.; Erickson, K.I.; Slepička, P.; Mudrák, J. The Relationship between Physical Activity, Self-Perceived Health, and Cognitive Function in Older Adults. Brain Sci. 2021, 11, 492. [Google Scholar] [CrossRef] [PubMed]
- Lera-López, F.; Garrues Irisarri, M.A.; Ollo-López, A.; Iriso, E.S.; Cabasés Hita, J.M.; Sánchez Santos, J.M. Actividad Física y Salud Autopercibida En Personas Mayores de 50 Años/Physical Activity and Self-Perceived Health among People Aged 50 and Over. Rev. Int. Med. Cienc. Act. Física Deporte 2017, 67, 559–571. [Google Scholar] [CrossRef]
- Casey, D.A. Depression in the Elderly: A Review and Update. Asia-Pac. Psychiatry 2012, 4, 160–167. [Google Scholar] [CrossRef]
- Blazer, D.G. Depression in Late Life: Review and Commentary. J. Gerontol. A. Biol. Sci. Med. Sci. 2003, 58, 249–265. [Google Scholar] [CrossRef]
- Simon, G.E.; Rohde, P.; Ludman, E.J.; Jeffery, R.W.; Linde, J.A.; Operskalski, B.H.; Arterburn, D. Association between Change in Depression and Change in Weight Among Women Enrolled in Weight Loss Treatment. Gen. Hosp. Psychiatry 2010, 32, 583–589. [Google Scholar] [CrossRef]
- Legenbauer, T.; De Zwaan, M.; Benecke, A.; Muhlhans, B.; Petrak, F.; Herpertz, S. Depression and Anxiety: Their Predictive Function for Weight Loss in Obese Individuals. Obes. Facts 2009, 2, 227–234. [Google Scholar] [CrossRef]
- Faulconbridge, L.F.; Wadden, T.A.; Berkowitz, R.I.; Sarwer, D.B.; Womble, L.G.; Hesson, L.A.; Stunkard, A.J.; Fabricatore, A.N. Changes in Symptoms of Depression with Weight Loss: Results of a Randomized Trial. Obes. Silver Spring Md. 2009, 17, 1009–1016. [Google Scholar] [CrossRef]
- Mazzeschi, C.; Pazzagli, C.; Buratta, L.; Reboldi, G.P.; Battistini, D.; Piana, N.; Pippi, R.; Fatone, C.; De Feo, P. Mutual Interactions between Depression/Quality of Life and Adherence to a Multidisciplinary Lifestyle Intervention in Obesity. J. Clin. Endocrinol. Metab. 2012, 97, E2261–E2265. [Google Scholar] [CrossRef]
- Lowry, K.A.; Vallejo, A.N.; Studenski, S.A. Successful Aging as a Continuum of Functional Independence: Lessons from Physical Disability Models of Aging. Aging Dis. 2012, 3, 5–15. [Google Scholar] [PubMed]
- Schofield, P.; Gibson, S. Fact Sheets, Pain in Older Adults; IASP: Washington, DC, USA, 2019. [Google Scholar]
- Wei, L.; Hu, Y.; Tao, Y.; Hu, R.; Zhang, L. The Effects of Physical Exercise on the Quality of Life of Healthy Older Adults in China: A Systematic Review. Front. Psychol. 2022, 13, 895373. [Google Scholar] [CrossRef] [PubMed]
- Atad, O.I.; Caspi, D. Exercise and Perceived Quality of Life among Frail Older Adults. Qual. Ageing Older Adults 2020, 21, 29–38. [Google Scholar] [CrossRef]
- Yen, H.-Y.; Lin, L.-J. Quality of Life in Older Adults: Benefits from the Productive Engagement in Physical Activity. J. Exerc. Sci. Fit. 2018, 16, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical Activity and Exercise for Chronic Pain in Adults: An Overview of Cochrane Reviews. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2017; p. CD011279.pub2. [Google Scholar]
- Melissas, J.; Kontakis, G.; Volakakis, E.; Tsepetis, T.; Alegakis, A.; Hadjipavlou, A. The Effect of Surgical Weight Reduction on Functional Status in Morbidly Obese Patients with Low Back Pain. Obes. Surg. 2005, 15, 378–381. [Google Scholar] [CrossRef]
- Bliddal, H.; Leeds, A.R.; Christensen, R. Osteoarthritis, Obesity and Weight Loss: Evidence, Hypotheses and Horizons—A Scoping Review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2014, 15, 578–586. [Google Scholar] [CrossRef] [PubMed]
- George, S.Z.; Dover, G.C.; Fillingim, R.B. Fear of Pain Influences Outcomes after Exercise-Induced Delayed Onset Muscle Soreness at the Shoulder. Clin. J. Pain 2007, 23, 76–84. [Google Scholar] [CrossRef]
- Donini, L.M.; Pinto, A.; Giusti, A.M.; Lenzi, A.; Poggiogalle, E. Obesity or BMI Paradox? Beneath the Tip of the Iceberg. Front. Nutr. 2020, 7, 53. [Google Scholar] [CrossRef]
- Lv, Y.-B.; Liu, S.; Yin, Z.-X.; Gao, X.; Kraus, V.B.; Mao, C.; Yuan, J.-Q.; Zhang, J.; Luo, J.-S.; Chen, H.-S.; et al. Associations of Body Mass Index and Waist Circumference with 3-Year All-Cause Mortality Among the Oldest Old: Evidence from a Chinese Community-Based Prospective Cohort Study. J. Am. Med. Dir. Assoc. 2018, 19, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Bosello, O.; Vanzo, A. Obesity Paradox and Aging. Eat. Weight. Disord. EWD 2021, 26, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.; Cheng, J.; Yu, Y.; Wang, T.; Zhou, W.; Yu, C.; Zhu, L.; Bao, H.; Cheng, X. Association Between Body Mass Index and All-Cause Mortality in a Prospective Cohort of Southern Chinese Adults Without Morbid Obesity. Front. Physiol. 2022, 13, 857787. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad, Consumo y Bienestar Social Encuesta Europea de Salud En España 2014. 2014. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2014.htm (accessed on 8 November 2022).
- Ministerio de Sanidad, Consumo y Bienestar Social Encuesta Europea de Salud En España 2020. 2020. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2020.htm (accessed on 8 November 2022).
- Ministerio de Sanidad, Consumo y Bienestar Social Encuesta Nacional de Salud de España 2017. 2017. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 8 November 2022).
- Zhang, J.; Begley, A.; Jackson, R.; Harrison, M.; Pellicori, P.; Clark, A.L.; Cleland, J.G.F. Body Mass Index and All-Cause Mortality in Heart Failure Patients with Normal and Reduced Ventricular Ejection Fraction: A Dose-Response Meta-Analysis. Clin. Res. Cardiol. 2019, 108, 119–132. [Google Scholar] [CrossRef]
- Rozen, G.; Elbaz-Greener, G.; Margolis, G.; Marai, I.; Heist, E.K.; Ruskin, J.N.; Carasso, S.; Roguin, A.; Birati, E.Y.; Amir, O. The Obesity Paradox in Real-World Nation-Wide Cohort of Patients Admitted for a Stroke in the U.S. J. Clin. Med. 2022, 11, 1678. [Google Scholar] [CrossRef]
- Lv, Y.; Mao, C.; Gao, X.; Ji, J.S.; Kraus, V.B.; Yin, Z.; Yuan, J.; Chen, H.; Luo, J.; Zhou, J.; et al. The Obesity Paradox Is Mostly Driven by Decreased Noncardiovascular Disease Mortality in the Oldest Old in China: A 20-Year Prospective Cohort Study. Nat. Aging 2022, 2, 389–396. [Google Scholar] [CrossRef]
- Kim, P.-J.; Kim, C.; Lee, S.-H.; Shon, J.-H.; Kwon, Y.; Kim, J.-H.; Kim, D.-K.; Yu, H.; Ahn, H.-J.; Jeon, J.-P.; et al. Another Look at Obesity Paradox in Acute Ischemic Stroke: Association Rule Mining. J. Pers. Med. 2021, 12, 16. [Google Scholar] [CrossRef]
- Wang, L.; Yi, Z. Obesity Paradox and Aging: Visceral Adiposity Index and All-Cause Mortality in Older Individuals: A Prospective Cohort Study. Front. Endocrinol. 2022, 13, 975209. [Google Scholar] [CrossRef]
- Feng, X.; Zhang, C.; Jiang, L.; Xu, L.; Tian, J.; Zhao, X.; Wang, D.; Zhang, Y.; Sun, K.; Xu, B.; et al. Body Mass Index and Mortality in Patients with Severe Coronary Artery Diseases: A Cohort Study from China. Nutr. Metab. Cardiovasc. Dis. NMCD 2021, 31, 448–454. [Google Scholar] [CrossRef]
- Kvamme, J.-M.; Olsen, J.A.; Florholmen, J.; Jacobsen, B.K. Risk of Malnutrition and Health-Related Quality of Life in Community-Living Elderly Men and Women: The Tromsø Study. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2011, 20, 575–582. [Google Scholar] [CrossRef]
- Gao, Q.; Hu, K.; Yan, C.; Zhao, B.; Mei, F.; Chen, F.; Zhao, L.; Shang, Y.; Ma, Y.; Ma, B. Associated Factors of Sarcopenia in Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 4291. [Google Scholar] [CrossRef] [PubMed]
- Bucholz, E.M.; Krumholz, H.A.; Krumholz, H.M. Underweight, Markers of Cachexia, and Mortality in Acute Myocardial Infarction: A Prospective Cohort Study of Elderly Medicare Beneficiaries. PLoS Med. 2016, 13, e1001998. [Google Scholar] [CrossRef] [PubMed]
- Warkentin, L.M.; Das, D.; Majumdar, S.R.; Johnson, J.A.; Padwal, R.S. The Effect of Weight Loss on Health-Related Quality of Life: Systematic Review and Meta-Analysis of Randomized Trials. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2014, 15, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Pan, A.; Kawachi, I.; Luo, N.; Manson, J.E.; Willett, W.C.; Hu, F.B.; Okereke, O.I. Changes in Body Weight and Health-Related Quality of Life: 2 Cohorts of US Women. Am. J. Epidemiol. 2014, 180, 254–262. [Google Scholar] [CrossRef]
- You, H.; Li, X.; Jing, K.; Li, Z.; Cao, H.; Wang, J.; Bai, L.; Gu, J.; Fan, X.; Gu, H. Association between Body Mass Index and Health-Related Quality of Life among Chinese Elderly—Evidence from a Community-Based Study. BMC Public Health 2018, 18, 1174. [Google Scholar] [CrossRef] [PubMed]
- Busutil, R.; Espallardo, O.; Torres, A.; Martínez-Galdeano, L.; Zozaya, N.; Hidalgo-Vega, Á. The Impact of Obesity on Health-Related Quality of Life in Spain. Health Qual. Life Outcomes 2017, 15, 197. [Google Scholar] [CrossRef]
- Oliva-Moreno, J.; Gil-Lacruz, A. Body Weight and Health-Related Quality of Life in Catalonia, Spain. Eur. J. Health Econ. HEPAC Health Econ. Prev. Care 2013, 14, 95–105. [Google Scholar] [CrossRef]
- Park, S. Pathways Linking Obesity to Health-Related Quality of Life. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2017, 26, 2209–2218. [Google Scholar] [CrossRef]
- de Wit, L.M.; van Straten, A.; van Herten, M.; Penninx, B.W.; Cuijpers, P. Depression and Body Mass Index, a u-Shaped Association. BMC Public Health 2009, 9, 14. [Google Scholar] [CrossRef]
- Pei, H.; Kang, N.; Guo, C.; Zhang, Y.; Chu, H.; Chen, G.; Zhang, L. Longitudinal Transition of Body Mass Index Status and Its Associated Factors among Chinese Middle-Aged and Older Adults in Markov Model. Front. Public Health 2022, 10, 973191. [Google Scholar] [CrossRef]
- Chen, C.; Winterstein, A.G.; Fillingim, R.B.; Wei, Y.-J. Body Weight, Frailty, and Chronic Pain in Older Adults: A Cross-Sectional Study. BMC Geriatr. 2019, 19, 143. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.C.; Looker, A.C.; Saag, K.G.; Curtis, J.R.; Delzell, E.S.; Randall, S.; Dawson-Hughes, B. The Recent Prevalence of Osteoporosis and Low Bone Mass in the United States Based on Bone Mineral Density at the Femoral Neck or Lumbar Spine. J. Bone Miner. Res. 2014, 29, 2520–2526. [Google Scholar] [CrossRef] [PubMed]
- White, M.C.; Holman, D.M.; Boehm, J.E.; Peipins, L.A.; Grossman, M.; Henley, S.J. Age and Cancer Risk: A Potentially Modifiable Relationship. Am. J. Prev. Med. 2014, 46, S7–S15. [Google Scholar] [CrossRef]
- Chin, S.-H.; Huang, W.-L.; Akter, S.; Binks, M. Obesity and Pain: A Systematic Review. Int. J. Obes. 2020, 44, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Lemos, E.C.W.M.; Guadagnin, E.C.; Mota, C.B. Influence of Strength Training and Multicomponent Training on the Functionality of Older Adults: Systematic Review and Meta-Analysis. Rev. Bras. Cineantropometria Desempenho Hum. 2020, 22, e60707. [Google Scholar] [CrossRef]
- Labata-Lezaun, N.; González-Rueda, V.; Llurda-Almuzara, L.; López-de-Celis, C.; Rodríguez-Sanz, J.; Bosch, J.; Vicente-Rodríguez, G.; Gorczakowska, D.; Araluze-Arizti, P.; Pérez-Bellmunt, A. Effectiveness of Multicomponent Training on Physical Performance in Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2023, 104, 104838. [Google Scholar] [CrossRef]
- Moreira, N.B.; Rodacki, A.L.F.; Costa, S.N.; Pitta, A.; Bento, P.C.B. Perceptive–Cognitive and Physical Function in Prefrail Older Adults: Exergaming Versus Traditional Multicomponent Training. Rejuvenation Res. 2021, 24, 28–36. [Google Scholar] [CrossRef]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef]
- Cho, J.; Jin, Y.; Kang, H. Weight Status, Physical Activity, and Depression in Korean Older Adults. J. Epidemiol. 2018, 28, 292–299. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as Medicine—Evidence for Prescribing Exercise as Therapy in 26 Different Chronic Diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef]
- Buss, J. Limitations of Body Mass Index to Assess Body Fat. Work. Health Saf. 2014, 62, 264. [Google Scholar] [CrossRef] [PubMed]
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front. Endocrinol. 2020, 10, 861. [Google Scholar] [CrossRef] [PubMed]
- Krul, A.J.; Daanen, H.A.M.; Choi, H. Self-Reported and Measured Weight, Height and Body Mass Index (BMI) in Italy, the Netherlands and North America. Eur. J. Public Health 2011, 21, 414–419. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denche-Zamorano, Á.; Salas-Gómez, D.; Carlos-Vivas, J.; Barrios-Fernandez, S.; Merellano-Navarro, E.; Collado-Mateo, D.; Olivares, P.R.; Adsuar, J.C. The Obesity Paradox: Associations between the Body Mass Index and Self-Perceived Health, Depression Status, and Pain Level in Older People. Appl. Sci. 2023, 13, 588. https://doi.org/10.3390/app13010588
Denche-Zamorano Á, Salas-Gómez D, Carlos-Vivas J, Barrios-Fernandez S, Merellano-Navarro E, Collado-Mateo D, Olivares PR, Adsuar JC. The Obesity Paradox: Associations between the Body Mass Index and Self-Perceived Health, Depression Status, and Pain Level in Older People. Applied Sciences. 2023; 13(1):588. https://doi.org/10.3390/app13010588
Chicago/Turabian StyleDenche-Zamorano, Ángel, Diana Salas-Gómez, Jorge Carlos-Vivas, Sabina Barrios-Fernandez, Eugenio Merellano-Navarro, Daniel Collado-Mateo, Pedro R. Olivares, and José Carmelo Adsuar. 2023. "The Obesity Paradox: Associations between the Body Mass Index and Self-Perceived Health, Depression Status, and Pain Level in Older People" Applied Sciences 13, no. 1: 588. https://doi.org/10.3390/app13010588
APA StyleDenche-Zamorano, Á., Salas-Gómez, D., Carlos-Vivas, J., Barrios-Fernandez, S., Merellano-Navarro, E., Collado-Mateo, D., Olivares, P. R., & Adsuar, J. C. (2023). The Obesity Paradox: Associations between the Body Mass Index and Self-Perceived Health, Depression Status, and Pain Level in Older People. Applied Sciences, 13(1), 588. https://doi.org/10.3390/app13010588











