Changes of Gait Patterns after Correction of Refractive Error in the Elderly with Cataracts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Evaluation of Gait Patterns
2.3. Experimental Procedures
2.4. Analysis of Measurements
3. Results
3.1. The Effect of Correction Glasses for Distance on Gait Patterns in Elderly Subjects
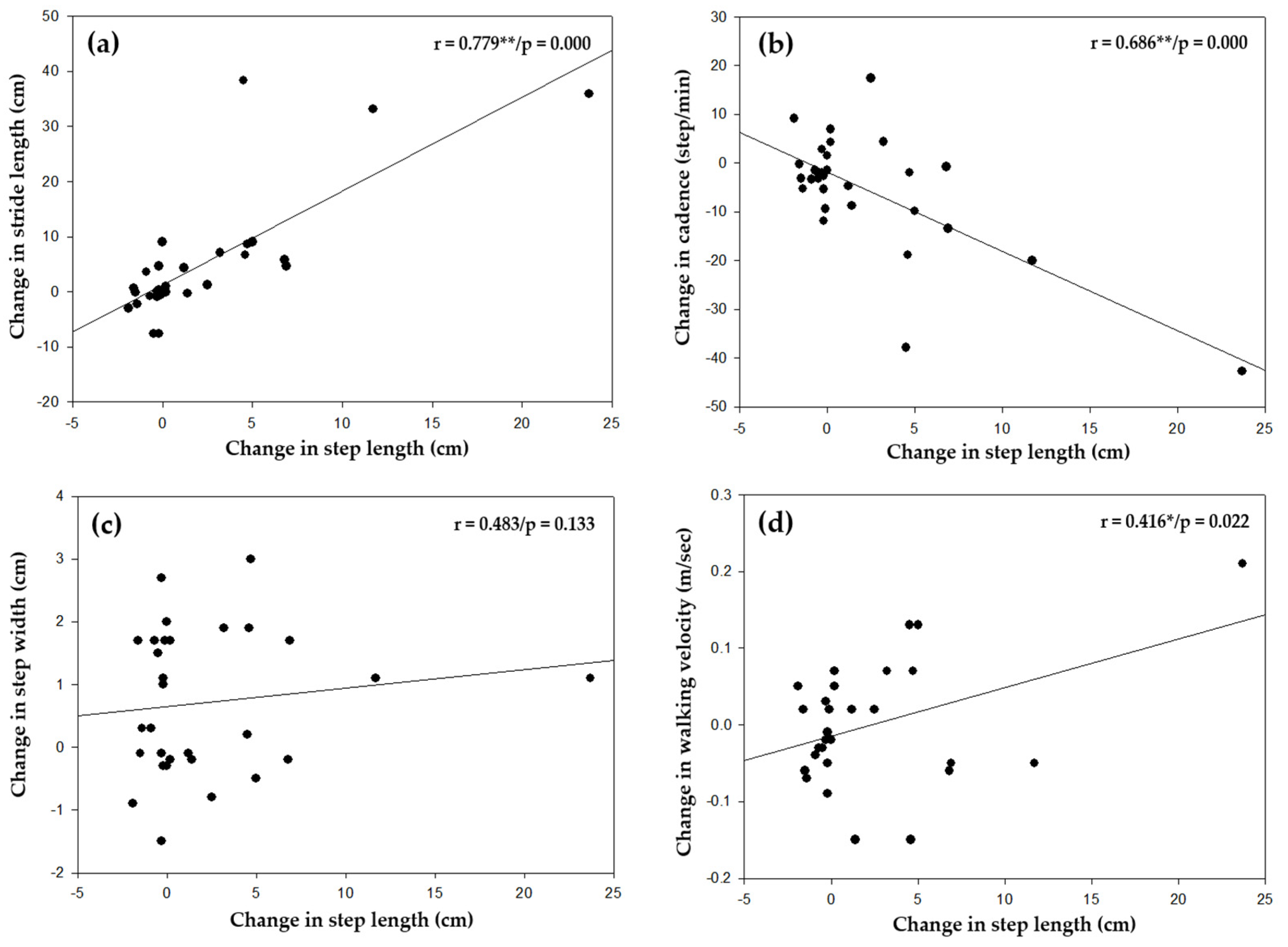
3.2. Analysis of Correlation between Change in Step Length and Each Gait Pattern
3.3. Analysis of Correlation between the Factors of Visual Measurements and Gait Patterns
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.H.; Oh, T.Y. The comparison of characteristics of foot pressure between treadmill and ground walking in normal person. J. Korean Phys. Ther. 2010, 5, 53–61. [Google Scholar]
- Winter, D.A. Human balance and posture control during standing and walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Lim, W.S.; Ryu, T.B.; Choi, H.W.; Chung, M.K. A comparison of gait characteristics between korean and western young people. J. Ergon. Soc. Korea 2006, 25, 33–41. [Google Scholar]
- Beom, J.W. Characteristics of elderly gait. Korean Soc. Prosthet. Orthot. 2014, 8, 29–32. [Google Scholar]
- Yamasaki, M.; Sasaki, T.; Torii, M. Sex difference in the pattern of lower limb movement during treadmill walking. Eur. J. Appl. Physiol. Occup. Physiol. 1991, 62, 99–103. [Google Scholar] [CrossRef]
- Gabell, A.; Nayak, U.S.L. The effect of age and variability in gait. J. Gerontol. 1984, 39, 662–666. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly people living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R.; Robbins, A.S. Falls in the nursing home. Ann. Intern. Med. 1994, 121, 442–451. [Google Scholar] [CrossRef]
- Lackner, J.R.; DiZio, P. Visual stimulation affects the perception of voluntary leg movements during walking. Perception 1998, 17, 71–80. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Plitnick, B.; Rea, M.S.; Gras, L.Z.; Rea, M.S. Lighting and perceptual cues: Effects on gait measures of older adults at high and low risk for falls. BMC Geriatr. 2011, 11, 49. [Google Scholar] [CrossRef]
- Elliott, D.B.; Bullimore, M.A.; Patla, A.E.; Whitaker, D. Effect of a cataract simulation on clinical and real world vision. Br. J. Ophthalmol. 1996, 80, 799–804. [Google Scholar] [CrossRef]
- Kim, J.H. A Study on travel errors of children with low vision. Korean J. Vis. Impair. 2005, 21, 27–41. [Google Scholar]
- Patla, A.E.; Vickers, J.N. Where and when do we look as we approach and step over an obstacle in the travel path. Neuroreport 1997, 8, 3661–3665. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.; Ellwein, L. Prevalence of refractive error in the United States, 1999–2004. Arch. Ophthalmol. 2008, 126, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Moon, B.Y.; Cho, H.G. Changes in falling risk depending on induced axis directions of astigmatism on static posture. J. Phys. Ther. Sci. 2015, 27, 1971–1973. [Google Scholar] [CrossRef]
- Moon, B.Y.; Choi, J.H.; Yu, D.S.; Kim, S.Y. Effect of induced hyperopia on fall risk and Fourier transformation of postural sway. PeerJ 2019, 7, e8329. [Google Scholar] [CrossRef]
- Bae, J.I.; Yu, D.S.; Kim, S.Y. Effect of optical correction by fully corrected glasses on postural stability. PLoS ONE 2020, 15, e0235919. [Google Scholar] [CrossRef]
- Choi, J.H.; Cho, H.G.; Moon, B.Y.; Yu, D.S.; Kim, S.Y. Changes in the gait pattern depending on induced refractive error and correlation analysis of visual functions. J. Korean Opthalmic. Opt. Soc. 2020, 25, 299–306. [Google Scholar] [CrossRef]
- Bernal, A.G.; Becerro-de-Bengoa-Vallejo, R.; Losa-lglesias, M.E. Reliability of the optogait portable photoelectric cell system for the quantification of spatial-temporal parameters of gait in young adults. Gait Posture 2016, 50, 196–200. [Google Scholar] [CrossRef]
- Whittle, M. Gait Analysis an Introduction, 4th ed.; Butterworth-Heinemann Elsevir: Philadelphia, PA, USA, 2007; pp. 54–57. [Google Scholar]
- Carlson, N.B.; Kurtz, D. Clinical Procedures for Ocular Examination, 3rd ed.; McGraw-Hill: New York, NY, USA, 2004; pp. 104–105. [Google Scholar]
- Daher, N.; Lee, S.; Yang, Y.J. Effects of elastic band orthosis (aider) on balance and gait in chronic stroke patients. J. Phys. Ther. Rehabil. Sci. 2013, 2, 81–86. [Google Scholar] [CrossRef]
- Beulertz, J.; Bloch, W.; Prokop, A.; Rustler, V.; Fizen, C.; Herich, L.; Streckmann, F.; Baumann, F.T. Limitations in ankle dorsiflexion range of motion, gait and walking efficiency in childhood cancer survivors. Cancer Nurs. 2016, 39, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Song, C.H.; Lee, K.J.; Jung, S.W.; Shin, D.C.; Shin, S.H. Concurrent validity and test-retest reliability of the OPTOGait phoelectric cell system for the assessment of spatio-temporal parameters of the gait of young adults. J. Phys. Ther. Sci. 2014, 26, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Gaerlan, M.G.; Alpert, P.T.; Cross, C.; Louis, M.; Kowalski, S. Postural balance in young adults: The role of visual, vestibular and somatosensory systems. J. Am. Acad. Nurse Pract. 2012, 24, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Callisaya, M.L.; Blizzard, L.; Schmidt, M.D.; McGinley, J.L.; Srikanth, V.K. Sex modifies the relationship between age and gait: A population-based study of older adults. J. Gerontol. 2008, 63, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Judge, J.O.; Davis, R.B.; Õunpuu, S. Step length reductions in advanced age: The role of ankle and hip kinetics. J. Gerontol. 1996, 51, 303–312. [Google Scholar] [CrossRef]
- Dingwell, J.B.; Marin, L.C. Kinematic variability and local dynamic stability of upper body motions when walking at different speeds. J. Biomech. 2006, 39, 444–452. [Google Scholar] [CrossRef]
- Hak, L.; Houdijk, H.; Steenbrink, F.; Mert, A.; van der Wurff, P.; Beek, P.J.; van Dieën, J.H. Stepping strategies for regulating gait adaptability and stability. J. Biomech. 2013, 46, 905–911. [Google Scholar] [CrossRef]
- Patla, A.E.; Davies, T.C.; Niechwiej, E. Obstacle avoidance during locomotion using haptic information in normally sighted humans. Exp. Brain. Res. 2004, 155, 173–185. [Google Scholar] [CrossRef]
- Wood, J.M.; Lacherez, P.F.; Black, A.A.; Cole, M.H.; Boon, M.Y.; Kerr, G.K. Postural stability and gait among older adults with age-related maculopathy. Investig. Ophthalmol. Vis. Sci. 2009, 50, 482–487. [Google Scholar] [CrossRef]
- Marigold, D.S.; Patla, A.E. Visual information from the lower visual field is important for walking across multi-surface terrain. Exp. Brain. Res. 2008, 188, 23–31. [Google Scholar] [CrossRef]
- Choi, J.H.; Moon, B.Y.; Yu, D.S.; Cho, H.G.; Kim, S.Y. Effects of induced refractive errors on gait patterns. J. Korean Opthalmic. Opt. Soc. 2018, 23, 259–264. [Google Scholar] [CrossRef]
- Brach, J.S.; Berlin, J.E.; VanSwearingen, J.M.; Newman, A.B.; Studenski, S.A. Too much or too little step width variability is associated with a fall history in older persons who walk at or near normal gait speed. J. Neuroeng. Rehabil. 2005, 2, 21. [Google Scholar] [CrossRef]
- Lee, D.N.; Eric, A. Visual proprioceptive control of standing in human infants. Percept. Psychophys. 1974, 15, 529–532. [Google Scholar] [CrossRef]
- Lee, D.N.; Lishman, J.R. Visual proprioceptive control of stance. J. Hum. Mov. Stud. 1975, 1, 87–95. [Google Scholar]
- Yu, D.S.; Kim, S.Y. Changes in postural control ability after wearing corrective glasses for distance in older adults and their causes. Int. J. Environ. Res. Public Health. 2022, 19, 6643. [Google Scholar] [CrossRef] [PubMed]
- Patla, A.E. Understanding the roles of vision in the control of human locomotion. Gait Posture 1997, 5, 54–69. [Google Scholar] [CrossRef]
- Mochon, S.; McMahon, T.A. Ballistic walking. J. Biomech. 1980, 13, 49–57. [Google Scholar] [CrossRef]
- Robert, R. Clinical prediction of falls in the elderly. Am. J. Phys. Med. Rehabil. 1997, 5, 54–69. [Google Scholar]
- Jack, C.I.A.; Smith, T.; Neoh, C.; Lye, M.; McGalliard, J.N. Prevalence of low vision in elderly patients admitted to an acute geriatric unit in Liverpool: Elderly people who fall are more likely to have low vision. Gerontology 1995, 41, 280–285. [Google Scholar] [CrossRef]
- Kannus, P.P.; Sieväneu, H.; Palvanen, M.; Järvien, T.; Parkkari, J. Prevention of falls and consequent injuries in elderly people. Lancet 2005, 366, 1885–1893. [Google Scholar] [CrossRef]

| Condition of Refractive Correction | Factors Affecting Gait Patterns | n | ||||
|---|---|---|---|---|---|---|
| Step Length (cm) | Stride Length (cm) | Cadence (Steps/min) | Step Width (cm) | Walking Velocity (m/s) | ||
| Before | 45.57 ± 5.37 | 89.09 ± 10.41 | 108.16 ± 12.59 | 10.21 ± 2.07 | 0.84 ± 0.16 | each 30 |
| After | 47.78 ± 5.81 | 94.09 ± 12.57 | 102.67 ± 19.74 | 10.93 ± 1.68 | 0.84 ± 0.17 | |
| t/p-value | −2.363/0.025 * | −2.43/0.022 * | 2.467/0.020 * | −3.410/0.002 * | 0.070/0.945 | |
| cogen’s d (effect size) | 0.395 | 0.433 | 0.332 | 0.203 | - | |
| Visual Measurement Factors | Gait Patterns | ||||
|---|---|---|---|---|---|
| Step Length (cm) | Stride Length (cm) | Cadence (Steps/min) | Step Width (cm) | Walking Velocity (m/s) | |
| Spherical equivalent power | r = −0.047/p = 0807 | r = −0.121/p = 0.524 | r = −0.011/p = 0.953 | r = −0.176/p = 0.351 | r = −0.095/p = 0.618 |
| Astigmatic diopter power | r = 0.193/p = 0.307 | r = 0.257/p = 0.171 | r = −0.134/p = 0.480 | r = 0.146/p = 0.442 | r = 0.228/p = 0226 |
| Improvement of visual acuity lines | r = 0.027/p = 0.887 | r = 0.056/p = 0.770 | r = −0.053/p = 0.780 | r = −0.082/p = 0.668 | r = −0.151/p = 0.427 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noh, J.-H.; Cho, H.-G.; Moon, B.-Y.; Yu, D.-S.; Kim, S.-Y. Changes of Gait Patterns after Correction of Refractive Error in the Elderly with Cataracts. Appl. Sci. 2023, 13, 6140. https://doi.org/10.3390/app13106140
Noh J-H, Cho H-G, Moon B-Y, Yu D-S, Kim S-Y. Changes of Gait Patterns after Correction of Refractive Error in the Elderly with Cataracts. Applied Sciences. 2023; 13(10):6140. https://doi.org/10.3390/app13106140
Chicago/Turabian StyleNoh, Jae-Hyeon, Hyun-Gug Cho, Byeong-Yeon Moon, Dong-Sik Yu, and Sang-Yeob Kim. 2023. "Changes of Gait Patterns after Correction of Refractive Error in the Elderly with Cataracts" Applied Sciences 13, no. 10: 6140. https://doi.org/10.3390/app13106140





