Evaluation of Different Priming Agents with Conventional and Bioactive Self-Adhesive Resin Cements on Shear Bond Strength to Zirconia
Abstract
:1. Introduction
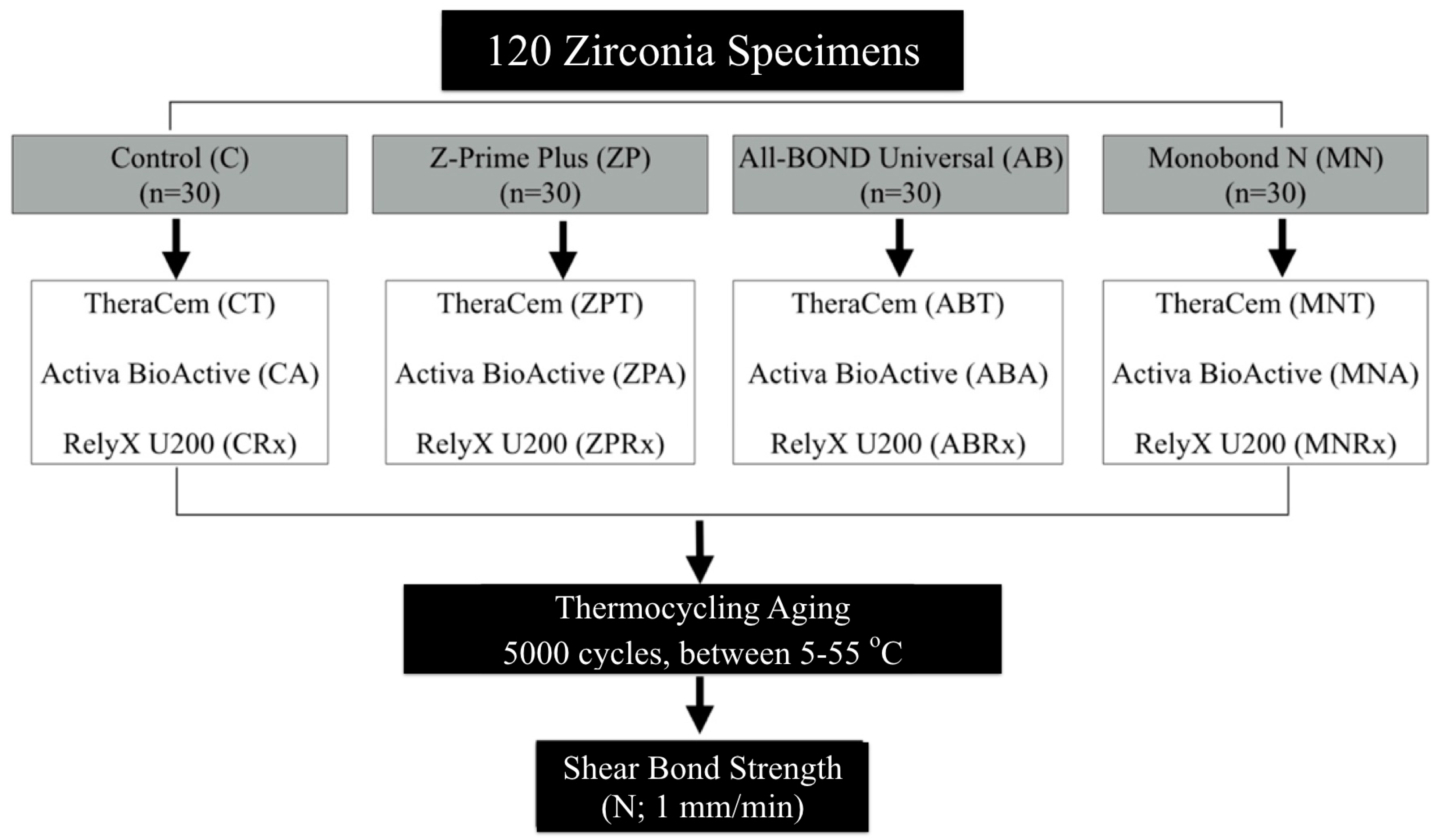
2. Materials and Methods
2.1. Experimental Specimens
2.2. Shear Bond Strength Test
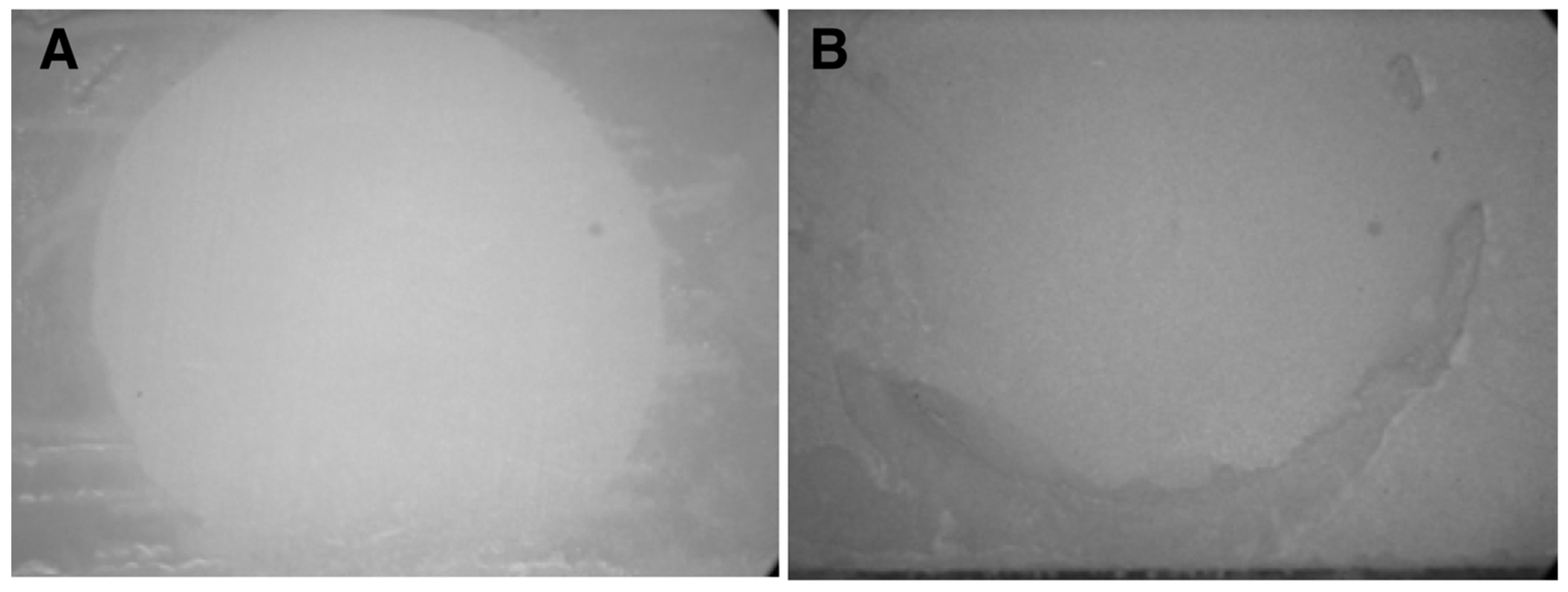
2.3. Failure Evaluation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Self-adhesive bioactive resin cements did not provide sufficient bond strength to zirconia without the application of priming agents.
- Both the priming agent and the cement type have a significant effect on the shear bond strength to zirconia.
- The application of the ceramic primer or bonding agent containing phosphate functional monomer is recommended to achieve a high bond strength.
- Regardless of the cement type, universal ceramic primer MN provided the highest shear bond strength to zirconia. Moreover, regardless of the priming agent used, conventional self-adhesive resin cement Rx provided higher bond strength to zirconia compared to bioactive cements.
- Not all phosphate functional monomers containing primers are effective in providing a reliable bond to zirconia. It is the clinician responsibility to evaluate and select the best cement–primer combination.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sulaiman, T.A.; Altak, A.; Abdulmajeed, A.; Rodgers, B.; Lawson, N. Cleaning zirconia surface prior to bonding: A comparative study of different methods and solutions. J. Prosthodont. 2022, 31, 239–244. [Google Scholar] [CrossRef]
- Hajjaj, M.S.; Alzahrani, S.J. Effect of different cleaning methods on shear bond strength of resin cement to contaminated zirconia. Materials 2022, 15, 5068. [Google Scholar] [CrossRef]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The effect of resin bonding on long-term success of high-strength ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef]
- Comino-Garayoa, R.; Peláez, J.; Tobar, C.; Rodríguez, V.; Suárez, M.J. Adhesion to zirconia: A systematic review of surface pretreatments and resin cements. Materials 2021, 14, 2751. [Google Scholar] [CrossRef]
- Akay, C.; Çakırbay Tanış, M.; Şen, M. Effects of hot chemical etching and 10-metacryloxydecyl dihydrogen phosphate (mdp) monomer on the bond strength of zirconia ceramics to resin-based cements. J. Prosthodont. 2017, 26, 419–423. [Google Scholar] [CrossRef]
- Scaminaci Russo, D.; Cinelli, F.; Sarti, C.; Giachetti, L. Adhesion to zirconia: A systematic review of current conditioning methods and bonding materials. Dent. J. 2019, 7, 74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M.; Bona, A.D.; Pecho, O.E.; Alessandretti, R. Roughness, surface energy, and superficial damages of cad/cam materials after surface treatment zirconia as a dental biomaterial. Clin. Oral Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2003, 19, 725–731. [Google Scholar]
- Nagaoka, N.; Yoshihara, K.; Feitosa, V.P.; Tamada, Y.; Irie, M.; Yoshida, Y.; Van Meerbeek, B.; Hayakawa, S. Chemical interaction mechanism of 10-mdp with zirconia. Sci. Rep. 2017, 7, 45563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Awad, M.M.; Alhalabi, F.; Alzahrani, K.M.; Almutiri, M.; Alqanawi, F.; Albdiri, L.; Alshehri, A.; Alrahlah, A.; Ahmed, M.H. 10-methacryloyloxydecyl dihydrogen phosphate (10-mdp)-containing cleaner improves bond strength to contaminated monolithic zirconia: An in-vitro study. Materials 2022, 15, 1023. [Google Scholar] [CrossRef]
- Inokoshi, M.; De Munck, J.; Minakuchi, S.; Van Meerbeek, B. Meta-analysis of bonding effectiveness to zirconia ceramics. J. Dent. Res. 2014, 93, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Steiner, R.; Heiss-Kisielewsky, I.; Schwarz, V.; Schnabl, D.; Dumfahrt, H.; Laimer, J.; Steinmassl, O.; Steinmassl, P.A. Zirconia primers improve the shear bond strength of dental zirconia. J. Prosthodont. 2020, 29, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Sanohkan, S.; Kukiattrakoon, B.; Larpboonphol, N.; Sae-Yib, T.; Jampa, T.; Manoppan, S. The effect of various primers on shear bond strength of zirconia ceramic and resin composite. J. Conserv. Dent. 2013, 16, 499–502. [Google Scholar]
- Shokry, M.; Al-Zordk, W.; Ghazy, M. Retention strength of monolithic zirconia crowns cemented with different primer-cement systems. BMC Oral. Health 2022, 22, 187. [Google Scholar] [CrossRef]
- Amaral, M.; Belli, R.; Cesar, P.F.; Valandro, L.F.; Petschelt, A.; Lohbauer, U. The potential of novel primers and universal adhesives to bond to zirconia. J. Dent. 2014, 42, 90–98. [Google Scholar] [CrossRef]
- Kim, J.H.; Chae, S.Y.; Lee, Y.; Han, G.J.; Cho, B.H. Effects of multipurpose, universal adhesives on resin bonding to zirconia ceramic. Oper. Dent. 2015, 40, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Klaisiri, A.; Krajangta, N.; Thamrongananskul, N. The durability of zirconia/resin composite shear bond strength using different functional monomer of universal adhesives. Eur. J. Dent. 2021, 16, 756–760. [Google Scholar] [CrossRef]
- Llerena-Icochea, A.E.; Costa, R.M.; Borges, A.; Bombonatti, J.; Furuse, A.Y. Bonding polycrystalline zirconia with 10-mdp-containing adhesives. Oper. Dent. 2017, 42, 335–341. [Google Scholar] [CrossRef]
- Tayal, A.; Niyogi, A.; Adhikari, H.D.; Adhya, P.; Ghosh, A. Comparative evaluation of effect of one coat 7 universal and tetric n-bond universal adhesives on shear bond strength at resin-zirconia interface: An in vitro study. J. Conserv. Dent. 2021, 24, 336–340. [Google Scholar] [CrossRef]
- Vasconcelos Monteiro, R.; Dos Santos, D.M.; Chrispim, B.; Bernardon, J.K.; Soares Porto, T.; De Souza, G.M. Effect of universal adhesives on long-term bond strength to zirconia. J. Adhes. Dent. 2022, 24, 385–394. [Google Scholar]
- Özcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J. Adhes. Dent. 2015, 17, 7–26. [Google Scholar] [PubMed]
- Abdelraouf, R.M.; Mohammed, M.; Abdelgawad, F. Evaluation of shear-bond-strength of dental self-adhering flowable resin-composite versus total-etch one to enamel and dentin surfaces: An in-vitro study. Open Access Maced. J. Med. Sci. 2019, 7, 2162–2166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamdy, T.M. Interfacial microscopic examination and chemical analysis of resin-dentin interface of self-adhering flowable resin composite. F1000Research 2017, 6, 1688. [Google Scholar] [CrossRef] [PubMed]
- Behr, M.; Zeman, F.; Baitinger, T.; Galler, J.; Koller, M.; Handel, G.; Rosentritt, M. The clinical performance of porcelain-fused-to-metal precious alloy single crowns: Chipping, recurrent caries, periodontitis, and loss of retention. Int. J. Prosthodont. 2014, 27, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Francois, P.; Fouquet, V.; Attal, J.P.; Dursun, E. Commercially available fluoride-releasing restorative materials: A review and a proposal for classification. Materials 2020, 13, 2313. [Google Scholar] [CrossRef] [PubMed]
- Başol, E.U.; Vallittu, P.K.; Lassila, L.V.J.; Cekic Nagas, I. Effect of bioactive glass particles on mechanical and adhesion properties of resin cements. J. Prosthodont. Res. 2023; Online ahead of print. [Google Scholar]
- Sakrana, A.A.; Al-Zordk, W.; Shoukry, H.; Özcan, M. Bond strength durability of adhesive cements to translucent zirconia: Effect of surface conditioning. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 161–171. [Google Scholar]
- Mahrous, A.; Radwan, M.M.; Kamel, S.M. Micro-shear bond strength of novel mdp calcium-fluoride-releasing self-adhesive resin cement after thermocycling. Int. J. Periodontics Restor. Dent. 2020, 40, 445–455. [Google Scholar] [CrossRef]
- Chen, L.; Yang, J.; Wang, J.R.; Suh, B.I. Physical and biological properties of a newly developed calcium silicate-based self-adhesive cement. Am. J. Dent. 2018, 31, 86–90. [Google Scholar]
- De-Paula, D.M.; Loguercio, A.D.; Reis, A.; Frota, N.M.; Melo, R.; Yoshihara, K.; Feitosa, V.P. Micro-raman vibrational identification of 10-mdp bond to zirconia and shear bond strength analysis. BioMed Res. Int. 2017, 2017, 8756396. [Google Scholar] [CrossRef] [Green Version]
- Vohra, F.; Altwaim, M.; Alshuwaier, A.S.; Alomayri, A.; Al Deeb, M.; AlFawaz, Y.F.; Alrabiah, M.; Al Ahdal, K.; Al Deeb, L.; Abduljabbar, T. Bond integrity and microleakage of dentin-bonded crowns cemented with bioactive cement in comparison to resin cements: In vitro study. J. Appl. Biomater. Funct. Mater. 2020, 18, 2280800020905768. [Google Scholar] [CrossRef]
- Zmener, O.; Pameijer, C.H.; Hernández, S. Resistance against bacterial leakage of four luting agents used for cementation of complete cast crowns. Am. J. Dent. 2014, 27, 51–55. [Google Scholar] [PubMed]
- Lööf, J.; Svahn, F.; Jarmar, T.; Engqvist, H.; Pameijer, C.H. A comparative study of the bioactivity of three materials for dental applications. Dent. Mater. 2008, 24, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, P.; Farheen, F.; Lawson, N.; Burgess, J.; Robles, A. Ion release and flexural strength of bioactive materials. In Proceedings of the AADR/CADR Annual Meeting, Fort Lauderdale, FL, USA, 21–24 March 2018; Volume 97. [Google Scholar]
- Owens, B.M.; Phebus, J.G.; Johnson, W.W. Evaluation of the marginal integrity of a bioactive restorative material. Gen. Dent. 2018, 66, 32–36. [Google Scholar] [PubMed]
- AbuHaimed, T.S.; Alzahrani, S.J.; Farsi, S.A.; Al-Turki, L.E.; Hajjaj, M.S. The effect of repeated pressing on the flexural strength, color stability, vickers hardness, and surface topography of heat-pressed lithium disilicate. Materials 2022, 15, 6787. [Google Scholar] [CrossRef]
- Kim, D.-S.; Ahn, J.-J.; Bae, E.-B.; Kim, G.-C.; Jeong, C.-M.; Huh, J.-B.; Lee, S.-H. Influence of non-thermal atmospheric pressure plasma treatment on shear bond strength between y-tzp and self-adhesive resin cement. Materials 2019, 12, 3321. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.E.; Kim, J.H.; Shim, J.S.; Roh, B.D.; Shin, Y. Effect of surface treatment on shear bond strength between resin cement and ce-tzp/al2o3. Biomed. Res. Int. 2016, 2016, 7576942. [Google Scholar] [CrossRef] [Green Version]
- Cacciafesta, V.; Sfondrini, M.F.; Lena, A.; Scribante, A.; Vallittu, P.K.; Lassila, L.V. Force levels of fiber-reinforced composites and orthodontic stainless steel wires: A 3-point bending test. Am. J. Orthod. Dentofacial Orthop. 2008, 133, 410–413. [Google Scholar] [CrossRef]
- Rodríguez-Ivich, J.; Razaghy, M.; Henriques, B.; Magne, P. Accelerated fatigue resistance of bonded composite resin and lithium disilicate screw-retained incisor crowns with long and short titanium bases. Int. J. Periodontics Restor. Dent. 2022, 42, 459–469. [Google Scholar] [CrossRef]
- Poggio, C.; Dagna, A.; Chiesa, M.; Colombo, M.; Scribante, A. Surface roughness of flowable resin composites eroded by acidic and alcoholic drinks. J. Conserv. Dent. 2012, 15, 137–140. [Google Scholar] [CrossRef] [Green Version]
- Abdulmajeed, A.A.; Suliman, A.A.; Selivany, B.J.; Altitinchi, A.; Sulaiman, T.A. Wear and color stability of preheated bulk-fill and conventional resin composites. Oper. Dent. 2022, 47, 585–592. [Google Scholar] [CrossRef]

| Materials | Manufacturer | Composition |
|---|---|---|
| IPS e.max ZirCAD MO 0 | Ivoclar Vivadent a | ZrO2, Y2O3, HfO2, Al2O3, and other oxides. |
| Korox 50 | BEGO b | Al2O3 (50 μm). |
| Z-PRIME Plus (ZP) | BISCO c | 10-MDP, carboxylic acid monomer, BPDM, and ethanol. |
| All-Bond Universal (AB) | BISCO c | 10-MDP, BPDM, Bis-GMA, HEMA, water, ethanol, and photoinitiator. |
| Monobond N (MN) | Ivoclar Vivadent a | Alcohol solution of silane methacrylate, phoshphoric acid methacrylate, and sulphide methacrylate. |
| TheraCem (T) | BISCO c | Base: Calcium base filler, glass filler, dimethacrylate, ytterbium fluoride, initiator, and amorphous silica. Catalyst: Glass filler, MDP, and amorphous silica. |
| ACTIVA BioACTIVE (A) | Pulpdent d | Base: Diurethane dimethacrylate and other methacrylate-based monomers and oligomers, polyacrylic acid/maleic acid copolymer, water, barium borosilicate glass, silica, reducing agents, photoinitiators, and colorants. Catalyst: Diurethane dimethacrylate and other methacrylate-based monomers and oligomers, aluminoflurosilicate ionomer glass, silica, and oxidizing agents. |
| RelyX U200 Automix (Rx) | 3M ESPE e | Base: Methacrylate monomers containing phosphoric acid groups, methacrylate monomers, silanated fillers, initiator components, stabilizer, and Rheological additives. Catalyst: Methacrylate monomers, alkaline (basic) fillers, silanated fillers, initiator components, stabilizer, pigments, and rheological additives. |
| Group | Mean (MPa) ± SD | Coefficient of Variation (CV) | Standard Error of Mean (SEM) | 95% Confidence Interval for Mean | Failure Mode (N) | ||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Adhesive Failure | Mixed Failure | ||||
| ZPT | 5.39 ± 2.60 C,D | 48.24% | 0.92 | 3.21 | 7.56 | 6 | 4 |
| ZPA | 4.89 ± 1.29 D | 26.30% | 0.41 | 3.97 | 5.81 | 8 | 2 |
| ZPRx | 7.07 ± 1.53 C,D | 21.61% | 0.51 | 5.89 | 8.24 | 5 | 5 |
| ABT | 5.60 ± 2.45 C,D | 43.82% | 0.87 | 3.55 | 7.65 | 9 | 1 |
| ABA | 6.19 ± 2.63 C,D | 42.46% | 0.83 | 4.31 | 8.07 | 7 | 3 |
| ABRx | 13.41 ± 2.27 A,B | 16.90% | 0.72 | 11.79 | 15.03 | 9 | 1 |
| MNT | 10.30 ± 3.14 B,C | 30.52% | 1.05 | 7.88 | 12.71 | 2 | 8 |
| MNA | 13.04 ± 4.34 A,B | 33.25% | 1.45 | 9.71 | 16.37 | 0 | 10 |
| MNRx | 16.46 ± 5.97 A | 36.26% | 1.99 | 11.88 | 21.05 | 0 | 10 |
| df | Mean Square | F | p Value | ||
|---|---|---|---|---|---|
| Between Groups | 1332.86 | 8 | 166.61 | 16.30 | 0.00000 * |
| Within Groups | 745.97 | 73 | 10.22 | ||
| Total | 2078.83 | 81 |
| Source | Type III Sum of Square | df | Mean Square | F | p * |
|---|---|---|---|---|---|
| Corrected Model | 1332.86 | 8 | 166.61 | 16.30 | <0.001 * |
| Intercept | 6818.81 | 1 | 6818.81 | 667.28 | <0.001 * |
| Priming agent | 777.11 | 2 | 388.56 | 38.02 | <0.001 * |
| Cement type | 420.03 | 2 | 210.02 | 20.55 | <0.001 * |
| Interaction | 119.14 | 4 | 29.78 | 2.91 | 0.027 * |
| Error | 745.97 | 73 | 10.22 | ||
| Total | 9023.36 | 82 | |||
| Corrected Total | 2078.83 | 81 |
| Priming Agent. | Mean (MPa) ± SD | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| MN | 13.27 ± 5.14 A | 12.04 | 14.49 |
| AB | 8.40 ± 4.36 B | 7.19 | 9.61 |
| ZP | 5.78 ± 2.01 C | 4.55 | 7.01 |
| Cement Type | Mean (Mpa) ± SD | 95% Confidence Interval | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| T | 7.10 ± 3.54 B | 5.82 | 8.37 |
| A | 8.04 ± 4.50 B | 6.86 | 9.22 |
| Rx | 12.3 ± 5.32 A | 11.11 | 13.52 |
| Priming Agent | Fracture Mode | Chi-Squared | p Value | |||
|---|---|---|---|---|---|---|
| Adhesive | Mixed | |||||
| ZP | 19 | 63.33% | 11 | 36.67% | 37.97 | <0.001 * |
| AB | 25 | 83.33% | 5 | 16.67% | ||
| MN | 2 | 6.67% | 28 | 93.33% | ||
| Cement Type | Fracture Mode | Chi-Squared | p Value | |||
|---|---|---|---|---|---|---|
| Adhesive | Mixed | |||||
| T | 17 | 56.67% | 13 | 43.33% | 0.62 | 0.732520 |
| A | 15 | 50.00% | 15 | 50.00% | ||
| Rx | 14 | 46.67% | 16 | 53.33% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hajjaj, M.S.; Barboud, H.M.; Almashabi, H.K.; Alzahrani, S.J.; Abu Haimed, T.S.; Alnoury, A.S.; Sulaiman, T.A. Evaluation of Different Priming Agents with Conventional and Bioactive Self-Adhesive Resin Cements on Shear Bond Strength to Zirconia. Appl. Sci. 2023, 13, 8369. https://doi.org/10.3390/app13148369
Hajjaj MS, Barboud HM, Almashabi HK, Alzahrani SJ, Abu Haimed TS, Alnoury AS, Sulaiman TA. Evaluation of Different Priming Agents with Conventional and Bioactive Self-Adhesive Resin Cements on Shear Bond Strength to Zirconia. Applied Sciences. 2023; 13(14):8369. https://doi.org/10.3390/app13148369
Chicago/Turabian StyleHajjaj, Maher S., Hebah M. Barboud, Heba K. Almashabi, Saeed J. Alzahrani, Tariq S. Abu Haimed, Arwa S. Alnoury, and Taiseer A. Sulaiman. 2023. "Evaluation of Different Priming Agents with Conventional and Bioactive Self-Adhesive Resin Cements on Shear Bond Strength to Zirconia" Applied Sciences 13, no. 14: 8369. https://doi.org/10.3390/app13148369






